Multifocal Choroiditis
Clinical Features:
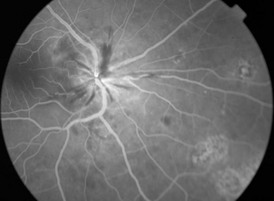
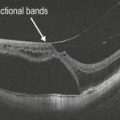
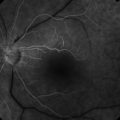
Presentation of MCP is variable. Most patients complain of decreased visual acuity, but photopsia, floaters, blurring of central vision, and enlargement of the blind spot can occur. Anterior segment inflammation may be present but is typically mild. Vitritis of variable severity, and optic disc edema may be present. Multiple small, round to ovoid, pale lesions occur at the level of the outer retina, retinal pigment epithelium (RPE) and choroid, usually 50–350 µm in size, variable in number, and involve mainly the posterior pole (Fig. 17.1.1). Older lesions become pigmented and ‘punched-out’, resembling histoplasmosis lesions. RPE metaplasia and choroidal neovascularization (peripapillary and macular) are common sequelae. CME, epiretinal membrane and subretinal fibrosis may be seen later.
OCT Features:
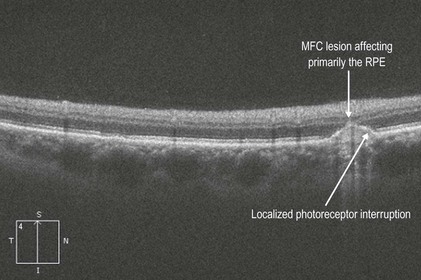
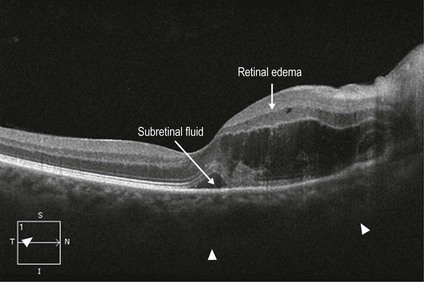
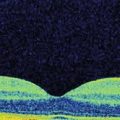
Active lesions show characteristic transretinal hyper-reflectivity and drusen-like material between the RPE and Bruch’s membrane (Figs 17.1.2 and 17.1.3). Nodular collections beneath the RPE appear to rupture with resulting inflammatory infiltration of the subretinal space and the outer retina. Slight choroidal thickening, localized choroidal hyper-reflectivity under the lesions, atrophy of the RPE and the retina overlying the lesions and vitreous cells may be seen. Widespread loss of outer retinal architecture, retinal thinning, destructuring of the retinal layers, and disappearance of IS–OS junction/ellipsoid layer has also been seen in more advanced cases and may be associated with worse vision. Occasionally, CNV, CME and serous retinal detachments may be seen
Ancillary Testing:
On fluorescein angiography, active lesions show early hypofluorescence due to blockage and late staining (see Fig. 17.1.1). Atrophic lesions show early hyperfluorescence, which fades later, due to RPE window defects. Choroidal neovascularization or CME may be seen in the late phases.
Visual field testing usually reveals an enlarged blind spot, but larger defects may be seen.