CHAPTER 23 Modular Bicompartmental Knee Arthroplasty
 Modular bicompartmental knee arthroplasty is an effective consideration for patients with bicompartmental disease, when there is reasonable range of knee motion, minimal deformity, and stable ligaments.
Modular bicompartmental knee arthroplasty is an effective consideration for patients with bicompartmental disease, when there is reasonable range of knee motion, minimal deformity, and stable ligaments.Introduction
Isolated unicompartmental knee arthroplasty (UKA) and patellofemoral arthroplasty (PFA) are effective for localized arthritis; however, arthritis commonly affects both the medial (or lateral) and patellofemoral compartments, and traditionally total knee arthroplasty (TKA) has been performed in those circumstances. While some have suggested that patellofemoral arthritis and symptoms can be ignored when performing UKA,1,2 others have not replicated that approach. Additionally, the presence of grade 3 or 4 chondromalacia in the medial or lateral compartments is a contraindication to PFA when treating patellofemoral arthritis, making TKA the conventional treatment.3
A disruptive evolutionary approach to tissue-sparing partial knee arthroplasty was introduced several years ago in the form of a monolithic bicompartmental knee arthroplasty, which resurfaces the medial and patellofemoral compartments, sparing the cruciate ligaments and lateral compartment.4 While the initial reception to the concept of bicompartmental knee arthroplasty was lukewarm, it is gaining interest and relevance as techniques improve, designs change, and results emerge. Two generic methods of bicompartmental knee arthroplasty are currently available—my preference is a modular approach, utilizing separate and unlinked UKAs and PFAs; the alternative, discussed in other chapters of this book, is either an off-the-shelf or custom monolithic prosthesis with a linked trochlear and unicondylar femoral segment. This chapter discusses the rationale for use of an unlinked modular bicompartmental knee arthroplasty and its clinical results.
Rationale for Bicompartmental Knee Arthroplasty
The rationale behind this strategy to knee arthroplasty is twofold. First, a large segment of patients undergoing TKA have isolated bicompartmental arthritis involving the medial (or lateral) and patellofemoral compartments and have no significant deformity, excellent motion, and intact cruciate ligaments. One radiographic study of 470 knees evaluated for osteoarthritis found that 50% had arthritis affecting both the medial and patellofemoral compartments, but sparing the lateral compartment, and that tricompartmental arthritis was rare.5 Often these patients are treated with TKA. While this is highly effective in providing considerable pain relief and survivorship, TKA patients often do not achieve the desired level of function and normalcy.6 This may be related to the altered kinematics of the knee following TKA, which tend to be relatively normal after UKA, PFA, and bicompartmental knee arthroplasty due to the retention of the anterior cruciate ligament and anatomic structures in the other compartments.7–9 Second, a number of knees treated with isolated patellofemoral or unicompartmental tibiofemoral arthroplasty will develop progressive arthritis in an un-resurfaced compartment of the knee over a period of time and are often converted to TKAs rather than adding a partial knee arthroplasty to the degenerated compartment. Staged modular bicompartmental arthroplasty may be a valid treatment method in these situations. However, despite its intuitive, rational philosophy, few data exist regarding how patients may fair if a modular stepwise approach to resurfacing is utilized rather than conversion to TKA in these patients.
Indications for Bicompartmental Knee Arthroplasty
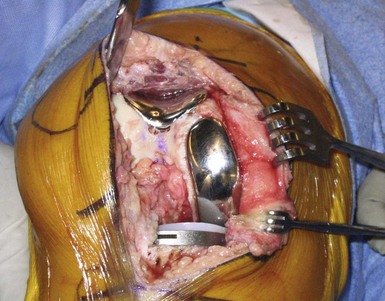
The indications for this procedure are similar to those used for UKA or PFA, with the addition of arthritis or painful chondromalacia in the “second” compartment (Fig. 23–1). Therefore, it can be used for patients with medial or lateral compartment and patellofemoral degenerative joint disease or painful chondromalacia, provided there is full extension (or less than a 5° flexion contracture), “good” range of motion (typically greater than 90° of flexion), minimal deformity, functional cruciate and collateral ligament stability, and an intact and painless “third” compartment. Further details of the indications for isolated unicompartmental and patellofemoral arthroplasty are given in their respective chapters in this book. While some surgeons may prefer to restrict this surgery to patients who are young and active, I have had great success in elderly patients and offer it to appropriate candidates without applying arbitrary age restrictions. Some surgeons have advocated isolated medial unicompartmental arthroplasty with a mobile-bearing implant design for bicompartmental arthritis involving the medial and patellofemoral compartments, in essence disregarding the arthritis and symptoms in the patellofemoral compartment.1,2 Berend et al.1 and Beard et al.2 have found that neither preoperative patellofemoral arthritis nor pain negatively impacts the results of the unicompartmental arthroplasty using a mobile-bearing implant. On the contrary, others have found that failures due to anterior knee pain will predictably occur when resurfacing only the medial compartment of the knee when there is also patellofemoral arthritis. Since the data regarding mobile-bearing knees in bicompartmental arthritis have not been replicated in other series (particularly those using fixed-bearing implants), and the rational explanation for the apparent absence of patellofemoral symptoms is elusive, my preference is to treat patients with bicompartmental arthritis and symptoms involving both the medial (or lateral) and patellofemoral compartments with modular bicompartmental arthroplasty (Figs. 23–2 and 23–3).
Rationale for Unlinked Modular Bicompartmental Knee Arthroplasty
With this philosophical approach to bicompartmental resurfacing, the varus-valgus alignment of the component is determined by the apposition of the lateral transitional edge of the trochlear component with the lateral femoral condyle. Given the variability in coronal alignment and morphology of the distal femur, there will be concomitant variability in how the implant can be aligned to ensure that the lateral edge of the trochlear prosthesis is flush with the lateral femoral condyle. This may compromise sizing and alignment of the condylar portion of the prosthesis. Certainly, an analysis of radiographs of the monolithic implant will show variability in the trochlear and condylar orientation relative to the distal femur with some components in varus, others in valgus, and others in neutral alignment relative to the femoral mechanical axis (Fig. 23–4). This malalignment can have detrimental implications for durability and functional outcomes. Except in ideal morphologies of the distal femur, it is rare to have both segments of the prosthesis (i.e., the trochlear and condylar segments) aligned and sized perfectly with a noncustomized monolithic prosthesis. Whether compromise in the alignment or position has deleterious implications on patellar tracking and midterm performance of the implant is not yet known; however, it may explain why one series of 42 monolithic bicompartmental knee arthroplasties reported 12% revisions and 25% anterior knee pain at short-term follow-up.10
The inherent challenges and concerns regarding use of a monolithic bicompartmental knee arthroplasty are further highlighted by a study of 117 computed tomography scans that identified considerable variability in the geometric relationships between the trochlear and medial or lateral femoral condylar surfaces.11 This study strengthens the argument for an unlinked modular approach to bicompartmental knee arthroplasty to optimize alignment and sizing of its individual components. Thus, the alternative approach to bicompartmental knee arthroplasty, and my personal preference, is a modular unlinked trochlear and medial femoral condylar prosthesis, which allows the individual compartmental resurfacing procedures to be performed “independent” of each other, ensuring appropriate orientation and alignment of the individual components relative to the critical axial and rotational axes of the distal femur, without having to compromise implant position based on how the component is positioned in the other compartment (see Figs. 23-2 and 23-3). This also allows size interchangeability between compartments to accommodate potential variability in femoral geometry and aspect ratios between patients and compartments of the knee. The modular approach to bicompartmental resurfacing is also highly compatible with robotic assistance for bone preparation and three-dimensional preoperative planning.12
When performing modular bicompartmental resurfacing, the gap between the transitional edge of the trochlear component and the proximal edge of the femoral component of the unicompartmental arthroplasty may vary in size. This distance may be as little as 1 mm and as large as 10 mm depending on the distal femoral shape and size (see Fig. 23–2). Problems with the transitional gap between the trochlear and condylar prostheses have not been observed with independent resurfacing, provided the implants are appropriately positioned flush with or recessed approximately 1 mm relative to the articular cartilage. Prominent edges could result in patellar prosthesis catching or snapping over the implants and should therefore be avoided. Implant edge prominence can result from technical errors or trochlear implant design features.13 Malaligned, malpositioned, improperly sized trochlear components or those that do not rest flush with the condylar surfaces can impact patellar tracking and have consequences relative to patellar tracking and short- and long-term success of bicompartmental arthroplasty.
Clinical Results of Modular Bicompartmental Knee Arthroplasty
Gait analysis and isokinetic strength tests indicate that normal knee mechanics and gait are restored after bicompartmental knee arthroplasty.9 Early clinical results of bicompartmental knee arthroplasty have shown excellent pain relief and knee function and restoration of appropriate knee alignment.4,14–18 Recipients can commonly rise independently and ascend stairs reciprocally.9,16 However, since the procedure is relatively new, long-term outcomes have still to be established.
There have been several recent reports on the results of modular unlinked bicompartmental knee arthroplasty. Heyse et al. reported on nine knees in nine patients with an average age at surgery of 64 ± 5 years treated with medial UKA and PFA.15 Three procedures were performed in a staged fashion, with a mean of 5 years between UKA and PFA. At a mean follow-up of 12 ± 5 years (range, 4–17 years), no revision surgeries were necessary, although one asymptomatic patient had substantial progression of lateral arthritis. The Knee Society knee score increased from 39 ± 24 preoperatively to 92 ± 10 (p = .007), and the Knee Society Functional Score increased from 30 ± 9 preoperatively to 83 ± 18 (p = .002), at latest follow-up (p = .002). Mean range of motion increased from 107° to 121° (p = .04), and all patients were satisfied or very satisfied.15 Mahoney et al. reported on short-term experience with 17 unlinked UKAs and PFAs, observing mild or no pain and greater than 120° of flexion in all patients.16 In that series, all patients were able to rise unassisted and ascend stairs in a reciprocal manner. There were no cases of incompatibility between the UKA or PFA components.16 John et al. reviewed the initial 30 consecutive modular unlinked bicompartmental UKA/PFAs performed by this author and found that, at a minimum 1-year follow-up (range, 1–2.5 years), the WOMAC pain score decreased from 11.0 to 2.8 (p = .0001), the WOMAC function score decreased from 13.6 to 3.2 (p = .0008), the WOMAC total score decreased from 24.6 to 6.0 (p = .0001), range of motion increased from 122° to 138° (p = .0001), and Knee Society Functional and Knee scores increased from 56 to 92 and 40 to 88, respectively (p = .0001). There were no perioperative complications and no radiographic evidence of loosening, polyethylene wear, or progressive arthritis of the lateral tibiofemoral compartment.17
Despite these encouraging results, the outcomes of bicompartmental knee arthroplasty can be compromised by poor implant design, component malalignment or malposition, improper patient selection, and progressive arthritis of the un-resurfaced compartment. In a series by Parratte et al., 6 of 77 knees treated with combined medial UKA and PFA developed asymptomatic progression of lateral compartment osteoarthritis at a mean 12-year follow-up. No revisions were necessary for arthritis progression, and in those surviving prostheses, there was substantial improvement in pain, function, and knee scores. However, in that series 27 knees failed at a mean of 8 years (range, 11 months to 22 years) due to aseptic loosening of the trochlear component (n = 20) and the tibial component (n = 7). Of the trochlear components that failed, 15 were cementless. Despite these failures, those authors continue to advocate for modular bicompartmental knee arthroplasty, recognizing that cementless trochlear component fixation, crude instrumentation and techniques, and poor polyethylene quality and implant designs were responsible for aseptic loosening in the series.14 The high rate of trochlear component failures in isolated PFAs with the same design used in the series by Parratte et al.14 was noted in previous series.19 Further study with newer techniques and designs will determine whether long-term durability compares to that of TKA. Certainly contemporary reports of improved early functionability and outcomes with bicompartmental knee arthroplasty are encouraging.4,12,17
Staged Bicompartmental Resurfacing
Another novel concept to consider is a staged approach to bicompartmental arthroplasty for progressive arthritis after unicompartmental or patellofemoral arthroplasty. After UKA, the development or progression of symptomatic patellofemoral arthritis may occur in 7–10% of patients at 10–15 years.20,21 Additionally, after PFA 10–25% of patients may develop progressive tibiofemoral arthritis at 7–16 years.19,22–24 Typically these patients are treated with revision to TKA. It makes intuitive sense that, in those patients with an isolated patellofemoral or unicompartmental arthroplasty, progressive degeneration of one of the un-resurfaced compartments of the knee can be treated with staged single-compartment resurfacing, rather than conversion to TKA, thereby performing a staged modular bicompartmental arthroplasty. However, despite one study that included three patients who underwent staged modular bicompartmental knee arthroplasty,15 there are no published data that review the results of this method of treatment as an alternative to revision to TKA.
1 Berend KR, Lombardi AV, Adams JB. Obesity, young age, patellofemoral disease, and anterior knee pain: identifying the unicondylar arthroplasty patient in the United States. Orthopedics. 2007;5(Suppl):19-23.
2 Beard DJ, Pandit H, Ostlere S, et al. Preoperative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br]. 2007;89:1602-1607.
3 Lonner JH. Patellofemoral arthroplasty. J Am Acad Orthop Surg. 2007;15:495-506.
4 Rolston L, Bresch J, Engh G, et al. Bicompartmental knee arthroplasty: a bone-sparing, ligament-sparing, and minimally invasive alternative for active patients. Orthopedics. 2007;30(8 Suppl):70-73.
5 Ledingham J, Regan M, Jones A, Doherty M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann Rheum Dis. 1993;52:520-526.
6 Noble PC, Gordon MJ, Weiss JM, et al. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;435:157-165.
7 Patil S, Colwell CWJr, Ezzet KA, D’Lima DD. Can normal knee kinematics be restored with unicompartmental knee replacement? J Bone Joint Surg [Am]. 2005;87:332-338.
8 Suggs JF, Park SE, Steffensmeier S, et al. Function of the anterior cruciate ligament after unicompartmental arthroplasty: an in vitro robotic study. J Arthroplasty. 2004;19:224-229.
9 Wang H, Dugan E, Frame J, Rolston L. Gait analysis after bi-compartmental knee replacement. Clin Biomech. 2009;24:751-754.
10 Tria AJJr. Bicompartmental arthroplasty of the knee. Instr Course Lect. 2010;59:61-73.
11 Banks SA, Abbasi A, Van Vorhis R, et al. Morphology of the distal femur for bicompartmental arthroplasty. Presented at the Annual Meeting of the American Academy of Orthopedic Surgeons. 2010.
12 Lonner JH. Modular bicompartmental knee arthroplasty with robotic arm assistance. Am J Orthop. 2009;38(2 Suppl):28-31.
13 Lonner JH. Patellofemoral arthroplasty: the impact of design on outcomes. Orthop Clin North Am. 2008;39:347-354.
14 Paratte S, Pauly V, Aubaniac JM, Argenson JN. Survival of bicompartmental knee arthroplasty at 5–23 years. Clin Orthop Relat Res. 2010;468:64-72.
15 Heyse TJ, Khefacha A, Cartier P. UKA in combination with PFR at average 12-year follow-up. Arch Orthop Trauma Surg. 2010;130:1227-1230.
16 Argenson JN, Parratte S, Bertani A, et al. The new arthritic patient and arthroplasty options. J Bone Joint Surg [Am]. 2009;91(Suppl 5):43-48.
17 John T, Sheth N, Lonner JH. Modular bicompartmental arthroplasty of the knee. Presented at the Annual Meeting of the Knee Society, September 2010.
18 Rolston L, Siewert K. Assessment of knee alignment after bicompartmental knee arthroplasty. J Arthoplasty. 2009;24:1111-1114.
19 Argenson JN, Flecher X, Parratte S, Aubaniac JM. Patellofemoral arthroplasty: an update. Clin Orthop Relat Res. 2005;440:50-53.
20 Kahn OH, Davies H, Newman JH, Weale AE. Radiological changes ten years after St. Georg Sled unicompartmental knee replacement. Knee. 2004;11:403-407.
21 Berger RA, Meneghini RM, Sheinkop MB, et al. The progression of patellofemoral arthrosis after medial unicompartmental replacement: results at 11 to 15 years. Clin Orthop Relat Res. 2004;428:92-99.
22 Cartier P, Sanouiller JL, Khefacha A. Long-term results with a first patellofemoral prosthesis. Clin Orthop Relat Res. 2005;436:47-54.
23 Nicol SG, Loveridge JM, Weale AE, et al. Arthritis progression after patellofemoral joint replacement. Knee. 2006;13:290-295.
24 Kooijman HJ, Driessen APPM, VanHorn JR. Long-term results of patellofemoral arthroplasty: a report of 56 arthroplasties with 17 years of follow-up. J Bone Joint Surg [Br]. 2003;85:836-840.