Motor System
What You Find and What It Means
WHAT YOU FIND
Remember:
See Figure 20.1.
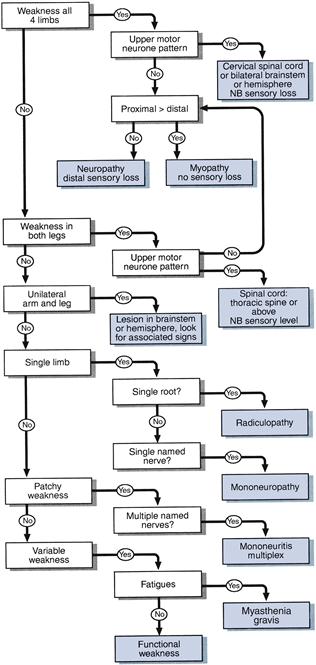
Figure 20.1 Flow chart: simplified approach to weakness
1 Weakness in all four limbs
a With increased reflexes and extensor plantar responses
b With absent reflexes
c Mixed upper motor neurone (in the legs) and lower motor neurone weakness (in the arms)
2 Weakness in both legs
a With increased reflexes and extensor plantar responses
b With absent reflexes in the legs
3 Unilateral arm and leg weakness
Upper motor neurone lesion in the high cervical cord, brainstem or above
• Contralateral sensory findings (pain and temperature loss) indicate lesion of half ipsilateral cervical cord lesion (Brown–Séquard) (see Chapter 21).
• Contralateral cranial nerve lesions or brainstem signs indicate the level of brainstem affected.
• Ipsilateral facial or tongue weakness indicate lesion above brainstem.
• Ipsilateral sensory loss indicate a lesion above the medulla.
• Visual field or higher function deficits indicate hemisphere lesion.
4 Syndromes limited to a single limb
Upper motor neurone signs limited to a single limb can be caused by lesions in the spinal cord, brainstem or cerebral hemisphere. Motor signs alone cannot distinguish between these possibilities. This relies on other signs—for example, cranial nerve or sensory abnormalities—or a diagnosis may not be possible without further investigation.
If lower motor neurone, common syndromes seen are as follows.
a Upper limb
Hand
(i) Median nerve: weakness and wasting of thenar eminence abductor pollicis brevis. Sensory loss: thumb, index and middle finger (Chapter 21).
(ii) Ulnar nerve: weakness with or without wasting of all muscles in hand excepting the LOAF. Sensory loss: little and half ring finger (Chapter 21).
(v) Bilateral wasting of small muscles:
Arm
(i) C5 root: weakness of shoulder abduction, external rotation and elbow flexion; loss of biceps reflex. Sensory loss: outer aspect of upper arm (Chapter 21).
(ii) C6 root: weakness of elbow flexion, pronation; loss of supinator reflex. Sensory loss: lateral aspect of forearm and thumb (Chapter 21).
(iii) C7 root: weakness of elbow and wrist extension; loss of triceps reflex. Sensory loss: middle finger (Chapter 21). N.B. cf. radial nerve.
(iv) C8 root: weakness of finger flexion; loss of finger reflex. Sensory loss: medial aspect of forearm (Chapter 21).
(v) Axillary nerve: weakness of shoulder abduction (deltoid). Sensory loss: small patch on lateral part of shoulder (Chapter 21).
b Lower limb
(i) Common peroneal palsy: weakness of foot dorsiflexion and eversion with preserved inversion. Sensory loss: lateral shin and dorsum of foot (Chapter 21). N.B. cf. L5 root.
(ii) L4 root: weakness of knee extension and foot dorsiflexion. Reflex loss: knee reflex. Sensory loss: medial shin (Chapter 21).
(iii) L5 root: weakness of foot dorsiflexion, inversion and eversion, extension of the big toe and hip abduction. Sensory loss: lateral shin and dorsum of foot (Chapter 21).
(iv) S1 root: weakness of plantar flexion, and foot eversion. Reflex loss: ankle reflex. Sensory loss: lateral border of foot, sole of foot (Chapter 21).
5 Variable weakness
6 Weakness that is not really there
Patients may appear weak when they are not, if:
• They find it difficult to understand what you want them to do (altered higher function).
• They are slow to initiate movements (bradykinesia as in Parkinson’s disease).
• They are not sure where their limb is due to proprioceptive loss.
If in doubt, re-examine them with these factors in mind.
WHAT IT MEANS
Myopathy (rare)
Causes
• Inherited: muscular dystrophies (Duchenne’s, Becker’s, fascio-scapular-humeral, myotonic dystrophy).
• Inflammatory: polymyositis, dermatomyositis, polymyalgia rheumatica.
• Endocrine: steroid-induced, hyperthyroid, hypothyroid.
• Metabolic: (very rare) glycogen storage disease (e.g. Pompe’s disease), McArdle’s disease.
Myasthenic syndromes (rare)
Mononeuropathies (very common)
Common causes
Radiculopathies (common)
Common causes
Peripheral neuropathies (common)
• Acute predominantly motor neuropathies: Guillain–Barré syndrome. Very rarely: diphtheria, porphyria.
• Chronic sensorimotor neuropathies:
– Acquired: diabetes mellitus; hypothyroidism; paraproteinaemias; amyloidosis.
– Inherited: hereditary motor and sensory neuropathy (Charcot–Marie–Tooth disease).
Mononeuritis multiplex (rare)
Polyradiculopathy (rare)
Indicates lesion to many roots. It is distinct from other peripheral neuropathies because it produces a more proximal weakness. The term is commonly applied to Guillain–Barré syndrome.
Spinal cord syndromes (common)
Sensory findings are needed to interpret the significance of motor signs indicating a spinal cord syndrome (see Chapter 21).
Brainstem lesions (common)
Hemisphere lesions (common)
Functional weakness
Difficult to assess. May be an elaboration of an underlying organic weakness. May indicate conversion disorder or other somatoform disorders; cf. functional sensory loss.

 TIP
TIP TIP
TIP TIP
TIP TIP
TIP