CHAPTER 28 Multiple-Ligament Knee Injuries and Management of Knee Dislocations
The combined anterior cruciate ligament–posterior cruciate ligament (ACL-PCL) injured (dislocated) knee is a severe injury that can result from high- or low-energy trauma. Both cruciates are torn, plus one or both collateral ligament complexes. The frequency of popliteal artery injuries occurs with the same frequency in bicruciate knee ligament injuries and frank tibiofemoral dislocations. Nerve injuries, associated fractures, other structural injuries, functional instability, and post-traumatic arthrosis may all occur with this injury complex.1,2
ANATOMY
Knee dislocations can be classified by the direction of tibial displacement, anatomic classification, open or closed injury status, and the energy level associated with the knee dislocation.3 Hyperextension of the tibiofemoral joint leads to anterior tibiofemoral dislocation. This mechanism may result in popliteal artery stretch, leading to intimal arterial damage, delayed thrombus formation, and ultimate arterial occlusion. The dashboard knee mechanism of injury leads to abrupt posterior tibial dislocation with the knee at 90 degrees of flexion, and may result in arterial transection. Varus force inducing tibiofemoral dislocation may result in peroneal nerve injury.1–3
PATIENT EVALUATION
History and Physical Examination
Initial evaluation of the acute bicruciate ligament injured knee includes evaluation of the deformity, location of abrasions or contusions, neurovascular status of the extremity, and presence or absence of a dimple sign. The presence of normal pulses, normal Doppler, and normal capillary refill in the presence of a reduced bicruciate (dislocated) knee does not guarantee the absence of vascular injury. Serial physical examinations, ankle brachial indices, and arteriography all must be used as necessary to document intact arterial circulation to the injured lower extremity.4–19
TREATMENT
Indications and Contraindications
The current consensus indicates that surgical treatment yields better results than nonsurgical treatment of the multiple-ligament injured knee.20–25 Technical advancements in the procurement, processing, and use of allograft tissue, arthroscopic surgical instruments, graft fixation methods, and improved surgical techniques, and an improved understanding of the ligament structures and the biomechanics of the knee, have led to more predictable and successful results in the treatment of these complex knee injuries. Various studies have published excellent results with return to preinjury level of function documented with physical examination, arthrometer measurements, knee ligament rating scales, and stress radiography.2,26–33
Arthroscopic Technique
Surgical Timing
Surgical timing in the acute bicruciate multiple-ligament injured knee is dependent on the vascular status of the involved extremity, collateral ligament injury severity, degree of instability, and postreduction stability. Delayed or staged reconstruction of 2 to 3 weeks postinjury has demonstrated a lower incidence of arthrofibrosis.30,31
Surgical timing in acute ACL-PCL lateral side injuries is dependent on the lateral side classification.34 We have described three types of posterolateral instability, A, B, and C.34 Posterolateral instability (PLI) type A has increased external rotation only, corresponding to injury to the popliteofibular ligament and popliteus tendon. PLI type B presents with increased external rotation and mild varus of approximately 5 to 10 mm, with increased lateral joint line opening to varus stress at 30 degrees of knee flexion. This occurs with damage to the popliteofibular ligament and popliteus tendon, and attenuation of the fibular collateral ligament. PLI type C presents with increased tibial external rotation and varus instability of 10 mm more than the normal knee tested at 30 degrees of knee flexion with varus stress. This occurs with injury to the popliteofibular ligament, popliteus tendon, fibular collateral ligament, and lateral capsular avulsion in addition to cruciate ligament disruption. The intact medial collateral ligament, tested with valgus stress at 30 degrees of knee flexion, is the stable hinge in the ACL-PCL- posterolateral corner (PLC)–injured knee.
Surgical timing in acute ACL-PCL medial side injuries is also dependent on the medial side classification. Some medial side injuries will heal with 4 to 6 weeks of brace treatment, provided that the tibiofemoral joint is reduced in all planes. Other medial side injuries require surgical intervention. Types A and B medial side injuries are repaired or reconstructed as a single-stage procedure with combined arthroscopic ACL-PCL reconstruction. Type C medial side injuries combined, with ACL-PCL tears are often treated with staged reconstruction. The medial posteromedial repair or reconstruction is performed within the first week after injury, followed by arthroscopic combined ACL-PCL reconstruction 3 to 6 weeks later.1,2,30,31,35,36
Surgical timing may be affected by factors beyond the surgeon’s control, and may cause the surgical treatment to be performed earlier or later than desired. These include injured extremity vascular status, open or closed injury, reduction stability, skin conditions, multiple system injuries, other orthopedic injuries, and meniscal and articular surface injuries.1,2
Patient Positioning
When there is a posterior cruciate ligament tear, the tear of the PCL is identified and the intact anterior cruciate ligament is confirmed. The residual stump of the posterior cruciate ligament is débrided with the synovial shaver and hand tools, as necessary. In the case of a combined ACL-PCL injury, the residual stumps of both the anterior and posterior cruciate ligaments are débrided. In patients with combined ACL-PCL injuries, the notchplasty for the ACL portion of the procedure is performed at this time.
Initial Incision
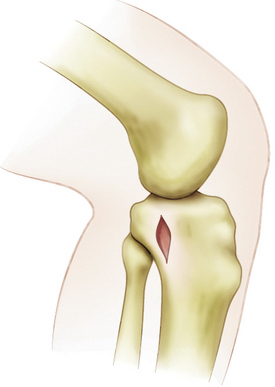
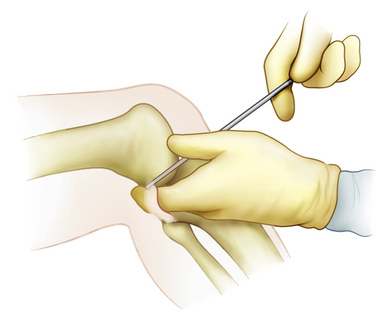
An extracapsular extra-articular posteromedial safety incision is made by creating an incision approximately 1.5 to 2 cm long, starting at the posteromedial border of the tibia approximately 1 inch below the level of the joint line and extending distally (Fig. 28-1). Dissection is carried down to the crural fascia, which is incised longitudinally. Care is taken to protect the neurovascular structures. An interval is developed between the medial head of the gastrocnemius muscle posterior and the capsule of the knee joint anterior. The surgeon’s gloved finger is able to position the neurovascular structures posterior to the finger and the capsule anterior to the finger (Fig. 28-2). In this way, the surgeon can monitor tools such as the over the top PCL instruments and the PCL-ACL drill guide as it is positioned in the posterior aspect of the knee. This also allows for accurate placement of the guide wire in medial lateral and proximal distal directions. The PCL and ACL reconstructions are performed with the knee in approximately 70 to 90 degrees of knee flexion.
Elevating the Capsule.
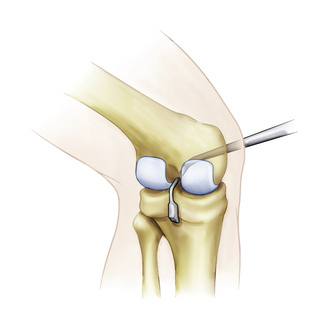
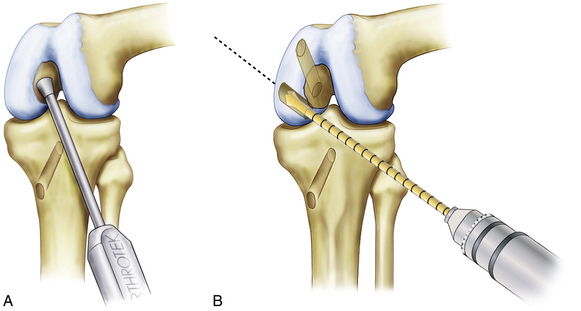
The curved over the top PCL instruments are used to lyse adhesions in the posterior aspect of the knee sequentially and elevate the capsule from the tibial ridge posteriorly. This will allow accurate placement of the drill guide and correct placement of the tibial tunnel (Fig. 28-3).
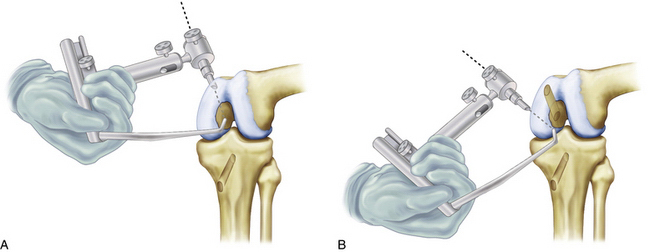
Positioning of the Guide
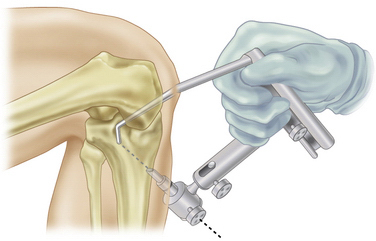
The arm of the PCL-ACL guide is inserted through the inferior medial patellar portal. The tip of the guide is positioned at the inferior lateral aspect of the PCL anatomic insertion site. This is below the tibial ridge posterior and in the lateral aspect of the PCL anatomic insertion site. The bullet portion of the guide contacts the anteromedial surface of the proximal tibia at a point midway between the posteromedial border of the tibia and the tibial crest anterior, approximately 1cm below the tibial tubercle (Fig. 28-4). This will provide an angle of graft orientation so that the graft will turn two very smooth 45-degree angles on the posterior aspect of the tibia and will not have an acute 90-degree angle turn, which may cause pressure necrosis of the graft. The tip of the guide, in the posterior aspect of the tibia, is confirmed with the surgeon’s finger through the extracapsular extra-articular posteromedial safety incision. Intraoperative anteroposterior (AP) and lateral x-rays may also be used. When the PCL-ACL guide is positioned in the desired area, a blunt spade-tipped guide wire is drilled from anterior to posterior. The arthroscope, in the posterior medial portal, visualizes the tip of the guide wire. The surgeon’s finger confirms the position of the guide wire through the posterior medial safety incision. This is a double safety check.
Tunnel Drilling
Drilling the Femoral Tunnel Outside-In: Single- and Double-Bundle Posterior Cruciate Ligament Reconstruction.
The PCL-ACL drill guide is positioned to create the femoral tunnel. The arm of the guide is introduced through the inferomedial patellar portal and is positioned so that the guide wire will exit through the center of the stump of the anterior lateral bundle of the posterior cruciate ligament (Fig. 28-5A). The blunt spade-tipped guide wire is drilled through the guide and, just as it begins to emerge through the center of the stump of the PCL anterior lateral bundle, the drill guide is disengaged. The accuracy of the placement of the wire is confirmed arthroscopically with probing and visualization. Care must be taken to ensure that the patellofemoral joint has not been violated by arthroscopically examining the patellofemoral joint prior to drilling. The appropriately sized standard cannulated reamer is used to create the femoral tunnel. A curette is used to cap the tip of the guide wire so that there is no inadvertent advancement of the guide wire, which could damage the anterior cruciate ligament or articular surface. As the reamer is about to penetrate interiorly, the reamer is disengaged from the drill and the final reaming is completed by hand. This adds an additional margin of safety. The reaming debris is evacuated with a synovial shaver to minimize any fat pad inflammatory response, with a subsequent risk of arthrofibrosis. The tunnel edges are chamfered and rasped.
When the double-bundle PCL reconstruction is performed, the PCL-ACL drill guide is positioned to create the second femoral tunnel. The arm of the guide is introduced through the inferior medial patellar portal and is positioned so that the guide wire will exit through the center of the stump of the posterior medial bundle of the PCL (see Fig. 28-5B). The blunt spade-tipped guide wire is drilled through the guide and, just as it begins to emerge through the center of the stump of the PCL posterior medial bundle, the drill guide is disengaged. The accuracy of the placement of the wire is confirmed arthroscopically with probing and visualization. Care must be taken to ensure that there will be an adequate bone bridge (approximately 5 mm) between the two femoral tunnels prior to drilling. This is accomplished using the calibrated probe and direct arthroscopic visualization. The appropriately sized standard cannulated reamer is used to create the posterior medial bundle femoral tunnel. A curette is used to cap the tip of the guide wire so that there is no inadvertent advancement of the guide wire, which could damage the anterior cruciate ligament, or articular surface. As the reamer is about to penetrate interiorly, the reamer is disengaged from the drill and the final reaming is completed by hand. This adds an additional margin of safety. The reaming debris is evacuated with a synovial shaver to minimize fat pad inflammatory response with subsequent risk of arthrofibrosis. The tunnel edges are chamfered and rasped.
Drilling the Femoral Tunnel Inside-Out: Single- and Double-Bundle Posterior Cruciate Ligament Reconstruction.
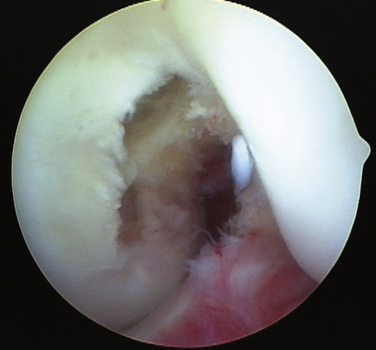
The PCL single- or double-bundle femoral tunnels can be made from inside-out using the double-bundle aimers. Inserting the appropriately sized double-bundle aimer through a low anterior lateral patellar arthroscopic portal creates the PCL anterior lateral bundle femoral tunnel. The double-bundle aimer is positioned directly on the footprint of the femoral anterior lateral bundle PCL insertion site (Fig. 28-6A). The appropriately sized guide wire is drilled through the aimer, through the bone, and out a small skin incision. Care is taken to ensure that there is no compromise of the articular surface. The double-bundle aimer is removed and an acorn reamer is used to drill endoscopically from inside-out the anterior lateral PCL femoral tunnel. The tunnel edges are chamfered and rasped. The reaming debris is evacuated with a synovial shaver to minimize fat pad inflammatory response with subsequent risk of arthrofibrosis. When the surgeon chooses to perform a double-bundle double femoral tunnel PCL reconstruction, the same process is repeated for the posterior medial bundle of the PCL (see Fig. 28-6B). Care must be taken to ensure that there will be an adequate bone bridge (approximately 5 mm) between the two femoral tunnels prior to drilling. This is accomplished using the calibrated probe and direct arthroscopic visualization (Fig. 28-7).
Posterior Cruciate Ligament Graft Tensioning and Tibial Fixation
Tension is placed on the PCL graft distally using the Biomet graft-tensioning boot with the knee in full extension, and the tension is set for 20 pounds (Fig. 28-8). This restores the anatomic tibial step-off. The knee is cycled through a full range of motion 25 times to allow pretensioning and settling of the graft. In double-bundle PCL reconstructions, both the anterolateral and posteromedial bundles have final fixation in 70 to 90 degrees of knee flexion. The process is repeated until there is no further change in the torque setting on the graft tensioner, indicating that all laxity is removed from the system. The knee is placed in 70 to 90 degrees of flexion; fixation is achieved on the tibial side of the PCL graft with a Biomet BioCore interference screw and cortical suspensory fixation with a bicortical screw and spiked ligament washer (Fig. 28-9).
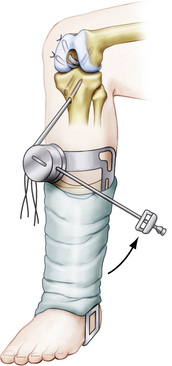
FIGURE 28-8 Biomet graft-tensioning boot applied to PCL reconstruction grafts
(Adapted from Fanelli GC. Rationale and Surgical Technique for PCL and Multiple Knee Ligament Reconstruction. 2nd ed. Warsaw, Ind: Biomet Sports Medicine; 2008.)
Anterior Cruciate Ligament Reconstruction Procedures
With the knee in approximately 90 degrees of flexion, the ACL tunnels are created using the PCL-ACL drill guide single-incision endoscopic surgical technique. The arm of the drill guide enters the knee joint through the inferior medial patellar portal. The bullet of the drill guide contacts the anterior medial proximal tibia externally at a point 1 cm proximal to the tibial tubercle, midway between the posterior medial border of the tibia and the tibial crest anteriorly. The guide wire is drilled through the guide to emerge through the center of the stump of the ACL tibial footprint. A standard cannulated reamer is used to create the tibial tunnel.
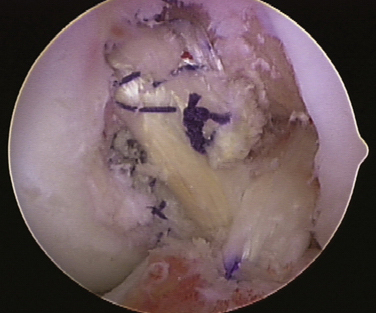
The ACL graft is tensioned on the tibial side using the Biomet graft-tensioning boot, with the knee in full extension. Traction is placed on the ACL graft sutures and tension is set for 20 pounds. The knee is then cycled through 25 full flexion and extension cycles to allow settling of the graft. The process is repeated until there is no further change in the torque setting on the graft tensioner, indicating that all laxity is removed from the system. The knee is placed in 30 degrees of flexion; fixation is achieved on the tibial side of the ACL graft with a Biomet BioCore interference screw and cortical suspensory fixation with a Biomet polyethylene ligament fixation button. The arthroscopic examination shows the completed reconstruction in the intercondylar notch (Fig. 28-10).
Lateral Posterolateral Reconstruction
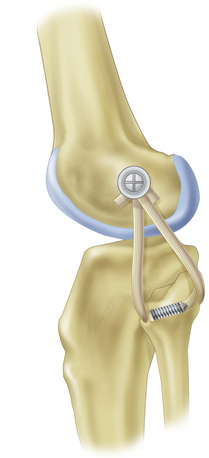
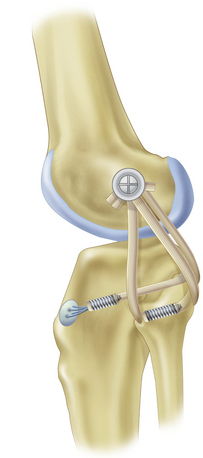
One surgical technique for posterolateral reconstruction is the free graft figure-of-eight technique using a semitendinosus autograft or allograft, Achilles tendon allograft, or other soft tissue allograft material (Fig. 28-11). This procedure requires an intact proximal tibiofibular joint and the absence of a hyperextension external rotation recurvatum deformity. This technique combined with capsular repair and/or posterolateral capsular shift procedures (Fig. 28-12), mimics the function of the popliteofibular ligament and lateral collateral ligament, tightens the posterolateral capsule, and provides a post of strong autogenous tissue to reinforce the posterolateral corner. When there is a disrupted proximal tibiofibular joint or hyperextension external rotation recurvatum deformity, a two-tailed (fibular head, proximal tibia) posterior lateral reconstruction is required (Fig. 28-13). For a comprehensive review of posterolateral reconstruction techniques, see Chapter 27.
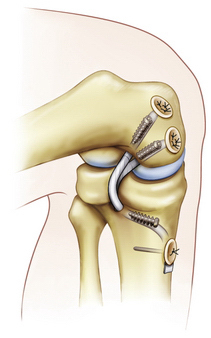
Medial Posteromedial Reconstruction
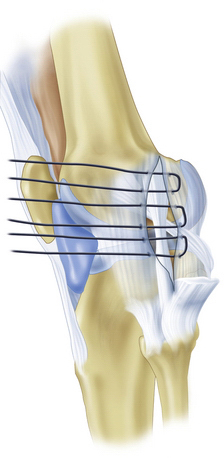
Posteromedial and medial reconstructions are performed through a medial hockey stick incision. Care is taken to maintain adequate skin bridges between incisions. The superficial medial collateral ligament is exposed and a longitudinal incision is made just posterior to the posterior border of the superficial MCL (Fig. 28-14). Care is taken not to damage the medial meniscus during the capsular incision. The interval between the posteromedial capsule and medial meniscus is developed. The posteromedial capsule is shifted anterosuperiorly. The medial meniscus is repaired to the new capsular position and the shifted capsule is sewn into the medial collateral ligament. When superficial MCL reconstruction is indicated, this is performed using allograft or autograft tissue (Fig. 28-15). This graft material is attached at the anatomic insertion sites of the superficial medial collateral ligament on the femur and tibia using a screw and spiked ligament washer or suture anchors. The posteromedial capsular advancement is performed and sewn into the newly reconstructed MCL (Fig. 28-16). The final graft-tensioning position is approximately 30 to 40 degrees of knee flexion.
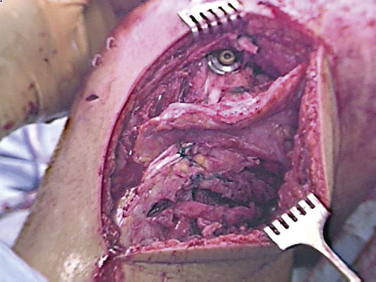
FIGURE 28-14 Intraoperative photograph of posterolateral reconstruction. Note peroneal nerve neurolysis.
(Courtesy of Dr. Gregory C. Fanelli.)
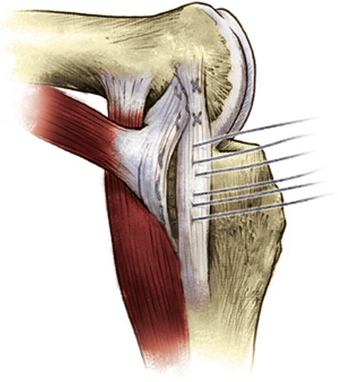
FIGURE 28-15 Posteromedial capsular shift procedure to address medial posteromedial instability.
(Adapted from Fanelli GC. Rationale and Surgical Technique for PCL and Multiple Knee Ligament Reconstruction. 2nd ed. Warsaw, Ind: Biomet Sports Medicine; 2008.)
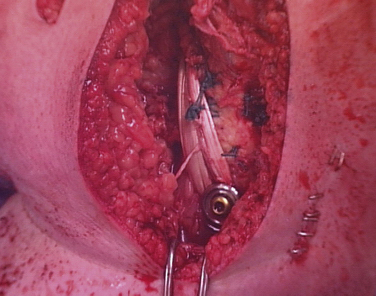
FIGURE 28-16 Intraoperative photograph of medial posteromedial reconstruction.
(Courtesy of Dr. Gregory C. Fanelli.)
PEARLS& PITFALLS
Postoperative Rehabilitation
Our specific rehabilitation program is as follows. The knee is kept locked in a long leg brace in full extension for 5 weeks, with non–weight bearing using crutches. The brace is unlocked at the end of postoperative week 5. Progressive range of motion is initiated during postoperative week number 6. Progressive weight bearing at 20% body weight per week begins during postoperative week 6, and progresses through postoperative week 10. Crutches are discontinued at the end of postoperative week 10 when the patient is fully weight bearing and has enough quadriceps control for unassisted ambulation. Progressive strengthening and proprioceptive skill training are initiated while protecting the healing grafts. Return to sports and heavy labor occurs 6 to 9 months postoperatively, when sufficient strength, range of motion, and proprioceptive skills have returned.37,38
Posterior cruciate ligament reconstruction performed according to the surgical techniques and rehabilitation program described has led to successful results. Documentation of these results has been performed by physical examination, arthrometer (KT-1000) measurements, knee ligament rating scales, and stress (Telos) radiography. PCL reconstruction in 41 chronic PCL-PLC reconstructions has resulted in 70% normal posterior drawer test and tibial step-off for the overall study group, and 92% normal posterior drawer and tibial step-off in a subgroup using a mechanical graft-tensioning boot.3 PCL reconstruction in 15 consecutive combined PCL–ACL-collateral ligament (multiple-ligament injured knee) reconstructions has resulted in 87% normal posterior drawer test and tibial step-off in these combined central pivot reconstructions using a mechanical graft-tensioning device.5
CONCLUSIONS
The results of surgical treatment of the bicruciate multiple-ligament injured (dislocated) knee have demonstrated excellent functional results, often achieving return to preinjury level of function. This has been demonstrated with physical examination, arthrometer measurements, knee ligament rating scales, and stress radiographs.2,26–33 Comparisons of single- and double-bundle PCL reconstructions in the multiple-ligament injured knee have demonstrated no superior surgical procedure.39–46 Both the single-bundle and double-bundle arthroscopically assisted transtibial posterior cruciate ligament reconstruction techniques are successful surgical procedures. Statistically significant improvements from preoperative to postoperative status evaluated by physical examination, knee ligament rating scales, arthrometer measurements, and stress radiography have been demonstrated. Factors contributing to the success of these surgical procedures include identification and treatment of all pathology (especially posterolateral and posteromedial instability), accurate tunnel placement, placement of strong graft material at anatomic graft insertion sites, minimizing graft bending, performing final PCL graft fixation at 70 to 90 degrees of knee flexion using the graft-tensioning boot, using primary and backup fixation, and the appropriate postoperative rehabilitation program.
The multiple-ligament injured knee is a severe injury that may also involve neurovascular injuries and fractures. Surgical treatment offers good functional results documented in the literature by physical examination, arthrometer testing, stress radiography, and knee ligament rating scales. Mechanical tensioning devices are helpful with cruciate ligament tensioning. Some low-grade medial collateral ligament complex injuries may be amenable to brace treatment, whereas high-grade medial side injuries require repair or reconstruction. Lateral posterolateral injuries are most successfully treated with surgical repair or reconstruction. Surgical timing in acute multiple-ligament injured knee cases depends on the ligaments injured, vascular status of the injured extremity, skin condition of the extremity, degree of instability, and the patient’s overall health. Allograft tissue is preferred for these complex surgical procedures. Delayed reconstruction of 2 to 3 weeks may decrease the incidence of arthrofibrosis, and it is important to address all components of the instability. Currently, there is no conclusive evidence that double-bundle PCL reconstruction provides superior results to single-bundle PCL reconstruction in the multiple-ligament injured knee.
1. Fanelli GC, Orcutt DR, Edson CJ. The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy. 2005;21:471-486.
2. Fanelli GC, Edson CJ, Orcutt DR, et al. Treatment of combined anterior cruciate-posterior cruciate ligament-medial-lateral side knee injuries. J Knee Surg. 2005;18:240-248.
3. Burke R, Walker D, Schenck RC, et al. The dislocated knee: a new classification system. South Med J. 1992;85(suppl):3S-S61.
4. Abou-Sayed H, Berger DL. Blunt lower-extremity trauma and popliteal artery injuries: revisiting the case for selective arteriography. Arch Surg. 2002;137:585-589.
5. Dennis JW, Jagger C, Butcher JL, et al. Reassessing the role of arteriograms in the management of posterior knee dislocations. J Trauma. 1993;35:692-695.
6. Hollis JD, Daley BJ. 10-year review of knee dislocations: is arteriography always necessary?. J Trauma. 2005;59:672-675.
7. Kaufman SL, Martin LG. Arterial injuries associated with complete dislocation of the knee. Radiology. 1992;184:153-155.
8. Kendall RW, Taylor DC, Salvian AJ, O’Brien PJ. The role of arteriography in assessing vascular injuries associated with dislocations of the knee. J Trauma. 1993;35:875-878.
9. Klineberg EO, Crites BM, Flinn WR, et al. The role of arteriography in assessing popliteal artery injury in knee dislocations. J Trauma. 2004;56:786-790.
10. Martinez D, Sweatman K, Thompson EC. Popliteal artery injury associated with knee dislocations. Am Surg. 2001;67:165-167.
11. Stannard JP, Sheils TM, Lopez-Ben RR, et al. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86:910-915.
12. Treiman GS, Yellin AE, Weaver FA, et al. Examination of the patient with a knee dislocation. The case for selective arteriography. Arch Surg. 1992;127:1056-1062.
13. Miranda FE, Dennis JW, Veldenz HC, et al. Confirmation of the safety and accuracy of physical examination in the evaluation of knee dislocation for injury of the popliteal artery: a prospective study. J Trauma. 2002;52:247-251.
14. Wascher DC. High-velocity knee dislocation with vascular injury. Treatment principles. Clin Sports Med. 2000;19:457-477.
15. Sawchuk AP, Eldrup-Jorgensen J, Tober C, et al. The natural history of intimal flaps in a canine model. Arch Surg. 1990;125:1614-1616.
16. Stain SC, Yellin AE, Weaver FA, Pentecost MJ. Selective management of nonocclusive arterial injuries. Arch Surg. 1989;124:1136-1401.
17. Welling RE, Kakkasseril J, Cranley JJ. Complete dislocations of the knee with popliteal vascular injury. J Trauma. 1981;21:450-453.
18. Witz M, Witz S, Tobi E, et al. Isolated complete popliteal artery rupture associated with knee dislocation. Case reports. Knee Surg Sports Traumatol Arthrosc. 2004;12:3-6.
19. Mills WJ, Barei DP, McNair P. The value of the ankle-brachial index for diagnosing arterial injury after knee dislocation: a prospective study. J Trauma. 2004;56:1261-1265.
20. Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations: a meta-analysis. Am J Knee Surg. 2001;14:33-38.
21. Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845-851.
22. Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262-273.
23. Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189-196.
24. Talbot M, Berry G, Fernandes J, Ranger P. Knee dislocations: experience at the Hopital du Sacre-Coeur de Montreal. Can J Surg. 2004;47:20-24.
25. Yeh WL, Tu YK, Su JY, Hsu RW. Knee dislocation: treatment of high-velocity knee dislocation. J Trauma. 1999;46:693-701.
26. Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23:580-587.
27. Noyes FR, Barber-Westin SD. The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am J Sports Med. 1995;23:380-389.
28. Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Am J Sports Med. 1997;25:769-778.
29. Wascher DC. Becker JR. Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189-196.
30. Fanelli GC, Gianotti BF, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction. Arthroscopy. 1996;12:5-14.
31. Fanelli GC, Edson CJ. Arthroscopically assisted combined ACL/PCL reconstruction. 2-10 year follow-up. Arthroscopy. 2002;18:703-714.
32. Fanelli GC, Edson CJ. Arthroscopically assisted combined PCL-posterolateral reconstruction. 2-10 year follow-up. Arthroscopy. 2004;Vol 20(4):339-345.
33. Harner CD. Waltrip RL. Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262-273.
34. Fanelli GC, Feldmann DD. Management of combined anterior cruciate ligament/posterior cruciate ligament/posterolateral complex injuries of the knee. Oper Tech Sports Med. 1999;7:143-149.
35. Fanelli GC, Harris JD. Surgical treatment of acute medial collateral ligament and posteromedial corner injuries of the knee. Sports Med Arthrosc Rev. 2006;14:78-83.
36. Fanelli GC, Harris JD. Late MCL (medial collateral ligament) reconstruction. Tech Knee Surg. 2007;6:99-105.
37. Edson CJ, Rehabilitation of the multiligament-reconstructed knee. Sports Med Arthrosc Rev. 2001;9:247-254.
38. Fanelli GC. Posterior cruciate ligament rehabilitation: how slow should we go?. Arthroscopy. 2008;24:234-235.
39. Levy B, Fanelli GC, Whalen D, et al. Modern perspectives for the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197-206.
40. Levy B, Dajani KA, Whalen DB, et al. Decision making in the multiple ligament injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430-438.
41. Fanelli GC, Edson CJ, Reinheimer KN, Beck J. Arthroscopic single bundle vs. double bundle posterior cruciate ligament reconstruction. Arthroscopy. 2008;24(suppl):e26.
42. Fanelli GC, Edson CJ, Reinheimer KN. Evaluation and treatment of the multiple ligament injured knee. Instr Course Lect. 2009;58:389-395.
43. Fanelli GC, Edson CJ, Reinheimer KN, Garofalo R. Posterior cruciate ligament and posterolateral corner reconstruction. Sports Med Arthrosc Rev. 2007;15:168-175.
44. Fanelli GC. Posterior Cruciate Ligament Injuries: A Practical Guide To Management. Springer-Verlag, New York, 2001.
45. Fanelli GC. The Multiple Ligament Injured Knee. A Practical Guide to Management. New York: Springer-Verlag; 2004.
46. Garafallo R, Jolles BM, Moretti B, Siegrist O. Double-bundle transtibial posterior cruciate ligament reconstruction with a tendon-patellar bone-semitendinosus tendon autograft: clinical results with a minimum 2 years’ follow-up. Arthroscopy. 2006;22:1331-1338.