Chapter 39 Musculoskeletal Disorders of the Lower Limb
Hip Tests
Faber or Patrick Test
The patient lies supine and the hip is flexed, abducted, and externally rotated with the ankle resting on the contralateral knee. The examiner applies pressure to the contralateral ilium and ipsilateral knee to further externally rotated the hip. The test is positive for sacroiliac joint pathologic findings if the patient’s buttock pain is reproduced. The test is positive for hip pathologic findings if the patient’s groin pain is reproduced.
Knee Tests
Rehabilitation Principles of Lower Limb Injury
Several terms are used throughout the chapter that might not be familiar to all readers. For the sake of clarity, we would like to first define some of these terms. First and foremost, the term kinetic chain refers to the model of human motion that analyzes and treats dysfunction along connected anatomic regions, rather than focusing only on the location of pain. This model recognizes that dysfunction in one anatomic region can cause dysfunction in other anatomic regions that are linked to the first region during motion. Treatment plans that address only the painful site, and ignore underlying pathologic conditions at other sites along the motion chain, have less chance of success than a treatment plan that restores proper function along the entire chain. Kinetic chain considerations are most relevant when discussing muscle and tendon pathologic conditions but should not be ignored when addressing bone and joint pathologic findings.
The term biomechanical deficit refers to any deficiencies in range of motion, flexibility, strength, endurance, or motor control. The term muscle imbalance refers to the divergence from normal function of different muscle groups that work as agonists or antagonists to stabilize a body part or create motion. Muscle imbalances often occur between muscles on the anterior versus posterior side of a joint, such as the hip flexors versus the hip extensors, or the medial versus lateral side of a joint, such as hip adductors versus hip abductors. Some authors have suggested that these types of muscle imbalances predispose to sports injuries.33,71,142
It is important to mention a precaution that should be taken into account when treating patients. It has been common practice to use nonsteroidal antiinflammatory drugs (NSAIDs) to treat musculoskeletal injuries to control pain and reduce inflammation. Evidence shows that NSAIDs can impair muscle healing by inhibiting the fusion of myogenic precursor cells, and this knowledge should be considered before prescribing these medications.101,132
Musculoskeletal Disorders of the Lower Limb
General Approach to Osteoarthritis in the Lower Limb
Plain films are the study of choice to assess for osteoarthritis. The radiologic hallmarks of osteoarthritis include decreased joint space, marginal osteophytosis, subchondral cyst formation, and subchondral sclerosis (Figure 39-1).88
Many treatment options are available for lower limb osteoarthritis. A patient can sometimes diminish symptoms simply by modifying activities. Switching from higher impact activities such as basketball to lower impact activities such as bicycling or swimming can decrease or eliminate joint pain.83,148 Ice, acetaminophen, and NSAIDs can all reduce joint pain. Glucosamine and chondroitin sulfate have shown mixed results for reducing pain in knee osteoarthritis.82,93,125,126,145 Strength training and aerobic exercise can improve joint control and decrease pain.113 Strategies aimed at reducing loads on joints include weight loss, cushioned shoes, and walking aids such as a cane.151 Intraarticular injection of anesthetic and steroid can be helpful both diagnostically and therapeutically.115,139 Recent evidence shows that bupivacaine in concentrations 0.5% or more is chondrotoxic, and it would seem judicious to avoid its use in joint injections.31 Injections of the foot, ankle, and hip joints are best performed under fluoroscopic guidance with contrast confirmation. Several investigations looking at knee osteoarthritis have concluded that intraarticular injections of hyaluronate relieve pain and improve function in patients with mild and moderate knee osteoarthritis.2,63,74,86 For patients with recalcitrant pain or severe functional limitations, arthroplasty can provide substantial improvement in pain and function.
Stress Reactions and Stress Fractures in the Lower Limb
Repetitive overload injuries to the bones of the lower limb are common in physically active individuals, especially those who participate in endurance activities such as distance running. In cases of repetitive stress, or in the setting of impaired bone metabolism, bone strain occurs on a continuum from “stress response” or “stress reaction” to overt stress fracture. Bone overload can occur in any location in the lower limb (Figure 39-2). The ability of bone to withstand repetitive forces without breaking down depends on several factors. The stronger the bone is before being subjected to repetitive loading, the better it is able to withstand the loads applied to it. Both intrinsic and extrinsic factors are important to consider in determining the risk for stress reactions or stress fractures. Intrinsic risk factors include poor dietary habits, altered menstrual status, and biomechanical abnormalities that do not allow for proper distribution of forces along the kinetic chain. Extrinsic factors can include hard training surfaces, training errors, and improper footwear and insoles.
Athletes report a greater frequency of disordered eating patterns than the general population, especially in sports emphasizing leanness.121 Individuals with disordered eating can have insufficient dietary intake of calories, protein, calcium, and other nutrients needed to achieve optimal bone quality. The triad of disordered eating, amenorrhea, and low bone density that occurs in athletic females is referred to as the female athlete triad. Restrictive eating behaviors increase the likelihood of stress fractures in women.14,15,46,105 Low caloric intake with negative protein balance has been hypothesized as one of the mechanisms for menstrual disturbances in female athletes.155 Evidence shows that menstrual and hormonal disturbances increase the risk of stress fracture and lead to premature bone loss, particularly at trabecular sites.64,103
Flexibility, although difficult to study, can play a role in fracture risk. Some studies have suggested that increased hip external rotation and decreased ankle dorsiflexion might increase the risk for stress fractures in certain populations.50,51,60
Skeletal alignment affects the amount of force absorbed by the foot, and how much force is transferred to proximal structures during ground contact. A rigid pes cavus foot is less able to absorb shock during and just after heel strike, and can transmit greater forces to proximal bones than a foot that is able to undergo normal pronation. Similarly, a pes planus foot does not allow the normal pronation mechanism to properly absorb forces. Either foot alignment can increase the risk of a stress fracture, the location of which can vary depending on the foot type and activity.91,134 Other studies looking at alignment have suggested that leg length discrepancy and increased Q angle can increase the risk of stress fracture.27
Although it is clear that training errors contribute to stress fractures, there is limited research identifying the contribution of various training components. Furthermore, appropriate training regimens vary greatly among individuals. Athletes should be encouraged to keep training logs documenting type of training, volume, intensity, and rest periods. A rapid increase in training volume and intensity often precedes a stress fracture, just as it might precede a muscle–tendon overload injury. Articles about training in military recruits have shown that elimination of running and marching on concrete, preentry physical conditioning, and inclusion of rest periods reduced stress fracture risk.54,130,131
Shoes and insoles can be an important component in minimizing stress fracture risk. Proper shoe fit that matches an individual’s foot type, as well as adequate support and shock absorption, is essential. Studies looking at the effect of insoles or other footwear modifications on the prevention of stress fractures have shown a reduction in the number of stress fractures by more than 50%.52,96,97
Imaging studies are not always necessary. A 6-week period of relative rest with nonimpact rehabilitation and alternative training methods such as pool running can be instituted. Imaging can be reserved for individuals who remain symptomatic and are unable to return to full activities. In these cases, or when definitive diagnosis is required sooner, the initial imaging study of choice is radiographs. It should be kept in mind, however, that plain films are relatively insensitive and detect less than 50% of stress fractures.75,76 When radiographs are normal but the suspicion for stress fracture remains high, advanced imaging studies are appropriate. Bone scans are sensitive for detecting stress fractures but lack anatomic definition. They can also remain positive long after symptoms have resolved. This limits the ability of bone scans to aid in return-to-sport decisions.138 Magnetic resonance imaging (MRI) provides excellent anatomic information and can be more useful in grading lesions and assessing soft tissue structures.6 At our institution, MRI is the study of choice to look for stress fractures. Computed tomography (CT) provides optimal definition of bony architecture.
Reduced muscle size and strength have been shown to predispose to stress fractures.59 In endurance events, muscle fatigue can increase the strain on bone.154 Muscle mass is important to build and maintain because the load placed on bone can be reduced at sites when muscles are better able to absorb repetitive impact.129 A strengthening program should begin immediately after a diagnosis of stress fracture is made. The exercises prescribed should not cause pain at the fracture site.
Inactivity has negative consequences on the cardiovascular system, metabolism, and skeletal muscle after even brief periods of rest. It is important that fitness be maintained in ways that avoid overloading the bone. The most common cross-training activities include cycling, swimming, water running, rowing, and Stairmaster. The more sport specific the cross-training, the better the carryover effect of the training. It is for this reason that deep water running has become so popular among runners with stress fractures. Studies have shown no significant differences in maximal oxygen uptake, anaerobic threshold, running economy, stride length, and 2-mile performance after 4 to 8 weeks of land versus deep water running training.38,58,153 In sports requiring specific skills, the neuromuscular adaptations are not easily duplicated with cross-training, and it is important to find appropriate ways to resume these isolated sport-specific skills as soon as possible.
Conditions of the Hip Region
Femoral Neck Stress Fractures
With femoral neck stress fractures, symptoms are often vague, and one should have a high index of suspicion to catch this diagnosis early and avoid complications such as displacement or avascular necrosis. If suspicion is present, an MRI should be obtained (Figure 39-3). Fractures on the tension side (lateral) are less common and require immediate surgical referral. Fractures on the compression side (medial) are more common. If the fracture line extends more than 50% of the width of the femoral neck, percutaneous fixation should be considered because the likelihood of displacement is higher.6,32,133 When the fracture line is less than 50% of the width of the femoral neck, strict non–weight-bearing status is necessary for about 4 to 6 weeks until the patient is pain free. This should be followed by functional rehabilitation with progressive weight-bearing over the next 4 to 8 weeks according to symptoms. If the athlete is not progressing as expected, additional radiologic evaluation should be considered.
Avascular Necrosis
Avascular necrosis, also called osteonecrosis, is the death of bone resulting from a lack of blood supply. This can lead to microfractures and eventually collapse of the bone. The femoral head is the most commonly affected location. Disruption of the normal blood supply to the femoral head can be caused by various conditions including trauma, high doses of corticosteroids, alcohol abuse, and systemic illness (such as diabetes, lupus, and sickle cell anemia).84 The severity of symptoms with avascular necrosis is usually related to the degree of articular surface disruption. Symptoms are similar to those experienced with hip osteoarthritis, including groin pain that increases with weight-bearing. Often there is limited motion and pain with internal rotation, flexion, and adduction of the hip. Radiographs can reveal sclerosis of the femoral head or, in severe cases, collapse of the femoral head (Figure 39-4). In mild cases, the plain films can be normal. MRI and CT can detect the condition in its earlier stages. Conservative treatment might include minimizing weight-bearing of the affected joint and use of pain medications. Once collapse occurs, joint replacement surgery is indicated.
Legg-Calvé-Perthes Disease
Legg-Calvé-Perthes disease is idiopathic osteonecrosis of the femoral head in children. It occurs most frequently in boys between the ages of 4 and 8 years. Because bone repair is relatively rapid in children, the prognosis is significantly better compared with adults with avascular necrosis. Signs of Legg-Calvé-Perthes disease in a child include limping and restriction in hip motion, especially hip abduction. The child might complain of groin or thigh pain. Healing can occur in children with revascularization of the femoral head and remodeling of the bone. The prognosis is better in younger children and those with milder involvement. In children under the age of 6 years, observation and use of an abduction brace to maintain the femoral head in a spherical state is reasonable. Osteotomy is sometimes performed in older children.85
Slipped Capital Femoral Epiphysis
The most common hip disorder in adolescents is slipped capital femoral epiphysis. Injury to the physeal plate of the proximal femur with medial displacement of the femoral head relative to the femoral shaft can be due to acute trauma or repetitive microtrauma. Slipped capital femoral epiphysis is rare in boys under age 11 years and girls under age 9 years, and is more common in overweight boys.85 There can be an association with hypothyroidism and renal osteodystrophy.48 Slipped capital femoral epiphysis is bilateral about 50% of the time.85 An adolescent with an acute slip typically presents with severe hip pain that is exacerbated with any motion. The individual tends to hold the hip flexed and externally rotated. Anteroposterior and lateral radiographs confirm the diagnosis(Figure 39-5). A mild slip can be treated conservatively.127 Otherwise, one attempt at closed reduction can be done. If this is unsuccessful, open reduction should be done. After reduction, gentle range of motion can be started within a few days, but weight-bearing is restricted for 4 to 6 weeks.127 After this period, gradually progressive strengthening and functional exercises can be advanced. Complications include nonunion, avascular necrosis of the femoral head, rotational deformity, and osteoarthritis.85,137
Hip Dislocation
Because of the depth of the acetabulum, dislocation of the femoral–acetabular joint requires significant trauma. In children, hip dislocation is more common than hip fractures. In adults, fractures of the acetabulum often accompany hip dislocations. Most commonly, the head of the femur dislocates posteriorly relative to the acetabulum.102 The patient with an acute posterior hip dislocation presents with severe hip pain and tends to hold the hip in flexion, internal rotation, and adduction. With the less common anterior dislocations, the hip is held in an extended, abducted, and externally rotated position.
On physical examination, there will be an obvious deformity. The patient will not tolerate range of motion or resistance testing because of pain. A complete neurologic examination should be performed to assess for lumbosacral plexopathy, sciatic neuropathy, and femoral neuropathy.92 One should always assess for associated injuries, in particular spine and ipsilateral knee trauma, which can be masked by hip pain. Radiographs are indicated to confirm the clinical diagnosis and look for associated injuries. Hip dislocations are an orthopedic emergency, and closed reduction under anesthesia should be performed as soon as possible. Postreduction radiographs are obtained to confirm anatomic alignment. At times, CT or MRI is obtained if further characterization of associated injuries is needed.
Surgery is indicated if attempts at closed reduction are unsuccessful. The surgical goals are to repair displaced or comminuted fractures and remove intraarticular loose bodies.36 Most clinicians recommend non–weight-bearing for 3 to 4 weeks, followed by protected weight-bearing for an additional 3 weeks.127 Gradually progressive rehabilitation can start a few days to a couple of weeks after reduction, depending on the patient’s comfort level and whether surgery was performed. The most concerning complications of hip dislocation include posttraumatic osteoarthritis and avascular necrosis, which occurs in up to 10% of patients.137 The risk of avascular necrosis increases with age, reduction delayed greater than 6 hours, and more severe trauma to the hip joint.
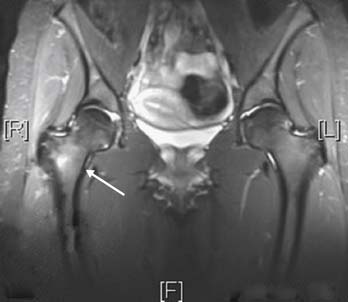
Labral Injuries
Acetabular labral tears are analogous to glenoid labral tears, with some notable exceptions. Patients with acetabular labral tears often present with painful catching of the hip, especially when the hip is at a particular angle.90 There might be a clear history of acute or repetitive trauma. Femoral–acetabular grind maneuvers might reproduce symptoms. Historical features and physical examination maneuvers are even less specific for acetabular labral tears than they are for glenoid labral tears. This might be because the hip is a larger, deeper joint with less sensitive innervation than the shoulder joint. Magnetic resonance arthrography with gadolinium contrast is the imaging study of choice to assess for these injuries (Figure 39-6). Definitive diagnosis is by arthroscopy or open surgery.
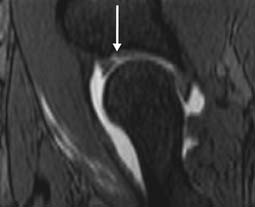
FIGURE 39-6 Gadolinium-enhanced sagittal magnetic resonance image of the hip, showing an anterior labral tear.
Treatments can include acetaminophen or NSAIDs, relative rest, intraarticular steroid injections, and surgical debridement or repair. The arthroscopic and open surgical approaches to labral injuries of the hip continue to evolve.20,21,39,69
Femoroacetabular Impingement Syndrome
In recent years, there has been greater attention given to the concept of femoroacetabular impingement. The condition is characterized by early contact during hip motion between skeletal prominences, limiting range of motion (particularly in flexion and internal rotation). Two types of impingement exist. Pincer impingement is the acetabular cause of impingement and is characterized by overcoverage of the femoral head. Cam impingement is the femoral cause and is due to an aspherical portion of the femoral head–neck junction. Currently, most authorities think that repetitive stress to these osseous prominences leads to chondral damage over time with resultant early osteoarthritis of the hip if the underlying cause of impingement is not addressed.47
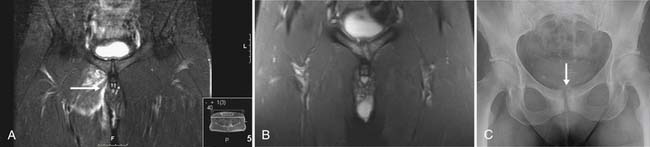
Athletic Pubalgia and Sportsman’s Hernia
Athletic pubalgia and sportsman’s hernia refer to a spectrum of disorders that cause pain in the lower abdomen and groin. Pain generators can include overload of one or more of the lower abdominal muscles near the superior pubic ramus, a strain of the hip flexors and/or hip adductors, stress response or stress fracture of the pubic rami, and pubic symphysitis (Figure 39-7).8,44,45,68,87 A defect in the fascia of the lower anterior abdominal wall has also been described. Overload injury in this region is most commonly seen in football, soccer, and hockey.∗ There can be a delay in accurate diagnosis, and rehabilitation is often incomplete. Because symptoms of athletic pubalgia can easily become chronic, it is imperative to establish an accurate and complete diagnosis and to institute comprehensive rehabilitation as early as possible. Maximizing core stability and restoring full range of motion, strength, endurance, and motor control of the core muscles, hip flexors, and hip adductors are keys to successful rehabilitation. A key tenet of the rehabilitation of athletic pubalgia is balancing abdominal strength with hip girdle flexibility to theoretically reduce sheer forces across the anterior pelvis. Functional exercises involving these muscle groups should be started as soon as the patient is able to tolerate them. Surgical consultation should be considered if there is a suspicion for a fascial defect of the anterior abdominal wall or a true inguinal hernia.135 Impact or repetitive loading activities should be avoided in the setting of bone overload, such as pelvic stress response or stress fracture.
Rectus Femoris Avulsion From the Anterior Inferior Iliac Spine
A forceful contraction of rectus femoris can result in an avulsion fracture of the anterior inferior iliac spine. This diagnosis is distinguished from a simple muscle strain by radiographs, but treatment follows the same rehabilitation guidelines: with ice, relative rest, and gently progressive stretching and strengthening exercises as tolerated. Surgery is indicated only for dramatically displaced avulsion fragments, which are uncommon.99,100
Conditions of the Thigh Region
Disorders of the Iliotibial Band, Including Trochanteric Bursitis
The iliotibial band (ITB) is a strong fascial band that runs along the lateral aspect of the thigh from the level of the greater trochanter to the proximal, anterolateral tibia (Figure 39-8). ITB motion is controlled proximally primarily by the gluteus maximus and tensor fascia lata, the two muscles that insert into it. The ITB inserts distally onto a bony prominence at the proximal, anterolateral tibia called Gerdy’s tubercle. Therefore the ITB can exert forces at the hip and knee. Conversely, alterations in various lower limb mechanics, such as genu valgum, pes planus, and tibial internal or external rotation, can affect ITB function. Three clinically important bursae are related to the ITB.112 The proximal bursa is positioned to decrease friction between the ITB and the greater trochanter of the femur. Another site of potential friction is where the ITB runs over the lateral epicondyle of the femur.18 The third lies at the ITB’s distal attachment on the tibia.
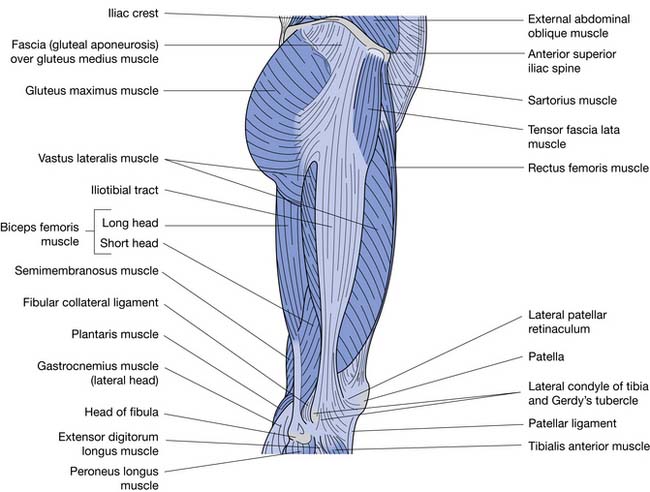
FIGURE 39-8 The iliotibial band is a strong fascial band that runs from the lateral hip to the lateral knee.
Although a bursa can become inflamed from sudden, direct trauma, it is far more common for a bursa to become gradually inflamed as a result of improper training techniques or abnormal biomechanics. In these cases, the bursal inflammation is not a primary process but rather secondary to muscle imbalance around the hip girdle or other abnormalities along the kinetic chain. The purpose of a bursa is to allow for low-friction gliding of soft tissues over a bony prominence. Any imbalance or dysfunction of the hip muscles can result in abnormal ITB motion and trochanteric bursitis. Patients with trochanteric bursitis can usually localize pain to the lateral hip. The pain is sometimes felt along the path of the ITB in the lateral thigh. On examination, there is tenderness to palpation directly over the greater trochanter or immediately posterior to it. Often weakness of the gluteus medius and the hip external rotators is seen, which can be detected with manual resistance testing.43 A typical hip girdle muscle imbalance seen in the setting of trochanteric bursitis includes tensor fascia lata tightness and gluteus maximus inhibition or weakness.
The modified Thomas test is an excellent physical examination maneuver to assess for inflexibility around the hip girdle. One should always check the function of the deep hip external rotators and muscle function along the entire kinetic chain, from the core region to the ankle. The function of the hip external rotators can be tested statically and dynamically. In runners and cyclists with ITB symptoms, it is important to perform a biomechanical assessment while the patient is running or riding. Occasionally an audible snap can be heard as the ITB rubs over the greater trochanter. This is sometimes referred to as lateral snapping hip syndrome. This condition is contrasted with the so-called internal snapping hip syndrome, in which a deeper, more medial snap is appreciated by the patient.55 Internal snapping hip is thought to be due to the iliopsoas tendon rubbing over the iliopectineal eminence or the femoral head. The same kinetic chain abnormalities that can cause ITB pain at the lateral hip can also cause pain and tenderness where the ITB passes over the lateral epicondyle of the femur, or at its insertion on to Gerdy’s tubercle. Symptoms are exacerbated by repetitive activities such as running or cycling.
Regardless of the location of symptoms related to ITB dysfunction, the treatment principles remain the same. The patient should reduce or eliminate the exacerbating activities. Ice is helpful for reducing pain and inflammation, and for facilitating a rehabilitation program. The exercise prescription should be based on the patient’s relevant biomechanical deficits, which are determined by the office examination and a functional examination of the patient while she or he is participating in activities. Merely providing standardized exercise handouts or prescribing nonspecific rehabilitation protocols can result in poor patient outcomes. One common example of prescribing nonspecific exercises for an ITB problem is to prescribe ITB stretches when the primary deficit is hip abductor weakness. Another common mistake is to focus on hip abductor strengthening if the most relevant biomechanical deficit is impaired eccentric control of the hip external rotators. Because all the hip girdle muscles originate on the pelvis, the core musculature must be able to adequately stabilize the pelvis for the hip girdle muscles to perform their functions during dynamic activities.
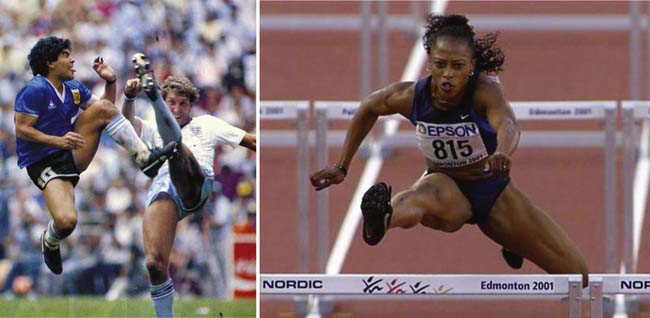
Disorders of the Hamstring Muscle Group
Strains of the thigh muscles are common in individuals participating in ballistic activities. The most commonly strained muscle group in the thigh is the hamstring group. The hamstring group includes the semimembranosus, semitendinosus, and short and long head of the biceps femoris. Hamstring strains most commonly occur with forceful eccentric contraction of the hamstring muscles, especially when the muscle is at a mechanical disadvantage near full flexion or full extension (Figure 39-9). The patient will usually be able to describe an acute overload mechanism. The hamstring pain can be reproduced by passive stretch of the muscle, by resistance testing of the muscle, and by direct palpation of the injured area. The strain can occur near the hamstring origin at the ischial tuberosity, in the belly of the muscle, or in the region of the distal musculotendinous junction. Severe hamstring strains will produce visible ecchymosis at and distal to the site of injury. A large muscle tear might produce a palpable defect. Imaging is usually not necessary to establish the diagnosis. If needed, MRI is the imaging modality of choice.78,136,149 Acute treatment consists of relative rest, ice, early gentle range of motion exercises, and gently progressive strengthening exercises as tolerated. Exercises should be progressed to higher weight and include more ballistic and sport-specific movements when tolerated. It is not uncommon for an acute hamstring strain to keep an individual from his or her usual athletic activities for 6 weeks or more.
With proximal hamstring injuries, occasionally the bone fails before the muscle or tendon fails, resulting in an ischial avulsion injury. The most common age-group for ischial avulsion fractures is 15 to 25 years of age.23,150 The most common activities that cause ischial avulsion fractures include gymnastics, hurdling, and dance. The patient can usually describe sudden onset of pain at the ischial tuberosity after a forceful movement involving hamstring contraction while the muscle was at maximum length with full hip flexion and knee extension. On physical examination, there is typically point tenderness at the ischial tuberosity, pain with passive hamstring stretch, and pain with knee flexion or hip extension against resistance. Plain films are usually adequate to visualize the avulsion (Figure 39-10). These fractures usually do not need surgery and can be treated similarly to other hamstring injuries, although the period of relative rest might be longer to allow for bone healing. If initial symptoms are severe enough to prevent comfortable ambulation, crutches can be used for a few days. Ice should be applied frequently over the first few days to decrease pain and swelling. Although surgical intervention is rarely needed, orthopedic consultation should be obtained if the avulsion fragment is displaced more than 2 cm, or if resolution of symptoms does not occur in the expected period. As pain decreases over the first 1 to 2 weeks, slowly progressive hamstring stretching and strengthening should be started. The rehabilitation program must be undertaken cautiously during the first several weeks to avoid further displacement of the avulsion. No amount of time, however, that one should wait before starting a stretching and strengthening program for the hamstring muscle group after this injury has been predetermined.14,28,144 A general guideline is that the patient should experience no discomfort or only mild discomfort with the rehabilitation program.
In skeletally mature individuals, the proximal hamstring tendon might avulse because in these individuals the weakest link is the tendon rather than the bone. The mechanism of injury is the same as described earlier. In high-demand athletes, surgical reattachment is usually indicated. Although late repair is feasible, early identification and surgical intervention usually produce the best outcomes.144
Hamstring muscle disorders can also have an insidious onset. Hamstring tendinopathy can occur at the ischial tuberosity or distally in the medial or lateral hamstring tendons. The terms tendinopathy and tendonitis, although sometimes used interchangeably, more correctly refer to chronic overload conditions and acute inflammation of tendons, respectively.79,108 In addition to pain with activities, a careful history often reveals a change in the patient’s activity level, such as a recent, rapid increase in running. The physical examination findings are similar to, but usually less dramatic than, those seen with an acute hamstring strain. In addition to the usual rehabilitation protocols such as relative rest, ice, and hamstring stretching and strengthening, one should try to identify and correct errors in training technique, running gait, cycling or jumping mechanics, and relevant biomechanical deficits. Eccentric training of the hamstring group helps the muscle to absorb more loading force, and restoring as much balance as possible to the quadriceps–hamstring force couple is also important. A local injection of steroid in the region of the ischial bursa might help facilitate the active exercise program during rehabilitation, but potential side effects need to be kept in mind.
Disorders of the Adductor Muscle Group
The adductor muscle group consists of adductor magnus, adductor longus, adductor brevis, sartorius, gracilis, and pectineus. As with other muscle or tendon injuries, strains of the hip adductor muscles usually occur with forceful activation of the muscles, especially when in a lengthened position. Adductor strains can be due to acute or repetitive overload. These injuries can occur in anyone but are particularly common in those involved in soccer, hockey, and skiing.34,147 Strains of the adductor group most commonly occur at or near their origin at the inferior pubic ramus. Intramuscular strains also occur. The adductor longus is the most commonly involved muscle.94,107 Isolated sartorius muscle strains can also occur. A sudden, forceful contraction of sartorius can result in an avulsion fracture at the muscle’s proximal attachment at the anterior superior iliac spine. This injury is treated similarly to other acute tendon strains, although a longer period of relative rest might be required before progressing the patient to stretching and strengthening exercises.
The pain can typically be reproduced by passive stretch and active resistance testing of the adductor group. Radiographs are not needed to establish a diagnosis of adductor strain but are useful when looking for bone injuries such as avulsion factures. If needed, MRI can frequently show signal change in the area of injury (Figure 39-11). Treatment includes early, gradually progressive range of motion exercises and careful strengthening exercises, with return-to-sport–specific exercises when tolerated. If the rehabilitation program is performed too aggressively in the early stages, there is a risk of further injury. Although the rehabilitation program focuses on the adductor muscle group, one needs to address the entire kinetic chain and the hip adductor–abductor force couple to decrease the chance of recurrent injury. Because the adductors arise from the pelvis, the pelvis must be stabilized with a core exercise program. The rehabilitation program should also seek to maximize flexibility, strength, motor control, and endurance of the hip flexors, hamstrings, hip abductors, and hip extensors. One should check for and correct tightness of the ITB, which if present can inhibit strengthening of the adductors.
Quadriceps Contusions and Myositis Ossificans
Contusions of the quadriceps muscle group resulting from a direct and forceful blow to the area are fairly common (Figure 39-12). The patient can usually provide a history of direct trauma to the front of the thigh. The patient typically reports pain at the site of the injury and might report stiffness and difficulty with weight-bearing. An antalgic gait is usually noted, along with tenderness, ecchymosis, and swelling in the anterior thigh. Knee flexion can be severely restricted. Extension is often preserved. Radiographs should be obtained to look for an underlying femur fracture. Ice should be applied aggressively to decrease swelling and pain. Early range of motion exercises should be started as soon as tolerated to decrease muscle stiffness, which invariably ensues. Some practitioners advocate immobilizing the knee in flexion for a few days to decrease contracture of the quadriceps muscle.61
After a severe quadriceps contusion, the intramuscular hematoma can undergo calcific transformation, resulting in myositis ossificans.11,12,29 Myositis ossificans occurs in up to 10% to 20% of all thigh contusions, and the quadriceps is the most common location for myositis ossificans to occur.73 Aspirin and standard antiinflammatory medications should be avoided in the first few days because of the theoretically increased risk of promoting additional bleeding into the injury site. If pain and stiffness persist or worsen after several weeks of appropriate care, consideration should be given to repeating radiographs and obtaining advanced imaging with a bone scan or MRI to look for calcification in the muscle. Bone scan and MRI are more sensitive in the early stages of myositis ossificans than plain films.
Conditions of the Knee Region
Patellofemoral Arthralgia
The patient with patellofemoral arthralgia can usually localize the pain to the anterior knee, or even say that the pain is “under the kneecap.” Sometimes one can elicit a history of a recent increase in activity, such as putting in a new floor without using knee pads, or a rapid increase in running distance. A mainstay of clinical diagnosis is tenderness with palpation under the medial and lateral aspects of the patella. Pain or apprehension with medial–lateral glide and tilt maneuvers of the patella also supports the diagnosis. The functional examination should look for all the biomechanical deficits listed in the previous paragraph. Single-leg and double-leg squats and lunges are particularly useful in the functional examination of a patient with patellofemoral symptoms. Conditions that share predisposing biomechanical risk factors, such as patellar tendonitis, can coexist with patellofemoral arthralgia. The differential diagnosis includes infrapatellar or suprapatellar bursitis, synovial plica, quadriceps tendonitis, patellar tendonitis, Sinding-Larsen-Johansson disease, and intraarticular pathology such as a meniscus tear.
Initial treatment protocols use the usual principles of musculoskeletal rehabilitation, including ice, acetaminophen or NSAIDs, strengthening weak or imbalanced muscle groups in the core and lower limbs, and stretching tight structures such as the ITB. Activity modification is important, such as temporarily substituting swimming for running. Many advocate the use of patellofemoral taping techniques to improve patellofemoral tracking and decrease pain. Specific patellofemoral control braces can also decrease pain and improve muscle activation in up to 50% of patients.122 Two prospective studies have shown that improving quadriceps strength strongly correlates with symptomatic improvement.67,104 Patellofemoral forces can be minimized during quadriceps strengthening by performing closed kinetic chain strengthening exercises between 0 and 30 degrees of flexion.140
Chondral and Osteochondral Lesions
Articular cartilage lines the joints and provides a smooth, low-friction surface and stress distribution during load bearing. Articular cartilage injuries occur commonly in the knee. Injuries can be limited to the articular cartilage or can involve disruption of the subchondral bone as well. The lack of vascular supply to articular cartilage creates a limited environment for repair. Injuries that do penetrate the subchondral bone, however, can initiate a vascular proliferative response that produces new but inferior “scar” fibrocartilage.19
Osteochondritis dissecans is a lesion of subchondral bone with or without involvement of the overlying articular cartilage. These lesions are classified into four categories. Grade 1 involves compression of subchondral trabeculae with preservation of the cartilage. Grade 2 involves incomplete detachment of an osteochondral fragment. Grade 3 involves complete avulsion of an osteochondral fragment without dislocation. Grade 4 involves complete avulsion of an osteochondral fragment with dislocation (loose body).16 The most common site for osteochondritis dissecans is the inferior portion of the medial femoral condyle, but they can also occur in the lateral femoral condyle or retropatellar cartilage. Symptoms include focal pain and swelling with activity that is lessened with rest. Mechanical symptoms (locking, catching, crepitus, grinding) can occur as a result of irregularities of the articular surface.
Cartilage injuries can occur with other injuries, such as meniscus tears and ligament injuries; therefore formal diagnosis usually awaits imaging studies or direct arthroscopic visualization. Treatment depends on the grading of the lesion and the severity of symptoms and can include anything from relative rest to surgery.42 Surgical techniques can be palliative (arthroscopic debridement), reparative (microfracture), or restorative (autologous chondrocyte implantation, osteochondral graft). Advanced osteoarthritis is a contraindication for articular cartilage restoration procedures. Concomitant management of associated pathology such as malalignment is essential for a successful outcome.
Meniscal Injuries
Injuries to the menisci are common. They can be the result of acute trauma or gradual degeneration. A sudden or forceful twisting motion on a planted foot is the most common mechanism of injury for acute meniscus tears. The patient typically reports a slow onset of swelling after the injury (often the day after injury), pain with weight-bearing and twisting maneuvers, and sometimes clicking within the knee. Locking of the knee suggests the presence of a bucket handle meniscus tear that has flipped up into the intercondylar notch (Figure 39-13). The hallmarks of the physical examination include medial or lateral joint line tenderness, effusion, and a positive McMurray’s test. MRI is the study of choice to look for meniscus tears. Initial treatments include ice, elevation, NSAIDs, and bracing. Additional treatments depend on healing potential and the patient’s goals. Simple tears have a greater chance of healing than complex tears. Tears in the outer portion of the meniscus, referred to as the vascularized “red zone,” have greater healing potential than tears located centrally in the avascular “white zone.” Vascular zone tears in younger individuals can be amenable to arthroscopic primary repair procedures. In older athletes, if there are no mechanical symptoms present, it is reasonable to allow 3 to 6 weeks of relative rest and rehabilitation to see whether symptoms improve. Referral for consideration of arthroscopic intervention is indicated if the patient remains limited in function, has persistent mechanical symptoms, or has recurrent episodes of pain and swelling. Patients who need to return to full activities quickly, such as elite athletes, can proceed with arthroscopy sooner. Arthroscopic treatment options include repair of the meniscus tear versus debridement of the meniscus with partial meniscectomy.
Knee Ligament Injuries
Four ligaments provide static stability to the knee. The most commonly injured knee ligaments are the medial collateral ligament (MCL) and the anterior cruciate ligament (ACL). The MCL courses from the medial femoral condyle to the proximal, medial tibia, and provides restraint against valgus force. Patients presenting with an MCL sprain might be able to describe sustaining a sudden valgus force with the foot planted. They will often be able to localize the pain to the medial side of the knee. The physical examination will be most notable for tenderness along the course of the MCL and a positive valgus stress test. If the patient is apprehensive with valgus stress testing but a firm end feel is appreciated, then the injury is most likely a grade 1 sprain with no gross tearing of the ligament (Figure 39-14). If the medial joint line opens up without apparent restraint, the injury is a grade 3 sprain, representing complete disruption of the ligament. Depending on the degree of ligament injury, medial knee swelling might be present, but an intraarticular effusion is absent in isolated MCL sprains because the MCL is extraarticular. Although plain films are usually unremarkable in an isolated MCL injury, anteroposterior and lateral radiographs are useful to rule out an associated bony injury. MRI is the imaging study of choice to evaluate the MCL but is usually obtained only if other injuries are suspected or if the patient is an elite athlete. Initial treatment most commonly consists of aggressive use of ice and elevation to decrease swelling and pain. A knee immobilizer can be used for 1 to 2 weeks to provide joint stability and allow reparative scar tissue to begin forming. Early, gentle knee flexion and extension exercises are initiated in the first 1 to 2 weeks, and gradual return to full activities as tolerated is progressed over 1 to 4 weeks, depending on the severity of the injury. Isolated MCL tears, even grade 3, rarely, if ever, require surgery.56
Tears of the ACL are the most functionally devastating because of the ACL’s crucial role in the dynamic stability of the knee, especially during activities involving side-to-side or cutting maneuvers. The ACL courses from the medial wall of the lateral femoral condyle anteromedially to the anterior spine of the tibial plateau. The ACL restrains anterior displacement of the tibia relative to the femur, and internal rotation of the tibia relative to the femur.110 ACL tears can occur as the result of contact or noncontact injuries. Although different mechanisms can place the ACL at risk, the individual is often rotated on a planted foot with the knee in flexion and the quadriceps activating strongly.26 The patient will often report hearing or feeling a “pop” followed by the development of an effusion. The patient will also describe a sense of knee instability, especially with twisting activities such as changing direction when walking. Return to sports participation can be difficult and associated with repeated episodes of instability. In the acute setting, pain might not be a prominent symptom. When significant pain is present acutely, it can suggest the presence of an associated injury such as a bone contusion or meniscus tear. On physical examination, an effusion is usually present, and the anterior drawer and Lachman’s test reveal increased anterior displacement of the tibia relative to the femur. Lachman’s test is reported to have greater sensitivity for detecting ACL insufficiency compared with the anterior drawer test.146 Plain films can show an effusion. The presence of a small capsular avulsion fracture of the lateral tibial plateau is termed a Segond fracture and is considered pathognomic of the presence of an ACL tear (Figure 39-15).26 An MRI is often obtained to confirm the clinical diagnosis and look for associated injuries, such as meniscal tears, capsular injuries, other ligament injuries, bone bruises, and popliteus injuries (Figure 39-16).
The management of acute ACL tears includes aggressive use of ice, elevation, and compression. A knee immobilizer or hinged knee brace can be used initially to provide stability. Crutches can also be used if needed. Early, gentle knee flexion and extension exercises can minimize the development of stiffness. Quadriceps inhibition is almost ubiquitous after ACL tears, and atrophy in this muscle group can be fairly dramatic even within a few weeks of injury. Straight leg raises performed in the knee immobilizer promote safe quadriceps activation and decrease the development of atrophy. The longer-term treatment of ACL tears depends primarily on the patient’s desired activity level. Young healthy individuals who participate in cutting sports should strongly consider ligament reconstruction to increase knee stability and decrease the chance of developing posttraumatic osteoarthritis from a chronically unstable knee.4,24 Sedentary individuals or individuals participating primarily in straight-ahead activities such as walking and cycling might opt for aggressive rehabilitation to maximize muscular control of the joint. It is also reasonable for patients to pursue aggressive rehabilitation and defer surgical reconstruction if they are not experiencing episodes of instability and are willing to avoid impact and aggressive cut–pivot activities. Most knee surgeons recommend waiting at least 1 to 2 weeks before reconstruction to allow time for swelling and stiffness to decrease. The use of functional knee braces in ACL-deficient patients seems to provide some benefit in moderate activities and appears to limit subluxation events, although the mechanism for this is unclear. No evidence shows that these braces prevent ACL injury.25
Injuries of the PCL are less common than injuries to the ACL. PCL deficiency generally results in less significant functional limitations compared with the ACL-deficient knee. The PCL courses posteriorly and inferiorly from the femoral intercondylar notch to the posterior tibial spine. It serves to restrain posterior displacement of the tibia relative to the femur. A common mechanism for PCL disruption is a forceful blow to the proximal, anterior leg. This can drive the tibia posterior relative to the femur. PCL disruptions have occurred in soccer goalkeepers who get kicked in the shin when sliding to make a save, in individuals who fall onto their shins, and in motor vehicle accidents when a front-seat passenger has the shin driven into the dashboard (the so-called “dashboard injury”). The clinical diagnosis of a PCL tear is primarily based on a positive posterior drawer test. Plain films are usually negative in isolated PCL injuries. MRI can be obtained to confirm the diagnosis and look for associated injuries. Acute management includes ice, elevation, pain control if needed, and early gentle range of motion exercises. If the individual is having difficulty walking, a knee immobilizer and crutches can be used for 1 to 2 weeks. Most individuals with isolated PCL injuries can return to full activities, including athletics, after functional rehabilitation.117 On rare occasions, surgical reconstruction of the PCL is undertaken if the individual continues to experience instability symptoms or functional limitations.
The lateral collateral ligament, also called the fibular collateral ligament, courses from the lateral femoral condyle to the fibular head and resists varus forces at the knee.66 The lateral collateral ligament is rarely injured in isolation but can be torn in multiligament injuries and knee dislocations.
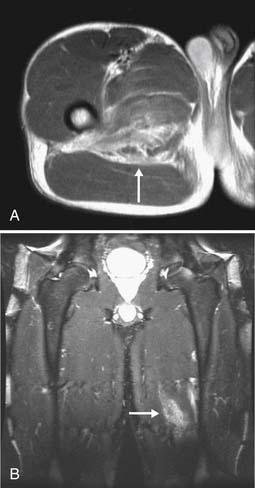
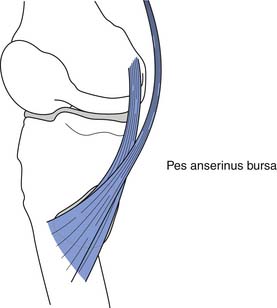
Pes Anserine Tendonitis or Bursitis
One hamstring muscle (semitendinosus) and two adductor muscles (sartorius and gracilis) course together along the medial aspect of the knee to insert on the proximal, anteromedial tibia (Figure 39-17). The anatomist who coined the name pes anserinus thought that the insertion of these three tendons looked like a goose’s foot. Acute inflammation of one or more of these three tendons near their insertion is called pes anserine tendonitis. Subacute or chronic irritation of one or more of these tendons near their tibial attachment is called pes anserine tendinosis. Inflammation of the bursa that lies just under the tendons near their insertion is termed pes anserine bursitis. Clinical differentiation between these conditions is difficult or impossible. Bursal pathology is usually secondary to dysfunction of the overlying tendons. The patient typically complains of pain in the region of the pes anserine insertion. The patient might provide a history of a sudden increase in activity level. On palpation, there is usually local tenderness at the pes anserine insertion. Common biomechanical deficits that are associated with this condition include a weak core, weak medial hamstrings, and weak hip adductors. Initial treatment includes ice and acetaminophen or NSAIDS to decrease pain and swelling. Although the rehabilitation program focuses on maximizing flexibility, strength, endurance, and motor control of the pes anserine muscles, the entire kinetic chain must be addressed. Core control should be maximized to allow for proper hamstring and hip adductor function. Anterior to posterior and medial to lateral muscle imbalances should be identified and rehabilitated. Impaired subtalar motion and abnormal tibial rotation should also be addressed. In runners and cyclists, running gait and cycling mechanics need to be observed and modified if necessary. Running shoes and inserts need to be appropriate for each individual’s biomechanical characteristics. Imaging is usually not indicated unless there is suspicion for stress fracture or intraarticular pathology, such as an injury to the meniscus. A local steroid injection can help facilitate the active exercise program at times.
Patellar Tendinopathy
A common term for patella tendinopathy is jumper’s knee. Symptoms of patella tendon overload most commonly start insidiously. When the patient is able to localize a point of maximal pain, it is usually at the inferior pole of the patella. The pain, however, can occur anywhere along the course of the tendon. Individuals at risk for patella tendon overload include those who participate in repetitive knee flexion and extension activities, such as basketball players, volleyball players, bicyclists, rowers, and mogul skiers.62 The diagnosis is usually made primarily by history. Patients might have tenderness along the course of the tendon. The examiner should look for biomechanical deficits that can lead to unequal distribution of forces along the links in the kinetic chain that are most involved with jumping. For example, the knee extensor mechanism can become overloaded during repetitive flexion and extension if more proximal muscle groups, such as the lumbar and hip extensors, are not adequately activating. Distally, the knee extensor mechanism can be placed at a biomechanical disadvantage if the individual lacks adequate ankle dorsiflexion, which is a necessary motion for squatting. Ankle dorsiflexion is also necessary for maximal activation of the calf muscles, which assist the quadriceps in jumping and eccentrically controlling the landing motion. The muscle groups involved in the jumping motion should be evaluated for their eccentric and concentric function because both types of muscle action are involved in jumping and landing. Imaging is usually not necessary to make the diagnosis. For refractory cases or when the clinical diagnosis is in question, MRI and ultrasound provide adequate visualization of the tendon (Figure 39-18).
Osgood-Schlatter Disease and Sinding-Larsen-Johansson Disease
When an adolescent presents with pain at the tibial tuberosity that is exacerbated with activities and direct contact, Osgood-Schlatter disease should be considered. The underlying cause of this relatively common condition is not clear, but repetitive overload at the patella tendon insertion can cause inflammation, irregularity, and/or partial avulsions of the secondary ossification center of the tibial tuberosity. Clinically, the diagnosis is made when there is significant pain and tenderness at the tibial tubercle. The radiographic hallmark of Osgood-Schlatter disease is irregularity and fragmentation of the tibial tuberosity (Figure 39-19). Although far less common than Osgood-Schlatter disease, similar findings can be seen at the origin of the patella tendon at the inferior pole of the patella, in which case the condition is called Sinding-Larsen-Johansson disease. For both conditions, the mainstays of treatment include ice, gently progressive quadriceps stretching, careful pain-free quadriceps strengthening, and activity modification. Activity modification is sometimes the most difficult part of the treatment regimen because the individuals who suffer from these conditions are usually active adolescents. Realistically, activity modification can mean encouraging the patient to participate in one sport per season rather than two or three. Symptoms might be intermittent or persistent until the growth plates close, at which point symptoms usually resolve spontaneously.
Quadriceps and Patella Tendon Rupture
Forceful quadriceps contraction with the foot planted can cause injury to the quadriceps muscle itself or failure of either the quadriceps or patella tendon (Figure 39-20).62 The patient can usually describe an appropriate mechanism of injury and might describe a sense of having an unstable knee. On examination, there is anterior knee swelling and a palpable defect just proximal or just distal to the patella. The patient will be unable to extend the knee. When the patient is asked to do so, the patella will not move if there is a quadriceps tendon rupture but will elevate without causing knee extension in the setting of a patella tendon rupture. A careful musculoskeletal and neurovascular examination should be performed to assess for associated injuries such as an ACL tear or femoral neuropathy. A patient with an acute quadriceps or patella tendon rupture should be placed in a knee immobilizer and made non–weight-bearing with crutches. Rupture of the quadriceps or patella tendons requires surgical repair within a few days for optimal results.
Conditions of the Leg
Tibial Stress Fractures
The “dreaded black line” is a tension-type stress fracture of the anterior cortex of the middle third of the tibia. These fractures are well known for their progression to nonunion or complete fracture. With continued activity, the risk of complete fracture is 60%.10 Even with appropriate activity modification for 9 to 12 months, nonsurgical treatment fails in 25% to 60% of cases.9 Initial treatment might consist of activity modification and pneumatic leg splints. Intramedullary fixation, however, should also be considered as an appropriate initial treatment.17
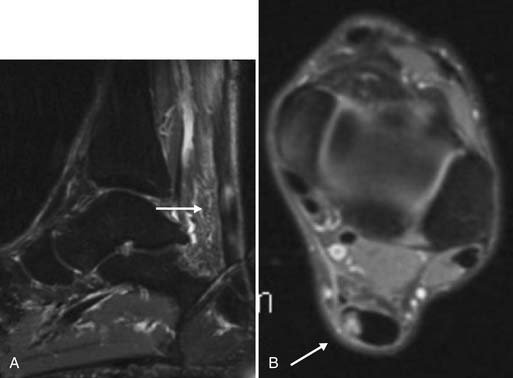
Achilles Tendinopathy and Rupture
Any of the muscles of the deep or superficial compartments of the posterior leg can become acutely or insidiously overloaded.5 As with other overload injuries, these muscles are more prone to sudden or repetitive eccentric overload. Achilles tendon overload is common and can be either chronic or acute. In the chronic setting, typical changes of tendinosis can be seen clinically by way of a swollen, nodular, tender Achilles tendon.65 Although not usually necessary for diagnosis, ultrasound and MRI show typical changes that correspond to microscopic features of breakdown in the normal collagen orientation, vacuole formation, and microscopic tearing (Figure 39-21). Treatment consists of ice, NSAIDs, activity modification, stretching, and strengthening exercises. Muscle groups along the kinetic chain that work synergistically with the ankle plantar flexors must also be tested and rehabilitated, if indicated. For example, in the running, jumping, and cycling motions, the ankle plantar flexors work synergistically with the knee and hip extensors. Errors in training technique should also be addressed, such as increasing the volume of running or jumping too rapidly, as well as technique issues such as toe running. Toe running can place excessive eccentric demands on the ankle plantar flexors. Eccentric strength training has been shown to be especially effective in the rehabilitation of chronic Achilles tendinopathy.1
A sudden, powerful eccentric force can cause an acute rupture of the Achilles tendon. Patients can almost always describe such a mechanism, usually during ballistic sporting activities such as basketball. The event is sometimes accompanied by an audible pop, with inability to continue the activity. Patients commonly relate that they feel as if they were “kicked in the calf.” Examination typically shows swelling in the region of the Achilles tendon and often the examiner can appreciate a palpable defect in the tendon. The patient typically has difficulty with plantar flexion, although some plantar flexion activity might be provided by the other posterior leg muscles. The treatment of acute Achilles tendon rupture includes surgical reconstruction followed by immobilization and then aggressive rehabilitation, versus immobilization followed by aggressive rehabilitation.116 The period of immobilization can be as long as 3 months. Which treatment to pursue depends on multiple factors, including the age, health, and activity level of the patient; the presence of a partial versus complete tear; the amount of retraction of the torn ends; and the preference of the patient and practitioner. Although good outcomes have been reported with and without surgery, the incidence of a repeat Achilles tendon rupture is lower after surgical reconstruction.8,77,106,109,152
Compartment Syndrome
The term compartment syndrome refers to a condition in which the pressure within a given muscle compartment is abnormally elevated. Two types of compartment syndrome exist: acute and chronic. Acute compartment syndrome is usually caused by significant trauma, such as a fracture or crush injury, and is a surgical emergency. Chronic exertional compartment syndrome (CECS) of the lower limb is seen most commonly in high-volume runners.120 Symptoms can mimic those of tendinopathy or stress fracture. Patients with CECS complain of recurrent leg cramping or pain with activities. Symptoms usually come on at a predictable time point in their exercise routine. Occasionally the patient can localize the cramping to a particular compartment of the leg (anterior, lateral, superficial posterior, and deep posterior). More often, however, the cramping is difficult to localize. Neurologic symptoms, such as temporary foot weakness during activities, can occur when high compartment pressures cause ischemia to the tibial or peroneal nerves. Definitive diagnosis is by intramuscular compartment pressure testing. In addition to a history and physical examination that are consistent with CECS, one or more of the following criteria must be met to formally establish the diagnosis:
Newer MRI techniques that measure increased T2 signal in a specific compartment after exercise might provide a noninvasive way of documenting selective compartment pressure increase.3,37,81,114 Treatment can be challenging. The primary nonsurgical treatment is avoiding the inciting activities. Massage therapy can sometimes be helpful. If prolonged activity modification and rehabilitation are unsuccessful, fasciotomy or fasciectomy should be considered. In carefully selected patients, surgery can be effective.141
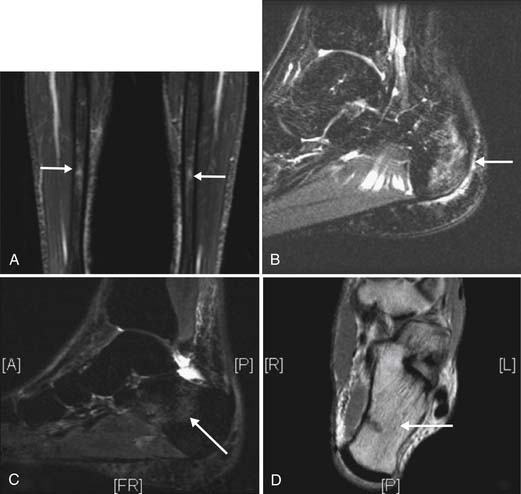
Fibularis Longus and Brevis Injuries
The correct anatomic name for the peroneus muscle has been changed to fibularis. However, for the purpose of this discussion we will refer to this muscle group in terms of its widespread usage, which is peroneus. The peroneal muscles can be injured either from a sudden, forceful contraction or from repetitive overload. Acute injuries sometimes occur at the time of a lateral ankle sprain, when the peroneal muscles will activate eccentrically to counteract the inversion moment.118,119 On physical examination, there is tenderness over the lateral leg, usually approximately 12 cm proximal to the lateral malleolus at the level of the musculotendinous junction. On MRI, a longitudinal tear of peroneus longus, peroneus brevis, or both can be seen (Figure 39-22). Although many of these injuries respond well to ankle rehabilitation, persistent cases can require surgical intervention.
Conditions of the Ankle and Foot Region
Navicular Stress Fractures
Navicular fractures have a higher likelihood of delayed union, nonunion, or avascular necrosis than other stress fractures. Evidence shows that continued weight-bearing on a tarsal navicular fracture is associated with a 74% failure rate of healing.70 Therefore early diagnosis and treatment are important. Radiographs are often normal, and an MRI or bone scan might be necessary to confirm the diagnosis. A CT scan is often the most appropriate study to optimally visualize the bone. Navicular fractures involving a cortical break at the dorsal aspect of the navicular alone have the best prognosis, typically healing by 3 months. With propagation of the fracture into the navicular body, healing time is slightly longer. Initial management of these fractures consists of non–weight-bearing with boot immobilization for 6 to 8 weeks. If symptoms persist, one should consider use of a bone stimulator or surgical fixation.57 Navicular fractures that propagate across the body and involve another cortex have a significantly higher risk of complication, and early surgical intervention should be considered.124,125
Fifth Metatarsal Stress Fractures
Stress fractures of the fifth metatarsal are prone to nonunion and refracture (Figure 39-23). Early stress fractures (bony edema only) are typically treated with non–weight-bearing immobilization for 6 weeks, followed by 6 weeks of protected weight-bearing. If healing still has not occurred, surgical fixation is appropriate. Surgery is usually considered as first-line treatment in cases where a clear fracture line is present or in elite athletes.17,111
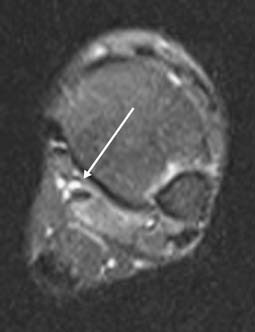
Osteochondral Lesions of the Ankle
The talus ranks third in location after the knee and elbow for osteochondral lesions. Osteochondral lesions occur in about 6.5% of all ankle sprains. A history of trauma is noted in about 80% of cases.143 Patients present with deep ankle pain that is worse with weight-bearing and improved with rest. Tenderness can sometimes be elicited with palpation in the region of the subtalar joint and with subtalar joint play maneuvers. MRI is more sensitive than plain films for visualizing the lesion and assessing soft tissue structures (Figure 39-24). Osteochondral lesions can affect the medial or lateral talus. Medial lesions usually occur after a compressive force with an inversion–flexion movement. Medial lesions are less commonly related to acute trauma, tend to be less severe, and are more likely to undergo spontaneous healing. Lateral talus osteochondral lesions often occur after forced eversion and dorsiflexion. Symptoms are more pronounced, and self-healing occurs less frequently. Osteoarthritic changes can develop earlier in these patients. Nonoperative treatment of symptomatic osteochondral lesions of the talus fails in 30% to 40% of patients. Generally, stage 1 disease is treated nonoperatively. Stage 4 is treated operatively. Stages 2 and 3 are treated conservatively on the medial side and surgically on the lateral side.143
Sprains
Ankle injuries are graded from simple distortion or partial tear in the ligament with no instability (grade 1) to partial or complete tear of the ligament with instability (grades 2 and 3, respectively). Accurate diagnosis can be difficult immediately after an injury because of the presence of pain and swelling. Grading the degree of ligament damage with the physical examination is sometimes more reliable several days after the injury. The combination of pain over the anterior talofibular ligament, hematoma discoloration, and a positive anterior drawer test has a sensitivity of 96% and specificity of 84% for diagnosing a grade 2 or 3 sprain.30 A positive squeeze test (compressing the tibia and fibula at midcalf) and external rotation test (externally rotating the dorsiflexed foot) are suggestive of a syndesmotic injury. When tenderness is present over the distal fibula, ankle joint, syndesmosis, base of the fifth metatarsal, or other bony structures, radiographs should be obtained to rule out fracture. Avulsion fractures of the base of the fifth metatarsal can occur from the pull of peroneus brevis (Figure 39-25). If nondisplaced or mildly displaced, these fractures can usually be treated nonoperatively with use of an orthopedic shoe for 1 to 2 weeks or until pain subsides. Greater displacement of the avulsion fragment might require screw or pin fixation.
Acute treatment of lateral ankle sprains includes icing and compressive wrapping of the ankle. Icing and elevation can help minimize swelling. Early mobilization and use of a brace for support can be helpful initially. Crutches are used only when pain precludes full weight-bearing. Sensorimotor control is reduced in persons with persistent instability complaints after injury. Balance and proprioceptive training improves sensorimotor control and can reduce the risk of future injury. As a patient progresses in therapy, dynamic strengthening and sport-specific functional drills should be incorporated into the exercise program.89 Functional tests to determine readiness to return to activity include “shuttle runs” and single-leg hopping. In returning to sport, taping or bracing has been shown in some studies to be helpful in reducing the risk of recurrent ankle sprains. These effects are probably due to mechanical restriction and neuromuscular and sensory mechanisms. Bracing is often favored over taping because it better restricts ankle motion without affecting performance; it retains its restrictive property longer; and it is more cost-effective in the long term.13,22,40,98 Medial ankle sprains and syndesmotic injuries require longer healing times than lateral sprains. A walking boot can be used for the first 2 to 4 weeks with these injuries. About one third of patients have mild to moderate residual pain with activity. In cases of a complete syndesmotic injury, screw fixation is indicated. Most other ankle sprains heal without complication.
With a functional rehabilitation program, the patient can return to full activity within a few days to weeks, depending on the severity of the sprain. Residual symptoms are more likely if the rehabilitation is incomplete. It has been reported that up to 40% of ankle sprains lead to persistent problems with pain and instability.49 Occult injuries must be suspected in these individuals. The most commonly overlooked injuries include fractures, osteochondral lesions, injuries to the subtalar joint or syndesmosis, peroneal tendinopathy or rupture, proprioceptive deficit, and impingement syndrome. Pain is the most common cause of subjective or “functional” instability. In these patients, physiologic range is not exceeded on examination. A few of the common causes include peroneal muscle weakness, proprioceptive deficit, and subtalar instability. If pain is not present between episodes of instability, there might be true mechanical instability. These patients have ankle mobility beyond the physiologic range of motion, with abnormal laxity on examination. Studies have shown that balance exercises and peroneal strengthening can restore functional stability to even the mechanically unstable ankle. Surgery can be indicated after failure of an extended period of appropriate aggressive ankle strength and stability treatment in patients with symptomatic mechanical instability.
Flexor Hallucis Longus Overload
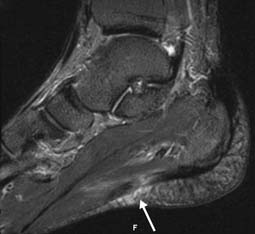
Overload of the flexor hallucis longus tendon is seen in dancers, gymnasts, and other active individuals who perform repetitive and forceful toe flexion.123 The patient can present with pain anywhere along the course of the flexor hallucis longus muscle–tendon unit. Symptoms are reproduced with flexion of the great toe against resistance and direct palpation of the tendon. Passive stretch of the muscle–tendon does not reproduce symptoms as reliably as with some other injuries, such as hamstring strains. Imaging studies are not initially indicated, but when necessary, MRI is the study of choice (Figure 39-26). As with other muscle and tendon overload conditions, treatment consists of ice, acetaminophen or NSAIDs, activity modification, and strengthening exercises. Local injection of anesthetic and corticosteroid around the tendon can decrease pain and inflammation, and facilitate progress with the exercise program.
Injury to the Plantar Foot Muscles and Plantar Fascia; Plantar Fasciitis
Four plantar foot muscles take their origin from the volar calcaneus: adductor hallucis, quadratus plantae, flexor digitorum brevis, and abductor digiti minimi quinti. Overload of these muscles can result in an enthesopathy at the calcaneus, causing volar heel pain. The same process can cause inflammation and pain in the plantar fascia. This condition is referred to as plantar fasciitis. Patients with plantar fasciitis present with volar heel pain that is often, but not always, worse with their first few steps in the morning. Tenderness to palpation is present at the volar aspect of the heel, usually slightly medial to midline. Imaging studies are usually not indicated unless there is a history of acute trauma or symptoms become recalcitrant. The presence or absence of a calcaneal traction spur correlates poorly with symptoms of plantar fasciitis.72
As with other musculotendinous injuries, a similar biomechanical approach should be taken when treating plantar fasciitis. The rehabilitation plan should focus on restoring range of motion, strength, endurance, and motor control of the heel cord and foot intrinsic muscles. If pain with the first few steps in the morning is a prominent symptom, then a resting night splint can be helpful in preventing overnight tightening of the heel cord and plantar structures (Figure 39-27). A kinetic chain evaluation might reveal predisposing biomechanical deficits. If the patient is a toe runner, then the foot intrinsic muscles can become eccentrically overloaded. Similarly, a tight heel cord or a tight hamstring can prevent proper heel strike and result in excessive forces being placed on the plantar foot muscles. If tibialis posterior and tibialis anterior are not doing their assigned job of supporting the medial longitudinal arch, the plantar foot muscles can become overloaded as they try to compensate for their more proximal agonists. More proximally still, the dynamic function of the hip external rotators should be assessed. The hip external rotators eccentrically control femoral internal rotation during the weight-bearing phase of running and have an indirect effect on tibial rotation and subtalar pronation. Local injection of corticosteroid can assist in decreasing local inflammation and pain, but the patient must be cautioned that corticosteroid can increase the risk of rupture of the plantar fascia(Figure 39-28).
Morton’s Interdigital Neuroma, Metatarsalgia, and Sesamoiditis
Although distinct clinical entities, these conditions are reviewed jointly because they have similar presentations. Morton’s neuroma is caused by irritation of one of the interdigital nerves of the foot as it passes below the transverse ligament of the metatarsal heads. The most common location for an interdigital neuroma is between the third and fourth metatarsal heads, but it can also occur between the other metatarsal heads.41 Symptoms usually start insidiously. The patient typically presents with pain in the region of the metatarsal heads. There can be referral of pain or paresthesias into the two toes innervated by the interdigital nerve in question. Patients sometimes describe a sensation of having a pebble in their shoe or a wrinkle in their sock. Pain is exacerbated with forefoot weight-bearing, narrow toe boxes, and high heels, all of which can load the region of the metatarsal heads and interdigital nerves. If there are no neurologic symptoms referred to the toes, the challenge of the physical examination is to distinguish between pain coming from between two metatarsal heads and pain coming from the metatarsal heads themselves, which would be more consistent with metatarsalgia. Occasionally the examiner appreciates a click when palpating a large or firm neuroma, especially when palpation is combined with squeezing the metatarsal heads together from the medial and lateral sides. Metatarsalgia, as its name implies, is pain coming from the metatarsal heads. Jumping, toe running, and high heels can all cause overload of the metatarsal heads, just as they can cause entrapment or irritation of the interdigital nerve beneath the transverse metatarsal ligament. The second metatarsal head is the most commonly involved.
When the pain is in the region of the first metatarsal head, the differential diagnosis includes injury to the sesamoid bones in the flexor hallucis tendon, such as stress response or stress fracture. Pain coming from an injured sesamoid bone is sometimes referred to as sesamoiditis. Distinguishing between metatarsalgia, sesamoid stress response, and sesamoid fracture can be clinically challenging. A bipartite sesamoid seen on plain films can be a normal variant, and advanced imaging with MRI or bone scan might be required to diagnose a fracture of the sesamoid.
1. Alfredson H., Pietila T., Jonsson P., et al. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26(3):360-366.
2. Altman R.D., Moskowitz R. Intra-articular sodium hyaluronate (Hyalgan) in the treatment of patients with osteoarthritis of the knee: a randomized clinical trial: Hyalgan Study Group. J Rheum. 1998;25:2203-2212. (Correction in: J Rheum 1999; 26:1216)
3. Amendola A., Rorabeck C.H., Vellett D., et al. The use of magnetic resonance imaging in exertional compartment syndromes. Am J Sports Med. 1990;18(1):29-34.
4. Andersson C., Odensten M., et al. Knee function after surgical or nonsurgical treatment of the acute rupture of the anterior cruciate ligament: a randomized study with a long-term follow-up period. Orthopaedics. 1991;264:255-263.
5. Andrews J.R. Overuse syndromes of the lower extremity. Clin Sports Med. 1983;2:137.
6. Arendt E.A., Griffiths H.J. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sport Med. 1997;16:291-306.
7. Ashby E.C. Chronic obscure groin pain is commonly caused by enthesopathy: ‘tennis elbow’ of the groin. Br J Surg. 1994;81:1632-1634.
8. Bahndari M., Guyatt G.H., Siddiqui F., et al. Treatment of acute Achilles tendon ruptures a systematic overview and metaanalysis. Clin Orthop. 2002;400:190-200.
9. Batt M.E., Kemp S., Kerslake R. Delayed union stress fractures of the anterior tibia: conservative management. Br J Sports Med. 2001;35:74-77.
10. Beals R.K., Cook R.D. Stress fractures of the anterior tibial diaphysis. Orthopedics. 1991;14:869-875.
11. Beiner J.M., Jokl P. Muscle contusion injuries: current treatment options. J Am Acad Orthop Surg. 2001;9(4):227-237.
12. Beiner J.M., Jokl P. Muscle contusion injury and myositis ossificans traumatica. Clin Orthop. 2002;403S:S110-S119.
13. Bennell K., McCrory P. The role of ankle support in the prevention of ankle injury. Sport Health. 1992;10:13-16.
14. Bennell K.L., Malcolm S.A., Thomas S.A., et al. Risk factors for stress fractures in female track-and-field athletes: a retrospective analysis. Clin J Sports Med. 1995;5:229-235.
15. Bennell K.L., Malcolm S.A., Thomas S.A., et al. Risk factors for stress fractures in track and field athletes: a 12-month prospective study. Am J Sports Med. 1996;24:810-818.
16. Berndt A.L., Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41:988-1020.
17. Boden B.P., Osbahr D.C. High-risk stress fractures: evaluation and treatment. J Am Acad Orthop Surg. 2000;8:344-353.
18. Brukner P., Khan K. Clinical sports medicine. Sydney: McGraw-Hill; 1993.
19. Buckwalter J.A. Articular cartilage injuries. Clin Orthop. 2002;402:21-37.
20. Byrd J.W., Jones K.S. Hip arthroscopy in athletes. Clin Sports Med. 2001;20(4):749-761.
21. Byrd J.W., Jones K.S. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16(6):578-587.
22. Callaghan M.J. Role of ankle taping and bracing in the athlete. Br J Sports Med. 1997;31:102-108.
23. Canale S.T., Beaty J.H. Pelvic and hip fractures. In Rockwood C.A.Jr., Wilkins K.E., Beaty J.H., editors: Fractures in children, ed 4, Philadelphia: JB Lippincott, 1996.
24. Casteleyn P., Handeberg F. Non-operative treatment of anterior cruciate ligament injuries in the general population. J Bone Joint Surg. 1996;78(3):446-451.
25. Cawley P.W., France E., Paulos L.E. The current state of functional knee bracing research: a review of the literature. Am J Sports Med. 1991;19:226-233.
26. Clancy W., Ray J. Acute tears of the anterior cruciate ligament. J Bone Joint Surg Am. 1988;70:1843-1848.
27. Cowan D.N., Jones B.H., Frykman P.N., et al. Lower limb morphology and risk of overuse injury among male infantry trainees. Med Sci Sports Exerc. 1996;28:945-952.
28. Croisier J., Forthomme B., Namurois M.H., et al. Hamstring muscle strain recurrence and strength performance disorders. Am J Sports Med. 2002;30(2):199-203.
29. Diaz J.A., Fischer D.A., Rettig A.C., et al. Severe quadriceps muscle contusions in athletes: a report of three cases. Am J Sports Med. 2003;31:289-293.
30. Dijk van C.N., Lin L.S.L., Bossuyt P.M.M., et al. Diagnosis of sprained ankles. J Bone Joint Surg. 1997;79:1039-1040.
31. Dragoo J., Korotkova T., Kanwar R., et al. The effect of local anesthetics administered via pain pump on chondrocyte viability. Am J Sports Med. 36, 2008. 1484–88
32. Egol K.A., Koval K.J., Kummer F., et al. Stress fractures of the femoral neck. Clin Orthop. 1998;348:72-78.
33. Ekstrand J., Gillquist J. The frequencies of muscle tightness and injuries in soccer players. Am J Sports Med. 1982;10:75-78.
34. Emery C.A., Meeuwisse W.H. Risk factors for groin injuries in hockey. Med Sci Sports Exerc. 2000;33(9):1423-1433.
35. Emery C.A., Meeuwisse W.H., Powell J.W. Groin and abdominal strain injuries in the National Hockey League. Clin J Sports Med. 1999;9(3):151-156.
36. Epstein H.C. Traumatic dislocations of the hip. Clin Orthop. 1973;92:116.
37. Eskelin M.K., Lotjonen J.M., Mantysaari M.J. Chronic exertional compartment syndrome: MR imaging at 0.1 T compared with tissue pressure measurement. Radiology. 1998;206(2):333-337.
38. Eyestone E.D., Fellingham F., George J., et al. Effect of water running and cycling on maximum oxygen consumption and 2-mile run performance. Am J Sports Med. 1993;21:41-44.
39. Farjo L.A., Glick J.M., Sampson T.G. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15(2):132-137.
40. Firer P. Effectiveness of taping for the prevention of ankle ligament sprains. Br J Sports Med. 1990;24:47-50.
41. Fitzgibbons T., Keown B., Sampson C., et al. Foot problems in athletes. In: Mellion M., editor. Office sports medicine. ed 2. Philadelphia: Hanley and Belfus; 1996:318-336.
42. Flynn J.M., Kocher M.S., Ganley T.J. Osteochondritis dissecans of the knee. J Pediatr Orthop. 2004;22(4):434-443.
43. Frederickson M., Cookingham C.L., Chaudhari A.M., et al. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000;10(3):169-175.
44. Fricker P.A. Management of groin pain in athletes. Br J Sports Med. 1997;31(2):97-101.
45. Fricker P.A., Taunton J.E., Ammann W. Osteitis pubis in athletes: infection, inflammation or injury? Sports Med. 1991;12(4):266-279.
46. Frusztajer N.T., Dhuper S., Warren M.P., et al. Nutrition and the incidence of stress fractures in ballet dancers. Am J Clin Nutr. 1990;51:779-783.
47. Ganz R., Parvizi J., Beck M., et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:1-9.
48. Garrick J., Webb D.R. Pelvis, hip, thigh injuries. In: Sports injuries: diagnosis and management. Philadelphia: Saunders; 1990.
49. Gerber J.P., Williams G.N., Scoville C.R., et al. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653-660.
50. Giladi M., Milgrom C., Simkin A., et al. Stress fractures: identifiable risk factors. Am J Sports Med. 1991;19:647-652.
51. Giladi M., Milgrom C., Stein M., et al. External rotation of the hip. A predictor of risk for stress fractures. Clin Orthop Relat Res. 1987;216:131-134.
52. Gillespie W.J., Grant I. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2000;2:CD000450.
53. Gilmore J. Groin pain in the soccer athlete: fact, fiction and treatment. Clin Sports Med. 1998;17(4):787-793.
54. Greaney R.B., Gerber R.H., Laughlin R.L., et al. Distribution and natural history of stress fractures in US marine recruits. Radiology. 1983;146:339-346.
55. Gruen G.S., Scioscia T.N., Lowenstein J.E. The surgical treatment of internal snapping hip. Am J Sports Med. 2002;30(4):607-613.
56. Haimes J., Wroble R., Grood E., et al. The role of the medial structures in the intact and ACL-deficient knee. Am J Sports Med. 1994;22(4):401-410.
57. Harmon K.G. Lower extremity stress fractures. Clin J Sports Med. 2003;13(6):358-364.
58. Hertler L., Provost-Craig M., Sestili D. Water running and the maintenance of maximum oxygen consumption and leg strength in runners [abstract]. Med Sci Sports Exerc. 1992;24:S23.
59. Hoffman J.R., Chapnik L., Shamis A., et al. The effect of leg strength on the incidence of lower extremity overuse injuries during military training. Mil Med. 1999;164:153-156.
60. Hughes L.Y. Biomechanical analysis of the foot and ankle for predisposition to developing stress fractures. J Orthop Sports Phys Ther. 1985;7:96-101.
61. Jackson D.W., Feagin J. Quadriceps contusions in young athletes: relation of severity of injury to treatment and prognosis. J Bone Joint Surg Am. 1973;55:95-105.
62. Jaivin J.S., Fox J.M. Thigh injuries. In: Nickolas J.A., Hershman E.B., editors. The lower extremity. St. Louis: Mosby, 1995.
63. Jones A.C., Pattrick M., Doherty S., et al. Intra-articular hyaluronic acid compared to intra-articular triamcinolone hexacetonide in inflammatory knee osteoarthritis. Osteoarthr Cartil. 1995;3:269-273.
64. Jonnavithula S., Warren M.P., Fox R.P., et al. Bone density is compromised in amenorrheic women despite return of menses: a 2-year study. Obstet Gynecol. 1993;81:669-674.
65. Kader D., Saxena A., Movin T., et al. Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med. 2002;36:239-249.
66. Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17(1):83-88.
67. Kannus P., Nittymaki S. Which factors predict outcome in the nonoperative treatment of patellofemoral pain syndrome? A prospective follow-up study. Med Sci Sports Exerc. 1994;26:289.
68. Karlsson J., Sward L., Kalebo P., et al. Chronic groin injuries in athletes: recommendations for treatment and rehabilitation. Sports Med. 1994;17(2):141-148.
69. Kelly B.T., Williams R.J., Phillippon M.J. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020-1037.
70. Khan K.M., Fuller P.J., Bruckner P.D., et al. Outcome of conservative and surgical management of navicular stress fracture in athletes: eighty-six cases proven with computerized tomography. Am J Sports Med. 1992;20:657-666.
71. Kibler W.B., Chandler T.J., Uhl T.L. A musculoskeletal approach to the preparticipation physical examination preventing injury and improving performance. Am J Sports Med. 1989;17:525.
72. Kibler W.B., Goldberg C., Chandler T.J. Functional biomechanical deficits in running athletes with plantar fasciitis. Am J Sports Med. 1991;19:66-71.
73. King J.B. Post-traumatic ectopic calcification in the muscles of athletes: a review. Br J Sports Med. 1998;32(2):287-290.
74. Kirwan J.R., Rankin E. Intra-articular therapy in osteoarthritis. Baillières Clin Rheumatol. 1997;11:769-794.
75. Kiuru M.J., Pihlajamaki H.K., Hietanen H.J., et al. MR imaging, bone scintigraphy, and radiography in bone stress injuries of the pelvis and the lower extremity. Acta Radiol. 2002;43:207-212.
76. Knapp T.P., Garrett W.E. Stress fractures: general concepts. Clin Sports Med. 1997;16:339-355.
77. Kocher M.S., Bishop J., Marshall R., et al. Operative versus nonoperative management of acute Achilles tendon rupture. Am J Sports Med. 2002;30(6):783-790.
78. Koulouris G., Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582-589.
79. Kraushaar B.S., Nirschl R.P. Tendinosis of the elbow. Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81:259-278.
80. Lacroiz U.J. A complete approach to groin pain. Phys Sports Med. 2000;28(1):66-86.
81. Lauder T.D., Stuart M.J., Amrami K.K., et al. Exertional compartment syndrome and the role of magnetic resonance imaging. Am J Phys Med Rehabil. 2002;81(4):315-319.
82. Leeb B.F., Schweitzer H., Montag K., et al. A meta-analysis of chondroitin sulfate in the treatment of osteoarthritis. Arthritis Rheum. 1998;41(suppl):S198.
83. Lequesne M.G., Dang N., Lane N.E. Sport practice and osteoarthritis of the limbs. Osteoarthr Cartil. 1997;5(2):75-86.
84. Lloyd-Smith R., Clement D.B., Mckenzie D.C., et al. A survey of overuse and traumatic hip and pelvis injuries in athletes. Phys Sports Med. 1995;13:131-141.
85. MacEwen G.D., Bunnell W.P., Ramsey P.L. The hip. In: Lovell W.W., Winter R.B., editors. Pediatric orthopaedics. Philadelphia: Lippincott, 1986.
86. Marshall K.W., Manolopoulos V., Mancer K., et al. Amelioration of disease severity by intraarticular hylan therapy in bilateral canine osteoarthritis. J Orthop Res. 2000;18(3):416-425.
87. Martens M.A., Hansen L., Mulier J.C. Adductor tendinitis and musculus rectus abdominis tendopathy. Am J Sports Med. 1987;15:353-356.
88. Martin J.A., Buckwalter J.A. Articular cartilage aging and degeneration. Sports Med Arthrosc Rev. 1996;4:263-275.
89. Mascaro T.B., Swanson L.E. Rehabilitation of the foot and ankle. Orthop Clin North Am. 1994;25:147-160.
90. Mason J.B. Acetabular labral tears in the athlete. Clin Sports Med. 2001;20(4):779-790.
91. Matheson G.O., Clement D.B., McKenzie D.C., et al. Stress fractures in athletes: a study of 320 cases. Am J Sports Med. 1987;15:46-58.
92. Matsumoto K., Sumi H., Sumi Y., et al. An analysis of hip dislocations among snowboarders and skiers: a 10-year prospective study from 1992 to 2002. J Trauma. 2003;55:946-948.
93. McAlindon T.E., LaValley M.P., Gulin J.P., et al. Glucosamine and chondroitin sulfate for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283(11):1469-1475.
94. Merrifield H.H., Cowan R.F.J. Groin strain injuries in ice hockey. J Sports Med. 1973;1(2):41-42.
95. Meyers W.C., Foley D.P., Garrett W.E., et al. Management of severe lower abdominal or inguinal pain in the high-performance athletes. Am J Sports Med. 2000;28(1):2-8.
96. Milgrom C., Finestone A., Shlamkovitch N., et al. Prevention of overuse injuries of the foot by improved shoe shock attenuation: a randomized, prospective study. Clin Orthop. 1992;281:189-192.
97. Milgrom C., Giladi M., Kashtan H., et al. A prospective study of the effect of a shock-absorbing orthotic device on the incidence of stress fractures in military recruits. Foot Ankle. 1985;6:101-104.
98. Miller E.A., Hergenroeder A.C. Prophylactic ankle bracing. Pediatr Clin North Am. 1990;37:1175-1185.
99. Miller M.L. Avulsion fractures of the anterior superior iliac spine in high school track athletic training. Athl Train. 1982;17:57.
100. Miller M.L. Avulsion fractures of the pelvis. Am J Sports Med. 1985;13:349-358.
101. Mishra D.K., Friden J., Schmitz M.C., et al. Antiinflammatory medication after muscle injury: a treatment resulting in short-term improvement but subsequent loss of muscle function. J Bone Joint Surg Am. 1995;77:1510-1519.
102. Moorman C.T., Warren R.F., Hershman E.B., et al. Traumatic posterior hip subluxation in American football. J Bone Joint Surg. 2003;85A:1190-1196.
103. Myburgh K.H., Bachrach L.K., Lewis B., et al. Low bone mineral density at axial and appendicular sites in amenorrheic athletes. Med Sci Sports Exerc. 1993;25:1197-1202.
104. Natri A., Kannus P., Jarvinen M. Which factors predict the long term outcome in chronic patellofemoral pain syndrome? A 7-yr prospective follow-up study. Med Sci Sports Exerc. 1998;30:1572.
105. Nattiv A., Puffer J.C., Green G.A. Lifestyles and health risks of collegiate athletes: a multi-center study. Clin J Sport Med. 1997;7:262-272.
106. Nelson G., Martens M., Burssens A. Surgical treatment of chronic Achilles tendonitis. Am J Sports Med. 1989;17:754.
107. Nicholas S.J., Tyler T.F. Adductor muscle strains in sport. Sports Med. 2002;32(5):339-344.
108. Nirschl R.P. Elbow tendinosis/tennis elbow. Clin Sports Med. 1992;11:851-870.
109. Nistor L. Surgical and non-surgical treatment of Achilles tendon ruptures. J Bone Joint Surg Am. 1981;63:394.
110. Noyes F., Butler D., Grood E. Biomechanical analysis of human ligament grafts used in knee ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66:344-352.
111. Nunley J.A. Fractures of the base of the fifth metatarsal. Orthop Clin North Am. 2001;32:171-180.
112. Orchard J.W., Fricker P.A., Abud A.T., et al. Biomechanics of iliotibial band friction syndrome in runners. Am J Sports Med. 1996;24(3):375-379.
113. O’Reilly S.C., Muir K.R., Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomized controlled trial. Ann Rheum Dis. 1999;58:15-19.
114. Ota Y., Senda M., Hashizume H., et al. Chronic compartment syndrome of the lower leg: a new diagnostic method using near-infrared spectroscopy and a new technique of endoscopic fasciotomy. Arthroscopy. 1999;15(4):439-443.
115. Owen D.S., Weiss J.J., Wilke W.S. When to aspirate and inject joints. Patient Care. 1990;24(14):128-145.
116. Paavola M., Kannus P., Jarvinen T., et al. Achilles tendinopathy. J Bone Joint Surg Am. 2002;84(11):2062-2076.
117. Parolie J.M., Bergfeld J.A. Long-term results of non-operative treatment of isolated PCL injuries in the athlete. Am J Sports Med. 1986;14:35-38.
118. Patterson JO: Ankle injuries. In Lillegard WA, Rucker KS (editors): Handbook of sports medicine, Boston, Andover, 1993.
119. Patterson M.J., Cox W.K. Peroneus longus tendon rupture as a cause of chronic lateral ankle pain. Clin Orthop Relat Res. 1999;365:163-166.
120. Pedowitz R.A., Hargens A.R., Murbarak S.J., et al. Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. 1990;18:35.
121. Picard C.L. The level of competition as a factor for the development of eating disorders in female collegiate athletes. J Youth Adolesc. 1999;28:583-594.
122. Powers C.M. The effects of patellar bracing on clinical changes and gait characteristics in subjects with patellofemoral pain [abstract]. Phys Ther. 1998;30:S48.
123. Quirk R. Common foot and ankle injuries in dance. Orthop Clin North Am. 1994;25:123-133.
124. Quirk R. Stress fractures of the navicular. Foot Ankle Int. 1998;19:494-496.
125. Reginster J.-Y., Deroisy R., Paul I., et al. Glucosamine sulfate significantly reduces progression of knee osteoarthritis over 3 years: a large randomized, placebo-controlled, double-blind, prospective trial [abstract]. Arthritis Rheum. 1999;42(suppl 9):S400.
126. Reginster J.Y., Deroisy R., Rovati L.C., et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomized, placebo-controlled clinical trial. Lancet. 2001;357(9252):251-256.
127. Reid D.C. Problems of the hip, pelvis, and sacroiliac joint. In: Sports injury assessment and rehabilitation. New York: Churchill Livingstone; 1992.
128. Saxena A., Fullem B., Hannaford D. Results of treatment of 22 navicular stress fractures and a new proposed radiographic classification system. J Foot Ankle Surg. 2000;39:96-103.
129. Scott S.H., Winter D.A. Internal forces at chronic running injury sites. Med Sci Sports Exerc. 1990;22:357-369.
130. Scully T.J., Besterman F. Stress fracture: a preventable training injury. Mil Med. 1982;147:285-287.
131. Shaffer R.A., Brodine S.K., Almeida S.A., et al. Use of simple measures of physical activity to predict stress fractures in young men undergoing a rigorous physical training program. Am J Epidemiol. 1999;149:236-242.
132. Shen W., Prisk V., Li Y., et al. Inhibited skeletal muscle healing in cyclooxygenase-2 gene-deficient mice: the role of PGE2 and PGF2. J Appl Physiol. 2006;101:1215-1221.
133. Shin A.Y., Gillingham B.L. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293-302.
134. Simkin A., Leichter I., Giladi M., et al. Combined effect of foot arch structure and an orthotic device on stress fractures. Foot Ankle. 1989;10:25-29.
135. Simonet W.T., Saylor H.L.III, Sim L. Abdominal wall muscle tears in hockey players. Int J Sports Med. 1995;20:31-37.
136. Slavotinek J.P., Verrall G.M., Fon G.T. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol. 2002;179:1621-1628.
137. Spector T., Harris P.A., Hart D.J. Risk of osteoarthritis associated with long-term weight bearing sports. Arthritis Rheum. 1996;39:995-998.
138. Spitz D.J., Newberg A.H. Imaging of stress fractures in the athlete. Radiol Clin North Am. 2002;40:313-331.
139. Stefanich R.J. Intra-articular corticosteroids in treatment of osteoarthritis. Orthop Rev. 1986;19:65-71.
140. Steinkamp L.A., Dillingham M.F., Markel M.D. Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med. 1993;21:438-444.
141. Styf J.R., Korner L.M. Chronic anterior-compartment syndrome of the leg: results of treatment by fasciotomy. J Bone Joint Surg Am. 1986;68:1338.
142. Taimela S., Kujalu U., Osterman K. Intrinsic risk factors and athletic injuries. Sports Med. 1990;9:205.
143. Tol J.L., Struijis P.A., Bossuyt P.M., et al. Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle. 2000;21:11-126.
144. Tornese D., Bandi M., Melegati G., et al. Principles of hamstring strain rehabilitation. J Sports Traumatol. 2000;22(2):70-85.
145. Towheed T.E. Glucosamine sulfate in osteoarthritis: a systematic review. Arthritis Rheum. 1998;41(suppl):S198.
146. Tria A.J. Ligaments of the Knee. New York: Churchill Livingstone; 1995.
147. Tyler T.F., Nicholas S.J., Campbell R.J., et al. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128.
148. Vad V., Hong H., Zazzali M., et al. Exercise recommendations in athletes with early osteoarthritis of the knee. Sports Med. 2002;11:729-773.
149. Verrall G.M., Slavotinek J.P., Barnes P.G., et al. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury: comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain. Am J Sports Med. 2003;31:969-973.
150. Waters P.M., Millis M.B. Hip and pelvic injuries in the young athlete. Clin Sports Med. 1988;7(3):513-526.
151. Watterson J.R., Esdaile J.M. Therapeutic mechanisms and clinical potential in osteoarthritis of the knee. J Am Acad Orthop Surg. 2000;8(5):277-284.
152. Weber M., Niemann M., Lanz R., et al. Nonoperative treatment of acute rupture of the Achilles tendon: results of a new protocol and comparison with operative treatment. Am J Sports Med. 2003;31:685-691.
153. Wilber R.L., Moffatt R.J., Scott B.E., et al. Influence of water-run training on running performance [abstract]. Med Sci Sports Exerc. 1994;26:S4.
154. Yoshikawa T., Mori S., Santiesteban A.J., et al. The effects of muscle fatigue on bone strain. J Exp Biol. 1994;188:17-33.
155. Zanker C.L., Swaine I.L. Relation between bone turnover, estradiol, and energy balance in women distance runners. Br J Sports Med. 1998;32:167-171.