107
Morphea

Irregularly shaped sclerotic plaque of localized morphea. Note wax-like appearance, which is also yellow with a surrounding faint hue of pink.
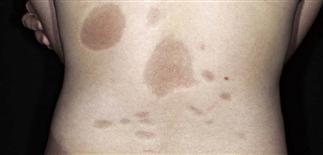
Multiple varying sized, hyperpigmented, light-brown patches of morphea on the back. These patches are soft and non-tender. The inflammatory process is no longer active.

En coup de sabre morphea on central forehead. A linear depressed sclerotic plaque extends from hairline to brow. Underlying soft tissue atrophy present. May be bony atrophy as well.

Violaceous oval patches of inflammatory phase of morphea. Skin biopsy was characteristic.
DESCRIPTION
Idiopathic disease manifesting as sclerotic dermal plaques with violaceous borders and central hypopigmentation. May be localized (more than two plaques) or generalized (more than three plaques). Generalized form accounts for 15%. Linear scleroderma accounts for 20% of localized scleroderma.
HISTORY
• More common in women than in men. • Mean onset, 32 years. • Onset slow and insidious or rapid and progressive. • Natural history unpredictable; lesions may spontaneously resolve after several years. • Although lesions may soften, hyperpigmentation often chronic. • Patients with generalized morphea may have asymptomatic internal organ involvement; evaluation is individualized.
PHYSICAL FINDINGS
• Early lesions are typically inflammatory and violaceous. Later lesions manifest hyperpigmentation, fibrosis, atrophy. • In generalized morphea, a large area may be involved; lesions often truncal but may involve extremities. • Linear scleroderma more common on extremities than on face. • En coup de sabre is term for linear scleroderma affecting forehead and scalp. In Parry–Romberg syndrome (progressive facial hemiatrophy), soft tissue and bony defects also apparent. • Skin biopsy can help confirm clinical diagnosis; biopsy to deep fat or fascia may be necessary if involvement is deep. • Eosinophilia common. • Antinuclear antibody commonly positive with generalized morphea.
TREATMENT
• As lesions may darken with sun exposure, advise sun protection. • Emollients may be comforting. • Education regarding the disease may be all that is required, because there is no reliable effective treatment. Reassure patient with plaque morphea that condition is benign, does not involve internal organs. • Mid- to high-potency topical steroid cream or ointment (group II or III) may be helpful in some cases to soften lesions and decrease pruritus. • Inflammatory lesions can be injected with intralesional triamcinolone 5–10 mg/mL; caution, as intralesional steroid injection may result in atrophy. • Calcipotriene ointment (Dovonex) twice daily can be used in adults and children; a reasonable trial of use is 8 weeks. • For rapidly progressing symptomatic disease, consider prednisone 20–40 mg q.d. for 6–8 weeks. Taper by 10 mg every other day if lesion improvement; this does not alter natural history. • Hydroxychloroquine 400 mg q.d. for 4-month trial is reasonable. If response, 200 mg q.d. maintenance dose considered. • Immune-suppressing medications, such as methotrexate or cyclosporine, may be used for short-term therapeutic trial of 3–6 months for inflammatory, symptomatic, and/or progressive disease. • Therapies with ultraviolet A1 (not widely available in USA), systemic or bath psoralen ultraviolet A reported effective in small uncontrolled trials.







