Minimally Invasive Non-Hysteroscopic Endometrial Ablation
Minimally invasive non-hysteroscopic techniques have largely replaced hysteroscopic endometrial ablation. The reasons for the gynecologist’s preference for these minimally invasive procedures relate to the following: minimal skill required, no distension medium needed, and rapid performance time expected. The results of these minimally invasive ablations have been generally good if one uses a final common path of reduced or normal bleeding. Amenorrhea rates are generally lower than with direct vision hysteroscopic endometrial ablation. Disadvantages of the minimally invasive techniques include that the techniques are mainly blind (the exception being the hydrothermablator [HTA] device), and they typically rely on low intrauterine volume and pressure to ensure safety.
The more commonly used devices are described below.
Hydrothermablator (Boston Scientific, Natick, MA) (Fig. 110–1A, B). A modified hysteroscope is placed into the uterine cavity. A bag of normal saline serves as a reservoir, and the entire system is fluid filled. The uterine cavity is distended, and any leaks are detected by drops in the reservoir. The saline is heated outside of the uterus and is flushed through the uterine cavity at low pressure. The ablation can be directly viewed via the telescope.
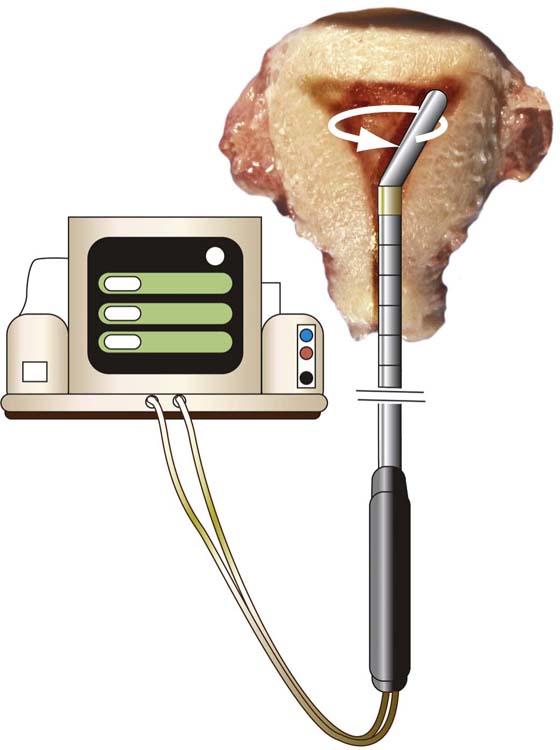
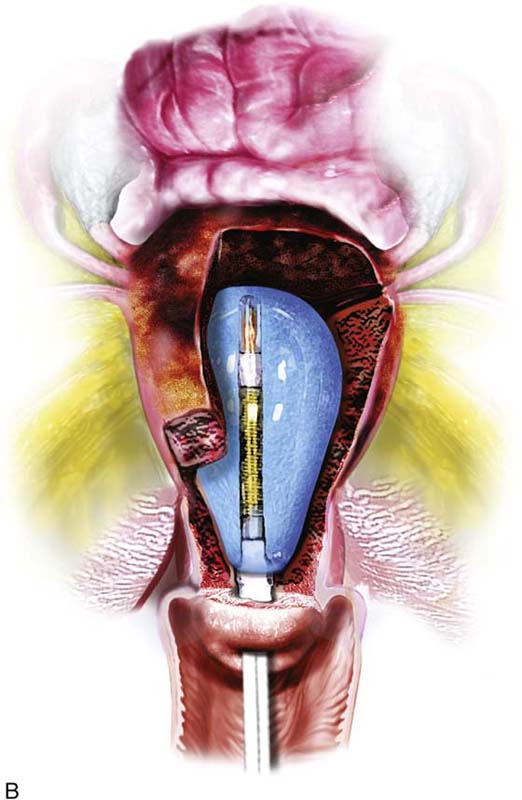
Microsulis (microwave endometrial ablation; Microsulis, Hampshire, UK) (Fig. 110–2). This electrosurgical device consists of a monopolar probe, which functions as a microwave because the radiofrequency generator delivers frequency in the megahertz operational range. The endometrium is ablated via conversion of electrical to thermal energy. This is one of the oldest non-hysteroscopic devices, dating back to 1991. High power outputs (e.g., 200 watts) are required to maintain a constant probe temperature of 65°C. The probe is rotated intraoperatively to obtain even dispersal of heat. The patient must wear a large neutral electrode throughout the procedure.
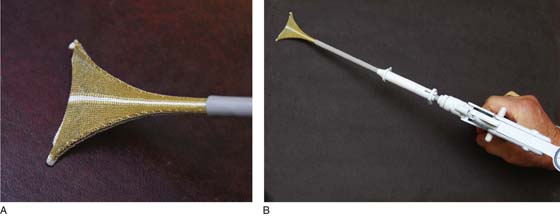
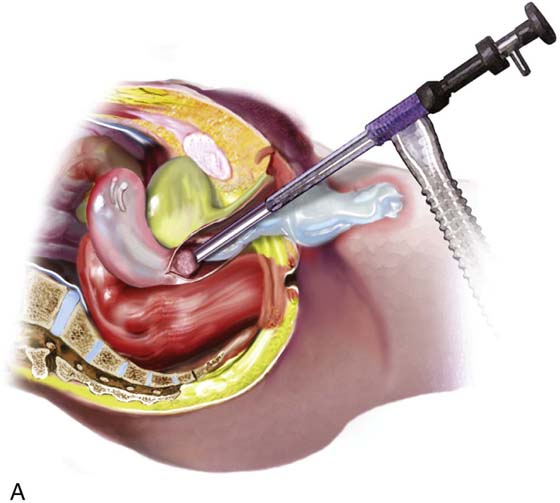
NovaSure (Hologic Inc., Marlborough, MA) (Fig. 110–3A, B). Consists of a bipolar mesh bag, which is inserted into the uterus collapsed via an applicator. The device must be oriented so that the kitelike frame can accommodate to the inverted triangular uterine cavity. A dial that reads the cavity width and depth is obtained from a device display. Carbon dioxide gas pressurizes the cavity to determine whether leakage is or is not occurring. Radiofrequency biopolar electrical energy coagulates the endometrium at 180 watts of output.
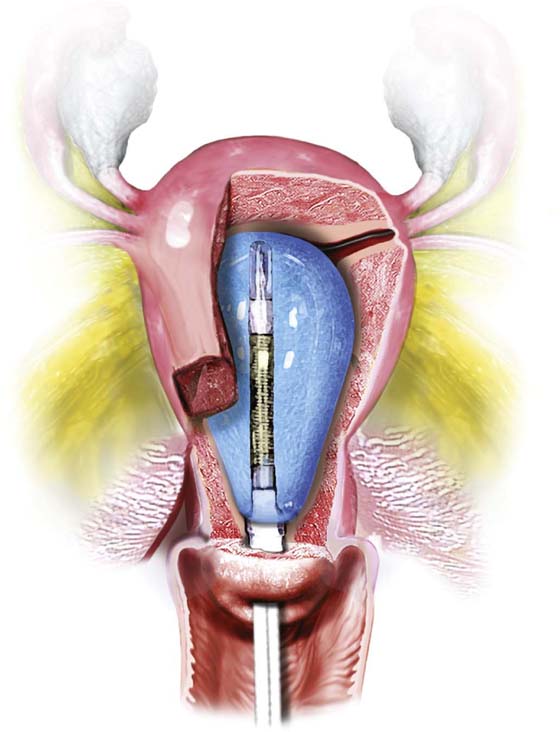
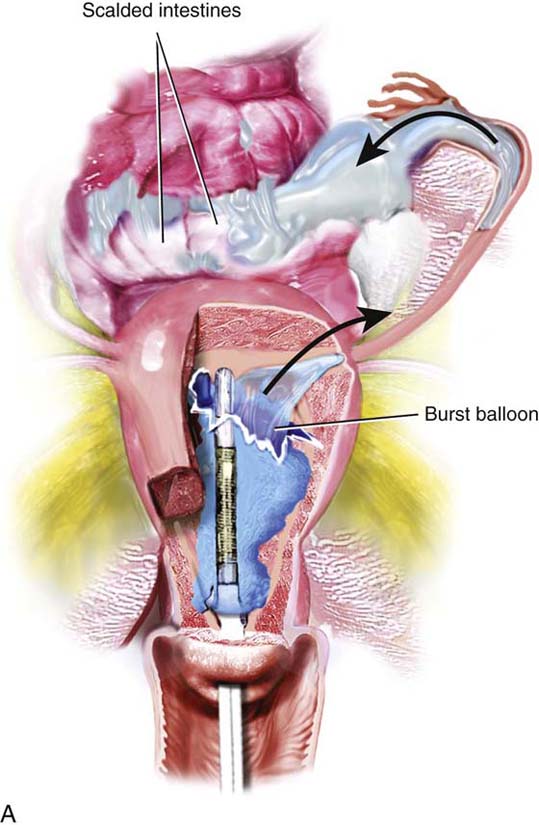
Thermachoice (Gynecare-Ethicon, Somerville, NJ) (Fig. 110–4). This is a balloon device. A collapsed balloon is inserted into the uterine cavity via an applicator. The balloon is distended with sterile water or saline. Based on the pressure reading, the gynecologist can determine that the balloon is intact. Approximately 15 mL of saline within the balloon is heated in situ, creating thermal destruction of the endometrium. The cavity must be normal in configuration for the balloon to deploy properly.
Complications
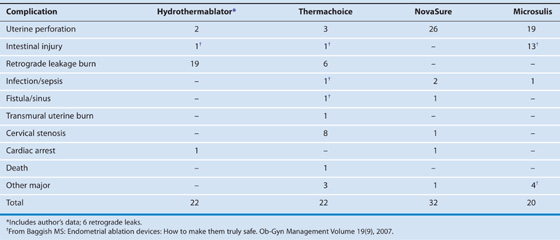
Table 110–1 (after Ob-Gyn Management Volume 19[9], 2007) depicts complications reported via the U.S. Food and Drug Administration (FDA). Each device has a peculiar footprint.
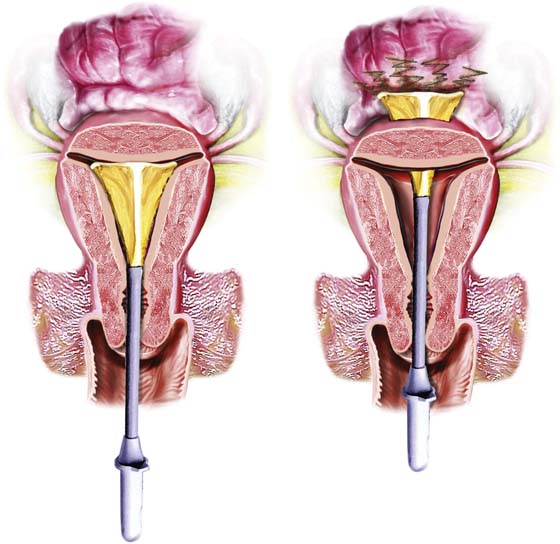
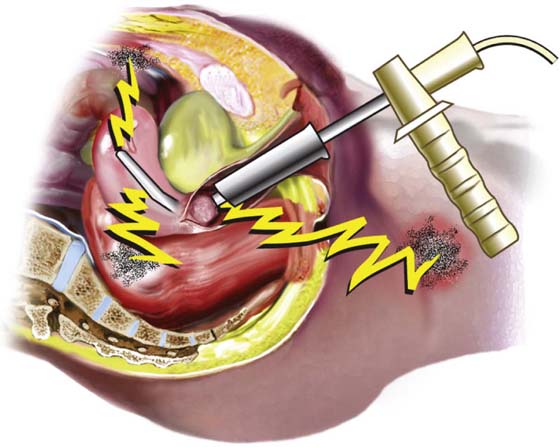
The principal complication associated with Thermachoice was perforation with balloon rupture (Fig. 110–5A, B). The HTA device was associated with retrograde leakage of hot fluid via the cervix (Fig. 110–6A). The company has recently developed a new sheath with a better cervical seal (Fig. 110–6B). The NovaSure device has a high propensity for uterine perforation as well as transmural thermal injury (Fig. 110–7). The microwave device is associated with high-frequency electrical leakage and thermal injury (Fig. 110–8).
FIGURE 110–1 A. The hydrothermablator (HTA) sheath is shown with entry and return tubing for the circulation of hot saline within the uterine cavity. The telescope permits the surgeon to view the process. B. The HTA unit consists of a control device, a heater, and a reservoir. The bag of saline fills the entire system with fluid.
FIGURE 110–2 The microwave probe and control unit are shown here. A neutral electrode belt is attached to the patient. The active electrode (probe) is rotated during the ablation procedure to obtain an even distribution of energy.
FIGURE 110–3 A. The NovaSure device consists of a mesh triangular framework with an underlying bipolar electrode. One portion of the electrode is the active electrode and the other, the neutral electrode. B. The device is folded within the application and is pushed open within the uterine cavity. A measurement of the opened width is indicated on a dial above the application grip.
FIGURE 110–4 The Thermachoice balloon is inserted into the uterus in a collapsed state. The balloon is distended with saline, which, in turn, is heated in situ. The hot distended balloon transmits heat to the surrounding endometrium, creating coagulation necrosis. (From Baggish MS, Valle RF, Guedj H: In Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Lippincott, Williams and Wilkins, Philadelphia, 2007.)
FIGURE 110–5 A. A ruptured balloon containing hot water or saline can spill into the abdominal cavity via the oviduct or into the vagina via the cervix. B. Transmural thermal injury to the uterine wall (through and through burn) can additionally create a bowel burn if the intestine is in contact with the serosal surface of the uterus. (From Baggish MS, Valle RF, Guedj H: In Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Lippincott, Williams and Wilkins, Philadelphia, 2007.)
FIGURE 110–6 A. A loose seal between the hydrothermablator (HTA) sheath and the cervix can result in retrograde leakage of scalding saline or water. B. An improved sheath permits a tighter cervical seal. Note the fine contact discs of Silastic-type construction. (From Baggish MS, Valle RF, Guedj H: In Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Lippincott, Williams and Wilkins, Philadelphia, 2007.)
FIGURE 110–7 The figure on the left shows the NovaSure device in proper position. The figure on the right shows the device perforating the uterus. If the electrode is activated, it will coagulate not only the uterine myometrium but also the surrounding intestine. (From Baggish MS, Valle RF, Guedj H: In Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Lippincott, Williams and Wilkins, Philadelphia, 2007.)
FIGURE 110–8 The microwave electrode has perforated the uterus just above the cervix. The activated electrode can cause thermal damage to neighboring structures (e.g., bowel, bladder). (From Baggish MS, Valle RF, Guedj H: In Hysteroscopy: Visual Perspectives of Uterine Anatomy, Physiology, and Pathology. 3rd ed. Lippincott, Williams and Wilkins, Philadelphia, 2007.)
TABLE 110–1  Complications Associated With Four Endometrial Ablation Devices
Complications Associated With Four Endometrial Ablation Devices