CHAPTER 57 Minimally Invasive Posterior Lumbar Instrumentation
Overview
Over recent years minimally invasive surgical techniques have evolved to safely allow access to the spine with less collateral damage as compared with traditional open surgical approaches. The basic principles of spinal surgery remain unchanged. The most basic tenant of minimally invasive spine surgery is to perform the same surgery as has traditionally been done open but with less soft tissue destruction and equal or better outcomes. Minimally invasive surgical techniques have demonstrated less blood loss, shorter hospital stays, and lower infection rates as compared with open surgical techniques.1–5 However, operative times are longer and there may be a trend toward more technical complications.1,2 Also, there is a prolonged and slow learning curve associated with minimally invasive surgery.
Obesity
Approximately one third of American adults older than the age of 20 are considered obese.6 Complication rates as high as 36% to 50% have been reported for obese patients undergoing lumbar fusion.6 Although obesity certainly makes minimally invasive surgery more challenging, it can be done safely and effectively in this population. The authors’ personal experience has found that oftentimes pedicle screws can be placed more easily through a minimally invasive Wiltse-type approach as compared with midline approaches because there is much less muscle, fat, and soft tissue retraction necessary to obtain the correct screw trajectory. Also, the retractor can help to keep adipose tissue and the deep (often thick) musculature out of the surgical field.
Park and colleagues7 compared the perioperative complications in patients with a BMI greater than 25 kg/m2 with patients having a BMI less than 25 kg/m2 who underwent a minimally invasive lumbar spinal surgery. Minimally invasive decompressions in patients with a BMI greater than 25 kg/m2 had a 6.5% complication rate as compared with 11.8% in patients with a BMI less than 25 kg/m2. Minimally invasive fusion procedures had a 24% complication rate in patients with a BMI greater than 25 kg/m2 as compared with 25% in patients with a BMI less than 25 kg/m2. No infections were recorded in either group. No statistical differences were noted between groups. Similarly, Rosen and colleagues6 did not find a correlation between BMI and postoperative changes in ODI, VAS, and SF-36 scores using a linear regression model.
Minimally invasive fusions in obese patients also create less postoperative dead space, which may lead to lower infection rates. O’Toole and colleagues8 reviewed surgical site infections in MIS decompressions, discectomy, and fusion cases. One-thousand, three-hundred, and thirty-eight cases were included for the review. Three postoperative surgical site infections were identified. Two patients developed superficial cellulitis after minimally invasive fusions, and one patient developed discitis after a microendoscopic discectomy (MED). The reported surgical site infection rate for simple decompressive procedures was 0.1% and 0.74% for fusion with internal fixation. The overall infection rate for the entire cohort was 0.22%. The reported infection rate for minimally invasive fusion compares favorably with open fusion infection rates. Importantly, there were no cases of postoperative deep wound infection in O’Toole and colleagues’ cohort. The one patient with discitis developed symptoms 1 month after developing a lower extremity cellulitis. The disc space biopsy grew the same organism as the cellulitis. No patient in their series required reoperation for a deep wound infection. In contrast, Picada and colleagues9 reported a 3.2% deep wound infection after reviewing 817 patients who underwent an open lumbosacral fusion. Minimally invasive fusions can be performed safely and effectively in obese patients, but these cases may be more technically demanding as the working length through the tube increases.
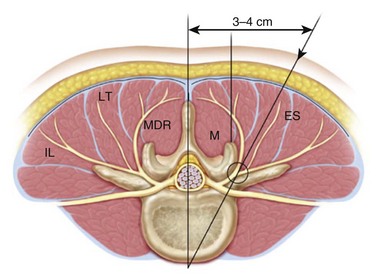
In obese patients the authors have found it helpful to measure the distance from the dorsal aspect of the facet at the level of the intended procedure on the preoperative magnetic resonance imaging (MRI) to help determine the length of retractor needed in heavier patients (Fig. 57–1). During a surgeon’s initial experience with minimally invasive fusions, patients with an expected retractor length greater than 80 mm are a relative contraindication, particularly early in the learning stages. However, with experience obese patients are a relative indication for minimally invasive fusion and instrumentation rather than a contraindication.
Technical Outcomes of Minimally Invasive Fusion Surgery
At the time of this publication there is still a relative paucity of published literature detailing the clinical results of minimally invasive fusion surgery. Early studies have demonstrated minimally invasive fusion to be safe and efficacious.5,10,11
Kim and colleagues12 compared tissue injury markers between minimally invasive posterior lateral lumbar interbody fusion (PLIF) and open PLIF. Significantly larger increases were observed in creatinine kinase, aldolase, IL-6, IL-10, and IL-1ra in the open PLIFs compared with the minimally invasive PLIFs. This confirms less muscle injury in the minimally invasive fusions and may result in a lower systemic inflammatory reaction in the immediate postoperative period, which in turn may lower acute medical morbidity. However, clinical studies have not documented this to date.
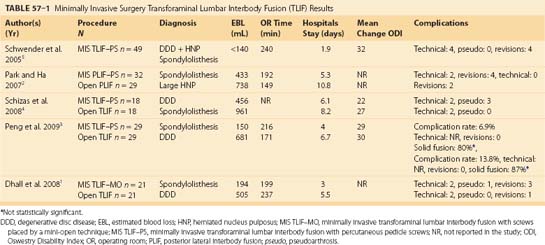
Shizas and colleagues4 and Peng and colleagues3 both compared minimally invasive transforaminal lumbar interbody fusion (TLIF) with open TLIF for the treatment of spondylolisthesis and degenerative disc disease. The average hospital stay was 2 days shorter following minimally invasive TLIF as compared with open TLIF. Blood loss was significantly less, but the operative time, at least in the Peng3 study, was 45 minutes longer. Overall the complication rates were similar between open TLIF and minimally invasive TLIF. Schizas and colleagues4 reported two technical complications in each group. However, they found three pseudoarthroses in the minimally invasive group compared with none in the open group. Peng and colleagues3 observed that 80% of the minimally invasive TLIFs were solidly fused compared with 87% of the open TLIFs. Peng and colleagues3 also noted a 7% complication rate in the minimally invasive group compared with a 14% complication rate in the open group. Both Peng and colleagues and Schizas and colleagues found similar improvements in Oswestry Disability Index (ODI) scores. Minimally invasive TLIF ODI scores improved by 22% compared with improvement of 27% in the open TLIF group reported by Schizas and colleagues. These authors observed a 29-point improvement in ODI scores in minimally invasive TLIFs and a 30-point improvement in open cases.
Traditional Pedicle Screws
Minimally invasive fusions use the surgical corridor as described by Wiltse13 between the multifidus and longissimus paraspinal muscles (Fig. 57–2). This trajectory is ideal for both pedicle screw placement and interbody work.
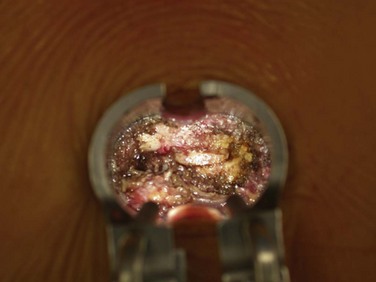
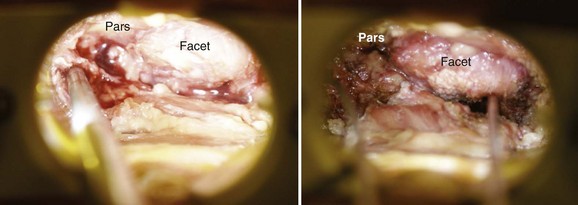
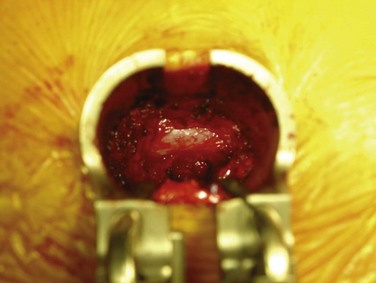
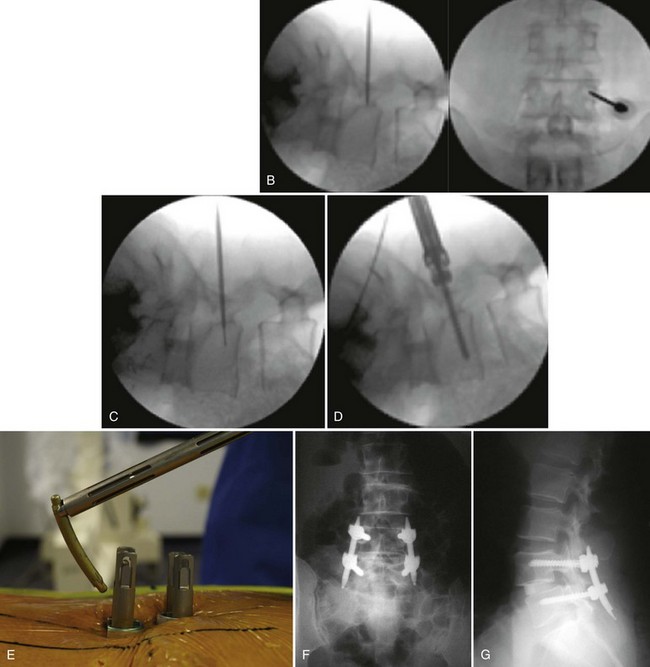
After the appropriate trajectory is localized with fluoroscopy, sequential dilators are passed through the fascia and docked onto the facet joint. A tubular retractor (typically 20 or 22 mm) is then docked and secured over the dilators. The use of an expandable retractor allows the blades to expand cephalad or caudad, creating a corridor for pedicle screw placement (Fig. 57–3). Soft tissue is cleared to expose the standard pedicle screw entry points (Fig. 57–4). Screws can be placed using a variety of methods including free hand, under C-arm guidance, or using navigation depending on surgeon preference. In addition, both posted- and tulip-style screws can be used if working through the tubular retractor systems that are available.
Surgeon preference dictates the sequence of steps during minimally invasive fusion. Early on in a surgeon’s experience it may be easiest to place the pedicle screw tracts first, before the decompression or facetectomy. This will preserve “normal” anatomy to help orient the surgeon to the anatomic starting points. However, it is the authors’ experience that it is more efficient to perform the decompression and interbody spacer placement before screw tract preparation if required. This minimizes the surgical exposure during the portion of the procedure that requires the most medial angulation of the retractor and thereby helps to limit muscle creep (Fig. 57–5).
Percutaneous Pedicle Screws
Pedicle screws can be safely and effectively placed percutaneously and thus avoid the additional dissection required for the placement of traditional pedicle screws. Percutaneous pedicle screw placement has the advantage of less muscle damage and less potential damage to the medial branch nerve (innervation of the multifidus), and it can be used effectively over long segment fusions.14,15 The placement of percutaneous pedicle screws can require more operative time and more x-ray exposure for accurate placement.
Technique of Percutaneous Pedicle Screw Placement
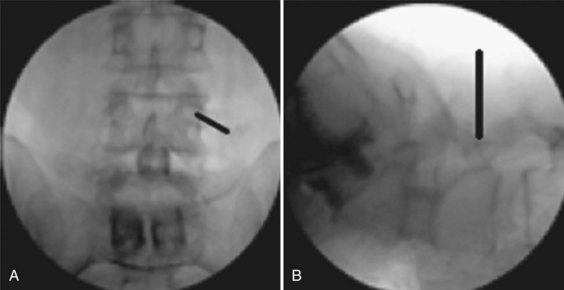
The authors prefer to place percutaneous pedicle screws using fluoroscopy because it is readily available. The orientation of the C-arm beam is of critical importance. The anteroposterior (AP) images must be true AP images of each pedicle for which you are planning screw placement (Fig. 57–6). The spinous process should be in the midline of the vertebral body, equally spaced between both pedicles. The superior and inferior endplates should be parallel, and the pedicles should be appropriately located at the caudal end of the ascending articular process. On the lateral view the superior endplate should appear as one line and the pedicles should overlap and thus appear as one. True AP and lateral radiographs are of critical importance because small variance can produce large errors.
The pedicle of interest is localized using the AP fluoroscopic image. The skin is incised just lateral to the pedicle. The thoracolumbar dorsal fascia and muscle fascia are incised. A Jamshidi trocar is used to cannulate the pedicle. The ideal starting point is at the 10 o’clock and 2 o’clock positions on the left and right pedicles, respectively. The Jamshidi is slowly advanced a few millimeters. A lateral fluoroscopic image is obtained and should confirm that the Jamshidi is placed within the center of the pedicle. Under AP fluoroscopic imaging the Jamshidi is advanced about 20 mm. The tip should stay lateral to the medial border of the pedicle. A lateral image is obtained and should show the tip of the Jamshidi at or past the neurocentral junction. If so, the Jamshidi can be safely advanced to its desired depth. If the tip of the Jamshidi is at or medial to the medial border of the pedicle on the AP view and has not yet passed the neurocentral junction on the lateral, the pedicel screw tract has breached the medial border of the pedicle (Fig. 57–7).
Studies Comparing Mini-Open and Percutaneous Pedicle Screws
The decision of which minimally invasive instrumentation technique to use is largely surgeon dependent. Regev and colleagues15 compared mini-open pedicle screw placement with percutaneous pedicle screw insertion in cadavers. After screw placement the authors dissected out the medial branch nerve. The medial branch nerve originates from the dorsal rami of each spinal nerve and innervates the multifidus muscle. The medial branch nerve was transected in 84% of cases using the mini-open technique as compared with 20% of the percutaneous insertion technique. The clinical importance of this difference is unknown. However, in this study percutaneous pedicle screw placement better preserved the segmental innervation of the multifidus compared with mini-open pedicle screw insertion.
No clinical studies have directly compared the use of traditional pedicle screws placed through a tubular retractor (mini-open) to percutaneous pedicle screws. However, multiple studies have reported perioperative data regarding percutaneous and open screw insertion (Table 57–1). Schizas and colleagues4 reported their experience with 18 minimally invasive TLIFs using percutaneous pedicle screw fixation and compared this with 18 open TLIFs. The percutaneous pedicle screw patients used 2.7 cGy/cm2 of radiation as compared with 1.8 cGy/cm2 in the open TLIF group. The minimally invasive TLIF operative time averaged 4.3 hours in the last third of their experience. Their estimated blood loss was 456 mL. Peng and colleagues3 also reviewed the results of minimally invasive TLIFs. They used an average of 105 seconds of fluoroscopy. They had an average estimated blood loss (EBL) of 150 mL and average operative time of 216 minutes. Neither of these studies reported any technical complications with minimally invasive TLIFs performed by percutaneous screws. Foley’s10 initial experience was similar with an average operative time of 290 minutes and estimated blood loss of 25 mL. He reported one technical complication of a loose locking plug that required revision. Dhall and colleagues1 compared minimally invasive TLIFs with traditional pedicle screws with open TLIFs. Their average EBL was 194 mL, and their average operating room (OR) time was 199 minutes. There were two technical complications in the minimally invasive group with one misplaced pedicle screw and one case of interbody cage migration. The open group also had one misplaced screw. Schwender and colleagues5 reported on their initial experience with minimally invasive TLIFs and percutaneous screw insertion. Their average operative time was 240 minutes, and the average EBL was 140 mL. In this series there were two misplaced screws and interbody cage dislodgement. Park and colleagues2 compared 32 minimally invasive PLIFs with 29 open PLIFs. All minimally invasive cases were stabilized with percutaneous screws. The average OR time was longer for the minimally invasive cases compared with open cases, 191 minutes and 150 minutes, respectively. The average EBL in the minimally invasive cases was 432 mL compared with 737 mL. There were two technical complications, one screw malposition and one interbody cage migration, reported in the minimally invasive group and none in the open group. These differences were not statistically significant.
In 2005 Kim and colleagues14 compared longitudinal changes in multifidus cross-sectional area and trunk extension strength in both open and percutaneous pedicle screw constructs. The T2 cross-sectional area of the multifidus muscle was recorded on preoperative and postoperative MRIs. Trunk extension strength was measured using a MedX lumbar extension machine. Multifidus cross-sectional area decreased from 1140 mm2 to 800 mm2 in open pedicle screw constructs as compared with percutaneous pedicle screw construction in which multifidus area decreased from 1320 mm2 to 1270 mm2. Trunk extension strength increased in both open and percutaneous pedicle screw constructs, but the improvements in strength were only statistically significant in the percutaneous pedicle screw group.
Screw Insertion Technique: Fluoroscopic Versus Navigation
Multiple techniques exist for the placement of percutaneous pedicle screws. Pedicle screws can be placed safely with conventional fluoroscopy or by computer navigation and three-dimensional imaging. The clear concern with the use of fluoroscopy is radiation exposure to both the surgeon and the patient. Bindal and colleagues16 prospectively recorded radiation exposure in 24 consecutive minimally invasive TLIF procedures. The mean fluoroscopy time was 1.69 minutes (101 seconds). The mean exposure was 76 mRem at the surgeon’s dominant hand, 27 mRem under a lead apron, and 32 mRem at an unprotected thyroid level. The mean exposure to the patient’s skin was between 59 mRem and 78 mRem depending on the orientation to the x-ray beam. According to Bindal and colleagues the radiation exposure to both surgeon and patient was relatively low. They extrapolated that it would take 194 cases to exceed the acceptable torso radiation limits. The radiation levels they observed also compared favorably with other fluoroscopic procedures such as percutaneous coronary interventions.
Nonetheless, all surgeons should be judicious and minimize radiation exposure to the patient, OR personnel, and themselves. Computer-assisted navigation has been proposed as one means to reduce fluoroscopic use. Kim and colleagues17 performed a two-phased cadaveric and prospective clinical review comparing navigation-assisted fluoroscopy and standard fluoroscopy use in minimally invasive TLIFs. In the cadaver study they noted a longer setup time for navigation (9.7 minutes) compared with fluoroscopy (4.8 minutes). The mean fluoroscopic time was 42 seconds in the fluoroscopy group and 29 seconds in the navigation group. The average radiation exposure to the surgeon was undetectable in the navigation group and was 12.4 mRem in the fluoroscopic group. Clinically, minimally invasive TLIFs with navigation used 57 seconds of fluoroscopy and minimally invasive TLIFs with fluoroscopy used 147 seconds. Kim and colleagues reported no cases of screw malposition in either group and blood loss, operating time, and hospital stay were similar in both groups.
Pearls and Pitfalls
Key Points
1 Dhall S, Wang M, Mummaneni P. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long term follow-up. J Neurosurg Spine. 2008;9:560-564.
2 Park P, Upadhyaya H, Garton H, et al. The impact of minimally invasive spine surgery on perioperative complications in overweight or obese patients. Neurosurgery. 2008;62:693-699.
3 Peng C, Yue W, Poh S, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine. 2009;34:1385-1389.
4 O’Toole J, Eichholz K, Fessler R. Surgical infection rates after minimally invasive spinal surgery. J Neurosurg Spine. 2009;11:471-476.
5 Kim D, Lee S, Chung S, et al. Comparison of multifidus muscle atrophy and trunk extension muscle strength. Percutaneous versus open pedicle screw fixation. Spine. 2005;30:123-129.
1 Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9:560-565.
2 Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine (Phila Pa 1976). 2007;32:537-543.
3 Peng CW, Yue WM, Poh SY, et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2009;34:1385-1389.
4 Schizas C, Tzinieris N, Tsiridis E, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop. 2009;33:1683-1688.
5 Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005;18(Suppl):S1-S6.
6 Rosen DS, Ferguson SD, Ogden AT, et al. Obesity and self-reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery. 2008;63:956-960. discussion 60
7 Park P, Upadhyaya C, Garton HJ, et al. The impact of minimally invasive spine surgery on perioperative complications in overweight or obese patients. Neurosurgery. 2008;62:693-699. discussion 693-699
8 O’Toole JE, Eichholz KM, Fessler RG. Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine. 2009;11:471-476.
9 Picada R, Winter RB, Lonstein JE, et al. Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord. 2000;13:42-45.
10 Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003;28:S26-S35.
11 Holly LT, Schwender JD, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006;20:E6.
12 Kim KT, Lee SH, Suk KS, et al. The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine (Phila Pa 1976). 2006;31:712-716.
13 Wiltse LL, Bateman JG, Hutchinson RH, et al. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am. 1968;50:919-926.
14 Kim DY, Lee SH, Chung SK, et al. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976). 2005;30:123-129.
15 Regev GJ, Lee YP, Taylor WR, et al. Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine (Phila Pa 1976). 2009;34:1239-1242.
16 Bindal RK, Glaze S, Ognoskie M, et al. Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine. 2008;9:570-573.
17 Kim CW, Lee YP, Taylor W, et al. Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J. 2008;8:584-590.