CHAPTER 18 Mobile-Bearing Uni
Long-Term Outcomes
Introduction: Prosthesis Design
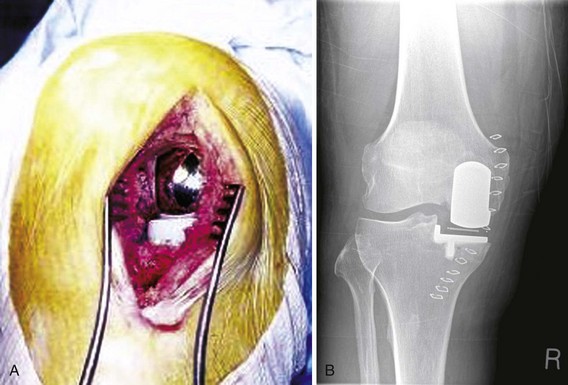
The implant most commonly used is the Oxford unicompartmental knee replacement.1 This design was originally used as a bicompartmental device but was first used as a unicompartmental device in 1982 (Phase 1). Since then two further design phases have been introduced, retaining the design features while improving the instrumentation and the method of implantation. In Phase 1 the femoral surface was prepared with cutting blocks to remove angular cuts of bone to fit the nonarticular surface of the femoral component. However, this did not allow accurate balance of the flexion-extension gap at implantation, and the Phase 2 prosthesis was introduced in 1987 and sought to improve this. The femoral component was changed to a spherically concave inner surface and the femoral bone surface was prepared with a mill rotating around a spigot. Incremental 1-mm milling of the distal femoral surface allows careful balancing of the knee ligaments throughout flexion (Fig. 18–1). The Phase 3 design, introduced in 1998, provided new instruments and an increased range of components to facilitate the implantation through a short incision. The aim was to gain the short-term advantages associated with this less invasive incision2 while maintaining the longer term survival, by maintaining the original design features of the fully congruent articulation (Fig. 18–2). Although the Oxford mobile-bearing unicompartmental knee was the first of its kind, there are several other mobile-bearing knees based on a similar philosophy. The AMC knee (Uniglide) utilizes a fully mobile bearing restoring the natural tension within the knee; however, there is a difference in the shape of the femoral component. The radius of the femoral component is constant up to 45° of flexion but decreases toward the posterior portion of the condyle.
We have reviewed the long-term results of the prostheses mentioned above. There is substantial literature regarding the Oxford Knee and more limited literature about the other prosthesis. Long-term outcome is an important factor since impressive early results of an implant may dramatically change with longer term follow-up. For example, in the PCA fixed-bearing unicompartmental prosthesis, 90% of patients were reported as having a satisfactory functional result at 2 years,3 yet the cumulative survival at 3.7 years was only 77%.4 Our aim is to review the long-term results, at 10 years and greater, of mobile-bearing unicompartmental replacements.
Measuring Outcome: Explanation of Study Types
Assessing Survivorship
The measurement of success in arthroplasty surgery is important to provide information not only for the surgeon selecting the type of surgery and individual prosthesis to use but also when counseling patients regarding expected outcome from an intervention. The most commonly used measure of success is the survival of the implant (time to revision), but it is also important to assess the functional outcome of the arthroplasty in surviving patients, since this provides more complete information regarding the success of the patients’ treatment than pure survival analysis.5 Modern survival analysis will define a failure end point and provide an assessment of how many patients failed and how long after the operation this failure occurred. It is therefore important to understand the exact nature of the defined end point in each study as some authors use removal of the implants as the failure end point, whereas others use further surgery of any type. The difference between the two end points may affect the reported survival. Survival analysis may be performed using the life table method or Kaplan-Meier method. Whichever is employed, there are a number of features that must be understood about the reported data. Survival figures are cumulative, which allows a prediction of the expected failure rate in the long term, reducing the need for large numbers of prostheses to have reached the long-term follow-up point. However, the number at risk at each time point must be known since, if this number reduces to less than 15, it becomes difficult to interpret the data. Loss to follow-up is also important, and studies should present worst- and best-case scenarios.
Study Types
Joint Registers
The prime function of registers is to assess the success of treatment in large, often nationwide, population-based cohorts. They provide data that represent clinical practice without the inherent bias in cohort studies and can be used to compare outcome of implant designs. For this reason, registers have always taken “revision” as the marker of failure and the “cumulative revision rate” as the comparator between implants. While revision is an event that will invariably bring a patient back into contact with a surgeon and is therefore easily measured, there are some difficulties with the interpretation of the revision rates. Unfortunately, arthroplasty registers collect few data and exert no control over patient selection, surgical expertise, and indication for revision. The term surgical routine was defined by Robertsson et al.6 in 2001 to describe these factors, and it was shown that the revision rate in centers that performed fewer than 23 unicompartmental knee arthroplasties (UKAs) annually had a risk of revision 1.63 times higher than centers with higher volumes of work. Over the last 10 years, the New Zealand Joint Registry has introduced patient-reported outcome data (PROMS) into the joint register. This allows additional information to be gained regarding true clinical outcome and patients’ functional score at the time of revision surgery, which offers an improved assessment of the true success of arthroplasty. Analysis of these data shows that, in every category of clinical outcome, a UKA is between four and six times as likely to be revised as a total knee arthroplasty (TKA). This highlights the problem of using registry data to compare between UKA and TKA, whereas a comparison between UKA designs is more relevant.
What Is Long-Term Outcome?
Ideally long-term outcome would reflect the results and outcome of all patients for their entire lifespan—in other words, when the patient is either dead or revised. There are currently no such studies on UKA; therefore, the next best assessment is a prediction of the “real” long-term outcome, and this is best achieved by survivorship analyses. Ten-year survivorship analysis has always been the gold standard for assessment of a prosthesis. For example, in the United Kingdom there is a 10-year benchmark of no more than 10% failure rate at 10 years.7 The next step toward better understanding of long-term outcome is to assess 20-year survivorship data. In truth, there are only a few studies available that allow assessment in the second decade; there are many more studies that report follow-up at less than 10 years, and these shorter term survivorship analyses can still provide valuable information that may guide surgical practice.
Lessons Learned from Midterm Assessment
There have been published series with midterm results that have then not reported results at long term. However, there are still valuable lessons that can be learned from these midterm results that are relevant to long-term outcome, and we highlight these here. Kort et al.8 assessed 130 patients with Phase 3 Oxford UKAs in an eight-surgeon series, with all surgeons performing less than 10 procedures per year. The overall survival is reported at 89%, with a range of follow-up of 2–7 years, but with no indication of how this survival figure was reached. Interestingly, of the 17 failures, they attribute 13 to human error of component malalignment and two further cases of trauma and infection. Thirty-seven patients had preoperative lateral compartment joint space narrowing and one patient had lateral joint space obliteration preoperatively. As a result, this center now closely adheres to the prosthesis guidelines and focuses all the UKAs to be performed by two of their surgeons. This study demonstrates that the indications for surgery, implantation technique, and surgical expertise are all relevant to midterm and therefore long-term outcome. Similarly, in a study of 437 patients with Phase 3 implants, Kuipers et al.9 reported a cumulative survival of 84.7% (confidence interval [CI], 80.1–89.3%) at 5 years (mean, 2.6 years), with 101 still at risk. Each surgeon in the study performed an average of 8 UKAs per year, and, interestingly, the authors noted that almost a quarter of their revisions were for continuing unexplained pain with no evidence of prosthesis malfunction and no mention as to whether the function improved post-revision. The authors concede these may have been unnecessary revisions. These results reinforce that patient selection and surgical routine are important determinants of early to midterm outcome and therefore must influence long-term outcome. Specifically, integrity of the anterior cruciate ligament (ACL) and preservation of the lateral compartment are important, as outlined in the published guidelines for UKA.1,10 When the indications are followed, the results can be excellent, as demonstrated by Pandit et al.,11 who assessed 688 patients with 96.5 cases at risk at 5 years and a cumulative survival rate of 97.3%.
The only comparisons of fixed versus mobile bearings unfortunately do not have long-term follow-up. Confalonieri et al.12 described a cohort of 40 consecutive patients randomly assigned to a fixed-bearing knee (Allegretto) or a mobile-bearing knee (AMC). There was no statistical difference in the outcome between the two groups, although one of the fixed bearings was revised while none of the mobile bearings were revised and none of the bearings had dislocated. Gleeson et al.13 randomized 47 patients to a mobile-bearing UKA (Oxford) and 57 to a fixed-bearing UKA (St. Georg Sled). At a mean of 4 years, four knees in the mobile-bearing group and three knees in the fixed-bearing group had been revised.
Long-Term Outcome
Registry Data
Three registers—the Swedish Knee Arthroplasty Register, the Finnish Arthroplasty Register, and the Australian Orthopaedic Association register—report on specific data for the Oxford UKA at approximately the 10-year time point, and we summarize the most recent outcome data from these registers. Several of the other registers, such as the New Zealand and the Norwegian registers, do not report separate outcome for fixed and mobile, nor in some cases medial and lateral, unicompartmental replacements, and the United Kingdom National Joint Registry presently reports revision rate for specific implants at only 3 years. Therefore, they are not included here. In the 2009 annual report of the Swedish Knee Arthroplasty Register,14 the cumulative 8-year survival for the Oxford replacement was greater than 91%. The Australian Orthopaedic Association joint registry data from 200915 reported a cumulative survival of 87.1% at 8 years. The Finnish Arthroplasty Register reported a 10-year survival of 81% for the Oxford UKA,16 slightly better than for a fixed-bearing device (79%, Miller-Galante). There is no more detailed information in these reports for mobile-bearing UKA. At other time points, important information has come from the registry data. In 1998, Lewold et al.17 reported the cause for revision of all unicompartmental replacement in the Swedish Knee Arthroplasty Register up to 10 years. This cited the most common cause for revision as component loosening and the second most common as contralateral compartment progression. Unfortunately, these are merged data for all types of unicompartmental replacement, with the most common being fixed-bearing devices, so the extrapolation to mobile-bearing devices is difficult. Prior to this the same authors did report the cause for revision at 6 years in the Oxford knee.18 Although these were not long-term data, they did show a proportionally high rate of dislocated bearings and loosening. These observations led one of the coauthors to later describe the absolute importance of good surgical routine, mentioned in the previous section.6
Cohort Studies
Ten-Year Studies
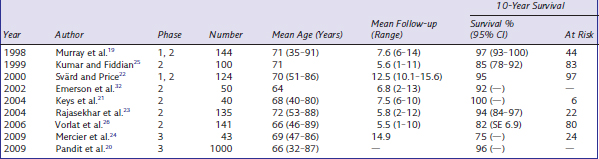
Ten-year follow-up of the Oxford prosthesis is reported in nine studies (Table 18–1), and there is a wide range in the reported survival. Six of the nine studies at 10 years reported a cumulative survival of 94% or greater; however, three series report a cumulative survival of 85% or less. The inventor series of Murray et al.19 for the Phase 1 and 2 Oxford knee reported a 10-year cumulative “worst-case” survival rate of 97% (CI, 93–100%). Forty-four knees remained at risk at 10 years, and no failures were due to polyethylene wear or aseptic loosening of the tibial component. Pandit et al.20 reported the inventor series of the Phase 3 Oxford knee with 1000 patients and a 96% cumulative revision rate at 10 years. Keys et al.21 reported their first 40 Phase 3 Oxford UKAs, also with excellent results, supporting the results of the inventor series. The average follow-up was 7.5 years and the survivorship at 10 years was 100% with no losses to follow-up. In another independent series of the Phase 1 and 2 knees, Svärd and Price22 showed a cumulative survival of 124 patients at 10 years of 95%, with an average follow-up of 12.5 years and no losses to follow-up. Rajasekher et al.23 showed similar results, with 94% cumulative survival of the Phase 2 knee at 10 years.
Other cohorts do not reveal similar success with the implant. Mercier et al.24 report an overall survival of 74.7%. However, they specifically draw attention to their broad selection criteria, including ACL-deficient knees and inflammatory arthropathy. When these cases are excluded, the 10-year survival is improved to greater than 85%. In similar fashion, Kumar and Fiddian25 reported a 10-year survival of 85% (CI, 78–92%) and a mean follow-up of 5.6 years. Again they noted that initial patient selection, such as inflammatory arthropathy, led to four of the seven failures, and functional assessment showed that 98% of all patients were pleased or satisfied with the outcome of their surgery. Vorlat et al.26 showed the effect of previous high tibial osteotomy (HTO) on the outcome of Oxford UKA. Overall, the cumulative survival at 10 years was 82%; however, four of the failures were in eight patients who had previously undergone HTO (two cases for lateral progression and two for unspecified reasons), and when these were excluded the results improved.
Twenty-Year Studies
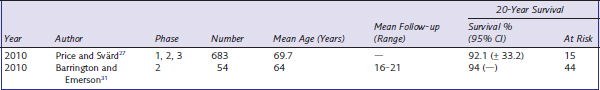
There are only two studies that reported 20-year survival (Table 18–2). Price and Svärd27 reported the continuation and further accumulation of the Svärd and Price 10-year study22 (also reported at 15 years28). The strength of this series is that it includes all cases performed with no loss to follow-up. Six hundred eighty-three consecutive knees were assessed and the overall cumulative survival was 92% at 20 years. The most common cause for revision was progression of arthritis in the lateral compartment, although over the 20-year period this only occurred in 10 patients or 1.5% of cases. While previous studies have shown that overcorrection of the varus deformity may lead to relatively rapid progression of lateral compartment disease,29 the low rate of progressive lateral arthrosis in this study shows that this is an uncommon feature with the Oxford UKA. This is supported by previous work by Weale et al.30 In addition, there were no failures attributable to patellofemoral joint problems, which is of note since preoperative patellofemoral disease was not a contraindication to unicompartmental replacement in this study. This study also reinforces the message that adhering to the present-day indications improves outcome since in a subgroup with previous HTO or ACL deficiency (included in the overall results) the failure rate was 71%. The most interesting feature of the Svärd and Price series is the relatively few failures that occur in the second decade. Infection and dislocation appear to be relatively early complications of this procedure, and lateral compartment osteoarthritis and loosening account for the majority of midterm failures. However, only three cases required revision in the second decade, two for lateral progression and one for femoral loosening. Of note, no failures in the second decade were due to polyethylene wear, suggesting that the design features of the implant in reducing contact stress as a design against wear can be successful. The 20-year results of Barrington and Emerson31 reinforce those of Svärd and Price. Their survivorship was 94% with no revisions for bearing dislocation, tibial subsidence, or polyethylene wear. They also reported excellent functional scores, with mean Knee Society scores improving from 47 preoperatively to 94 postoperatively.
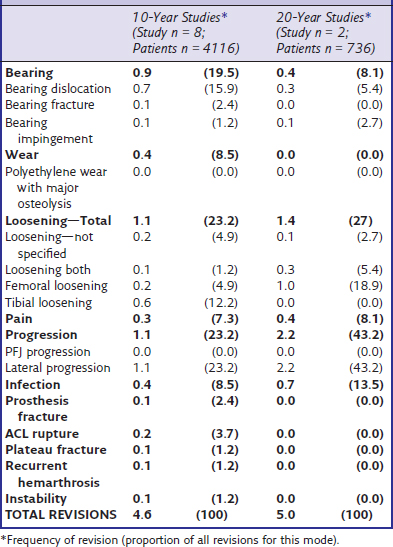
The modes of failure for the 10-year and 20-year studies are listed on Table 18–3. Perhaps unsurprisingly, lateral progression becomes a higher proportion of total failures as time progresses, but it still only affects 0.11% per year of follow-up.
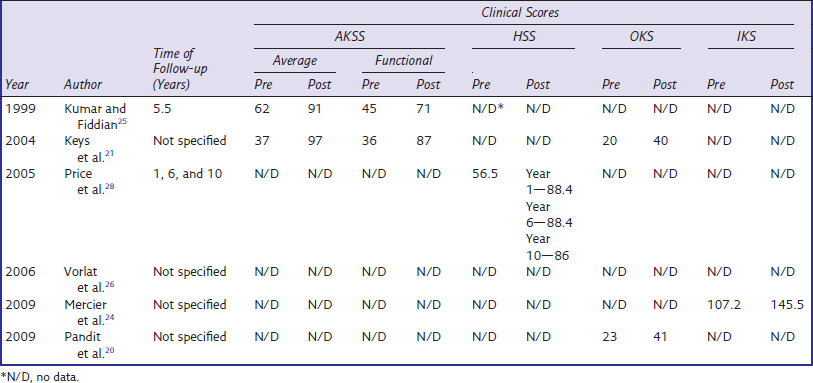
Clinical Outcome
Very few long-term clinical outcome data are reported; those that are available are summarized in Table 18–4. In assessing the few studies available, it is clear there is no consistency of the clinical outcome assessment used, making generalized interpretation difficult. However, all of the clinical scores significantly improve from postoperation to final follow-up. Price et al.28 did report robust longitudinal data from 1, 6, and 10 years postoperatively. Interestingly, this shows that the significant increase in clinical scores does not decrease with time; in other words, patient function is just as good 10 years postoperatively as at 1 year.
1 Goodfellow J. Unicompartmental Arthroplasty with the Oxford Knee. Oxford: Oxford University Press; 2006.
2 Rees JL, Price AJ, Beard DJ, et al. Minimally invasive Oxford unicompartmental knee arthroplasty: functional results at 1 year and the effect of surgical inexperience. Knee. 2004;11:363-367.
3 Magnussen PA, Bartlett RJ. Cementless PCA unicompartmental joint arthroplasty for osteoarthritis of the knee: a prospective study of 51 cases. J Arthroplasty. 1990;5:151-158.
4 Harilainen A, Ylinen P, Sandelin J, Vahvanen V. Survival analysis and predictors of failure in unicompartmental knee replacement using a PCA prosthesis. Knee. 1995;1:201-207.
5 Price AJ, Longino D, Rees J, et al. Are pain and function better measures of outcome than revision rates after TKR in the younger patient? Knee. 2010;17:196-199.
6 Robertsson O, Knutson K, Lewold S, Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg [Br]. 2001;83:45-49.
7 Medical Devices Agency NIfCE, British Orthopaedic Association. Post-market surveillance of CE marked joint replacement implants including guidance to manufacturers on postmarket clinical studies. EC Medical Devices Directive. London: British Orthopaedic Association; 2000.
8 Kort NP, van Raay JJ, van Horn JJ. The Oxford phase III unicompartmental knee replacement in patients less than 60 years of age. Knee Surg Sports Traumatol Arthrosc. 2007;15:356-360.
9 Kuipers B, Kollen B, Kaijser Bots P, et al. Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee. 2010;17:48-52.
10 Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg [Am]. 1989;71:145-150.
11 Pandit H, Jenkins C, Barker K, et al. The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg [Br]. 2006;88:54-60.
12 Confalonieri N, Manzotti A, Pullen C. Comparison of a mobile with a fixed tibial bearing unicompartimental knee prosthesis: a prospective randomized trial using a dedicated outcome score. Knee. 2004;11:357-362.
13 Gleeson RE, Evans R, Ackroyd CE, et al. Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee. 2004;11:379-384.
14 Lidgren L, Robertsson O, Dahl A. Swedish Knee Arthoplasty Register—Annual Report. Lund: Swedish Knee Arthoplasty Register; 2009. pp 30-34
15 Graves S. Australian Orthopaedic Association National Joint Registry—Annual Report. Adelaide: Australian Orthopaedic Association; 2009. pp 112-124
16 Koskinen E, Paavolainen P, Eskelinen A, et al. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128-135.
17 Lewold S, Robertsson O, Knutson K, Lidgren L. Revision of unicompartmental knee arthroplasty: outcome in 1,135 cases from the Swedish Knee Arthroplasty study. Acta Orthop Scand. 1998;69:469-474.
18 Lewold S, Goodman S, Knutson K, et al. Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis: a Swedish multicenter survival study. J Arthroplasty. 1995;10:722-731.
19 Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg [Br]. 1998;80:983-989.
20 Pandit H, Jenkins C, Beard D, et al. Minimally invasive medial Oxford UKR 10 year survival. Presented at the Annual Meeting of the American Academy of Orthopedic Surgeons, Las Vegas, 2009.
21 Keys GW, Ul-Abiddin Z, Toh EM. Analysis of first forty Oxford medial unicompartmental knee replacement from a small district hospital in UK. Knee. 2004;11:375-377.
22 Svärd UC, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of an independent series. J Bone Joint Surg [Br]. 2001;83:191-194.
23 Rajasekhar C, Das S, Smith A. Unicompartmental knee arthroplasty: 2- to 12-year results in a community hospital. J Bone Joint Surg [Br]. 2004;86:983-985.
24 Mercier N, Wimsey S, Saragaglia D. Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty. Int Orthop. 2010;34:1137-1143.
25 Kumar A, Fiddian NJ. Medial unicompartmental arthroplasty of the knee. Knee. 1999;6:21-23.
26 Vorlat P, Putzeys G, Cottenie D, et al. The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc. 2006;14:40-45.
27 Price AJ Svärd U. A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2011;469:174-179.
28 Price A, Waite J, Svärd U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;435:171-180.
29 Dejour D, Chatain F, Habi S. The role of the femoropatellar articulation and the opposite compartment in the degradation of the functional result of unicompartmental prostheses. [Role de l’articulation femoro-patellaire et du compartiment oppose dans la degradation du resultat fonctionnel des protheses unicompartimentales.]. Rev Chir Orthop Reparatrice Appar Mot. 1996;82:37-39.
30 Weale AE, Murray DW, Crawford R, et al. Does arthritis progress in the retained compartments after “Oxford” medial unicompartmental arthroplasty? A clinical and radiological study with a minimum ten-year follow-up. J Bone Joint Surg [Br]. 1999;81:783-789.
31 Barrington J, Emerson R. The Oxford knee: first report of 20-year follow-up in the US. Presented at the Annual Meeting of the American Academy of Orthopedic Surgeons, New Orleans, 2010.
32 Emerson RHJr, Hansborough T, Reitman RD, et al. Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res. 2002;404:62-70.