Chapter 97 Multiligament Knee Injury: Should Surgical Reconstruction Be Acute or Delayed?
Multiple ligament knee injuries involve rupture of at least 2 major ligaments of the knee usually involving 1 or both of the cruciates with or without injury to the collateral ligaments. Multiple knee ligament injuries are relatively rare and often the result of high-energy traumatic injuries. The optimal amount of time between injury and surgical intervention is controversial. Some argue for intervention in the acute stage, commonly defined as within 3 weeks of injury, whereas others have recommended delaying surgery a number of months depending on a variety of factors.1–6
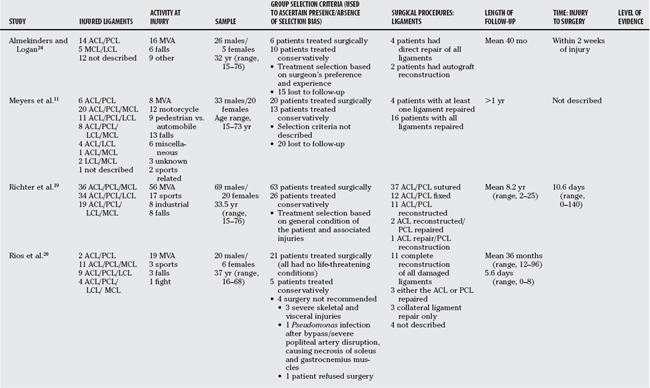
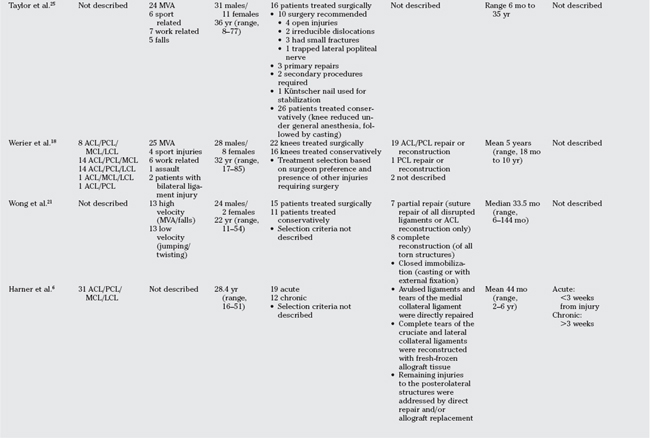
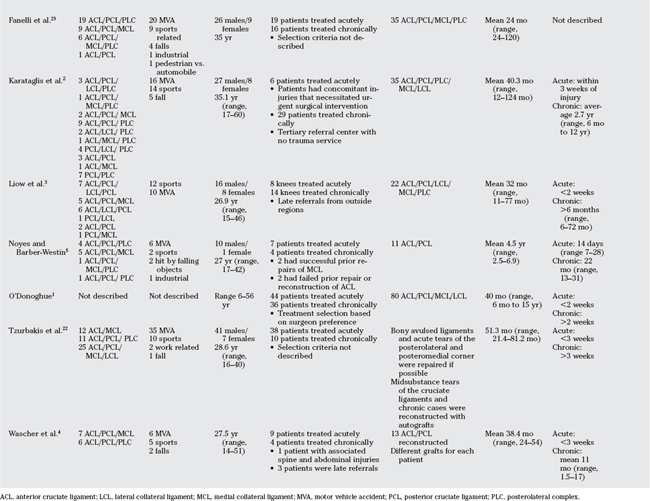
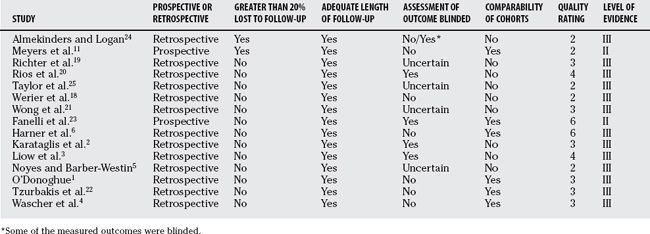
We identified 16 articles; 7 studies compared acute with conservative treatment, and 9 studies compared acute with chronic surgical repair. The characteristics and levels of evidence of these studies are displayed in Table 97-1. There were no randomized trials, and only 1 study was prospective. Of the 9 studies that addressed acute versus chronic repair, 1 study7 was excluded because it did not provide a direct comparison between the 2 cohorts. All studies included a variety of combinations of injured ligaments. The average sample size was 39 (range, 11–89). Studies were evaluated for methodologic quality according to a modified version of the Newstead–Ottawa Scale (NOS)8; a scale designed to assess the quality of nonrandomized studies (Table 97-2). Using this rating scale, each study is judged on 3 broad perspectives: the selection of study groups, the comparability of the groups, and the ascertainment of the outcome of interest. The maximum number of points is 8, which indicates a high-quality study. In general, the methodologic quality was poor; the maximum number of points awarded on the NOS was 6, and the majority of studies were awarded 3 points. The methodologic features of these studies are summarized in Table 97-3.
TABLE 97-2 Newstead–Ottawa Scale
Rights were not granted to include this table in electronic media. Please refer to the printed book.
From The Newcastle-Ottawa Scale (NOS). Assessing the quality of non-randomized studies in meta-analysis. Proceedings of the 3rd Symposium on Systematic Reviews: Beyond the Basics-Improving Quality and Impact. Oxford, St. Catherine’s College, July 2000.
SUBJECTIVE OUTCOME MEASURES: A BRIEF DESCRIPTION
Functional Status
Five subjective functional outcome measures were common among studies: (1) Lysholm,9 (2) International Knee Documentation Committee (IKDC),10 (3) Meyer’s Rating Scale,11 (4) Knee Outcome Survey,12 and (5) Hospital for Special Surgery.13 A brief description of these outcome instruments follows.
The Lysholm scale is designed to document the patient’s evaluation of function. It is a conditionspecific outcome measure that contains 8 domains: limp, locking, pain, stair climbing, use of supports, instability, swelling, and squatting.9 An overall score from 0 to 100 points is calculated, with 95 to 100 points indicating an excellent outcome; 84 to 94 points, a good outcome; 65 to 83 points, a fair outcome; and less than 65 points, a poor outcome. The instrument has face validity and acceptable construct and criterion validity, as well as test-retest reliability and adequate responsiveness.14
The IKDC scale has 2 versions. The older version included a subjective patient-rated assessment within a generally physician-rated form (now Knee Examination Form). The subjective portion included 2 patient-rated questions that ask, “How does your knee function?” and “How does your knee affect your activity level?” Patients provide a rating of normal (A), nearly normal (B), abnormal (C), or severely abnormal (D). The question with the lowest rating provides the score for that patient.10,15 The latest version of the IKDC contains a separate form titled “The Subjective Knee Evaluation Form”10 that is an 18-item, knee-specific questionnaire designed to detect changes in patients with a variety of knee conditions. The questions address 3 domains: physical symptoms (7 items), sports activities (10 items), and function before injury (1 item). The resulting total score is out of 100 possible points, which represents perfect knee function. This instrument has face validity and demonstrated construct validity, excellent testretest reliability, and sensitivity to change.10,15
Meyers and coworkers11 developed a rating scale to measure the functional ability of patients after treatment for knee dislocations. They defined “excellent” as the ability to return to work or previous level of activity without impairment and with a stable knee; “good” included having knee symptoms that did not preclude the patient’s return to normal occupation and activities of daily living. In this classification, pain is present but is considered an annoyance, and symptoms of instability are unusual or minimal. A rating of “fair” means the patient is performing all activities of daily living but has difficulty walking upstairs, walking on tiptoes, or running, and tends to avoid such activities. Finally, a “poor” functional rating is assigned to patients who cannot work and who are unable to perform daily activities.
The Knee Outcome Survey was developed to measure symptoms and functional limitations for patients with a variety of knee disorders, including ligamentous and meniscal injuries.12 The Knee Outcome Survey consists of two scales, the Activities of Daily Living Scale and the Sports Activity Scale. The Activities of Daily Living Scale measures symptoms and functional limitations during activities of daily living. The score ranges from 0 to 100 points, with 100 points indicating an absence of symptoms and functional limitations during activities of daily living. The Activities of Daily Living Scale has been shown to be a reliable, valid, and responsive measure of symptoms and functional limitations during activities of daily living in individuals with a variety of knee injuries. The Sports Activity Scale measures symptoms and functional limitations experienced during sports activities. The Sports Activity Scale score ranges from 0 to 100 points, with 100 points representing the absence of symptoms and functional limitations during sports activities.12
Return to Activity
Two scales are used to measure patient activity level: (1) the Tegner Activity Level Scale and (2) the IKDC activity level scale. The Tegner Activity Level Scale rates the level of activity on a scale of 0 (off of work) to 10 (competitive contact sports).16 The IKDC activity level scale measures return to activity on four levels: I is return to intensive activity, II is moderate activity, III is light activity, and IV is remain sedentary.
Ligament Stability
The overall IKDC Knee Examination Form assesses the function of the knee based on 4 factors: (1) subjective assessment, (2) symptoms, (3) range of motion (ROM), and (4) ligament examination. These factors are rated as normal (A), nearly normal (B), abnormal (C), and severely abnormal (D).17 The overall final IKDC rating is based on group ratings for function, symptoms, ROM, and laxity. The worst problem area qualification defines the overall final qualification.
RESULTS
Lysholm Scale
Werier and colleagues18 found that the average Lysholm scale score of 85 (95% confidence interval [CI], 80–90) in the reconstructed group was significantly greater than the average score of 69 (95% CI, 57–81) in those patients who were treated conservatively. When comparing the components of the Lysholm, the reconstructed group had a better ability to climb stairs and experienced less symptomatic instability. Similarly, Richter and investigators19 found that the Lysholm score was significantly greater in those who underwent surgical treatment (78.3 ± 13.4) compared with those who had nonoperative treatment (64.8 ± 16.3).
International Knee Documentation Committee Subjective Score
Rios and coauthors20 report the IKDC subjective score in terms of having excellent, good, fair, or poor results. The authors did not provide a definition of these classifications. The surgical group (n = 21) had 4 patients with excellent results and 10 patients with good results, whereas none of the patients in the conservatively managed group (n = 5) had excellent or good results. In a similar study, Wong and colleagues21 found that operative patients had a significantly greater average IKDC score (75.8 ± 10.0) compared with the conservative group (63.7 ± 9.1), whose average was considered suboptimal.
Meyer’s Rating Scale
According to the Meyer’s Rating Scale, Meyers and researchers11 found that of the 13 patients in the conservatively managed group, 10 reported poor functional outcome, 2 fair, and 1 good. Three patients in the surgical group (n = 20) were rated as poor, 3 fair, 11 good, and 3 excellent. The authors conclude that the surgical group had better outcomes after treatment compared with those patients who did not undergo ligament repair. Similarly, Rios and colleagues20 reported that all of the patients in the conservatively managed group (n = 5) were reported to have fair or poor functional outcomes on the Meyer’s scale, whereas only 2 patients were rated as fair and 2 as poor in the surgical group (n = 21). Sixteen patients in the surgical group had excellent or good results.
ACUTE VERSUS DELAYED RECONSTRUCTION
Lysholm Scale
Harner and colleagues6 found that the 19 patients who underwent acute surgery had an average Lysholm score of 91 ± 7.0 points, compared with 80 ± 16.9 points for the 12 patients whose surgery was delayed. Although the acute group had a greater average score than the chronic group, this difference did not reach statistical significance. Similarly, Tzurbakis and coauthors22 report a mean Lysholm score of 88.3 ± 11.9 for the acutely treated patients and a mean score of 81.7 ± 13.3 for the delayed group (P > 0.05). Similar differences were observed in Liow and investigators’ study3 in which those patients who underwent surgery during the acute phase had better functional ratings (87; 95% CI, 81–91) than those patients who underwent late reconstruction (75; 95% CI, 53–100). All acutely treated knees had a Lysholm score of more than 80 compared with only 5 of the 14 (36%) knees with delayed treatment. Likewise, Wascher and coauthors4 report a greater Lysholm score for patients treated acutely compared with chronic patients, with a mean score of 91.3 and 79.3, respectively. Finally, Fanelli and coauthors23 report no statistically significant difference in the Lysholm score between acute and delayed treated knees; although no data were provided to support these conclusions.
International Knee Documentation Committee Patient Subjective Assessment
Tzurbakis and coauthors22 report that 30 patients in the acutely treated group (n = 38) considered their knee to be normal or nearly normal. Only 5 of 10 patients treated in the delayed phase rated their knee as normal or nearly normal. This difference was statistically significant.
Meyer’s Rating Scale
Harner and colleagues6 report that 16 of 19 patients in the acute group had an excellent or good rating, and 3 had a fair rating. Of the 12 patients in the delayed group, 7 received an excellent or good rating, 2 received a fair rating, and 3 received a poor rating. The difference between the acute and delayed groups was not statistically significant. Similarly, Wascher and coauthors4 found that 4 patients who underwent surgery in the acute phase (n = 9) had an excellent rating and 5 had a good outcome, whereas no patients were classified as fair or poor. In the delayed group (n = 4), 2 patients were rated as excellent, 1 rated as fair, and 1 rated as poor.
Knee Outcome Survey
One study6 evaluated patients using the Knee Outcome Survey. The average score on the Activities of Daily Living scale for the acutely treated patients was 91 ± 6.4, and the patients who received delayed treatment had an average score of 84 ± 11.8. Despite the trend toward a better outcome in the acutely treated patients, this difference was not statistically significant. On the Sports Activity Scale, the patients in the acute group had a significantly greater average score (89 ± 10.3), compared with those in the delayed group (69 ± 27.9) points.
Using their own classification, Noyes and Barber-Westin5 had all patients complete a separate rating of their perception of the overall outcome and knee condition, rated as poor, fair, good, very good, or normal. Three patients in the acute group (n = 7) rated their knees as normal; two patients rated as good, and two patients rated as poor. In the delayed group (n = 4), one patient rated their knee condition as very good, one patient as good, and two patients as fair. The authors conclude that the acute patients had better overall perceptions of their outcome compared with the chronic group.
RETURN TO ACTIVITY
Acute versus Nonoperative
Richter and colleagues19 report that patients who underwent surgical intervention returned to higher levels of activity (4.0) according to the Tegner Activity Scale compared with those who received nonoperative treatment (2.7). In this same study, the IKDC showed that significantly more patients in the surgical group returned to intense or moderate activities compared with the group managed without surgery.
Acute versus Delayed
According to the Tegner Activity score, Liow and investigators3 found that 5 patients from the acute group (n = 8) had activity levels greater than 5, compared with 7 of the 14 patients who underwent delayed reconstruction. The mean Tegner level showed a trend toward the early reconstruction group returning to higher levels of activity than the late reconstruction group with average scores of 5 (range, 3–7) and 4.4 (range, 1–7), respectively. Fanelli and coauthors23 also compared the results of the Tegner score between the acutely treated and delayed treatment patients. The authors conclude no statistically significant difference between acute and delayed treatment knees in their ability to return to activities after surgery. Noyes and Barber-Westin5 found that of the four patients treated acutely, two patients had decreased work activities because of their knee condition, one had decreased work activities because of reasons unrelated to their knee, and two remained in the same occupation. Only one patient had returned to activity at follow-up. Three patients returned to occupations rated as light. All patients with delayed treatment had decreased their activities, sports and work-related activities, because of their knee condition.
LIGAMENT STABILITY
Acute versus Non-operative
Richter and investigators19 report that the proportion of patients who obtained a rating of nearly normal or normal (B) was significantly greater in those undergoing surgery (14/59) compared with those receiving nonoperative treatment (1/18).
Acute versus Delayed
Tzurbakis and coauthors22 report that 27 of 35 patients in the acute group were graded as normal or nearly normal compared with 5 of the 9 patients in the delayed group. This difference was not statistically significant. From a possible 31 patients, Harner and colleagues6 reported the final overall IKDC rating as nearly normal for 11 knees, abnormal for 12, and severely abnormal for 8. No knee received a normal overall IKDC rating. Ten of the 11 knees that received a nearly normal IKDC score had been treated acutely. An equal number of severely abnormal knees was reported in the acute and delayed groups. In a similar study, Liow and investigators3 found no statistically significant difference in overall IKDC rating between patients who underwent reconstruction in either the acute or the delayed phase. They report that 3 of the 8 knees in the acute patients were rated as nearly normal, compared with 5 of the 14 knees that underwent delayed reconstruction. Of the patients who underwent surgical intervention in the acute phase, Wascher and coauthors4 report four patients who rated their knees as nearly normal and four patients who gave a rating of abnormal. Of the patients in the delayed group, 2 knees were rated as nearly normal, one as abnormal, and one as severely abnormal.
Lachman Testing
Acute versus Non-operative.
Werier and colleagues18 reported the results of the Lachman test in 20 degrees of knee flexion. The Lachman test was classified as grade I (0–5 mm displacement), grade II (5–10 mm displacement), or grade III (>10 mm displacement).18 A significantly greater number of individuals with a grade III Lachman were in the nonoperative group compared with the operative group.
Acute versus Delayed.
Wascher and coauthors4 measured the Lachman test with the knee in 20 degrees of flexion and reported that, in the acute group, 7 of 9 patients were normal, and 2 patients had 3 to 5 mm of anterior tibial translation. In the delayed group, 2 patients were graded as normal, and 2 patients had 3 to 5 mm of anterior translation. All patients in both groups had firm end points.
KT-1000 Arthrometer
Acute versus Non-operative.
Two studies19,24 used the KT-1000 arthrometer to measure cruciate ligament laxity. Almekinders and Logan24 specifically looked at anteroposterior (AP) laxity of the knee. They defined abnormal AP laxity as 3-mm or more side-to-side difference when compared with the unaffected knee. The authors found that all patients in the nonoperative group had abnormal AP laxity compared with their contralateral knee, whereas only 2 of the 6 patients in the operative group experienced greater than 3 mm excursion. Similarly, Richter and investigators19 examined cruciate ligament stability using KT arthrometer whereas performing the Lachman test (at 25 degrees of knee flexion) with 20 pounds of force. They report that, on average, patients treated without surgery had significantly greater translation (8.2 ± 3.4 mm) compared with the surgical group (5.1 ± 2.4 mm). Furthermore, in a similar study, Wong and investigators21 report the mean AP tibial translation for the surgical group as 4.6 mm compared with 9.4 mm for the group managed without surgery.
Acute versus Delayed.
Fanelli and coauthors,23 Tzurbakis and coauthors,22 and Mariani8 all report no statistically significant difference in KT-1000 arthrometer measurement between acute and delayed cases in their respective studies. Similarly, Noyes and Barber-Westin5 found that all but 1 patient in the acute group (n = 7) had less than a 3-mm difference in AP displacement testing compared with the contralateral knee. Two patients treated in the delayed phase (n = 4) had a less than 3-mm difference whereas 2 patients had greater than a 6-mm side-to-side difference. Similarly, Wascher and coauthors4 report a mean side-to-side difference of 4.1 mm in the acute group compared with an average of 5.6 mm in the delayed treatment group. Conversely, Liow and investigators3 reported that 6 of 8 acute ACL reconstructions had 3 to 5 mm difference compared with 9 of 14 delayed surgeries cases.
RANGE OF MOTION
Acute versus Nonoperative
Wong and colleagues21 report the average ROM for the surgical patients to be 128 degrees compared with a mean of 137 degrees in the nonoperative patients. This difference was not statistically significant. There were significantly more flexion contractures in the surgical group. The authors emphasize the role of aggressive physiotherapy. Similarly, Richter and investigators19 did not find a statistically significant difference in the proportion of patients with a deficit in either flexion or extension. In the surgical group, 29 of 59 patients that were managed had an extension deficit of 3 degrees or more, whereas 10 of 18 in the nonoperative group experienced this same deficit. Similarly, 44 patients in the surgical group and 16 patients in the nonoperative group had a flexion deficit of 3 degrees or more. Werier and colleagues’18 study found that operative patients had a slightly smaller range of flexion at 120 degrees compared with the nonoperative treatment group at 130 degrees. In contrast, Almekinders and Logan’s24 study reported that ROM in the operative group was slightly better (129 ± 18 degrees) than in the nonoperative group (108 ± 22 degrees).
Acute versus Delayed
Harner and colleagues6 found that total ROM was similar between patients who had undergone surgical treatment during the acute phase (128 ± 10 degrees) compared with those patients who underwent delayed surgery (129 ± 15 degrees). Similarly, Liow and investigators3 report that the mean loss of extension in the acute group was 10 degrees compared with 7 degrees in the group that underwent late reconstruction. The acute group had a smaller loss of flexion (4 degrees) compared with the late reconstructions (8 degrees). Noyes and Barber-Westin5 found that 5 of 7 patients treated during the acute phase had normal knee ROM, whereas all chronic patients (n = 4) had achieved normal knee ROM. Wascher and coauthors4 found that the acute group had a mean ROM of 132.4 degrees, whereas for delayed patients, it was 125.8 degrees. Tzurbakis and coauthors22 also found similar mean ROM between acute and chronic patients (129.5 ± 12.6 and 131.7 ± 12.3 degrees, respectively). They also report similar measures of mean flexion and extension losses between the acute and delayed patients.
RADIOGRAPHIC OUTCOMES
Almekinders and Logan24 used a blinded observer to rate the degenerative changes on plain radiograph. The overall score ranged from 0, no evidence of degenerative arthritis, to a maximum score of 10, severe degenerative arthritis. This study did not demonstrate any significant differences in the degenerative changes between the surgical and nonoperative treatment groups. Werier and colleagues18 used the same rating scale and found that radiographic scores did not differ significantly between the 2 treatment groups. Fifty percent and 60% of the reconstructed and unreconstructed group, respectively, had completely normal radiographs. Richter and colleagues19 used the Jager and Wirth radiologic scale to measure the degree of osteoarthritis in the affected knee. This scale ranges from grade 0 (no signs of osteoarthritis) to grade IV (severe osteoarthritis). The proportion of individuals with grade III or IV osteoarthritis was significantly greater in those who had a nonsurgical intervention compared with those who had surgery. This finding suggests that the use of a larger study may show a benefit to having surgery in terms of the subsequent development of osteoarthritis.
OTHER
Taylor and coworkers25 assessed their patients on 3 factors—stability, pain, and movements—and classified each factor as either good, fair, or poor. They defined “good” as a stable, painless knee that had 90 degrees or greater flexion; “fair” as experiencing slight instability on straining, no pain, and range of flexion between 60 and 90 degrees; and “poor” as the remainder of patients. In contrast with the previous studies, Taylor and coworkers25 found that the nonoperative patients achieved better function on the measured factors than the surgical group. In the conservative group of 26 patients, 18 were classified as good, 6 as fair, and two as poor compared with four good, 6 fair, and 6 poor in the operative group.
COMPLICATIONS
A common postoperative complication reported in the literature was knee joint stiffness. The evidence suggests that surgery during the acute phase is associated with a greater risk for motion loss or arthrofibrosis.3,23 Liow and investigators3 conclude that early repair or reconstruction of all injured ligaments may produce a better functional outcome and a more stable knee, but they also note that the risk for arthrofibrosis remains a concern in acutely treated patients. Fanelli and coauthors23 made a similar suggestion that delaying surgery 2 to 3 weeks allows for swelling to decrease and offers a protected ROM. Noyes and Barber-Westin5 and Wascher and coauthors4 also note that acute reconstruction of the ligaments may increase the risk for postoperative arthrofibrosis; however, they stress the importance of aggressive rehabilitation to prevent this complication. Conversely, Harner and colleagues6 found no increased joint stiffness in the acutely treated patients and advocate early ligament repair.
DISCUSSION
Selection bias refers to a systematic difference between treatment groups in prognosis and subsequent responsiveness to the intervention as a result of the way they were chosen for participation in the study.26 A randomized, controlled trial with adequate concealment of allocation protects against selection bias by ensuring that patient eligibility is determined before randomization so that clinician knowledge of treatment allocation cannot influence the decision whether to include or exclude a patient from the study. Our review did not identify any randomized studies. In fact, decisions about treatment, for the majority of studies, were left to the preference of the treating physician and were usually based on the presence or absence of concomitant injuries and the prognosis of the patient, almost certainly ensuring a selection bias. For example, Werier and colleagues18 made the decision to perform operative repair based on the presence of injuries that required surgery (i.e., vascular injury, nerve injury), and Rios and coauthors20 chose their nonoperative group based on the severity of concomitant injuries (i.e., patients were not fit for surgery). In this review, it was not possible to explore the magnitude of the bias introduced through selection strategies because no study was without methodologic flaws.
The proportion of patients lost to follow-up is another potential threat to the internal validity of a study. In general, a lost-to-follow-up rate of greater than 20% is considered to be a serious threat to the validity of the results because patients are rarely lost to follow-up for arbitrary reasons,27 and there is a good possibility that those patients without complete follow-up have difference outcomes than patients with complete follow-up. In this review, 2 of the 15 eligible studies11,24 reported a greater than 20% lost-to-follow-up rate.
One final methodologic feature that is important to maintaining the internal validity of the study is blinding of the data collector. Blinding is defined as concealment of group assignment from the patients, investigators, and/or outcome assessors in a trial.27 Blinding reduces the potential influence on the measurement or interpretation of outcomes that conscious or unconscious opinions about the effectiveness of the intervention could potentially cause and reduces the potential for imbalances in cointerventions.27 For example, in Richter and investigators’19 study, 27 of 63 surgical patients also underwent a functional rehabilitation regimen in addition to their surgical intervention, but none of the conservatively managed patients received this program.
Finally, it is important to note that there are important differences between studies that make it difficult to summarize the results. Specifically, the involved ligaments, concomitant injuries, patient function/pain before surgery, surgical procedure, and the type of postsurgical rehabilitation differed across studies. For example, Richter and investigators19 report 43% of the surgical group participated in a functional rehabilitation program after surgery, whereas the others in this group and the nonoperative treatment group did not participate in this rehabilitation program. In addition, 19% of the nonoperative treatment group underwent an operative procedure on structures other than the cruciate ligaments. Noyes and Barber-Westin5 also report that the patients in the delayed treatment group had significant symptoms and functional limitations before surgery, whereas none of the seven patients in the acute group had any knee symptoms before their injuries.
Our systematic review of the literature failed to reveal a sound basis for the treatment algorithms or current “dogma” in caring for patients with multiligament knee injuries. However, methodologic shortcomings of these articles and their potential influence on reported outcomes are clearly related limitations in studying this patient population. The injuries remain relatively rare, and it is estimated that the average orthopedic surgeon will treat only 3 or 4 of these injuries during their entire career. It has been reported that incidence of these injuries is increasing because of several factors, including the expanded definition and the increase in the number of people participating in high-speed, risk-taking sports. Although awareness of multiligament knee injuries has improved dramatically, the definitive management of these complex injuries remains controversial because of the number of ligament injury patterns, varying degrees of concomitant injuries, differing patient function/pain before surgery, as well as the variety of surgical procedures and postsurgical rehabilitation protocols that have been recommended. Thus, it will likely take a much larger multicenter trial to ensure that patient enrollment is sufficient to power a study to be able to draw more definitive conclusions regarding best treatment for these patients. Table 97-4 provides a summary of recommendations.
| STATEMENT | LEVEL OF EVIDENCE | GRADE OF RECOMMENDATION |
|---|---|---|
1 O’Donoghue DH. An analysis of end results of surgical treatment of major injuries to the ligaments of the knee. J Bone Joint Surg Am. 1955;37-A:1-13.
2 Karataglis D, Bisbinas I, Green MA, Learmonth DJ. Functional outcome following reconstruction in chronic multiple ligament deficient knees. Knee Surg Sports Traumatol Arthrosc. 2006;14:843-847.
3 Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845-851.
4 Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189-196.
5 Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med. 1997;25:769-778.
6 Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262-273.
7 Mariani PP, Margheritini F, Camillieri G. One-stage arthroscopically assisted anterior and posterior cruciate ligament reconstruction. Arthroscopy. 2001;17:700-707.
8 Anonymous. The Newcastle-Ottawa Scale (NOS). Assessing the quality of non-randomized studies in meta-analysis. Proceedings of the the 3rd Symposium on Systematic Reviews: Beyond the Basics-Improving Quality and Impact. Oxford: St. Catherine’s College, 2000.
9 Kocher MS, Steadman JR, Briggs KK, et al. Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am. 2004;86-A:1139-1145.
10 Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107-114.
11 Meyers MH, Moore TM, Harvey JPJr. Traumatic dislocation of the knee joint. J Bone Joint Surg Am. 1975;57:430-433.
12 Irrgang JJ, Snyder-Mackler L, Wainner RS, et al. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132-1145.
13 Mancuso CA, Sculco TP, Wickiewicz TL, et al. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83-A:1005-1012.
14 Kocher MS, Steadman JR, Briggs KK, et al. Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am. 2004;86-A:1139-1145.
15 Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600-613.
16 Briggs KK, Kocher MS, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg Am. 2006;88:698-705.
17 Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226-234.
18 Werier J, Keating JF, Meek RN. Complete dislocation of the knee—the long-term results of ligamentous reconstruction. Knee. 1998;5:255-260.
19 Richter M, Bosch U, Wippermann B, et al. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718-727.
20 Rios A, Villa A, Fahandezh J, et al. Results after treatment of traumatic knee dislocations: A report of 26 cases. J Trauma. 2003;55:489-494.
21 Wong CH, Tan JL, Chang HC, et al. Knee dislocations: A retrospective study comparing operative versus closed immobilization treatment outcomes. Knee Surg Sports Traumatol Arthrosc. 2004;12:540-544.
22 Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2-8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14:739-749.
23 Fanelli GC, Edson CJ, Maish DR. Combined anterior/posterior cruciate ligament/medial/lateral side injuries of the knee. Sports Med Arthosc. 2001;9:208-218.
24 Almekinders LC, Logan TC. Results following treatment of traumatic dislocations of the knee joint. Clin Orthop Relat Res.; 284; 1992; 203-207.
25 Taylor AR, Arden GP, Rainey HA. Traumatic dislocation of the knee. A report of forty-three cases with special reference to conservative treatment. J Bone Joint Surg Br. 1972;54:96-102.
26 Bandolier on-line. Available at: http://www.jr2.ox.ac.uk/bandolier/aboutus.html. Accessed June 27, 2007.
27 Haynes RB, Sackett DL, Guyatt GH, Tugwell P. Clinical Epidemiology: How to Do Clinical Practice Research, 3rd ed. New York: Lippincott Williams & Wilkins, 2006.