Muscle tone
What is normal muscle tone?
Muscle tone is often referred to as a state of readiness in a muscle at rest (resting tone) which provides us with a background level of tone from which we can function efficiently. It is defined by the resistance to passive movement, which is an expression of the stiffness of the muscle fibres (Brodal 2004). Normal tone should be high enough to keep you up against gravity but low enough to allow movement.
• The individual will ‘follow’ the movement (i.e. the muscles are active but allowing the movement to occur)
• The limb can be ‘placed’ at any point in the movement and will remain in its designated position.
Muscle tone is considered to depend physiologically on two factors:
Non-neural factors
This is a consequence of the mechanical-elastic properties of the soft tissues (compliance or stiffness of soft tissue structures) and incorporates the thixotropic properties (viscosity) of the muscle and the muscle length. These factors contribute a significant component to the normal resting tone of a muscle which explains how we are able to stand still with only minimal corrective bursts of postural muscle activity (Simons and Mense 1998). These non-neural factors can be influenced by age, temperature and exercise.
Neural factors
The neural factors relate to the degree of activation of the contractile apparatus of the muscle. Our muscles are constantly contracting or active and it is the nervous system that controls the appropriate level of this background activity. The level of muscle contraction is a result of the output from the alpha motor neuron (AMN) in the ventral horn of the spinal cord (S2.13) which innervates the muscle itself. The AMN output is dictated by the final outcome of competing inhibitory and excitatory synapses from various inputs related to both the peripheral and central nervous systems. These include:
• Muscle spindles (tonic component of the stretch reflex) (TSR) (S2.13)
• Golgi tendon organ (GTO) (S2.13)
• Somatosensory receptors in the body (skin, joints, connective tissue, muscles) (S3.23)
• Sensory systems such as visual, auditory, vestibular (S2.10)
• Limbic system related to our emotional state (S2.9)
• Interneurons within the spinal cord
• Various higher centres via the descending tracts (Reticular formation S2.10) (Nielsen et al. 2007).
What is abnormal muscle tone?
Individuals who have a neurological lesions affecting the central nervous system (CNS) may lose the ability to control the level of muscle tone and may present with resting tone that is either too low (hypotonia) or too high (hypertonia) (Brodal 2004). It is also common to see both these characteristics present in an individual patient.
In CNS lesions, muscle weakness (S3.30) is evident in association with both hypotonia (reduced muscle tone) and hypertonia (increased muscle tone). The relationship between these concepts is complex but it appears likely that both altered tone states directly contribute to a reduction in force production (weakness) of the muscle. The pathophysiology which defines alterations in muscle tone will also lead to a dysfunction in the timing or pattern of motor unit recruitment or the number of units able to be recruited. This will lead to a presentation of muscle weakness during certain movements. It should also be noted that when altered tone exists over a prolonged period, the outcome may be disuse of the part, and further muscle weakness may occur as a consequence of sarcomere loss and reduction in cross-sectional area (S3.30).
In terms of assessment, a comparison of the conceptual definitions gives the therapist a simplified tool by which to differentiate muscle tone and weakness. Muscle tone is defined as the resistance to passive movement, representing the background level of tension or stiffness in a muscle (Moore and Kowalske 2000). Therefore it should be assessed in a muscle at rest. Muscle weakness on the other hand is defined as the inability to generate sufficient force to overcome the resistance of a task and therefore by definition should be assessed during movement activities.
Hypotonia
Pathophysiology of hypotonia
Hypotonia presents in many pathologies involving the central nervous system, e.g. multiple sclerosis, traumatic brain injury and cerebrovascular accident (CVA). Where an acute insult occurs, the nervous system may go into a state of neural shock (Kwakkel et al. 2003). The shock results in reduced neuronal conduction (S2.6) and a breakdown in communication within the nervous system. If the motor systems are affected, an insufficient number of alpha motor neurons can be recruited and hypotonia presents. Over time, as the nervous system recovers the neural shock subsides, neural transmission is resumed and muscle tone begins to return. However, there is no guarantee that it will return to normal.
If the patient still presents with hypotonia after a 4-week period, the presentation is sometimes termed ‘prolonged muscular flaccidity’ (Kwakkel et al. 2003). In CVA, the prognosis for the final outcome is poor if this state remains beyond 3 months (Formisano et al. 2005). The definitive cause of prolonged muscular flaccidity is unclear in the current literature. It has been hypothesized to result from a reduction in the levels of arousal and central drive leading to insufficient excitation at the alpha motor neuron. However, the cortical loops associated with the basal ganglia and cerebellum are also found to be severely affected in patients with prolonged muscular flaccidity (Pantano et al. 1995).
Hypertonia
Rigidity defined
Traditionally, rigidity is defined as an increased resistance to passive movement which is constant throughout the range of movement. The resistance occurs throughout the full range of a passive movement and will be present in all muscles (including the face). The resistance is described as ‘lead-pipe’ (constant through range) or ‘cogwheel’ (resistance followed by a period of ‘give’) (Fung and Thompson 2002; Xia and Rymer 2004). As a result of rigidity affecting all muscle groups, patients often present with a lack of rotation, especially in the trunk (Wright et al. 2007). Recent studies have shown that rigidity is also velocity dependent (Mak et al. 2007; Xia et al. 2009). Voluntary movement is difficult both to initiate and arrest. Tendon reflexes are usually normal.
Pathophysiology of rigidity
Neural factors
The neural factors are a result of damage to the basal ganglia (S2.11) and particularly, the dopamine-producing cells of the substantia nigra (SN). The dopaminergic neurons of the SN project to the striatum and normally modulate the activity of both the direct and indirect pathways within the basal ganglia (S2.11), having the opposite effect on each. The direct pathway facilitates the initiation and selection of the correct voluntary movement programmes to achieve a task, while the indirect pathway helps to prevent any unwanted movement programmes. In PD, the loss of dopaminergic cells in the SN means that the ability to modulate motor programme selection is lost and there is inappropriate competition between the correct and incorrect movement programmes being sent to the cortex. At a muscular level, this presents as inappropriate co-contraction (Xia and Rymer 2004; Xia et al. 2009) attributed to inadequate reciprocal inhibition (Meunier et al. 2000). Consequently, a hypokinetic movement disorder presents, or in simple terms a lack of movement.
Non-neural
Altered muscle activity and joint movement leads to structural and functional changes in the musculoskeletal system. Muscles lose sarcomeres, becoming shorter, stiffer and more thixotropic and collagen production may be altered and disorganized. This structural change is considered to significantly contribute to the resistance to passive movement (Bhakta 2000; Chung et al. 2004; Vattanasilp et al. 2000).
Hypertonia (related to spasticity) defined
Hypertonia (related to spasticity) is notoriously difficult to understand for the novice therapist. This is primarily because in clinical practice the term ‘spasticity’ is often used interchangeably with hypertonia. This is misleading. Spasticity is defined as velocity- and length-dependent increase in the tonic stretch reflex with exaggerated tendon reflexes and is described as a range of positive and negative features (Table 21.1), one of which is hypertonia (Lance 1980; Platz et al. 2005; Burridge et al. 2005). Therefore, for clarity, this text will use the term ‘hypertonia (related to spasticity)’. Hypertonia (related to spasticity) is defined as an increase in resistance to a passive movement that increases with the velocity of the movement and then fades away as the muscle is held in a constant stretch, when it is described as ‘clasp knife’. The clinical presentation is a feeling of stiffness during part of or all of the range of movement and the patient’s limb may be held in an abnormal posture. The pattern of hypertonia (related to spasticity) may be present in any muscle group, however common presentations have been linked with lesions of different levels of the brain:
Table 21.1
The positive and negative features of spasticity
| Positive features | Negative features |
| Hyper-reflexia (S3.22) | Weakness (S3.30) |
| Hypertonia | Inability to fractionate |
| Gross movement patterns (S3.18) | Poor selective movement |
| Associated reactions (S3.18) | |
| Abnormal co-contraction | |
| Clonus (S3.18) |
Decorticate: a lesion at the level of the cerebral cortex (S2.7) or subcortical diencephalon (S2.9) the posture of hypertonia tends to be a flexor pattern of the upper limbs and an extensor pattern of the lower limbs (Magee 2002), the antigravity muscles.
Decerebrate: a lesion at the level of the brain stem (S2.10) the posture tends to be a predominance of extensor tone throughout (Kandel et al. 2000; Magee 2002).
Clinical observation seems to indicate that voluntary movement, increased effort and increased sensory stimulation may further increase hypertonia. However, evidence shows that in terms of reflex activity, this is not the case (Sharp and Brouwer 1997; Ada et al. 1998; Burne et al. 2005).
Pathophysiology of hypertonia (related to spasticity)
Hypertonia (related to spasticity) may be seen in patients with a lesion of the CNS. However, the nature of the pathology will dictate whether the onset is immediate (traumatic brain injury) or slowly evolving (CVA, multiple sclerosis, spinal cord injury) (Edwards 2002). The presentation of increased resistance to passive movement is related to a combination of neural and non-neural factors:
Neural factors
Interruption of the inhibitory pathways. Damage to the CNS, particularly the cortico-reticular pathway (Rathore 2002), results in reduced cortical drive to the inhibitory centre in the reticular formation (S2.10). The outcome is a release of the tonic stretch reflex (TSR) from higher centre inhibitory control (S2.13), which means that it becomes inappropriately responsive and muscle tone is increased. This is hypertonia. There is strong evidence linking spasticity with the release of the TSR in cerebral injury (Lin and Sabbahi 1999; Burne et al. 2005).
Increased activity of the excitatory pathways. Following damage to the nervous system, the surviving adjacent neurons undergo physiological changes which lead to structural adaptations (Nielsen et al. 2007). These adaptations are a result of neuroplastic processes which include denervation supersensitivity, collateral sprouting, unmasking and synaptic strengthening. However, these processes do not necessarily lead to a positive functional outcome. In the case of spasticity, it is thought that increased sensitivity of the post-synaptic receptors on the remaining neurons and sprouting of adjacent dorsal root afferents can lead to an overall increase in excitatory inputs to the alpha motor neuron and hence hypertonia. This latter explanation of hypertonia could explain why hypertonia tends to develop over time (Sheean 2002).
Non-neural
Altered muscle activity and joint movement leads to structural and functional changes in the musculoskeletal system. Muscles lose sarcomeres, becoming shorter, stiffer and more thixotropic and collagen production may be altered and disorganized. This structural change is considered to significantly contribute to the resistance to passive movement (Bhakta 2000; Chung et al. 2004; Vattanasilp et al. 2000).
In the literature, there remains uncertainty as to the relevant contributions of neural and non-neural factors. Electromyography studies show that the reflex-mediated increase in muscle tone reaches its maximum between 1 and 3 months post-lesion (Bhakta 2000; Teasell and Heitzner 1998), whereas others state that reflexic activity is only evident when a limb is moved quickly (Vattanasilp et al. 2000). However, after 3 months, the increased resistance to passive stretch is proposed to be primarily due to the intrinsic non-neural stiffness of the muscle (Bhakta 2000; Chung et al. 2004; Vattanasilp et al. 2000).
Why do I need to assess muscle tone?
It is important to assess muscle tone because of its potential effect on functional ability. Hypotonia appears to be a negative prognostic indicator in CVA and also prolongs the rehabilitation process (Formisano et al. 2005). A direct correlation between hypertonia and the level of disability has not been established (Sommerfeld et al. 2004) and little is known about hypertonia in a contracting muscle. In fact, some evidence implies that movement disorders observed in patients who present with hypertonia are the result of weakness in the agonist muscle rather than hypertonia in the antagonist. It is therefore unclear how, or if, hypertonia contributes directly to the movement disorders itself. However, a detrimental effect on function has been associated with the secondary side-effects of hypertonia, which include pain (Pizzi 2005), contracture (Watkins et al. 2002; Pizzi 2005), limitation of range of movement (Lin and Sabbahi 1999) and muscle weakness (Maruishi et al. 2001).
How do I assess muscle tone?
Observation
Therapist
Are left and right sides similar in terms of muscle bulk? Increased muscle bulk may be indicative of hypertonia, where hypertrophy has occurred. Decreased muscle bulk may signify hypotonia. These signs are not definitive because other factors can produce differences in bulk between sides (e.g. handedness and level, type and frequency of functional activities).
Are there asymmetrical excessive skin creases present (Fig. 21.1)? These may indicate that the underlying muscle is underactive due to hypotonia.
Figure 21.1 Skin creases in sitting.
Does the patient present with any abnormal patterns of movement (S3.18)? Signs of hypotonia relate to postural instability, the inability to stabilize body segments against the effects of gravity. Therapists often evaluate active movement looking for gross patterns of movement, increased effort and associated reactions as signs of spasticity, however although hypertonia is often associated with these signs, there is no evidence to suggest a direct link (Ada and O’Dwyer 2001; Bhakta et al. 2001). The novice therapist should therefore be clear about what is being evaluated and why.
Passive movements
Therapist
Limb testing
1. Support the full weight of the limb to be tested (Figs 21.2, 21.3).
2. Move the limb slowly through its full range of motion.
3. Re-evaluate that the movement is passive (no effort on the part of the patient).
4. The therapist may need to repeat the movement, however this should be kept to a minimum as movement may influence the non-neural component in hypertonic muscles.
5. If hypertonia is suspected an increase in the speed of the passive movement may help in confirming the diagnosis. This specifically tests the reflex component of muscle stiffness. The velocity-dependent hypertonic muscle then offers greater resistance.
6. Repeat the passive movements in all directions of movement and for all joints, including both upper and lower limb. For example, at the shoulder, assess medial/lateral rotation, abduction/adduction and flexion/extension.
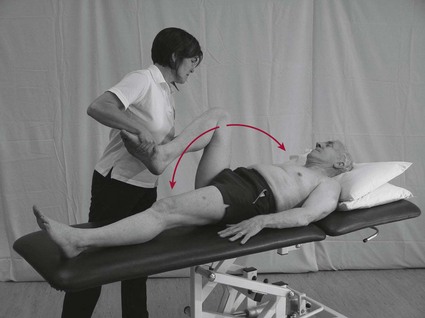
Figure 21.2 Assessing muscle tone (lower limbs).
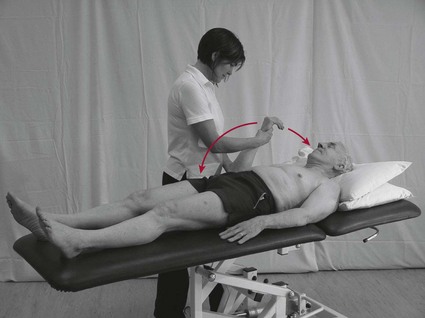
Figure 21.3 Assessing muscle tone (upper limbs).
Trunk testing
This involves performing a passive movement to the patient’s trunk.
1. This can be achieved with the patient in sitting (Fig. 21.4) but equally well in side lying (Fig. 21.5).

Figure 21.4 Assessing muscle tone (trunk) in sitting.

Figure 21.5 Assessing muscle tone (trunk) in side lying.
2. The trunk/thorax should be moved in all directions in relation to the pelvis in order to assess the resistance in the trunk muscles.
3. In order to carry this out effectively, one segment (pelvis) may need to be stabilized while the other (trunk) is moved. This will require two therapists.
Is there any resistance to the passive movement? Yes, indicates hypertonia. No, indicates normal tone or hypotonia.
At what point in the movement is the resistance felt? Hypertonia associated with spasticity can occur in part of the movement range or throughout range, whereas that associated with rigidity occurs throughout the full range.
Are there any defining characteristics to the resistance offered? Clasp knife (related to spasticity) or cog wheel/lead pipe related to rigidity. Hypertonia in all muscle groups is indicative of rigidity, whereas a presentation confined to particular muscle groups is likely to be hypertonia (related to spasticity).
Does the resistance increase if the speed of the passive movement is increased? This velocity-dependent change indicates hypertonia, but it could be spasticity or rigidity.
Does the limb feel heavy and provide little or no resistance to the movement? This is hypotonia.
Reflex testing
Therapist
Reflex testing (S3.22) is carried out to evaluate or confirm the integrity of the reflex pathway and the reflexic properties of the muscle. This may tell us in part about the neural component of muscle tone but it does not tell us about the overall stiffness of a muscle. Therefore it is an inappropriate tool to use for testing muscle tone in isolation. In terms of hypo-reflexia, the peripheral or central nervous system could be implicated. A hyper-reflexic muscle may confirm the involvement spasticity, however caution is advised when directly relating this finding to hypertonia as the evidence indicates that there is a low correlation between the existence of hypertonia and increased tendon jerk reflexes (S2.22) (Teasell and Heitzner 1998).
Recording
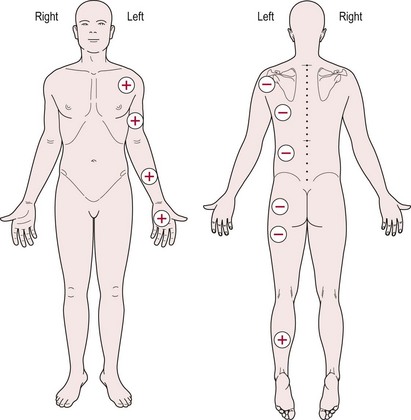
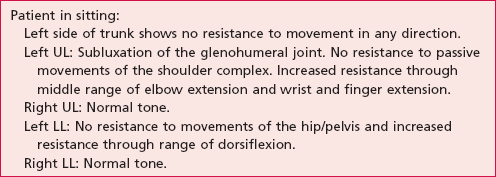
When recording findings, the therapist may use a body chart (Fig. 21.6) or a text description (Table 21.2).
Analysis
Analysis of the example shown in Figure 21.6 and Table 21.2 leads to the hypothesis that hypotonia exists through the left trunk, shoulder and hip girdles, with hypertonia evident in the flexor muscles of the left elbow, wrist and hand and in the extensor muscles of the left ankle.
References and Further Reading
Ada, L, O’Dwyer, N. Do associated reactions in the upper limb after stroke contribute to contracture? Clinical Rehabilitation. 2001; 15:186–194.
Ada, L, Vattanasilp, W, O’Dwyer, N, et al. Does spasticity contribute to walking dysfunction after stroke? Journal of Neurology Neurosurgery and Psychiatry. 1998; 64:628–635.
Bhakta, BB. Management of spasticity in stroke. British Medical Bulletin. 2000; 56:476–485.
Bhakta, BB, Cozens, JA, Chamberlain, MA, et al. Quantifying associated reactions in the paretic arm in stroke and their relationship to spasticity. Clinical Rehabilitation. 2001; 15:195–206.
Brodal, P. The central nervous system: structure and function, ed 3. Oxford: Oxford University Press; 2004.
Burne, JA, Carleton, VL, O’Dwyer, NJ. The spasticity paradox: movement disorder or disorder of resting limbs? Journal of Neurology Neurosurgery and Psychiatry. 2005; 76:47–54.
Burridge, JH, Wood, DE, Hermens, HJ, et al. Theoretical and methodological considerations in the measurement of spasticity. Disability and Rehabilitation. 2005; 271/2:69–80.
Chung, SG, van Rey, E, Bai, Z, et al. Biomechanic changes in passive properties of hemiplegic ankles with spastic hypertonia. Archives of Physical Medicine and Rehabilitation. 2004; 85:1638–1646.
Corden, DM, Lippold, OC, Buchanan, K, et al. Long-latency component of the stretch reflex in human muscle is not mediated by intramuscular stretch receptors. Journal of Neurophysiology. 2000; 84:184–188.
Edwards, S. Neurological physiotherapy. Edinburgh: Churchill Livingstone; 2002.
Formisano, R, Pantano, P, Buzzi, MG, et al. Late motor recovery is influenced by muscle tone changes after stroke. Archives of Physical Medicine and Rehabilitation. 2005; 86:308–311.
Fung, VS, Thompson, PD. Rigidity and spasticity. In: Jankovic JJ, Tolosa E, eds. Parkinson’s disease and movement disorders. ed 4. Philadelphia: Lippincott Williams and Wilkins; 2002:473–482.
Kandel, ER, Schwartz, JH, Jessell, TM. Principles of neural science, ed 4. New York: McGraw-Hill; 2000.
Kwakkel, G, Kollen, BJ, van der Grond, J, et al. Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke. 2003; 34:2181–2186.
Lance, JW. Spasticity: disordered motor control. In: Feldman RG, Young RR, Koella WP, eds. Spasticity: disordered motor control. Chicago: Year Book Medical; 1980:485–494.
Lin, F-M, Sabbahi, M. Correlation of spasticity with hyperactive stretch reflexes and motor dysfunction in hemiplegia. Archives of Physical Medicine and Rehabilitation. 1999; 80:526–530.
Magee, DJ. Orthopaedic physical assessment, ed 4. Canada: Elsevier Sciences; 2002.
Mak, MK, Wong, EC, Hui-Chan, CW. Quantitative measurement of trunk rigidity in parkinsonian patients. Journal of Neurology. 2007; 254:202–209.
Maruishi, M, Mano, Y, Sasaki, T, et al. Cerebral palsy in adults: independent effects of muscle strength and muscle tone. Archives of Physical Medicine and Rehabilitation. 2001; 82:637–641.
Meunier, S, Pol, S, Houeto, JL, et al. Abnormal reciprocal inhibition between antagonist muscles in Parkinson’s disease. Brain. 2000; 123:1017–1026.
Moore, DP, Kowalske, KJ. Neuromuscular rehabilitation and electrodiagnosis of myopathy. Archives of Physical Medicine and Rehabilitation. 2000; 81:S-32–S-35.
Nielsen, JB, Crone, C, Hultborn, H. The spinal pathophysiology of spasticity – from a basic science point of view. Acta Physiologica. 2007; 1892:171–18010.
Pantano, P, Formisano, R, Ricci, M, et al. Prolonged muscular flaccidity after stroke: morphological and functional brain alterations. Brain. 1995; 118:1329–1338.
Platz, T, Eickhof, C, Nuyens, G, et al. Clinical scales for the assessment of spasticity associated phenomena and function: a systematic review of the literature. Disability and Rehabilitation. 2005; 271/2:7–18.
Pizzi, A, Carlucci, G, Falsini, C, et al. Evaluation of upper-limb spasticity after stroke: a clinical and neurophysiologic study. Archives of Physical Medicine and Rehabilitation. 2005; 86:410–415.
Rathore, SS, Hinn, AR, Cooper, LS, et al. Characterization of incident stroke signs and symptoms: findings from the Atherosclerosis Risk in Communities Study. Stroke. 2002; 33:2718–2721.
Sharp, SA, Brouwer, BJ. Isokinetic strength training of the hemiparetic knee: effects on function and spasticity. Archives of Physical Medicine and Rehabilitation. 1997; 78:1231–1236.
Sheean, G. The pathophysiology of spasticity. European Journal of Neurology. 2002; 9:3–9.
Simons, DG, Mense, S. Understanding and measurement of muscle tone as related to clinical muscle pain. Pain. 1998; 75:1–17.
Sommerfeld, DK, EekE, U-B, Svensson, A-K, et al. Spasticity after stroke: its occurrence and association with motor impairments and activity limitations. Stroke. 2004; 35:134–140.
Teasell, RW, Heitzner, JD. The painful hemiplegic shoulder. Physical Medicine and Rehabilitation: State of the Art. 1998; 12:489–500.
Vattanasilp, W, Ada, L, Crosbie, J. Contribution of thixotropy spasticity and contracture to ankle stiffness after stroke. Journal of Neurology Neurosurgery and Psychiatry. 2000; 69:34–39.
Watkins, C, Leathley, M, Gregson, J, et al. Prevalence of spasticity post stroke. Clinical Rehabilitation. 2002; 165:515–522.
Woollacott, AJ, Burne, JA. The tonic stretch reflex and spastic hypertonia after spinal cord injury. Experimental Brain Research. 2006; 1742:386–396.
Wright, WG, Gurfinkel, VS, Nutt, J, et al. Axial hypertonicity in Parkinson’s disease: direct measurements of trunk and hip torque. Experimental Neurology. 2007; 208:38–46.
Xia, R, Rymer, WZ. Reflex reciprocal facilitation of antagonist muscles in spinal cord injury. Spinal Cord. 2004; 43:14–21.
Xia, R, Sun, S, Threlkeld, J. Analysis of interactive effect of stretch reflex and shortening reaction on rigidity in Parkinson’s disease. Clinical Neurophysiology. 2009; 120:1400–1407.