Chapter 35 Modified uvulopalatopharyngoplasty with uvula preservation
1 INTRODUCTION
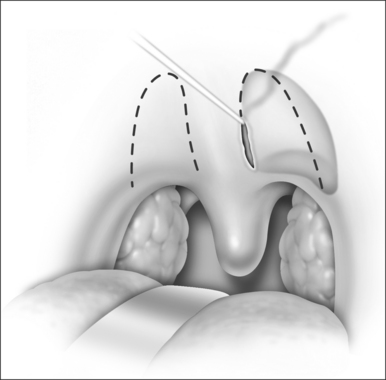
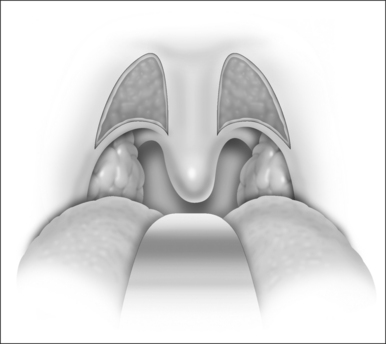
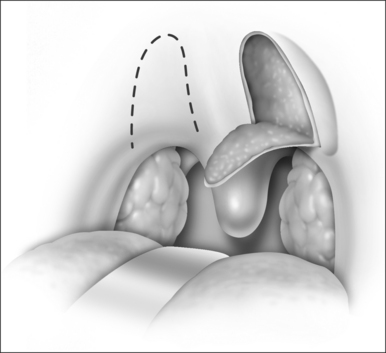
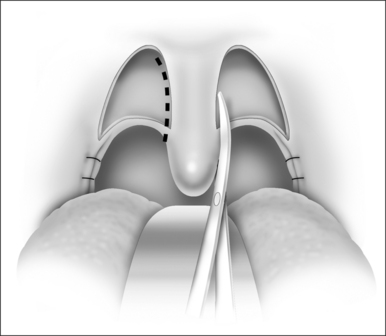
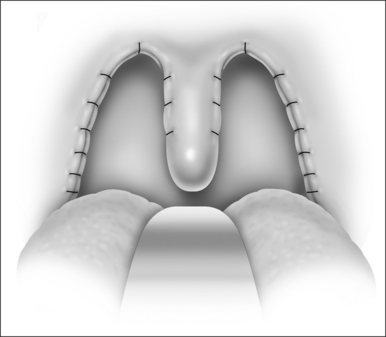
A narrow upper airway is one of the main causes of obstructive sleep apnea/hypopnea syndrome (OSAHS). Uvulopalatopharyngoplasty (UPPP), which ablates both the two tonsils and part of the redundant soft palate to decrease the oropharyngeal obstruction, is still the most widely used surgery. Unfortunately there are about 50% non-responders to UPPP for unselected patients and the classic UPPP has complications such as palatopharyngeal incompetence and palatopharyngeal stenosis. To reduce the UPPP complication rate without compromising the surgical response, the first author designed a new method of UPPP, in which the uvula is preserved, a larger portion of the soft palate is removed, and the basic structure of the oropharyngeal cavity is maintained. This revised UPPP with uvula preservation was first introduced by Han Demin in 2000 and was named Han-UPPP (H-UPPP). H-UPPP is widely used in China and has been proved to be an effective surgical method, causing fewer complications compared with classic UPPP.
2 PATIENT SELECTION
2.1 INDICATIONS
3 CLINICAL EVALUATION AND PREOPERATIVE MANAGEMENT
4 TECHNIQUES
5 POSTOPERATIVE MANAGEMENT
6 CLINICAL OUTCOMES AND COMPLICATIONS
6.2 THE SIGNIFICANCE OF UVULA PRESERVATION
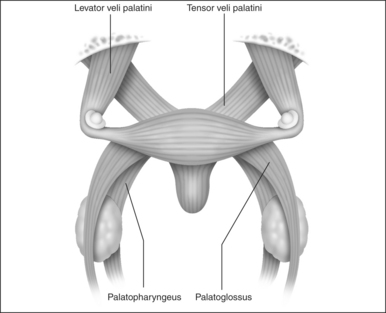
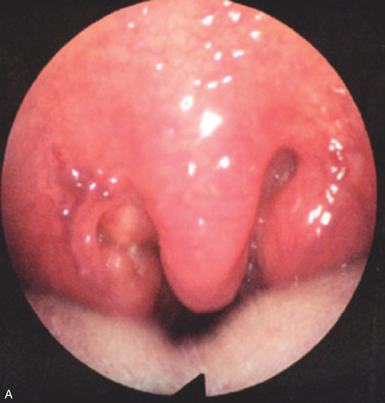
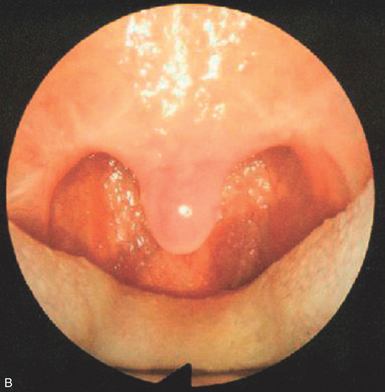
The long uvula becomes a ‘normal’ one through contraction of scar tissue of the soft palate and the bilateral sides of the palato-uvularis and the lower margin of the tensor palatini (Fig. 35.8 A&B). The uvula has important functions like deglutition, respiration, speech and pharyngeal airway dilation. Zakkar found that there is highly concentrated neutral endotryptase in the uvula of normal subjects, but decreased levels in the membrane of the uvula in OSAHS patients, and it is speculated that the uvula is where airflow receptors are distributed. The preservation of the uvula would seem to be very important to maintain the pharyngeal airway muscular tension and normal physiologic functions. To safeguard these important functions, the intact uvularis and its corresponding mucosal membrane (both dorsal and ventral) are preserved. The results show that H-UPPP effectively enlarges the oropharyngeal cavity and avoids some major postoperative complications of classic UPPP.
6.3 CLINICAL OUTCOMES AND FACTORS INFLUENCING SURGICAL EFFECTIVENESS
It has been reported that successful responders to UPPP amount to 33–77%, but the criteria for patient selection and successful surgical response definitions are not the same between studies. The response rate of H-UPPP was 51.9–69.12%, defined as a >50% reduction of the AHI or AHI < 20/h postoperatively. In patients who have been carefully selected for upper airway reconstruction and whose site of primary obstruction is at the oropharyngeal level, the surgical response rate is 68.57–90%.
Demin H, Jingying Y, Jun W, et al. Determining the site of airway obstruction in obstructive sleep apnea with airway pressure measurements during sleep. Laryngoscope. 2002;112(11):2081-2085.
Dickson RI, Mintz DR. One-stage laser assisted uvulopalatoplasty. J Otolaryngol. 1996;25:155-162.
Esclamado RM, Glenn MG, McCulloch TM, et al. Perioperative complications and risk factors in the surgical treatment of obstructive sleep apnea syndrome. Laryngoscope. 1989;99:1125-1129.
Fujita et al. Fujita S, Convey W, Zorick, F, et al. Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 181:89:923–34.
Han Demin, Ye Jingying, Lin Zhonghui, et al. Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study. J Otorhinolaryngol Relat Spec. 2005;67(4):213-219.
Han DM, Ye JY, Li YR, et al. Preoperative overnight airway pressure measurement for predicting the outcome of revised uvulopalatopharyngoplasty. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2006;41(10):753-758.
Huang MH, Lee ST, Rajendran K. Structure of the musculus uvulae: functional and surgical implications of an anatomic study. Cleft Palate Craniofac J. 1997;34(6):466-474.
Isono S, Remmers JE. Anatomy and physiology of upper airway obstruction. In: Kryger MH, et al, editors. Principles and Practice of Sleep Medicine. 3rd edn. Philadelphia: WB Saunders; 2000:840-858.
Li YR, Han DM, Ye JY, et al. Sites of obstruction in obstructive sleep apnea patients and their influencing factors: an overnight study. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2006;41(6):437-442.
Loube DI. Uvulopalatopharyngoplasty may compromise nasal CPAP therapy in sleep apnea syndrome. Am J Respir Crit Care Med. 1996;154:1759-1762.
Meiljetaig H, Mataika S, Haight JS, et al. Subjective and objective assessment of uvulopalatopharyngoplasty for treatment of snoring and sleep apnea. Is J Respir Crit Care Med. 1994;150:1286-1290.
Mortimore IL, Bradley PA, Murray JAM. Uvulopalatopharyngoplasty may compromise nasal CPAP therapy in sleep apnea syndrome. Is J Respir Crit Care Med. 1996;154:1759-1762.
Powell N, Riley R, Guilleminault C, Troell R. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep. 1996;19(7):593-599.
Rennotte MT, Baele P, Aubert G, et al. Nasal continuous positive airway pressure in the perioperative management of patients with obstructive sleep apnea submitted to surgery. Chest. 1995;107:367-374.
Riley RW, Powell NB, Li KK, et al. Surgical therapy for obstructive sleep apnea–hypopnea syndrome. In: Kryger MH, et al, editors. Principles and Practice of Sleep Medicine. 3rd edn. Philadelphia: WB Saunders; 2000:913-928.
Series F, Cote C, Simoneau JA, Gelinas Y, et al. Physiologic, metabolic, and muscle fiber type characteristics of musculus uvulae in sleep apnea hypopnea syndrome and in snorers. J Clin Invest. 1995;95(1):20-25.
Series F, Simoneau JA, St Pierre S. Muscle fiber area distribution of musculus uvulae in obstructive sleep apnea and non-apneic snorers. Int J Obes Relat Metab Disord. 2000;24(4):410-415.
Van Duyne J, Coleman JAJr. Treatment of nasopharyngeal inlet stenosis following uvulopalatopharyngoplasty with the CO2 laser. Laryngoscope. 1995;105(9 Pt 1):914-918.
Wang J, Han D, Lin Z, et al. Clinical study of uvulopalatopharyngoplasty treatment for middle degree of obstructive sleep apnea syndromes. Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2003;17(2):84-85.
Ye JY, Han DM, Wang J, et al. Computer assisted fiberoptic pharyngoscopy in obstructive sleep apnea syndrome. Chin Arch Otolaryngol Head Neck Surg. 2004;11:371-375.
Zakkar M, Sekosan M, Wenig B, et al. Decrease in immunoreactive neutral endopeptidase in uvula epithelium of patients with obstructive sleep apnea. Ann Otol Rhino Laryngol. 1997;106:474-477.