33 Musculocutaneous Nerve Block
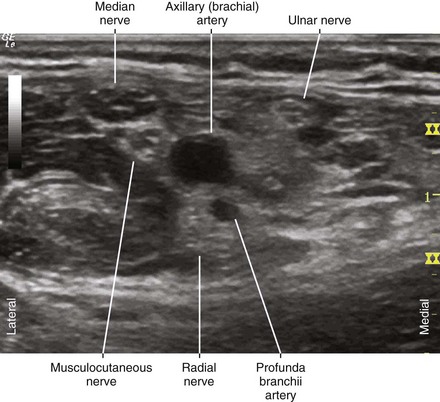
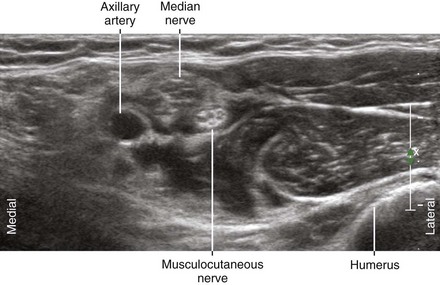
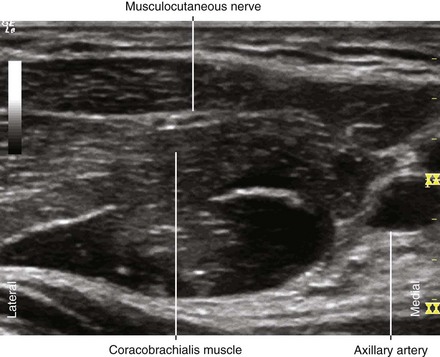
The musculocutaneous nerve usually passes through the coracobrachialis muscle. The musculocutaneous nerve exits the coracobrachialis between its two parts and the short head of the biceps, forming a triangle with these three muscular components.1 The musculocutaneous nerve lies between the biceps and the brachialis more distally.
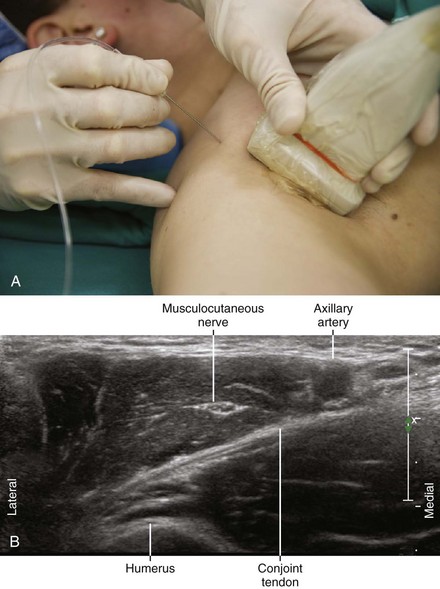
Suggested Technique
Ultrasound imaging of the musculocutaneous nerve in the axilla can be used to facilitate regional block.2 This directly addresses one of the primary weaknesses of traditional axillary block.
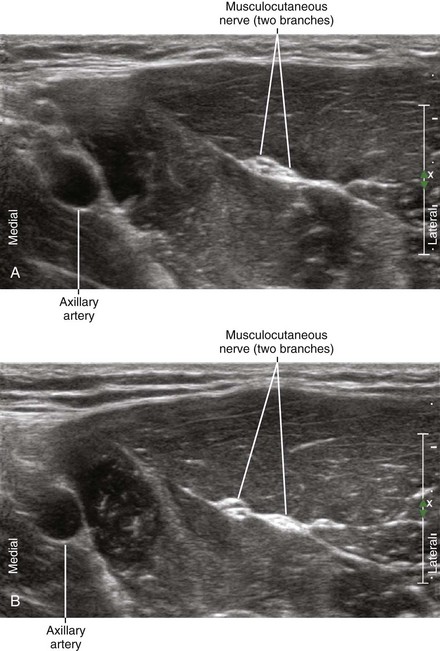
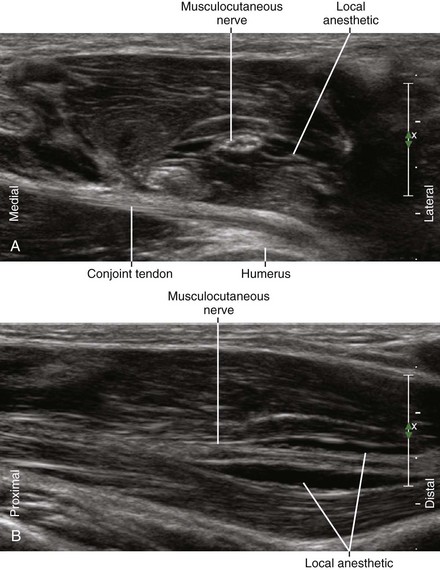
The lateral course of the nerve and its changes in shape as it passes through the coracobrachialis muscle are characteristic features that allow ultrasound identification of the nerve.3 The nerve typically has a flat shape within the coracobrachialis muscle; therefore, this is a desirable location for regional block. The relatively high surface area–to–volume ratio may improve onset kinetics of the block.
The lateral cutaneous branch of the musculocutaneous nerve can be more selectively blocked distal to the nerve exit from the coracobrachialis muscle. The point of exit is usually easy to identify because the nerve has a triangular shape in that location. Blockade of the more proximal motor fibers of the musculocutaneous nerve is unlikely with this approach. However, the nerve to the biceps brachii continues for about 4 cm after the exit from the coracobrachialis before branching off.4
The estimated incidence of pass-over musculocutaneous nerve (musculocutaneous nerve path over the coracobrachialis muscle rather than through it) ranges from 8% to 30%.5 This usually does not present a problem because the nerve can be directly imaged.
Fusion of the median nerve and musculocutaneous nerve is another common anomaly (a low-lying lateral cord). In these fusion products, the median contribution is typically larger and more superficial than the musculocutaneous contribution.6 Small muscular branches can sometimes be identified that course medial to lateral from the musculocutaneous contribution.
Key Points
| Musculocutaneous Nerve Block | The Essentials |
|---|---|
| Anatomy | The MCN usually has a lateral course through the CBr. |
| The MCN has a flat shape within the CBr. | |
| The MCN becomes triangular in shape where it exits the CBr. | |
| The MCN is about 2.5 mm in diameter. | |
| Image orientation | The MCN lies lateral to the axillary artery. |
| Positioning | Arm supinated and abducted |
| Operator | Standing on lateral (cephalad) side of armboard (for laptop system) |
| At the side of the patient (for system with movable display) | |
| Display | Across the armboard (for laptop system) |
| Across the table (for system with movable display) | |
| Transducer | High-frequency linear, 38- to 50-mm footprint |
| Initial depth setting | 25 mm |
| Needle | 21 to 22 gauge, 50 to 70 mm in length |
| Anatomic location | Begin by scanning in the proximal axilla. |
| Slide distally to observe MCN moving away from AA. | |
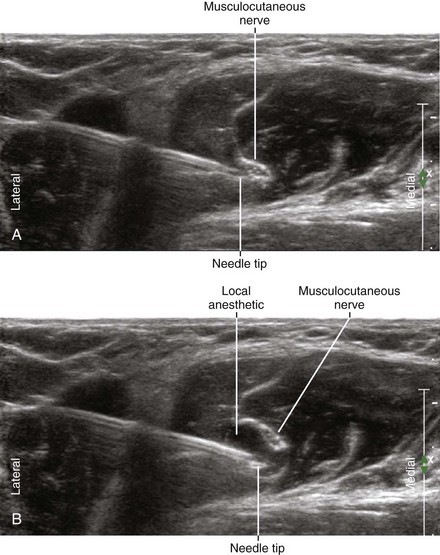
| Approach | SAX view of MCN, in-plane from lateral to medial |
| Place the needle tip at lateral corner of MCN within CBr. | |
| Sonographic assessment | The injection should track along the MCN within CBr. |
| Anatomic variation | Passover MCN (8%-30%) |
| The MCN can travel over the CBr rather than through it. | |
| MCN-median fusion (5%-10%) | |
| The MCN can be fused with the median nerve in the axilla. | |
| This is sometimes referred to as a low-lying lateral cord. |
AA, Axillary artery; CBr, coracobrachialis muscle; MCN, musculocutaneous nerve; SAX, short axis.
1 Tagliafico AS, Michaud J, Marchetti A, et al. US imaging of the musculocutaneous nerve. Skeletal Radiol. 2011;40(5):609–616. Epub 2010, Oct 8
2 Spence BC, Sites BD, Beach ML. Ultrasound-guided musculocutaneous nerve block: a description of a novel technique. Reg Anesth Pain Med. 2005;30:198–201.
3 Schafhalter-Zoppoth I, Gray AT. The musculocutaneous nerve: ultrasound appearance for peripheral nerve block. Reg Anesth Pain Med. 2005;30:385–390.
4 Macchi V, Tiengo C, Porzionato A, et al. Musculocutaneous nerve: histotopographic study and clinical implications. Clin Anat. 2007;20:400–406.
5 Remerand F, Laulan J, Couvret C, et al. Is the musculocutaneous nerve really in the coracobrachialis muscle when performing an axillary block? An ultrasound study. Anesth Analg. 2010;110(6):1729–1734. Epub 2010, Apr 30
6 Orebaugh SL, Pennington S. Variant location of the musculocutaneous nerve during axillary nerve block. J Clin Anesth. 2006;18:541–544.