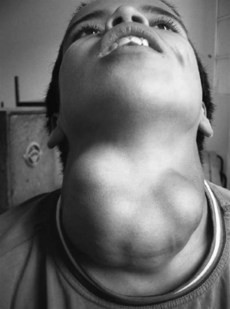
140 Multinodular goitre
Salient features
History
• Stridor: trachea must be narrowed to 20–30% for this symptom
• Hoarseness of voice (caused by pressure on recurrent laryngeal nerve), suggests thyroid malignancy
• Acute painful enlargement, suggests bleeding into thyroid nodule
• Suffusion of face when the patient raises the arms above the head, suggests substernal goitre
• Deafness: if caused by eighth cranial nerve involvement suggests Pendreds syndrome (rare)
Questions
How would you investigate a nodular goitre?
• Serum thyroid-stimulating hormone (TSH) and free thyroxine (T4) should be measured to identify those with subclinical or overt hyperthyroidism. If the TSH is suppressed, radionuclide scanning should be performed.
• Ultrasonography of the thyroid gland indicates whether goitre is cystic or solid:
• Patients with features of tracheal compression (inspiratory stridor and dyspnoea) should undergo CT or MRI of the neck and upper thorax, pulmonary function tests especially flow volume loop studies. When CT is used, iodinated contrast agents should not be given because of the risk of inducing hyperthyroidism.
• Antibodies against thyroglobulin (AbTG), anti-thyroperoxidase antibodies (AbTPOs) and calcitonin.
• If the patient has a family history of medullary thyroid carcinoma or multiple endocrine neoplasia type 2, the serum calcitonin level should also be checked.
How would you treat such a patient?
• Beta-blockers to control thyrotoxicosis
• Warfarin in atrial fibrillation to prevent embolic complications
• Radioiodine for hyperthyroidism
• Surgery if the patient refuses radioiodine, for large multinodular goitres or malignancy
• In patients <20 years of age, and in the case of a high clinical suspicion for cancer (e.g. follicular neoplasia as diagnosed by fine-needle aspiration and a non-functioning nodule revealed on scanning), the patient should be offered hemithyroidectomy regardless of the results of fine-needle aspiration
What are indications for treatment of patients with non-toxic multinodular goitre?
Compression of the trachea or oesophagus and venous-outflow obstruction.
What are the treatment options available for non-toxic multinodular goitre?
• Surgery is the standard therapy, especially when rapid decompression of vital structures is required. It allows pathological examination of the thyroid. Disadvantages include postoperative tracheal obstruction, recurrent laryngeal nerve injury, hypoparathyroidism, hypothyroidism and goitre recurrence.
• Thyroxine therapy to shrink goiters is no longer recommended. Disadvantages are that it causes only a small decrease in thyroid volume; long-term efficacy is not known; it causes a decrease in bone mineral density in postmenopausal women; and there are possible cardiac side effects.
• Radioiodine is an alternative to surgery in elderly patients and in those with cardiopulmonary disease. It results in a substantial decrease in thyroid volume and improvement of compressive symptoms in most patients. Disadvantages are that it only causes a gradual decrease in thyroid volume; radiation thyroiditis (usually mild) and radiation-induced thyroid dysfunction (hyperthyroidism in 5%, hypothyroidism in 20–30%) ) can occur; and there is a possible risk of radiation-induced cancer (N Engl J Med 1998;338:1438–47).
• Treatment options depends on the nodule:
What are the treatment options available for toxic multinodular goitre?
• Antithyroid drugs are valuable as pretreatment for surgery and before and after radioiodine treatment in elderly patients and those with concurrent health problems. Long-term treatment is recommended only when other therapies cannot be used. The disadvantages are that the treatment is lifelong and there are potential adverse effects such as agranulocytosis.
• Surgery should be considered in large goitres when rapid relief is needed. The other advantage is that it provides tissue for a pathological diagnosis. Disadvantages include surgical mortality and morbidity; hypothyroidism and persistence or recurrence of hyperthyroidism.
• Radioiodine is an appealing option in the majority of the patients because it is highly effective for reversal of hyperthyroidism. The disadvantages include a gradual diminution of the hyperthyroid state, more than one dose may be necessary, hypothyroidism (<20%) and the theoretical risk of radiation-induced cancer (N Engl J Med 1998;338:1438–47).
Advanced-level questions
How do you differentiate between Graves’ disease and toxic nodular goitre?
| Graves’ disease | Toxic nodular goitre |
|---|---|
| Younger age group | Older individuals |
| Diffuse goitre | Nodular enlargement of the gland |
| Eye signs common | Eye signs are rare |
| Atrial fibrillation is uncommon | Atrial fibrillation is common (about 40% of the patients) |
| Other autoimmune diseases are common | Other autoimmune diseases are uncommon |