Chapter 15 Musculo-Skeletal System
Bone
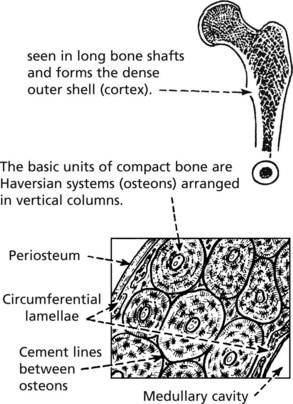
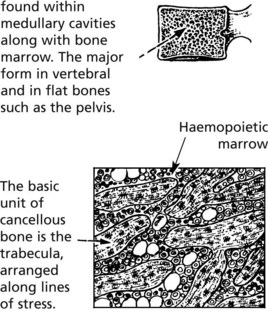
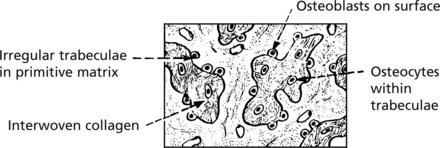
There are two different forms of normal adult bone, both with a lamellar (layered) structure.
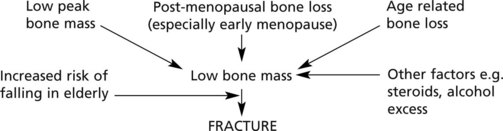
Osteoporosis
OSTEOPOROSIS is the commonest disorder of bone. It is defined as a systemic disease characterised by:
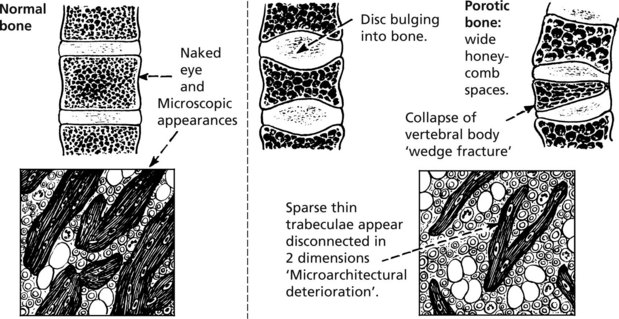
Pathology: The changes in the vertebral bodies are shown.
Aetiology
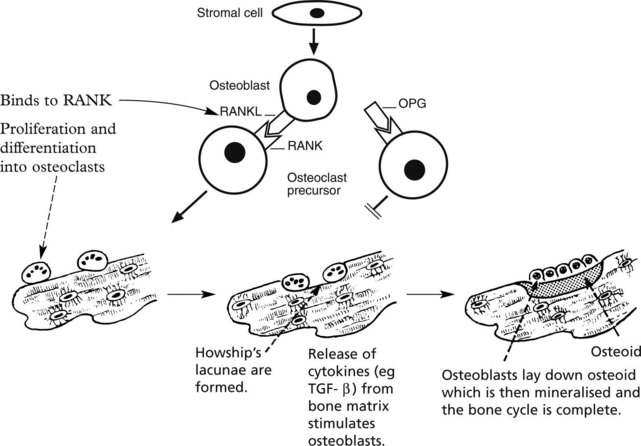
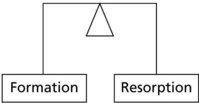
In normal bone the dynamic processes of formation and resorption are in balance.
In osteoporosis the balance is upset by
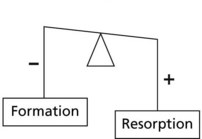
Bone mass decreases with age in both sexes: in old age, osteoblastic activity falls.
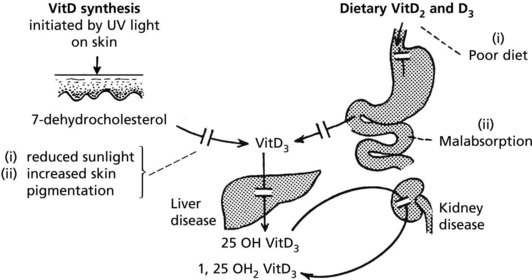
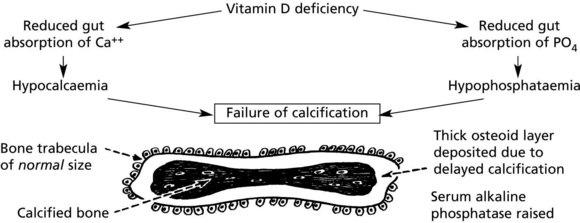
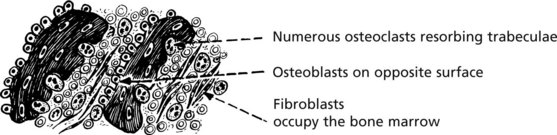
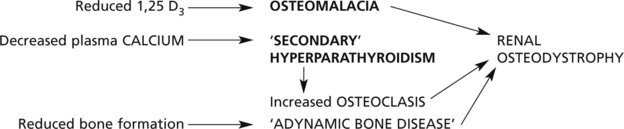
Osteomalacia and Rickets
Osteomalacia and rickets are disorders of bone due to failure of mineralisation of newly formed osteoid, caused by vitamin D deficiency in almost all cases. The poorly calcified bones are soft causing deformity or fracture.
Metabolic Bone Disease
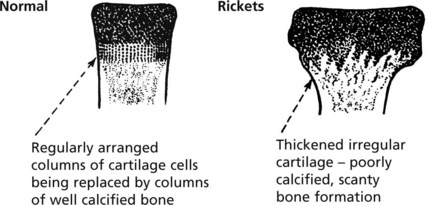
In rickets the growing ends of long bones are abnormal.
This results in stunting of growth and bowing of the lower limbs.
In females permanent deformities of the pelvis can cause serious difficulty during childbirth.
Enlargement of costochondral junctions gives the so-called rickety rosary
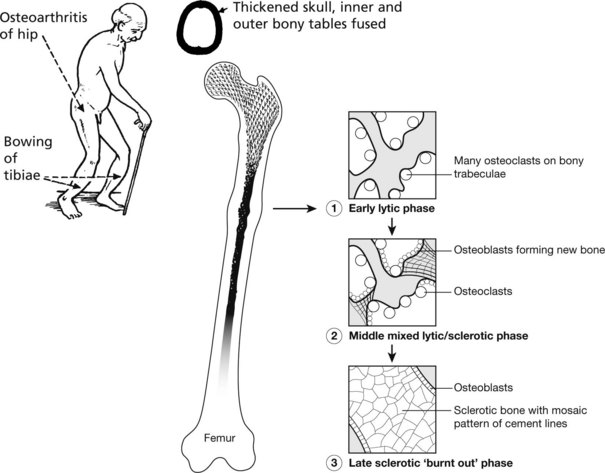
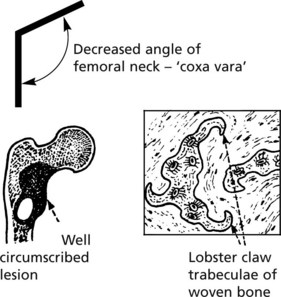
Paget’s Disease of Bone
This disease of unknown aetiology usually presents after the age of 50 years and is more common in males. It is fairly common (3% of autopsies), but only in its more severe forms are there clinical symptoms. The disorder is focal: the bones particularly affected are the pelvis, vertebrae, skull and lower limbs. It has been suggested that virus infection (e.g. measles, distemper) of osteoclasts is responsible. Genetic factors are important.
Often asymptomatic, the main effects are:
The use of bisphosphonates offers effective therapy in many cases.
Bone – Miscellaneous
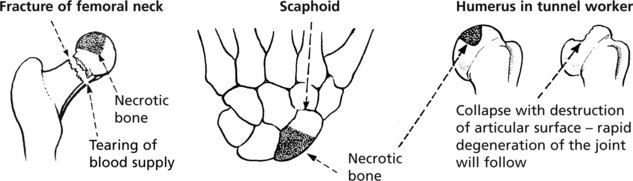
Osteonecrosis (Avascular Necrosis)
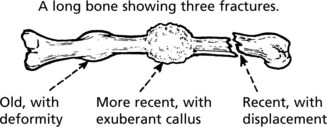
Interruption of its blood supply causes bone to undergo necrosis. This tends to occur with fractures at sites where the vascular supply is damaged. Fractures of the femoral neck and scaphoid bone are good examples.
Bone necrosis occuring at an articular surface often leads to degenerative arthritis.
Infections of Bone
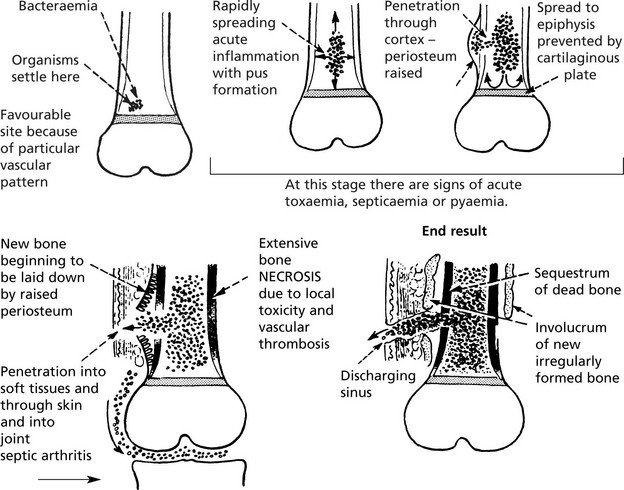
Acute Osteomyelitis
Classically caused by Staphylococcus aureus. This affects the metaphyses of long bones in children. Nowadays the incidence has been greatly reduced and the use of antibiotics aborts the development of the disease. The bacteria are blood borne and settle in the cancellous bone of the metaphysis. The effects are dramatic and rapidly progressive.
The presence of necrotic bone ensures that the inflammation continues.
Developmental Abnormalities
Generalised abnormalities are rare and usually inherited.
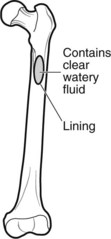
Tumours in Bone
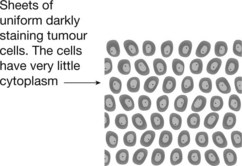
Primary bone tumours are rare. There are both benign and malignant forms, examples of which follow. In contrast, metastatic tumours and myeloma are common.
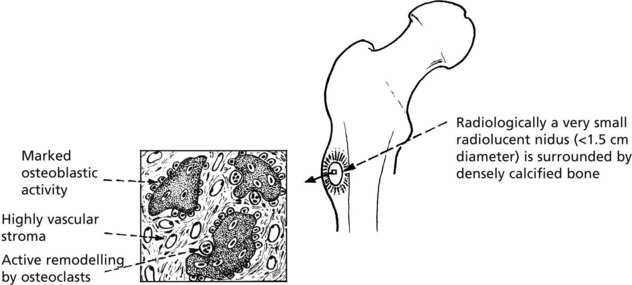
Osteoid Osteoma
This uncommon benign tumour has a striking clinical presentation and a distinctive pathology.
Note: Reaction in surrounding bone; sclerosis of adjacent cortex and periosteal bone thickening.
Malignant Tumours
Primary malignant tumours of bone are not common, but they are important as many arise in young people and are highly malignant. Some arise in older people with pre-existing bone disorders, e.g. Paget’s disease, previous irradiation.
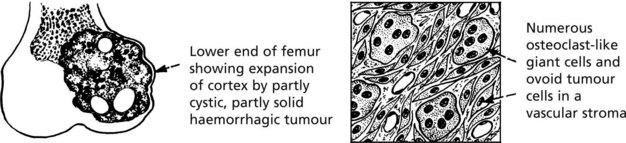
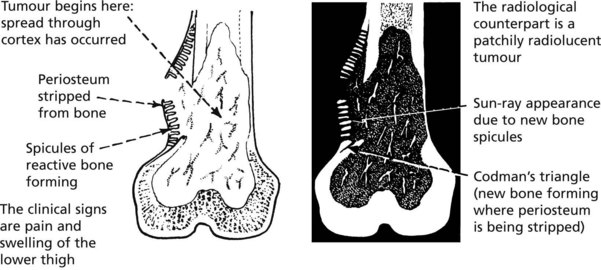
Osteosarcoma
| Young age group – majority of cases (10–25 years) | Elderly subjects (over 60 yrs.) |
|---|---|
| The tumour usually arises near the end of a limb long bone (particularly around the knee). | In 50% of this group, Paget’s disease is associated. Long bones, vertebrae and pelvis are often affected, and tumours may be multicentric in origin. |
Chondrosarcoma
This shows a much slower growth pattern and affects the age group 40–70 years. Multiple enchondromatosis pre-exists in a small number of cases. The tumours arise particularly in the limb girdles and proximal long bones and consist of lobules of cartilage. Progressive local extension is usual. Metastases, usually to the lung, are rare.
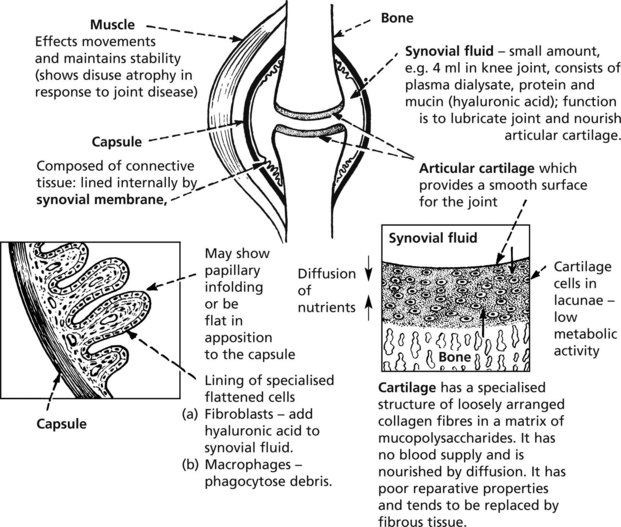
Joint Diseases
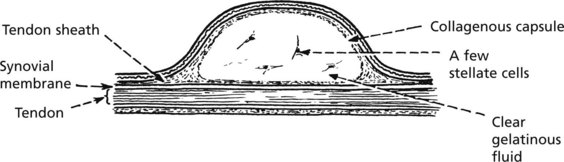
The diagram illustrates the structure of a synovial joint.
As the diseases progress, other secondary effects are added and may obscure the basic pathology.
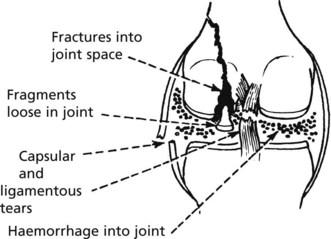
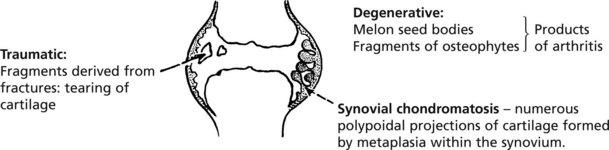
Joint Trauma
Trauma is very variable in its severity and effects.
Serious damage to joints include:
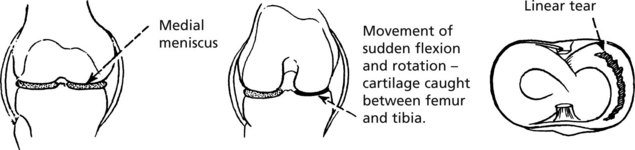
The medial meniscus of the knee is susceptible to tears:
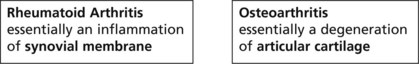
Osteoarthritis (OA)
Osteoarthritis (OA)
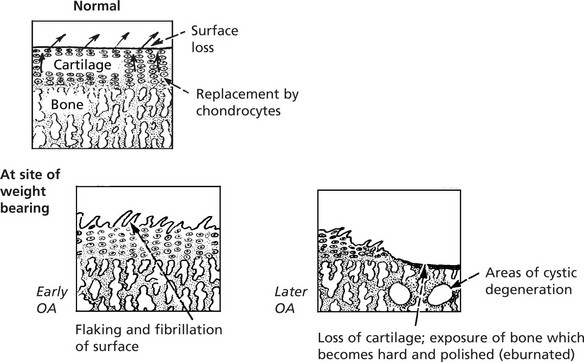
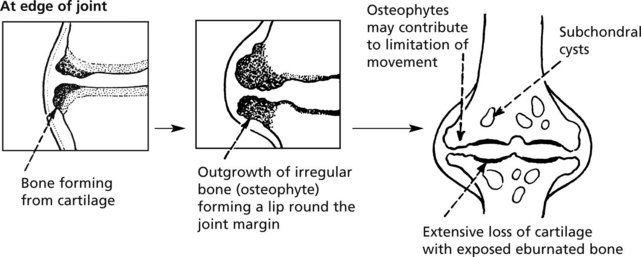
This is the commonest disorder of joints and, by causing pain and stiffness, is the commonest cause of chronic disability after middle age. The basic pathology is degenerative and is similar to the changes of ageing.
The earliest change in ageing and OA is in the chemical composition of the matrix which becomes softer. This is followed by progressive characteristic morphological changes.
Distribution: secondary OA often affects a single predisposed joint.
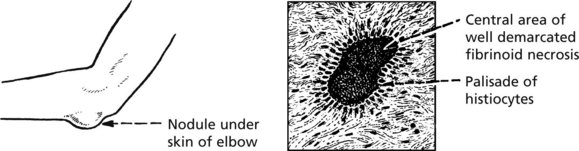
Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a common systemic disease (1–3% of population in Europe). The most affected tissue is the synovial membrane. The typical clinical course is insidious in its onset and progression; in a minority, the onset is acute and the progress rapid. Frequently there are remissions and exacerbations.
| Incidence: female > male 3:1 | Age of onset: usually 35–55 years, but also in childhood – usually severe. |
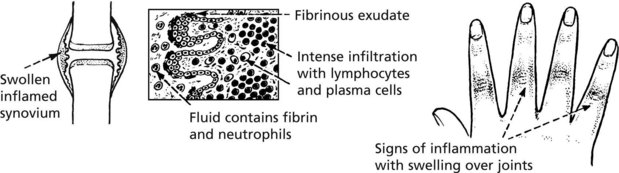
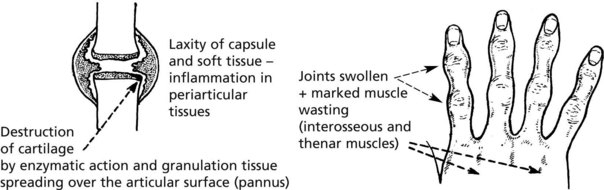
Pathology: The synovial membrane shows chronic inflammation.
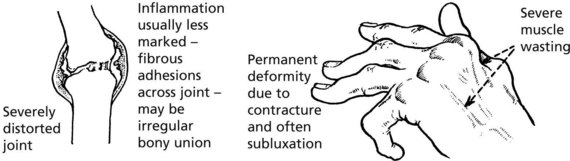
Late
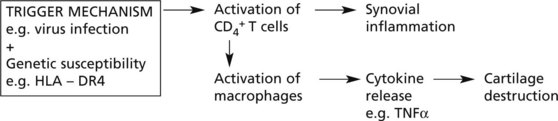
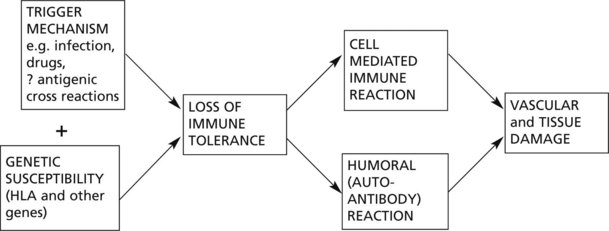
Rheumatoid arthritis is an autoimmune disease, with no single provoking factor. A possible hypothesis is:
Modern therapy directed against TNFα suppresses disease activity and stops joint destruction.
Rheumatoid Factors
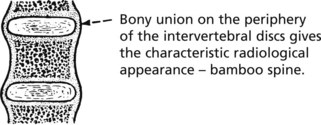
Sero-Negative Arthritis
Ankylosing spondylitis (AS) is an arthritis affecting particularly the sacroiliac, costovertebral and vertebral joints, but peripheral arthritis is also seen.
| Incidence: 0.05% of population male:female; 3:1. | Age of onset: Young adults progressing into middle age. Rheumatoid factor negative. |
Aortitis leading to aortic incompetence and uveitis may be seen.
| OSTEOARTHRITIS | RHEUMATOID ARTHRITIS | |
|---|---|---|
| Type of disorder | Degenerative | Inflammatory |
| Site of initial damage | Articular cartilage | Synovial membrane |
| Age | Late middle age + | 3rd decade (any age) |
| Joints affected | Large weight bearing often single, pre-existing local factors in some cases | Small joints of hands and feet, multiple |
| Systemic disease | None ESR – normal Rheumatoid factor – absent |
++ ESR ↑ Rheumatoid factor positive Secondary anaemia |
Infections of Joints
Joint and Soft Tissues – Miscellaneous
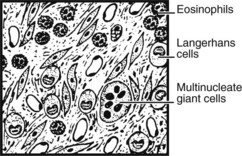
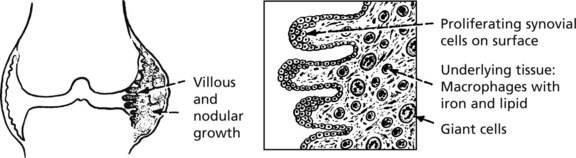
Pigmented Villonodular Synovitis (PVNS) (Tenosynovial Giant Cell Tumour)
This may affect any synovial tissue, but the knee and hip joints are most commonly involved.
It is now thought to be neoplastic but to all intents it never metastasises.
Similar but well-defined nodules are common in the fingers and toes.
Para-Articular Tissues – Miscellaneous
Collagen Diseases
This term describes a group of multisystem diseases, many autoimmune in origin.
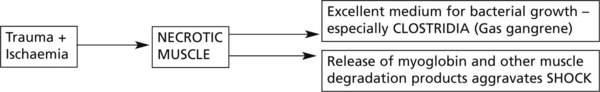
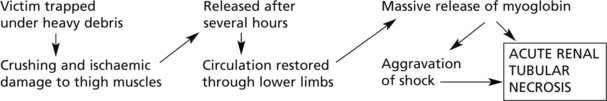
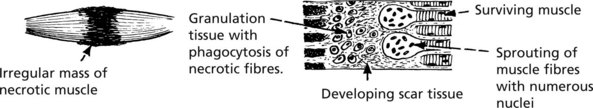
Skeletal Muscle
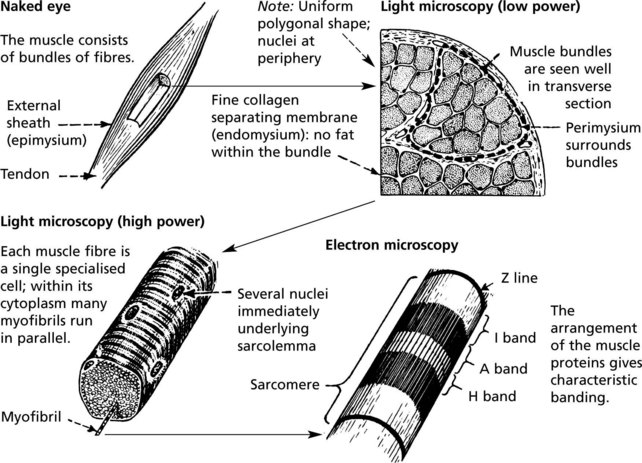
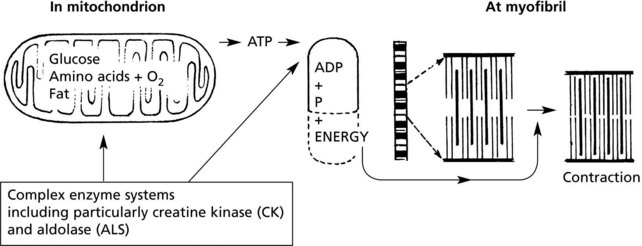
Muscle Contraction
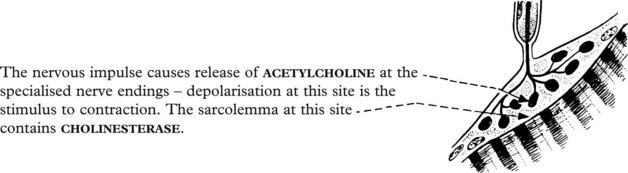
The basic mechanism is as follows:
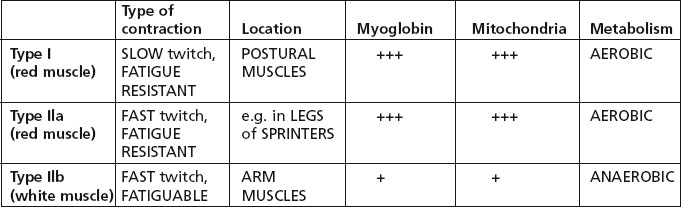
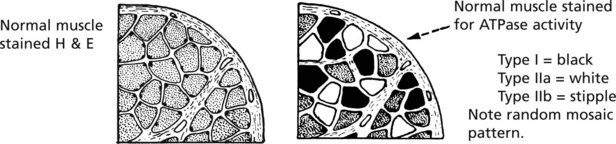
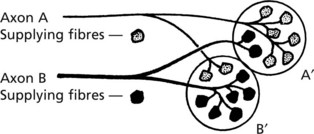
There are 3 types of muscle fibre, related to differences in functional activity.
In section, the three fibre types are identified by their ATPase activity.
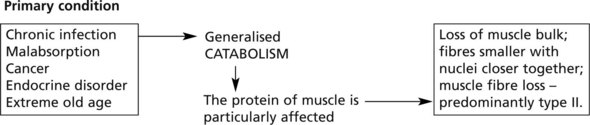
Atrophy And Hypertrophy
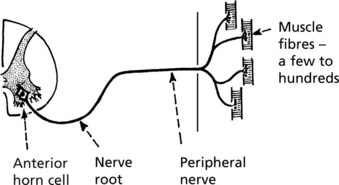
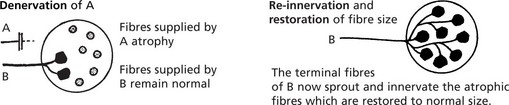
Generalised disuse atrophy occurs as a result of prolonged immobilisation in bed. Local atrophy follows immobilisation due to joint disease or after bone fractures.
Hypertrophy of muscle tissue in response to increased work load is well seen in athletes.
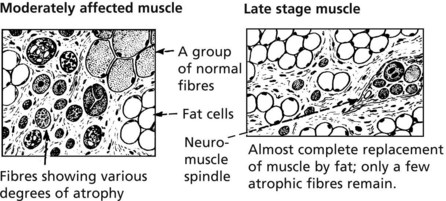
Note: Atrophy may be partially masked by increased fat in the septal tissues.
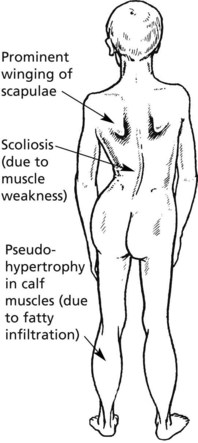
Muscular Dystrophy
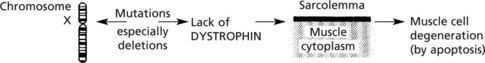
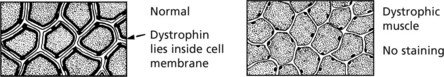
Muscular dystrophies are inherited diseases, causing muscle damage and weakness.
Inherited Myopathies
Specific Metabolic Defects
There is a group of genetic myopathies with specific biochemical or morphological abnormalities.
| (1) Glycogen storage | (2) Lipid metabolism | (3) Periodic paralysis |
| Type 2 (Pompe) – deficiency of acid maltase Type 5 (McArdle) – muscle phosphorylase Type 7 – phosphofructokinase (PFK) |
Defect in free fatty acid transport into and utilisation within fibre. |



These myopathies vary in age of onset, clinical presentation and prognosis.
Acquired Myopathies
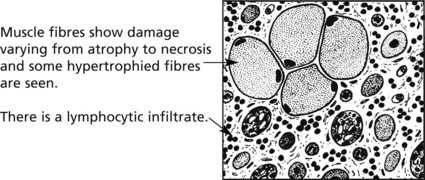
Inflammatory myopathies – polymyositis and dermatomyositis – are two similar inflammatory disorders of muscle.
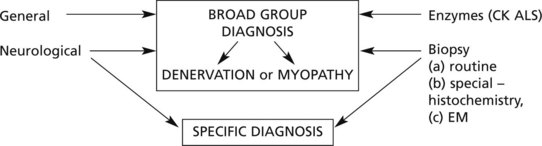
Muscle Diseases – Diagnosis
Accurate diagnosis of muscular weakness and atrophy is important since there is considerable variation in prognosis and management of these disorders, although often there is no treatment.
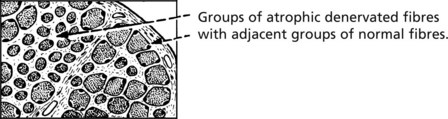
These methods distinguish primary myopathies, including myotonias, from denervation atrophy.
EM examination and biochemical analysis may identify specific disorders.