Multiple Trauma
Perspective
The care of the injured patient remains one of the mainstays of emergency medicine practice. Emergency physicians play a vital role in the stabilization and diagnostic phases of trauma care. Management of trauma patients involves complex, time-dependent decision-making, leadership capability, and technical skill. Proper resuscitation can enhance functional outcomes, even in severely injured patients.1
Epidemiology
In 2009, there were 117,176 deaths from unintentional injury, of which 31% were motor vehicle related. Accidents continue to be the leading cause of death in people aged 1 to 44 years.2 The motor vehicle fatality rate has declined over the past decade from 15.3 deaths per 100,000 population in 1999 to 11.0 deaths per 100,000 in 2009.3 Likewise, the number of people injured in motor vehicle collisions (MVCs) has declined as well, to 2.2 million people in 2009.4 Firearm deaths continue to be of significant concern in the United States. In 2009, there were 31,228 deaths by firearm.2 The economic cost of traumatic injuries is staggering. It is estimated that the total cost of injuries that occurred in 2000 is $406 billion; this includes medical costs and lost productivity. Motor vehicle and fall injuries account for 22% ($89 billion) and 20% ($81 billion) of this total, respectively.5
Many of these injuries are avoidable. Proper use of lap and shoulder belts can reduce the risk of fatal injury from an MVC; it is estimated that in 2009 alone, seatbelts saved 12,713 lives.6 In 2009, 29% of occupant MVC fatalities involved individuals who were not restrained.3 The number of MVC fatalities has been decreasing steadily since 1994, but there is room for improvement. Young adults continue to use restraints at a lower rate than the national average, but usage by this age group is increasing. Eighty-four percent of adults aged 25 to 69 years use seatbelts compared with 81% of 16- to 24-year-olds.7 It is interesting to note that there are racial differences in seat belt use. Seventy-nine percent of blacks use seatbelts compared with 84% of whites and 89% of other races.7 It is estimated that proper restraint use in vehicles by occupants age 5 years and older would have prevented 3688 MVC-related deaths.6 Child safety seats reduce the risk of death in passenger cars by 71% for infants and by 54% for toddlers ages 1 to 4 years.8 Educational and law enforcement initiatives addressing seat belts, proper child restraint, drinking and driving, gun safety, and fall prevention can assist in raising public awareness. For example, the National Highway Traffic Safety Administration (NHTSA) “Click It or Ticket” campaign increased belt use in 41 of 50 states and the District of Columbia during a 2-month time period.9 NHTSA recently finished a small pilot study of a device to provide haptic feedback to the gas pedal when drivers attempted to drive over 25 mph. The researchers noted 100% seat belt use when this technology was implemented.10 Further study of new technologies may improve restraint use. The effect of firearm laws on decreasing firearm violence is less concrete (even though a decrease in injuries related to firearm violence has been seen).11 Further study is needed to determine the impact of legislation, public education, and prevention programs on firearm violence.
Trauma Systems
The first document to set criteria for categorizing hospitals as trauma centers was promulgated by the American College of Surgeons (ACS) Committee on Trauma in 1976.12 As other groups recognized the importance of structured trauma care, legislation and funding to promote the development of trauma systems grew. In the early 1990s the Health Resources and Services Administration developed the Model Trauma Care System Plan, a well-designed framework for progress measurement in trauma systems. Unfortunately, this program lost funding in 2006. As of 1998, 38 states and the District of Columbia had at least one critical element in place for a formal trauma system.10 More up-to-date data are not readily available because the program was the main source for this information.
Data on the benefit of regionalized trauma systems are convincing. The National Study on the Costs and Outcomes of Trauma showed a 25% reduction in mortality for severely injured patients who received care at a level I trauma center versus patients at a non–trauma center.13 A meta-analysis of 14 studies demonstrated an overall 15% decline in mortality caused in the presence of a trauma system.14 However, this apparent reduction in fatalities may be confounded by other factors. A nationwide study suggests that mortality reduction could not be solely attributed to the presence of a trauma system because its impact was small and statistically not significant. Rather, the presence of a primary seat belt law and mean per capita income were associated with a reduction in occupant mortality rates, whereas rural population and speed limits faster than 65 mph were associated with an increase in mortality rates.15 As new trauma systems mature, more research will be needed to guide implementation of new system strategies to further reduce morbidity and mortality from traumatic injury.
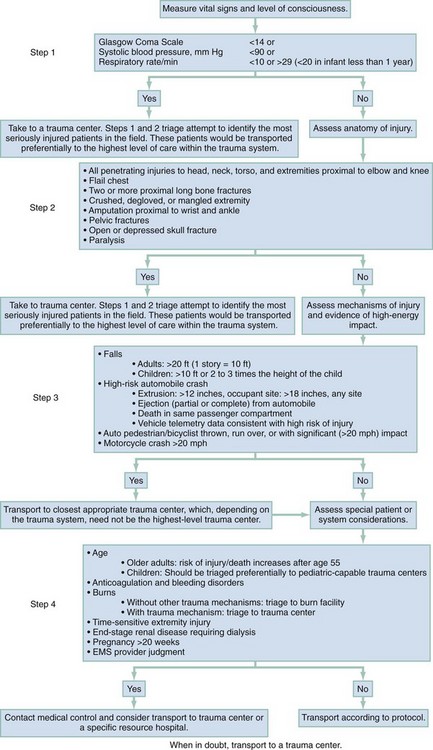
One goal of the out-of-hospital trauma system is to transport the patient to the closest appropriate facility in a timely manner. Problems with over-triage and under-triage occur. Most efforts are aimed at reducing under-triage (transport of severely injured patients to lower-level trauma centers), which may result in preventable morbidity and mortality owing to a delay in definitive care. Over-triage (transport of minimally injured patients to higher-level trauma centers) has no deleterious effects on patient care; however, it may contribute to unnecessary resource utilization and potential overcrowding in tertiary care, level 1 trauma centers. The Centers for Disease Control and Prevention (CDC) worked with experts in 2006 to establish the Field Triage Decision Scheme. Based on initial work by the ACS Committee on Trauma, this scheme outlines triage criteria to assist in proper triage of the injured patient (Fig. 36-1).16 The scheme is endorsed by the American College of Emergency Physicians, the ACS, and many other organizations.
Limitations to effective use of regionalized trauma systems remain. Hospital crowding, ambulance diversion, lack of specialist on-call availability, and reimbursement issues all contribute. In addition, from 1990 to 2009 the number of hospital emergency departments (EDs) in nonrural areas declined from 2446 to 1779. During this time, 1041 EDs closed and 374 hospitals opened EDs.17 Trends such as this increase the burden of emergency care on those remaining hospitals, potentially compromising care. Future funding and legislative decisions at the state and national levels will have a significant impact on the future of high-quality trauma care in the United States.
Principles of Disease
The emergency physician faces significant clinical uncertainty when a multiple trauma patient arrives in the ED. Much of the diagnostic dilemma and subsequent evaluation can be guided by knowledge of the mechanism of injury. Although mechanisms of injury alone are not good predictors of major trauma,18 common patterns of injuries can be anticipated and specifically assessed in ED patients. Table 36-1 outlines several blunt trauma mechanisms of injury with potential associated clinical findings.
Table 36-1
Blunt Trauma Mechanisms and Associated Injuries
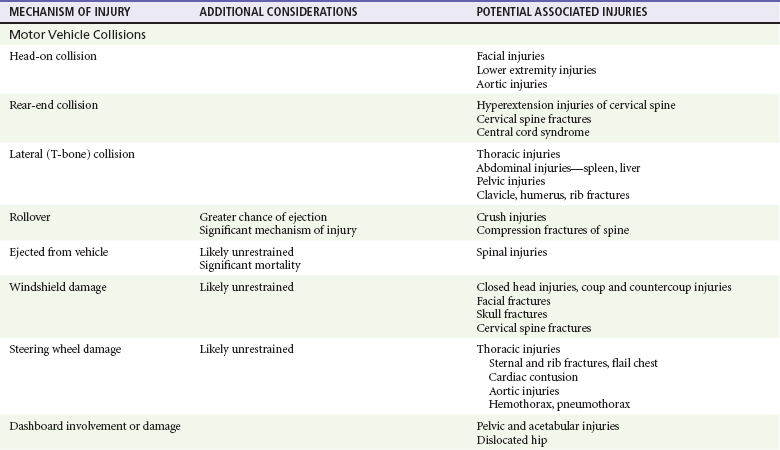
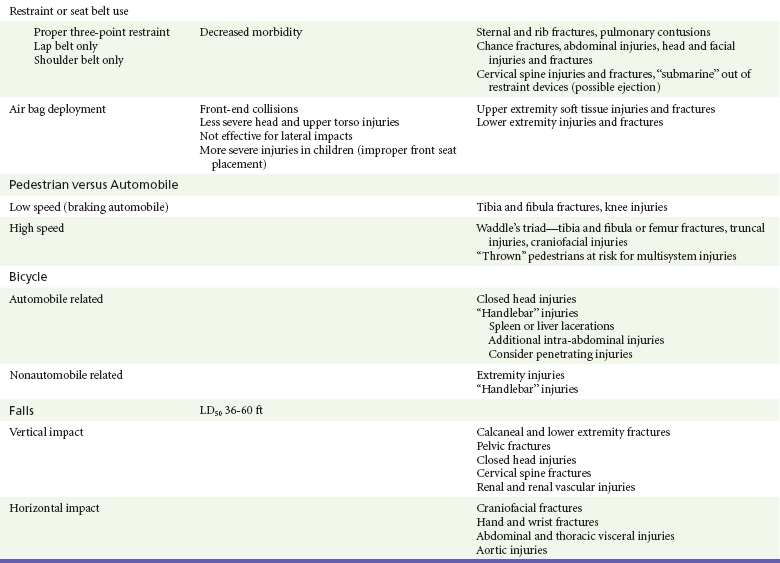
LD50, the height of fall that would be fatal for 50% of those falling.
Injury patterns can differ significantly between adults and children subjected to similar mechanisms of trauma. The major anatomic distinctions relate to the smaller size and surface area, larger head-to-body ratio, and less protected abdominal cavity of the child. As a result, children are more vulnerable to multisystem injury in blunt trauma, more frequently sustain significant head and intra-abdominal injuries, and are more at risk for hypothermia.15–18
Accidents were the fifth leading cause of death in 2009.2 Elder patients commonly sustain extremity, craniofacial, and closed head injuries. The majority of these occur as the result of a fall or an MVC. Elder trauma patients typically have normal, age-related changes in organ system function related to decreased cardiopulmonary functional reserve, decreased renal function, decreased bone density, and cerebral atrophy. These changes can increase susceptibility to shear forces and other aspects of trauma.19
Comorbidities and preexisting medication use further complicate the management of elder trauma patients. Lower extremity weakness, gait disturbances, decreased visual acuity, and the use of psychotropics, antihypertensives, and sedatives have been associated with falls in elders, resulting in major injury.20 The use of these medications, particularly antihypertensives, should not be considered causative in trauma patients with hypotension until acute hemorrhage has been assessed and managed. In addition, anticoagulants, antiplatelet drugs, and aspirin are commonly prescribed, and their effects should be suspected and reversed if possible in elder trauma patients.
Management
The majority of life-threatening injuries that require intervention by out-of-hospital providers are related to airway, breathing, and circulation (the ABCs). Preventing aspiration of gastric contents and providing adequate tissue oxygenation are the primary goals of endotracheal intubation. Although controversy exists regarding the use of out-of-hospital rapid sequence induction,21–27 securing an unprotected airway is essential in this phase of trauma management. Tension pneumothorax is the fundamental threat to adequate ventilation and requires immediate needle thoracostomy. Systemic hypotension with impaired end-organ perfusion necessitates treatment in the trauma patient, despite the debate surrounding controlled hypotension versus aggressive fluid resuscitation.
In the United States, rapid transport to the nearest appropriate facility is one of the fundamental concepts in trauma management. Much of the controversy regarding various out-of-hospital approaches to the ABCs is rooted in attempts to limit transport times and avoid further infringement on the “golden hour” of trauma care. In contrast, physician-operated emergency medical services (EMS) systems more aggressively manage airway and ventilatory issues and are more likely to commit out-of-hospital time resources to establishing hemodynamic stability before transport.28,29 Rural EMS systems in the United States, where transport times may be prolonged because of the distance to a receiving facility, may benefit from more advanced interventions, such as rapid sequence induction and intubation and more aggressive fluid resuscitative measures.
Emergency Department
For level 1 trauma centers, the ACS requires the presence of a surgeon or an appropriate representative (e.g., a fourth- or fifth-year surgery resident) to be present in the hospital 24 hours a day. The attending surgeon is expected to be present in the ED no later than 15 minutes after the ED arrival of trauma patients (Box 36-1).30 As the specialty of emergency medicine has evolved and the number of residency-trained and board-certified emergency physicians has increased, the need for a surgeon for all trauma patients has been increasingly debated; study has shown equivalent outcomes when the trauma team is led by either a surgeon or an emergency medicine physician.31–33 Optimal patient care is best provided in a collaborative, patient-centered manner.
The priorities in the treatment of trauma patients are similar to those for any other life-threatening condition. Securing the airway, maintaining ventilation, controlling hemorrhage, and treating shock are first priorities because of their crucial importance for survival. The emergency physician should give consideration to the worst possible injury and act accordingly until the diagnosis has been confirmed or excluded. The consequences of an overzealous evaluation are more acceptable than those of a missed injury. Based on ATLS, the phases of ED care are divided into the primary survey with interventions and adjuncts, consideration of transfer, the secondary survey and adjuncts, and continued monitoring and disposition.34
Primary Survey
Airway and Breathing.: Proper assessment and management of airway, oxygenation, and ventilation in the trauma patient are of utmost importance but can be challenging. In a review of 44,404 trauma patient admissions and 2594 deaths, airway management was responsible for 16% of preventable errors likely contributing to trauma mortality.35 The goals of airway management are threefold: airway protection, adequate oxygenation, and adequate ventilation.
Airway protection is necessary in many trauma patients. Airway obstruction necessitates immediate intervention. Obstruction from debris, blood, or vomitus may be easily removed with suction. Neck or facial trauma may cause more complicated problems. Swelling, distorted anatomy, and hematoma formation may all contribute to impending obstruction. Early airway control is safest because these conditions may rapidly worsen. Inability to adequately protect the airway, such as in patients with depressed levels of consciousness, is another indication for intervention. Airway control is recommended in patients with significant head injury (Glasgow Coma Scale [GCS] score below 9).36 Low GCS scores from intoxication, and not injury, may not necessitate intubation, as loss of airway reflexes cannot be predicted by GCS alone in this group.37
As a general rule, all trauma patients should be placed on supplemental oxygen. Adequate oxygenation has a direct effect on outcome of many trauma patients. In head-injured patients, hypoxia and extreme hyperoxia in both out-of-hospital and hospital phases of resuscitation have been associated with poorer outcomes.38–41 Hypoxia may also worsen outcome in spinal cord injury.42 Maintenance of arterial oxygen concentration (PaO2) above 60 mm Hg has been recommended.43 Inadequate ventilation, which may lead to respiratory acidosis, can be noted by the rate and quality of respirations. Signs of inadequate oxygenation may be more subtle and include agitation and restlessness. Assessment for injury that may compromise oxygenation, ventilation, or both requires careful inspection and auscultation of the chest. Signs of such compromising injury include increased work of breathing, tachypnea, penetrating wounds, flail segments, tracheal deviation, and distended neck veins. In determining the need for more aggressive airway management, these data are put into the context of the patient’s overall presentation. Certain ventilatory problems, such as pneumothorax or hemothorax, may require tube thoracostomy in addition to intubation. Early intervention is preferable in the tenuous patient.
Once the decision to intubate the patient has been made, many considerations are taken into account. If the patient’s condition allows, a brief neurologic examination before paralytics can be helpful in determining the extent of injury. Also, cervical spine injury precautions should be considered for patients with blunt trauma and gunshot wounds to the neck. Rapid sequence induction and orotracheal intubation with in-line cervical stabilization provide a safe method. There have been no reported cases of spinal cord injury from orotracheal intubation if proper stabilization has been applied.44 There are many approaches to airway control, and many alternative devices, such as video-assisted laryngoscopy, the flexible fiberoptic scope, and the intubating laryngeal mask airway, are now available to assist in intubation. In particular, video-assisted laryngoscopy causes less cervical spine motion and results in improved vocal cord view when compared with direct laryngoscopy.45,46 However, the choice will be based on clinical scenario and physician comfort. Nasotracheal intubation is generally undesirable in trauma patients owing to the lower success rate36 and higher complication rate47 than that for orotracheal intubation, the potential for abrupt rises in intracranial pressure, and the relative contraindications of severe midface trauma or severe basilar skull fracture.
Surgical airways are indicated in cases of failure of or contraindication to orotracheal or nasotracheal intubation. Cricothyrotomy is the preferred method, although it is performed in less than 0.5% of cases.48 Given the rarity of use, we recommend the use of the four-step method described by Brofeldt and colleagues, either with or without a bougie.49,50 A variety of devices for percutaneous cricothyrotomy are also available that show good success rates and are easy to use.51–53 If there is any question about the ability to identify the cricothyroid membrane, the traditional surgical approach with a vertical incision should be used.
Circulation.: Assessment of hemodynamics and circulatory status is of critical importance after the airway has been evaluated and controlled and adequate ventilation has been ensured. The assessment of circulation is multidimensional. Clinical indicators of adequate perfusion include mental status, skin color and temperature, heart rate, blood pressure, and capillary refill. A normal finding for any single sign does not rule out shock. Mental status changes associated with hypoperfusion can include anxiety, agitation, or sedation. Cool, pale skin or extremities with delayed capillary refill suggest inadequate perfusion and shock. A normal heart rate, blood pressure, or both can be present despite significant hemorrhage. Conversely, tachycardia may be seen without evidence of significant volume loss.
Control of external hemorrhage is crucial. Traditionally, direct pressure to external bleeding sites has been advocated, and the use of tourniquets has been discouraged. The use of direct pressure on the bleeding site remains first-line therapy; recent data have suggested the more liberal use of tourniquets for massive extremity bleeding that is not easily controlled.54–57 Similarly, recent studies of newer hemostatic agents have shown potential application in both combat and out-of-hospital settings.58–60
Intravenous access is required early in the assessment of circulation. Two large-bore (14- or 16-gauge) intravenous catheters are recommended. Routine intravenous access may be difficult or unobtainable in certain cases. Intraosseous vascular access can be obtained rapidly in both pediatric61 and adult62 patients and allows the safe infusion of large amounts of fluid or blood products. Compact, battery-operated intraosseous drills have recently been introduced. Ultrasound-guided peripheral venous access by both nurses and physicians should be considered in patients when blind peripheral attempts are unsuccessful.63,64 Central venous access may also be indicated in the appropriate clinical scenario or based on physician discretion. The use of ultrasound has been shown to increase successful vein cannulation and decrease complications in the placement of central venous lines.65–68 Central venous pressure measurements may be used to direct resuscitative efforts but should not delay definitive care.
The choice of fluids for resuscitation includes crystalloid, colloid, and blood products. Fluid replacement is generally based on a 3 : 1 ratio of fluids to blood loss. There are few clinically significant differences between lactated Ringer’s and normal saline. The debate regarding the choice of fluid for resuscitation is ongoing. No indisputable advantages of colloids have been demonstrated. Therefore the less expensive and more readily available crystalloids are the routine mainstay as first line of therapy. No clear benefit to the use of hypertonic saline has been established.69–72 Current ATLS guidelines standardize the ratio of replacement fluids to loss and recommend 2 L of crystalloid be infused in all patients in shock, followed by blood products. O-positive blood should be used except in women of childbearing age. Type-specific blood should be used when available, but emergent transfusion should not be delayed. The use of the antifibrinolytic agent tranexamic acid has been shown to decrease mortality in trauma patients at risk of major bleeding.73,74
The concept of “permissive hypotension” is based on the concern that resuscitation to normal blood pressures may increase bleeding from a site that is contained and not actively hemorrhaging.75 Clinically, restoration of normal blood pressure is delayed until active bleeding foci have been ruled out. Although data exist to support this strategy,75,76 a Cochrane review of the six available clinical trials meeting inclusion criteria did not support (or disprove) the use of early or larger-volume intravenous fluids in uncontrolled bleeding.77 Permissive hypotension is contraindicated in the management of traumatic brain injury because of the risk of hypoperfusion.78,79
The extended focused abdominal sonography in trauma (eFAST) examination should be performed on all patients as an adjunct to the assessment of circulation. The presence or absence of free intra-abdominal, intrathoracic, or intrapelvic hemorrhage or pneumothorax diagnosed by ultrasound will direct the management of trauma patients. Pericardial effusions or tamponade can be readily identified. In addition, ultrasound evaluation of the inferior vena cava may be useful in the overall assessment of fluid status in resuscitation.80–85
Disability.: A rapid assessment of the patient’s neurologic status is necessary early in the ED course. The GCS score is commonly used (see Chapter 41).
Exposure.: The final phase of the primary survey is completely undressing the patient to assess for inconspicuous injuries. Special attention to the axilla, perineum, and skin folds is needed. Preventing hypothermia is essential in this phase. Blankets, warming lights, and warm fluids may be used as indicated.
Secondary Survey
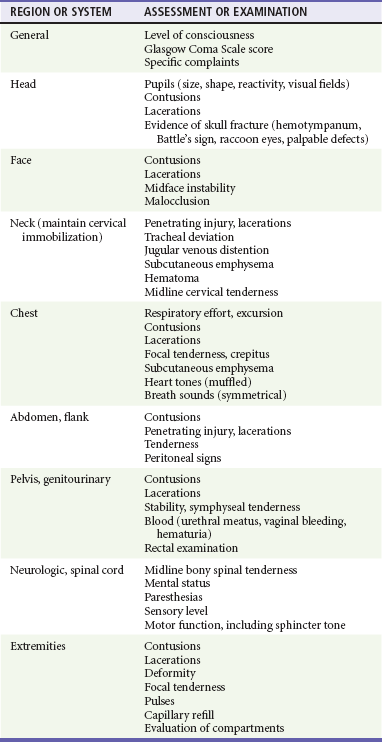
The goals of the secondary survey are to obtain pertinent historical data about the patient and injury as well as evaluate and treat injuries not found on the primary survey. An AMPLE (allergies, medications, past medical history, last meal, environments and events) history should be obtained. Frequent reassessment of the ABCs throughout the ED phase of management is necessary. If deterioration occurs, a complete reevaluation of the primary survey should be initiated. Features of the secondary survey and management are listed in Table 36-2.
Pitfalls
The goal of trauma management in the ED is to provide lifesaving interventions and evaluate for injuries. The tenets of ATLS provide a structured approach to ensure a thorough assessment is performed. Because multiple trauma patients have a variety of injuries from varying mechanisms, the initial focus is directed at defining the most serious pathology. The emergency physician should be aware of potential pitfalls. Studies from large trauma centers have shown that preventable deaths frequently result from human error and are related to the inability to intubate or secure the airway; delayed control of thoracic, abdominal, and pelvic hemorrhage; and several inpatient factors.35,86 Head-injured, unconscious, and intubated patients frequently have injuries that are not identified early in their hospital course.87–89 More aggressive diagnostics may be indicated in this subset of patients when history and patient-specific complaints are not obtainable. When cervical radiography is indicated, it is essential that the imaging obtained be complete and adequate. Limited radiographic series and inadequate cervical spine imaging have been shown to result in missed or delayed diagnosis of injuries.90,91
Radiographic Evaluation
Imaging of the cervical spine can usually be delayed; however, in a patient with neurologic findings and persistent moderate hypotension (e.g., 70 mm Hg), neurogenic shock should be considered. A positive finding on C-spine imaging (e.g., fracture, soft tissue swelling, and subluxation) may confirm this if other causes of hypotension have been ruled out. A single cross-table lateral cervical radiograph is not adequate to fully assess the cervical spine; in trauma patients, the sensitivity is too low to rule out fracture.92,93
Imaging of the cervical spine in trauma patients is a topic of some controversy. Radiographs are not necessary in all trauma patients.94 The NEXUS (National Emergency X-Radiography Utilization Study) criteria allow clinical clearance of the cervical spine in patients without posterior midline tenderness, focal neurologic deficit, altered mental status, intoxication, or distracting injury.95 The Canadian C-spine rule uses a different set of criteria and, although more complex, has higher specificity and therefore allows the elimination of a higher percentage of unnecessary x-ray studies.96 In a patient with a concerning mechanism of injury or physical examination findings, computed tomography (CT) scanning is more efficient and effective than plain radiography.92 However, routine use of CT scan in all post–blunt trauma patients is associated with higher cost and radiation dose. An algorithm to help determine which blunt trauma patients should undergo CT versus plain radiography to screen for cervical spine fracture was shown to have a 100% negative predictive value for cervical spine fracture.97,98 This algorithm combines the NEXUS criteria,95 the Canadian Head CT rule,99 and Hanson’s high-risk criteria.100 If plain radiography is used, three views of the cervical spine (lateral, anteroposterior, and odontoid) should be obtained.101
Imaging studies of the thoracolumbar spine and extremities can also be delayed until higher-priority assessments and interventions are complete. Once the patient has been stabilized, the clinical examination can direct whether additional radiographic examinations are necessary. If CT is performed, reformatted sagittal and coronal images will be more sensitive than axial images alone.102
Imaging of the thorax early in the evaluation of the trauma patient can give important information about potentially life-threatening injuries. However, the dogmatic “chest x-ray (CXR) for all trauma patients” approach to radiographic evaluation of the chest has undergone some recent challenges. Plain radiography of the chest is considered an acceptable first screening modality. The sensitivity of chest x-ray examination alone, even in patients with normal physical examination findings, may be too low for its use as the primary screening tool to rule out injury to the mediastinum or a blunt aortic dissection,103,104 and the results of those radiographs likely do not affect decision-making.105 The combination of chest x-ray examination with abdominal and pelvic CT (already being performed in a number of these patients) may provide sufficient screening, thereby limiting thoracic CT to only those patients with significant worrisome injury mechanisms.106 Other preliminary evidence suggests that some patients may not require chest imaging.107,108 Ultrasound is gaining favor as the initial screening tool for pneumothorax and hemothorax because it shows better sensitivity and is more rapid than chest x-ray examination.109,110 One possible approach for initial screening of the blunt trauma patient with a significant mechanism of injury could be carried out by thoracic ultrasound to identify life-threatening pneumothorax or hemothorax that must be immediately managed, followed by abdominopelvic CT scan, chest CT scan, or both to further elucidate other injuries. In patients with penetrating thoracic injury, primary CT scan, rather than repeat chest x-ray examinations, can speed disposition.111 Cost and radiation considerations are, of course, taken into account.
Pelvic radiographs are useful in the severely injured trauma patient. Pelvic fractures can account for significant hemorrhage, and early recognition of fracture and closure of the pelvic space can mitigate hypotension in these patients. Although not validated in large multicenter studies, evidence suggests that pelvic radiographs may be omitted in patients without altered level of consciousness, and with no complaints of pelvic pain, pelvic tenderness on examination, distracting injury, or clinical intoxication.112,113 Smaller similar studies have suggested the same for pediatric patients.114 Stable patients undergoing CT scan of the abdomen and pelvis can be further evaluated by bone windows of the CT scan.
As mentioned previously, the eFAST examination should take place early in the evaluation of the trauma patient, ideally as part of the primary survey. A positive scan in hypotensive patients can identify, with good sensitivity, those in need of emergent laparotomy.115 In addition, valuable information regarding the presence or absence of pericardial effusion can be obtained. False-negative scans can occur with hollow viscus injuries or solid organ injuries without free fluid.116 A normal scan does not eliminate the need for further abdominal imaging in significantly injured patients.117 Further discussion and suggested algorithms are found in Chapter 46.
Laboratory Evaluation
Lactate and base deficit have both been used to measure adequacy of resuscitation and predict outcome in the trauma patient.118,119 New noninvasive methods, such as near-infrared spectroscopy, tissue oxygen saturation, and sublingual capnometry, have shown promise in assessing severity of shock and predicting multiorgan dysfunction and mortality.120–122 Following changes in the central venous oxygen saturation may also be worthwhile; low values in hemodynamically stabilized trauma patients have been shown to worsen outcome.123 Use of one of these objective markers can assist in ensuring proper resuscitation of these patients.
Special Considerations
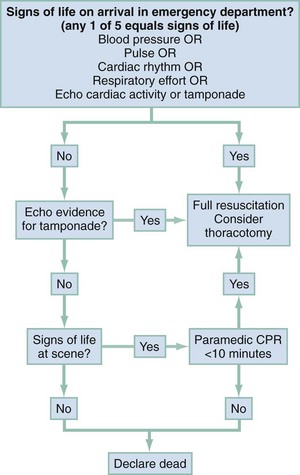
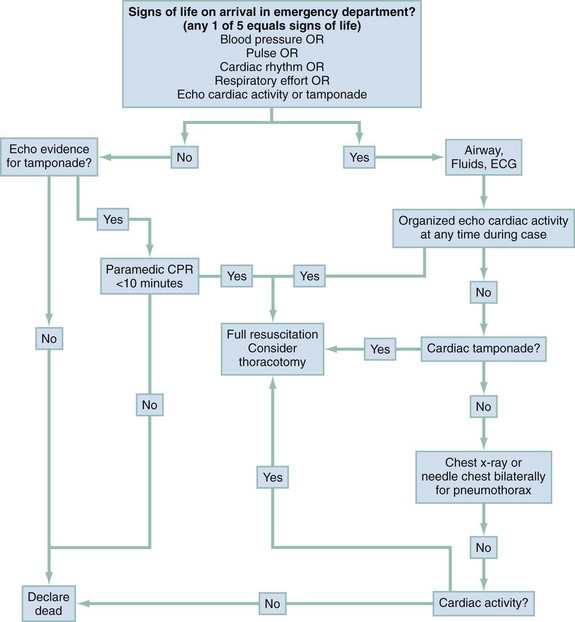
The role of ED thoracotomy (EDT) has become more selective to limit futile resuscitation efforts and minimize risk to providers. Patients with penetrating trauma who have cardiac arrest while in transport or the ED are most likely to benefit from EDT. In contrast, cardiac arrest patients with blunt trauma, prolonged cardiopulmonary resuscitation (CPR), or delayed transport times generally have dismal outcomes not altered by EDT.124–126 Most institutions have protocols in place outlining criteria regarding when EDT should be performed. The National Association of EMS Physicians and the ACS Committee on Trauma have published guidelines for withholding or terminating resuscitation efforts in out-of-hospital traumatic cardiac arrest patients. As a result, these guidelines often limit the transport of patients who would not likely benefit from EDT. Patients who may not be transported include any blunt trauma patient without vital signs at the scene, apneic or pulseless penetrating trauma victims without other signs of life, patients receiving more than 15 minutes of CPR, or patients with transport times of more than 15 minutes after arrest.127 Suggested algorithms for the application of EDT are outlined in Figures 36-2 and 36-3.
References
1. Nijboer, JM, van der Sluis, CK, van der Naalt, J, Nijsten, MW, Ten Duis, HJ. Two cohorts of severely injured trauma patients, nearly two decades apart: Unchanged mortality but improved quality of life despite higher age. J Trauma. 2007;63:670–675.
2. Kochanek, KD, et al. Deaths: Preliminary data for 2009. Natl Vital Stat Rep. 2011;59:29–30.
3. National Highway Traffic Safety System. Fatality Analysis Reporting System Encyclopedia. http://www-fars.nhtsa.dot.gov/, 2011.
4. National Highway Traffic Safety Administration. Traffic Safety Facts 2009. Washington, DC: National Highway Traffic Safety Administration; 2010.
5. Finkelstein, EA, Corso, PS, Miller, TR. Incidence and Economic Burden of Injuries in the United States. New York: Oxford University Press; 2006.
6. National Highway Traffic Safety Administration. Traffic Safety Facts: Lives Saved in 2009 by Restraint Use and Minimum-Drinking-Age Laws. Washington, DC: National Highway Traffic Safety Administration; 2010.
7. Pickrell, TM, Ye, TJ. Occupant Restraint Use in 2009—Results from the National Occupant Protection Use Survey Controlled Intersection Study. Washington, DC: National Highway Traffic Safety Administration; 2010.
8. National Highway Traffic Safety Administration. Traffic Safety Facts 2005: Children. Report No. DOT HS 810 618. Washington, DC:National Highway Traffic Safety Administration; 2006.
9. Solomon, MG, Chaffe, RHB, Cosgrove, LA. May 2004 Click It or Ticket Seat Belt Mobilization Evaluation. Washington, DC: National Highway Traffic Safety Administration; 2007.
10. Houten, RV, Hilton, B, Schulman, R, Reagan, I. Using Haptic Feedback to Increase Seat Belt Use of Service Vehicle Drivers. Washington, DC: National Highway Traffic Safety Administration; 2011.
11. Centers for Disease Control and Prevention. Violence-related firearm deaths among residents of metropolitan areas and cities—United States, 2006-2007. MMWR Morb Mortal Wkly Rep. 2011;60:573–578.
12. Committee on Trauma, American College of Surgeons. Optimal hospital resources for care of the seriously injured. Bull Am Coll Surg. 1976;61:15–22.
13. MacKenzie, EJ, et al. A national evaluation of the effect of trauma center care on mortality. N Engl J Med. 2006;354:366–378.
14. Celso, B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–378.
15. Shafi, S, Nathens, AB, Elliott, AC, Gentilello, L. Effect of trauma systems on motor vehicle occupant mortality: A comparison between states with and without a formal system. J Trauma. 2006;61:1374–1379.
16. Centers for Disease Control and Prevention. Guidelines for field triage of injured patients. MMWR Morb Mortal Wkly Rep. 2009;58:2–12.
17. Hsai, RY, Kellerman, AL, Shen, Y. Factors associated with closures of emergency departments in the United States. JAMA. 2011;305:1978–1985.
18. Boyle, MJ. Is mechanism of injury alone in the prehopital setting a predictor of major trauma—a review of the literature. J Trauma Manag Outcomes. 2007;1:4.
19. Aschkenasy, MT, Rothenhaus, TC. Trauma and falls in the elderly. Emerg Med Clin North Am. 2006;24:413–432.
20. Koski, K, Luukinen, H, Laippala, P, Kivela, SL. Physiological factors and medications as predictors of injurious falls by elderly people: A prospective population-based study. Age Ageing. 1996;25:29–38.
21. Bulger, EM, et al. An analysis of advanced prehospital airway management. J Emerg Med. 2002;23:183–189.
22. Wang, HE, Balasubramani, GK, Cook, LJ, Lave, JR, Yealy, DM. Out-of-hospital endotracheal intubation experience and patient outcomes. Ann Emerg Med. 2010;55:527–537.
23. Wang, HE, Cook, LJ, Chang, CC, Yealy, DM, Lave, JR. Outcomes after out-of-hospital endotracheal intubation errors. Resuscitation. 2009;80:50–55.
24. Davis, DP, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–453.
25. Poste, JC, et al. Air medical transport of severely head-injured patients undergoing paramedic rapid sequence intubation. Air Med J. 2004;23:36–40.
26. Gausche, M, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA. 2000;283:783–790.
27. Bernard, SA, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: A randomized controlled trial. Ann Surg. 2010;252:959–965.
28. Roudsari, BS, et al. Emergency medical services (EMS) systems in developed and developing countries. Injury. 2007;38:1001–1013.
29. Roudsari, BS, et al. International comparison of prehospital trauma care systems. Injury. 2007;38:993–1000.
30. Committee on Trauma, American College of Surgeons. Resources for the Optimal Care of the Injured Patient. Chicago: American College of Surgeons; 2006.
31. Green, SM. Is there evidence to support the need for routine surgeon presence on trauma patient arrival? Ann Emerg Med. 2006;47:413–414.
32. Moore, EE. Role of the acute care surgeon in the emergency department management of trauma. Ann Emerg Med. 2006;47:413–414.
33. Cummings, GE, Mayes, DC. A comparative study of designated trauma team leaders on trauma patient survival and emergency department length-of-stay. CJEM. 2007;9:105–110.
34. American College of Surgeons. Advanced Trauma Life Support for Doctors, 8th ed. Chicago: American College of Surgeons; 2008.
35. Gruen, RL, Jurkovich, GJ, McIntyre, LK, Foy, HM, Maier, RV. Patterns of errors contributing to trauma mortality: Lessons learned from 2,594 deaths. Ann Surg. 2006;244:371–380.
36. Dunham, CM, et al. Guidelines for emergency tracheal intubation immediately after traumatic injury. J Trauma. 2003;55:162–179.
37. Duncan, R, Thakore, S. Decreased Glasgow Coma Scale score does not mandate endotracheal intubation in the emergency department. J Emerg Med. 2009;37:451–455.
38. Miller, JD, Sweet, RC, Narayan, R, Becker, DP. Early insults to the injured brain. JAMA. 1978;240:439–442.
39. Spiotta, AM, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113:571–580.
40. Davis, DP, et al. Both hypoxemia and extreme hyperoxemia may be detrimental in patients with severe traumatic brain injury. J Neurotrauma. 2009;26:2217–2223.
41. Davis, DP, et al. The impact of hypoxia and hyperventilation on outcome after paramedic rapid sequence intubation of severely head-injured patients. J Trauma. 2004;57:1–8.
42. Yanagawa, Y, Marcillo, A, Garcia-Rojas, R, Loor, KE, Dietrich, WD. Influence of posttraumatic hypoxia on behavioral recovery and histopathological outcome following moderate spinal cord injury in rats. J Neurotrauma. 2001;18:635–644.
43. The Brain Trauma Foundation. The American Association of Neurological Surgeons. The Joint Section on Neurotrauma and Critical Care. Resuscitation of blood pressure and oxygenation. J Neurotrauma. 2000;17:471–478.
44. McGill, J. Airway management in trauma: An update. Emerg Med Clin North Am. 2007;25:603–622.
45. Turkstra, TP, Pelz, DM, Jones, PM. Cervical spine motion: A fluoroscopic comparison of the AirTraq laryngoscope versus the Macintosh laryngoscope. Anesthesiology. 2009;111:97–101.
46. Serocki, G, Bein, B, Scholz, J, Dörges, V. Management of the predicted difficult airway: A comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur J Anaesthesiol. 2010;27:24–30.
47. Dronen, SC. A comparison of blind nasotracheal and succinylcholine-assisted intubation in the poisoned patient. Ann Emerg Med. 1987;16:650.
48. Stephens, CT, Kahntroff, S, Dutton, RP. The success of emergency endotracheal intubation in trauma patients: A 10-year experience at a major adult trauma referral center. Anesth Analg. 2009;109:866–872.
49. Brofeldt, BT, Panacek, EA, Richards, JR. An easy cricothyrotomy approach: The rapid four-step technique. Acad Emerg Med. 1996;3:1060–1063.
50. Hill, C, Reardon, R, Joing, S, Falvey, D, Miner, J. Cricothyrotomy technique using gum elastic bougie is faster than standard technique: A study of emergency medicine residents and medical students in an animal lab. Acad Emerg Med. 2010;17:666–669.
51. Mouadeb, DA, Rees, CJ, Belafsky, PC. Utilization of the LifeStat emergency airway device. Ann Otol Rhinol Laryngol. 2008;117:1–4.
52. Melker, JS, Gabrielli, A. Melker cricothyrotomy kit: An alternative to the surgical technique. Ann Otol Rhinol Laryngol. 2005;114:525–528.
53. Fikkers, BG, van Vugt, S, van der Hoeven, JG, van den Hoogen, FJ, Marres, HA. Emergency cricothyrotomy: A randomised crossover trial comparing the wire-guided and catheter-over-needle techniques. Anaesthesia. 2004;59:1008–1011.
54. Doyle, GS, Taillac, PP. Tourniquets: A review of current use with proposals for expanded prehospital use. Prehosp Emerg Care. 2008;12:241–256.
55. Beekley, AC, et al. Prehospital tourniquet use in operation Iraqi Freedom: Effect on hemorrhage control and outcomes. J Trauma. 2008;63:S28–S37.
56. Kragh, JF, Jr., et al. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249:1–7.
57. Kragh, JF, Jr., et al. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma. 2008;64:S38–S50.
58. Cox, ED, Schreiber, MA, McManus, J, Wade, CE, Holcomb, JB. New hemostatic agents in the combat setting. Transfusion. 2009;49:248S–255S.
59. Achneck, HE, et al. A comprehensive review of topical hemostatic agents: Efficacy and recommendations for use. Ann Surg. 2010;251:217–228.
60. Granville-Chapman, J, Jacobs, N, Midwinter, MJ. Pre-hospital haemostatic dressings: A systematic review. Injury. 2011;42:447–459.
61. Guy, J, Haley, K, Zuspan, SJ. Use of intraosseous infusion in the pediatric trauma patient. J Pediatr Surg. 1993;28:158–161.
62. Greaves, I, Evans, G, Boyle, A. Intraosseous infusions in the adult. Trauma. 1999;1:291–299.
63. Mahler, SA, Wang, H, Lester, C, Conrad, SA. Ultrasound-guided peripheral intravenous access in the emergency department using a modified Seldinger technique. J Emerg Med. 2010;39:325–329.
64. White, A, Lopez, F, Stone, P. Developing and sustaining an ultrasound-guided peripheral intravenous access program for emergency nurses. Adv Emerg Nurs J. 2010;32:173–188.
65. Stone, MB, Nagdev, A, Murphy, MC, Sisson, CA. Ultrasound detection of guidewire position during central venous catheterization. Am J Emerg Med. 2010;28:82–84.
66. Balls, A, et al. Ultrasound guidance for central venous catheter placement: Results from the central line emergency access registry database. Am J Emerg Med. 2010;28:561–567.
67. Froehlich, CD, et al. Ultrasound-guided central venous catheter placement decreases complications and decreases placement attempts compared with the landmark technique in patients in a pediatric intensive care unit. Crit Care Med. 2009;37:1090–1096.
68. Leung, J, Duffy, M, Finckh, A. Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: A randomized, prospective study. Ann Emerg Med. 2006;48:540–547.
69. Bulger, EM, et al. Hypertonic resuscitation of hypovolemic shock after blunt trauma. Arch Surg. 2008;143:139–148.
70. Brod, VI, Krausz, MM, Hirsh, M, Adir, Y, Bitterman, H. Hemodynamic effects of combined treatment with oxygen and hypertonic saline in hemorrhagic shock. Crit Care Med. 2006;34:2784–2791.
71. Oda, J, et al. Hypertonic lactated saline resuscitation reduces the risk of abdominal compartment syndrome in severely burned patients. J Trauma. 2006;60:64–71.
72. Bernard, SS, Ponsford, J. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: A randomized controlled trial. JAMA. 2004;291:1350–1357.
73. CRASH-2 collaborators. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): A randomised, placebo-controlled trial. Lancet. 2010;376:23–32.
74. CRASH-2 collaborators. The importance of early treatment with tranexamic acid in bleeding trauma patients: An exploratory analysis of the CRASH-2 randomised controlled trial. Lancet. 2011;377:1096–1101.
75. Bickell, WH, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105–1109.
76. Dutton, RP, Mackenzie, CF, Scalea, TM. Hypotensive resuscitation during active hemorrhage: Impact on in-hospital mortality. J Trauma. 2002;52:1141–1146.
77. Kwan, I, Burn, F, Roberts, I. Timing and volume of fluid administration for patients bleeding following trauma (Cochrane review). In: The Cochrane Library. Oxford: Update Software; 2001.
78. Henzler, D, Cooper, DJ, Tremayne, AB, Rossaint, R, Higgins, A. Early modifiable factors associated with fatal outcome in patients with severe traumatic brain injury: A case control study. Crit Care Med. 2007;35:1027–1031.
79. Shutter, LA, Narayan, RK. Blood pressure management in traumatic brain injury. Ann Emerg Med. 2008;51:S37–S38.
80. Prekker, ME, et al. Ultrasound measurement of inferior vena caval diameter is more accurate than the internal jugular vein aspect ratio to estimate central venous pressure in ICU patients. Am J Respir Crit Care Med. 2010;181:A4580.
81. Fields, JM, et al. The interrater reliability of inferior vena cava ultrasound by bedside clinician sonographers in emergency department patients. Acad Emerg Med. 2011;18:98–101.
82. Avyazyan, S, et al. Ultrasound of the inferior vena cava can assess volume status in pediatric patients. J Emerg Med. 2009;37:219.
83. Yanagawa, Y, Nishi, K, Sakamoto, T, Okada, Y. Early diagnosis of hypovolemic shock by sonographic measurement of inferior vena cava in trauma patients. J Trauma. 2005;58:825–829.
84. Lyon, M, Blaivas, M, Brannam, L. Sonographic measurement of the inferior vena cava as a marker of blood loss. Am J Emerg Med. 2005;23:45–50.
85. Baumann, UA, et al. Estimation of central venous pressure by ultrasound. Resuscitation. 2005;64:193–199.
86. Teixeira, PGR, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007;63:1338–1347.
87. Thomson, CB, Greaves, I. Missed injury and the tertiary trauma survey. Injury. 2008;39:107–114.
88. Wurmb, TE, Frühwald, P, Hopfner, W, Roewer, N, Brederlau, J. Whole-body multislice computed tomography as the primary and sole diagnostic tool in patients with blunt trauma: Searching for its appropriate indication. Am J Emerg Med. 2007;25:1057–1062.
89. Enderson, BL, et al. The tertiary trauma survey: A prospective study of missed injury. J Trauma. 1990;30:666–670.
90. Hashem, R, Evans, CC, Farrokhyar, F, Kahnamoui, K. Plain radiography does not add any clinically significant advantage to multidetector row computed tomography in diagnosing cervical spine injuries in blunt trauma patients. J Trauma. 2009;66:423–428.
91. Rana, AR, Drongowski, R, Breckner, G, Ehrlich, PF. Traumatic cervical spine injuries: Characteristics of missed injuries. J Pediatr Surg. 2009;44:151–155.
92. Bailitz, J, et al. CT should replace three-view radiographs as the initial screening test in patients at high, moderate, and low risk for blunt cervical spine injury: A prospective comparison. J Trauma. 2009;66:1605–1609.
93. Mathen, R, et al. Prospective evaluation of multislice computed tomography versus plain radiographic cervical spine clearance in trauma patients. J Trauma. 2007;62:1427–1431.
94. Gonzalez, RP, Cummings, GR, Phelan, HA, Bosarge, PL, Rodning, CB. Clinical examination in complement with computed tomography scan: An effective method for identification of cervical spine injury. J Trauma. 2009;67:1297–1304.
95. Hoffman, JR, Mower, WR, Wolfson, AB, Todd, KH, Zucker, MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343:94–99.
96. Stiell, IG, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286:1841–1848.
97. Kokabi, N, Raper, DM, Xing, M, Giuffre, BM. Application of imaging guidelines in patients with suspected cervical spine trauma: Retrospective analysis and literature review. Emerg Radiol. 2011;18:31–38.
98. Goergen, SK, Fong, C, Dalziel, K, Fennessy, G. Can an evidence-based guideline reduce unnecessary imaging of road trauma patients with cervical spine injury in the emergency department? Australas Radiol. 2006;50:563–569.
99. Stiell, IG, et al. The Canadian CT head rule for patients with minor head injury. Lancet. 2001;357:1391–1396.
100. Hanson, JA, Blackmore, CC, Mann, FA, Wilson, AJ. Cervical spine injury: A clinical decision rule to identify high-risk patients for helical CT screening. AJR Am J Roentgenol. 2000;174:713–717.
101. West, OC, Anbari, MM, Pilgram, TK. Acute cervical spine trauma: Diagnostic performance of single-view versus three-view radiographic screening. Radiology. 1997;204:819–823.
102. Gross, EA. CT screening for thoracic and lumbar fractures: Is spine reformatting necessary? Am J Emerg Med. 2010;28:73–75.
103. Salim, A, et al. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: Results of a prospective study. Arch Surg. 2006;141:473–475.
104. Exadaktylos, AK, Sclabas, G, Schmid, SW, Schaller, B, Zimmermann, H. Do we really need routine computed tomographic scanning in the primary evaluation of blunt chest trauma in patients with “normal” chest radiograph? J Trauma. 2001;51:1173–1176.
105. Wisbach, GG, et al. What is the role of chest x-ray in the initial assessment of stable trauma patients? J Trauma. 2007;62:74–78.
106. Barrios, C, Jr., et al. Ability of a chest x-ray and an abdominal computed tomography scan to identify traumatic thoracic injury. Am J Surg. 2010;200:741–744.
107. Rodriguez, RM, Hendey, GW, Marek, G, Dery, RA, Bjoring, A. A pilot study to derive clinical variables for selective chest radiography in blunt trauma patients. Ann Emerg Med. 2006;47:415–418.
108. Traub, M, et al. The use of chest computed tomography versus chest x-ray in patients with major blunt trauma. Injury. 2007;38:43–47.
109. Wilkerson, RG, Stone, MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010;17:11–17.
110. McEwan, K, Thompson, P. Ultrasound to detect haemothorax after chest injury. Emerg Med J. 2007;24:581–582.
111. Magnotti, LJ, Weinberg, JA, Schroeppel, TJ, et al. Initial chest CT obviates the need for repeat chest radiograph after penetrating thoracic trauma. Am Surg. 2007;73:572–573.
112. Gross, EA, Neidens, BA. Validation of a decision instrument to limit pelvic radiography in blunt trauma. J Emerg Med. 2005;28:263–266.
113. Duane, TM, et al. Blunt trauma and the role of routine pelvic radiographs: A prospective analysis. J Trauma. 2002;53:463–468.
114. Ramirez, DW, Schuette, JJ, Knight, V. Necessity of routing pelvic radiograph in the pediatric blunt trauma patient. Clin Pediatr. 2008;47:935–940.
115. Lee, BC, Ormsby, EL, McGahan, JP, Melendres, GM, Richards, JR. The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol. 2007;188:415–421.
116. Shanmuganathan, K, Mirvis, SE, Sherbourne, CD, Chiu, WC, Rodriguez, A. Hemoperitoneum as the sole indicator of abdominal visceral injuries: A potential limitation of screening abdominal US for trauma. Radiology. 1999;212:423–430.
117. Gaarder, C, et al. Ultrasound performed by radiologists—confirming the truth about FAST in trauma. J Trauma. 2009;67:323–329.
118. Guyette, F, et al. Prehospital serum lactate as a predictor of outcomes in trauma patients: A retrospective observational study. J Trauma. 2011;70:782–786.
119. Mofidi, M, Hasani, A, Kianmehr, N. Determining the accuracy of base deficit in diagnosis of intra-abdominal injury in patients with blunt abdominal trauma. Am J Emerg Med. 2010;28:933–936.
120. Baron, BJ, et al. Sublingual capnometry for rapid determination of the severity of hemorrhagic shock. J Trauma. 2007;62:120–124.
121. Beekley, AC, et al. Continuous noninvasive tissue oximetry in the early evaluation of the combat casualty: A prospective study. J Trauma. 2010;69(Suppl 1):S14–S25.
122. Cohn, SM, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62:44–54.
123. Hosking, C, et al. Low central venous oxygen saturation in haemodynamically stabilized trauma patients is associated with poor outcome. Acta Anaesthesiol Scand. 2011;55:713–721.
124. Moore, EE, et al. Defining the limits of resuscitative emergency department thoracotomy: A contemporary Western Trauma Association perspective. J Trauma. 2011;70:334–339.
125. Rhee, PM, et al. Survival after emergency department thoracotomy: Review of published data from the past 25 years. J Am Coll Surg. 2000;190:288–298.
126. Branney, SW, Moore, EE, Feldhaus, KM, Wolfe, RE. Critical analysis of two decades of experience with postinjury emergency department thoracotomy in a regional trauma center. J Trauma. 1998;45:87–94.
127. Hopson, LR, et al. Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest: Joint position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. J Am Coll Surg. 2003;196:106–112.