Chapter 58 Multiple Trauma
1 What is the importance of trauma to the health of children?
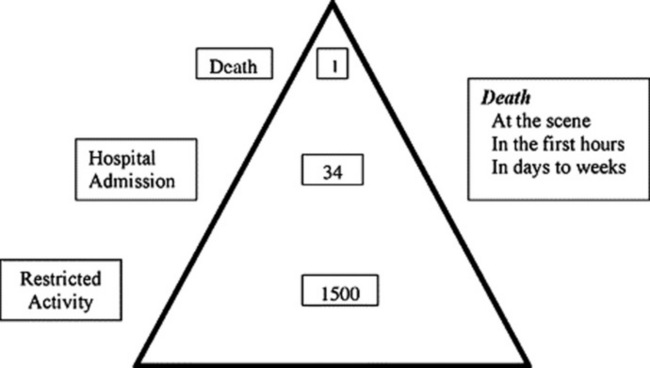
Injury is the leading cause of death in children older than 1 year (Fig. 58-1). Although injury death rates in the U.S. population have declined since 1991 (except for 2001 because of September 11), trauma is still the number one killer of children. Most injury is responsible for intermediate morbidity, with significant impact on the functioning of children and their progress to adulthood. Trauma is responsible for about 22,000 deaths per year in children age 19 years and younger. The number of permanently disabled may approach over 100,000 per year. Hospital admissions in the 0–14 age group for trauma is estimated to exceed 250,000 per year (> 51/100,000 population).
Centers for Disease Control and Prevention: National Vital Statistics Report. Deaths: Preliminary data for 2002: www.cdc.gov/nchs/data/nvsr/nvsr53/nvsr53_15.pdf
Centers for Disease Control and Prevention, National Center for Health Statistics. National trends in injury hospitalizations: 1971–2001: www.cdc.gov/nchs/data/injury/InjuryChartbook79–01.pdf
2 What specific mechanisms of injury are seen typically in children?
 Motor vehicle-related crashes are the leading cause of death from injuries in children, both as passengers and as pedestrians struck.
Motor vehicle-related crashes are the leading cause of death from injuries in children, both as passengers and as pedestrians struck.
 Drowning is the second leading cause of pediatric injury death in most areas.
Drowning is the second leading cause of pediatric injury death in most areas.
 Deaths from burns and smoke inhalation have declined but remain third.
Deaths from burns and smoke inhalation have declined but remain third.
 Mortality rates (%) are highest for gunshot wounds, especially in teens, but also in the young.
Mortality rates (%) are highest for gunshot wounds, especially in teens, but also in the young.
 Falls are the most common mechanism; severity of injury is minor except in falls greater than 10–20 feet.
Falls are the most common mechanism; severity of injury is minor except in falls greater than 10–20 feet.
Centers for Disease Control and Prevention: Web-based Injury Statistics Query and Reporting System: www.cdc.gov/ncipc/wisqars/
KEY POINTS: THE CHALLENGE OF PEDIATRIC TRAUMA
1 “Multiple trauma” is injury to two or more body areas.
2 Patients with severe head injuries are at high risk of poor outcome or death.
3 Lack of cooperation with examination due to age or fear, initially occult injuries, altered mental status due to alcohol or illicit substances, and nonaccidental trauma may interfere with rapid determination of isolated versus multiple trauma.
4 Describe the prehospital care capability for children with potentially serious injuries
KEY POINTS: ABNORMAL VITAL SIGNS IN THE INJURED CHILD
1 Tachycardia in an injured patient may be due to pain or loss of blood volume.
2 Carefully evaluate the tachycardic trauma patient for the possibility of compensated shock.
3 An older child in compensated shock may be deceivingly responsive and alert.
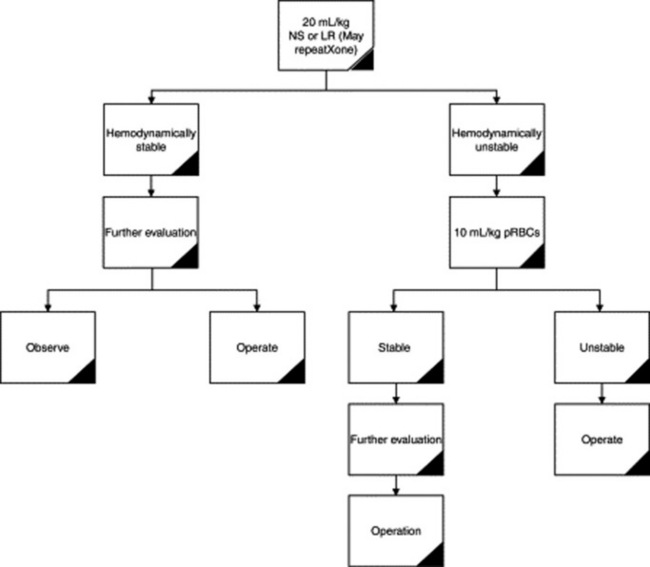
4 Shock in the trauma patient should be treated with a 20-mL/kg bolus of normal saline or lactated Ringer’s solution, which should be repeated once if shock persists.
5 If the patient is refractory to treatment with crystalloid, rapidly infuse packed red cells and emergently seek operative intervention.
5 Describe the initial approach to children with potentially serious injuries
 Airway management with cervical spine control
Airway management with cervical spine control
 Breathing: Maximize oxygen delivery
Breathing: Maximize oxygen delivery
 Circulation: Establish vascular access, control external hemorrhage, and restore circulatory volume
Circulation: Establish vascular access, control external hemorrhage, and restore circulatory volume
 Disability: Assess potentially critical injury to the central nervous system
Disability: Assess potentially critical injury to the central nervous system
 Exposure: Visualize every part of the patient to assess for injury and control body temperature (especially important in young infants and children)
Exposure: Visualize every part of the patient to assess for injury and control body temperature (especially important in young infants and children)
7 Is hypertonic saline beneficial in the fluid resuscitation of the multiply injured trauma patient with severe head injury?
9 What components of the neurologic examination should be conducted during the primary and secondary surveys?
11 Discuss the uses and complications of medical antishock trousers or pneumatic antishock garments in children
13 Describe the presentation and treatment of tension pneumothorax. Define open pneumothorax. How is it managed?
14 In a child who has suffered blunt abdominal trauma, what class of hemorrhage results in diminished pulse pressure, prolonged capillary refill, and normal systolic blood pressure?
15 What is the “3-for-1” rule in trauma fluid resuscitation?
The 3-for-1 rule is a rough guideline for the total amount of crystalloid required in the acute management of hypovolemia. Each milliliter of lost blood should be replaced with 3 mL of crystalloid fluid. This amount allows replacement of plasma volume lost into the interstitial space. The patient’s response to fluid therapy remains the most important guideline for further fluid resuscitation (Fig. 58-2).
16 Which visceral injuries are more common in children?
KEY POINTS: PITFALLS IN RESUSCITATION OF INJURED CHILDREN
1 Failure to recognize impending respiratory failure or potential airway obstruction
2 Failure to recognize early shock when the patient has a “normal” blood pressure with other signs of hemorrhage (e.g., tachycardia, delayed capillary refill, diaphoresis, altered mental status)
3 Failure to recognize impending neurologic deterioration from unsuspected head injury
17 True or false: To open the airway in a pediatric trauma patient, the head-tilt chin-lift maneuver is the recommended procedure
18 What are the factors that may interfere in the detection of multiple injuries in the pediatric patient?
23 How might airbags and pediatric restraint devices in vehicles influence motor vehicle crash-related injuries?
American Academy of Pediatrics: Car safety seats: A guide for families 2007: www.aap.org/family/carseatguide.htm
National Highway Traffic Safety Administration: www.nhtsa.dot.gov
26 What is the most likely injury in a child with blunt head trauma and no evidence of external bleeding who presents with signs of shock?
31 When a trauma patient requires transfer to a trauma center, what are the responsibilities of the transferring physician?
 Identification of the patient requiring transfer
Identification of the patient requiring transfer
 Initiation of the transfer process via phone contact with the receiving doctor
Initiation of the transfer process via phone contact with the receiving doctor
 Maximal stabilization using the capabilities of the local institution
Maximal stabilization using the capabilities of the local institution
 Determination of the best mode of transport
Determination of the best mode of transport
 Assurance that the level of care remains stable and does not deteriorate
Assurance that the level of care remains stable and does not deteriorate
 Transfer of all relevant records, results, and radiographs to the receiving facility
Transfer of all relevant records, results, and radiographs to the receiving facility
1 Advanced Trauma Life Support for Doctors. Student Manual. Chicago: American College of Surgeons, 1997. 2005
2 Tepas IIIJJ, Fallat ME, Moriarty TM. Trauma. In: Gausche-Hill M, Fuchs S, Yamamoto L, editors. APLS: The Pediatric Emergency Medicine Course. 4th ed. Dallas: American College of Emergency Physicians, American Academy of Pediatrics; 2004:268-323.
3 Trauma. In: Dieckman RA, editor. Pediatric Education for Prehospital Professionals (PEPP). Elk Grove Village, IL: American Academy of Pediatrics; 2000:129-155.
4 Trauma resuscitation and spinal immobilization. In: Zaritsky AL, Nadkarni VM, Hickey RW, Schexnayder SM, Berg RA, editors. Pediatric Advanced Life Support. Dallas: American Academy of Pediatrics, American Heart Association; 2002:253-286.