chapter 8 Mind–body medicine
INTRODUCTION AND OVERVIEW
WHAT IS MIND–BODY MEDICINE?
A practical way of expressing this principle is to say that psychological states such as chronic stress, depression, anxiety and fear produce profound and clinically relevant effects upon the body. These effects have implications for health and illness. Psychological states and social context can have both positive and negative effects that manifest on many different levels, all the way from muscle tension to genetic expression. Over time the cumulative effects of negative mental and emotional states can take a heavy toll on the body. Conversely, research also suggests that psychosocial interventions can play an important part in ameliorating these negative effects and can assist in promoting healing.
Despite the enormous scope and clinical potential of MBM, it has been relatively slow to enter mainstream medical education and practice. This lack of awareness among clinicians tends not to be reflected in the general community, which has a strong interest in and intuitive appreciation of MBM principles, although expectations are sometimes unrealistic. The desire for a ‘holistic philosophy’ to underpin healthcare is a major reason that many people search out complementary therapies.2
THE CAUSE AND EFFECTS OF STRESS
Most affluent countries around the world are observing significant increases in the rates of stress, depression and suicide. Evidence suggests that stress hormones play an important role in the development of psychiatric disorders3 as well as having direct effects on serotonergic pathways.4 Serotonin is the principal neurotransmitter implicated in depression, and antidepressant medications are largely aimed at modulating serotonin.
These changes, designed to help the body cope with demands and potential injury, will mobilise according to whatever we perceive as a threat. When the situation is over, the physiology should return to rest if the situation is mentally left in the past. Even one’s own doctor can be perceived as a threat. The prospect of having one’s blood pressure measured is enough to elevate it to a point where approximately 25% of patients are inappropriately diagnosed with hypertension.5 This is known as ‘white-coat hypertension’ and is just another example of the clinical implications of the mind–body response.
The activation of the fight-or-flight response is not detrimental to health, provided it is mobilised only when it needs to be, is deactivated when it is no longer required, and is not prolonged. Unfortunately, in the vast majority of occasions on which this response is mobilised, it is done so unnecessarily and is maintained long after the event is passed, and the person is unable to deactivate it. Much of the inappropriate activation of the response has to do with the imagination of future and past events taken to be real. The word ‘anxiety’ comes from a Latin word, anxius, meaning to ‘anticipate some future event’. Furthermore, mentally replaying an event can reproduce the stress response many times even though the event is over and happened only once. In the most extreme cases this replaying can be so vivid that a person’s present experience is all but totally overlaid with the past, leading to what is called ‘post-traumatic stress disorder’. Here, through neuron plasticity, the memory, emotion and physiological response have become wired into the neural circuitry of the brain, principally through the limbic system, which mediates memory and emotion.
The chronic or long-term inappropriate activation of the stress response, mediated through the SNS, leads to a significant level of physiological wear and tear. This is called ‘allostatic load’.6 It is much like a car being driven so hard that the heavy demands placed upon it will lead to failure of its parts. High allostatic load is associated with both anxiety and depression and will lead to, among other things:
These effects are logical sequelae of the prolonged activation of the SNS. Stress and inflammatory mediators, such as cytokines, also have important effects on mood, behaviour and emotion.7 Activation of the immune system via these immune mediators, such as takes place during an acute infection, induces sickness behaviour (apathy, lethargy, lack of motivation and appetite). This behaviour is the body’s way of ensuring that one takes the rest required to assist the body in recovering from an infection. Many of these symptoms are also seen in depression and a significant part of the reason may be because of the high levels of cytokines associated with high allostatic load. Some cytokines activate cerebral noradrenergic and serotonergic systems and so anxiety and depression are often seen as a mixed picture. It may also be part of the reason that depression occurs more frequently in people with medical disorders associated with immune dysfunction. From a therapeutic perspective it is important to remember that every investment in reducing anxiety, improving coping and enhancing wellbeing is a step towards reducing suicide risk.
MENTAL HEALTH INDICATORS
In spite of recent clinical and research advances, an increased burden of mortality and morbidity related to stress and mental ill health can be noted, especially in European societies and populations undergoing stressful transitions and dramatic changes. A societal syndrome, consisting of depression, suicide, abuse, risk-taking and violent behaviour as well as vascular morbidity and mortality, can be observed.8
Evidence suggests that the stress associated with modern life has been increasing at a surprisingly rapid rate: 45% over the past 30 years in some surveys.9 Depression currently ‘causes the largest amount of non-fatal burden, accounting for almost 12% of all total years lived with disability worldwide’10 and it is estimated that in Australia mental health issues, principally depression, will be the major cause of morbidity within the next two decades.11 Among affluent countries around the world it is estimated that, by the year 2030, unipolar depression will account for over 1.5 times the burden of disease that will be accounted for by cardiovascular disease.12 This is independent of the secondary effects of depression, such as it being an independent risk factor for heart disease and associated co-morbidities such as substance abuse.
Today, higher rates of depression are occurring at younger ages. Suicidal ideation is surprisingly common in adolescents. Data suggest that 1 in 2 young people report experiencing high levels of psychological stress and as many as 25% of 15–24 year-olds presenting to a GP for any reason reported experiencing recent suicidal thoughts13 despite the fact that most did not present for psychological reasons.
Evidence suggests that antidepressant medications in children and adolescents, although widely used, are not effective and that such approaches have to be questioned.14,15 Part of their overuse may be driven by marketing forces and parental anxiety. Particularly in this group of patients it is important for attention to be paid to the social and domestic causes of stress and to the fostering of protective factors and resilience through education and community programs.
Some groups on the fringe of society, such as the Goth subculture, seem to be at very high risk for self-harm and attempted suicide.17 Music is also a powerful modulator of emotion and behaviour and can significantly increase risk-taking behaviour.18 The assessment and management of mental health issues among adolescents therefore requires attention to such issues.
DOPAMINE AND REWARD SYSTEMS
Different brain pathways accord with differing approaches to pursuing fulfillment. Dopamine is a neurotransmitter with multiple actions at each level of the mesocorticolimbic reward pathway—it is intimately associated with the ability to experience pleasure and motivation.19 The pursuit of pleasure is a vital activity associated with survival. For example, we would not eat or reproduce unless it was pleasurable. Some people are, however, more genetically at risk of developing addictive behaviours, and the over-activation of the mesolimbic system can trigger addictions of various kinds. In such situations it requires increasingly intense and frequent stimuli to produce the same pleasure response; over time, this ‘tires’ the reward system, predisposing to anhedonia and depression. Dysfunction of dopamine transmission in the reward circuit is associated with symptoms such as anhedonia (inability to experience pleasure), apathy and dysphoria (disturbed mood). It is found in various neuropsychiatric disorders, including Parkinson’s disease, depression and drug addiction. Prolonged and significant stress early in life can also affect one’s dopamine pathways for life.20 What begins as a pursuit of pleasure eventually becomes an uneasy retreat from the pain and anxiety associated with withdrawal. This has implications for the development of impulsivity and reactivity.
Increased dopamine release is also seen in the brain during the relaxation response. This is associated with reduced impulsivity or reactivity,21 which may have something to do with the development of emotional and impulse regulation associated with long-term meditation practice. This may also help to facilitate healthy lifestyle change.
Mood, neurochemistry and behaviour are intimately entwined. Mood affects behaviour and is a common reason for relapse into unhealthy behaviours.22 Major depression, for example, triples the risk of progression to daily smoking23 but, conversely, a history of daily smoking nearly doubles the risk of major depression. In adolescents, experimental smoking very significantly increases the risk of taking up smoking as a habit. Depression, anxiety and peer smoking strongly predict the risk of experimental smoking, and depression and anxiety increase susceptibility to peer influence to establish risk-taking behaviours. Building resilience and emotional intelligence in adolescents, particularly boys, may therefore produce a number of benefits including the ability to avoid unhealthy behaviours. It also goes part of the way towards explaining why CBT and antidepressant medications both reduce relapse rates for smokers.24,25
Brain scans show that mental anticipation can have as significant an effect upon brain activity as physical stimulation. The thought of eating activates areas of the brain associated with rewards and pleasure.26 As these centres are important in addictions it is likely that potential forms of therapy for treating addictions will be developed that target these biochemical reactions pharmacologically27 and behaviourally.
STRESS AND PERCEPTION
These help to reverse the effects of inappropriate stress by attacking it at its cause—thought. Reviews of the literature suggest that cognitive and relaxation-based forms of stress management are the most effective strategies in general practice settings, and that working in groups potentiates outcomes.29 A certain amount of stress can be useful in enhancing motivation. Furthermore, the fight-or-flight response can be entirely necessary in extreme situations. Aside from this, however, most of the stress experienced in daily life is neither necessary nor helpful in improving our ability to deal with a challenge. Most of the unhelpful stress experienced is associated with an agitated and unfocused mind that also has a limited capacity at the time to distinguish between present-time reality and imagination. Mental projections and anticipation are given a reality they do not deserve. Examples might include projecting fears into the future about upcoming exams or interviews or habitually recreating past anxieties and conflicts. Here the stressors are in the mind, not in reality, but the body will nevertheless faithfully translate this mentally generated stressor into the stress response. It will not stop until it is told to, regardless of whether the stressor is real or imagined. If one imagines a rope to be a snake, the body will react to the perception, not the reality. Even events that are actually happening at the time will only cause stress depending on the mental interpretation of them. To attribute our stress solely to the events around us and to ignore our own role in generating stress is disempowering and will lead to less than favourable therapeutic outcomes.
GENDER AND THE STRESS RESPONSE
Much of the early stress research focused on men, and hence the fight-or-flight response, which is largely a male response, has become the predominant paradigm in stress medicine. But there is good evidence to suggest that women do not respond to stressful situations in entirely the same way as men, emotionally, socially, behaviourally or physiologically. Reviews of the literature ‘suggest that the female stress response of tending to offspring and affiliating with a social group is facilitated by the process of “befriending”, which is the creation of networks of associations that provide resources and protection for the female and her offspring under conditions of stress’.30
Both males and females have the capacity to activate the fight-or-flight response if required, but men are especially built for this response. Testosterone contributes significantly to this31 and also has a role in the development of ‘rough- and-tumble play’ and sporting interests among boys. Excessive testosterone levels are implicated in excessive physical aggression and crime among men. Female aggression, on the other hand, is more ‘cerebral’—that is, it seems more likely to be expressed ‘in the form of gossip, rumour-spreading and enlisting the cooperation of a third party in undermining an acquaintance’.32
The females of most species are more involved in tending the young because they have the biological or behavioural disposition to ‘tend-and-befriend’. In humans this effect is largely mediated through female hormones such as oxytocin and oestrogen.33 Levels of these hormones are highest during activities like breastfeeding as well as in social interaction, massage and caring physical contact. These hormones have a calming or settling effect on stress and down-regulate the fight-or-flight response.34 Women therefore have less of a tendency to become overly aggressive. None of this suggests that men cannot tend and befriend, or that women cannot elicit the fight-or-flight response when required, but it does suggest that each gender is more or less adapted for one or other response. This is an example of the complementarity of nature but equally it is part of the reason that men and women will respond in different ways to life events and therapies. Women, for example, will tend to feel more comfortable with talking-based therapies, especially dealing with emotional content, whereas men will more often wish to approach problems in an action-based way.
STRESS AND PERFORMANCE
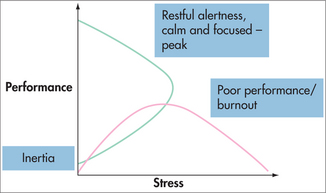
One of the reasons that many people value stress is that they use it as a motivator to enhance performance. It is an assumption for many that if there were no stress there would be no performance. Inertia is, initially at least, a low-stress state but as stress increases, perhaps before an exam or a deadline, stress will often stimulate an increase in performance (Fig 8.1). If the stress remains manageable and is not too prolonged, then there tends not to be a significant problem. If, however, the stress escalates due to rising demands on performance, and stress is the only motivator being used to drive performance, then the person goes over the top of the stress-performance curve (red line) and finds that, despite high stress and energy consumption, performance drops. If this situation goes on for long, burnout soon eventuates.
Unfortunately, burnout is common, particularly among doctors. A study of medical interns found a steady increase in the point prevalence of burnout, which peaked at a prevalence of 75%, 8 months into the intern year. Seventy-three per cent of interns met the criteria for psychiatric morbidity—that is, an anxiety or depressive disorder—on at least one occasion throughout the year.35 For this reason, an increasing number of medical schools are introducing self-care skills into medical education to foster resilience for later careers. Burnout is measured by levels of things such as depersonalisation, lack of motivation and low sense of achievement.
Even in the absence of burnout, living and working in a ‘hyperkinetic environment’ encourages a lower level of focus, which some call ‘attention deficit trait’ (ADT).36 In dealing with so much input coming at such a speed, a person tends to become increasingly reactive, adopts ‘black-and-white thinking’, has difficulty staying organised and setting priorities, and manages time poorly. It is often associated with a constant low level of panic and guilt. The management of ADT is through learning to focus or regulate attention, lifestyle maintenance, changing the environment to be less frenetic and learning how to stop at the end of the day.
Studies of learning styles indicate that certain motivation and learning styles need stress to drive performance, and others don’t. Biggs’ model describes three learning approaches: surface learning, achievement learning and deep learning.37 Deep learners are driven by interest, not stress, and do not need stress to perform well. They integrate what they learn and tend to enjoy it far more. Surface learners tend to learn by rote and the main motivation is to avoid failure. Achievement learners often study hard but are motivated by ego-enhancement, that is, wishing to achieve well in order to earn respect or look good. Surface and achievement learners tend to need stress to perform. The highest achievers all use deep approaches, while third-class honours students tend to use surface approaches.38
MIND AND BRAIN
Depression is an emotional state that is also associated with a range of other symptoms and somatic effects. These are mediated via the neurotransmitter and hormonal changes associated with depression and the rich interconnections between emotional and cognitive centres in the brain. Although there are undoubtedly changes in neurotransmitter profiles in the brain associated with depression, serotonin being the most important, sophisticated brain-imaging techniques are making it clear that thought and belief have a major role in driving brain activity. Functional MRI (fMRI), for example, can show that changes in brain activity associated with the placebo response when a person receives a mock antidepressant is biologically similar to that in people who receive the active drug. Such observations are impossible to explain with the view that the cause of recovery from depression is purely a chemical one. The same is also seen in people who receive placebo analgesics by mapping regional metabolic changes in parts of the brain that modulate the pain response.39,40 Interestingly, brain scans mapping the recovery from depression associated with cognitive approaches demonstrate that it is via different pathways than those associated with pharmacological therapies.41,42
In various chronic pain syndromes, the changes in the brain associated with stress and sympathetic nervous system reactivity sensitise the pain pathways in the brain to register pain messages even with relatively low-level stimuli and in the absence of tissue damage. To the person experiencing the chronic pain syndrome, the experience of pain feels real. This is part of the reason that chronic pain and other manifestations of somatisation are such common accompaniments to emotional states such as depression, anxiety and burnout. It also explains, at least in part, why it is often difficult to demonstrate tissue damage associated with pain in various conditions such as chronic musculoskeletal pain, chronic low back pain, chronic fatigue syndrome and fibromyalgia.43 Sustained attention and arousal are crucial in creating and sustaining the neural loops associated with chronic pain.44 In other words, when a person becomes highly vigilant and reactive to pain messages, the brain will fire off pain messages with fewer and fewer stimuli. From a therapeutic perspective, this may be part of the reason that attention regulation exercises, such as mindfulness meditation, help in chronic pain syndromes. It is likely that the reduced reactivity to sensations may actually help to ‘rewire’ the brain in a way that minimises these effects.
Depression, stress and other psychological and emotional states are undoubtedly associated with physical sequelae. For instance, it has been shown that chronic severe depression is associated with a fivefold-increased risk of coronary heart disease independent of other risk factors.45 These effects are not just the result of changes to one neurotransmitter—serotonin. There is a huge variety of biochemical, physiological and hormonal changes relevant to the cardiovascular system that are associated with depression. It therefore follows that treating depression with antidepressants does not significantly reduce the risk of cardiovascular disease. If, however, thought changes biology, then changing thought for the better among depressed patients should have a more significant effect in reducing the risk of cardiovascular disease, which it does. A meta-analysis of 23 studies clearly showed major reductions in ongoing morbidity and mortality for cardiac patients who received, as part of their rehabilitation, psychosocial interventions aimed at improving coping and emotional health.46 The increased risk for those with no psychosocial treatment as a part of their ongoing management was 1.70 for mortality and 1.84 for recurrence. The conclusions drawn from this study were unambiguous: ‘The addition of psychosocial treatments to standard cardiac rehabilitation regimens reduces mortality and morbidity, psychological distress, and some biological risk factors … It is recommended to include routinely psychosocial treatment components in cardiac rehabilitation.’
The above discussion has given some indication of the scope and potential of MBM.
MAPPING MIND AND BRAIN
Many long-held myths about the brain have recently been challenged, particularly since the rise of neuron-imaging techniques. It was once thought that, after initial development, the CNS changes very little for the rest of the lifespan, but it is now becoming increasingly obvious that major modification of the brain takes place in response to experience, memory, attention and emotion. This is called ‘neuroplasticity’. It suggests that although maladaptive reactions and ways of coping can become ‘wired’ into the circuitry of the brain, from a therapeutic perspective these reactions can also be wired out again, given the right strategies and persistence. The adaptability of the brain is exemplified by experiments on the effects of stress on the animal brain.47 It was demonstrated that remodelling, particularly of the amygdala, which is associated with emotions and anxiety states, took place over a few weeks. This ‘rewiring’ is reversed if the animal is allowed to return to a stress-free environment. Such modelling and remodelling is more rapid in younger animals than in older animals. From a developmental perspective, it has significant implications for the long-term development of anxiety and depression. Memory of emotionally traumatic events with a high level of emotional reactivity reinforces the pairing of the thought with the emotion and accompanying physiological response. In its most extreme form it leads to post-traumatic stress disorder.
There are a number of changes to the brain associated with persistently high allostatic load. The brain is biochemically and structurally very responsive to stress hormones. The hippocampus, important for learning and memory, tends to atrophy and is vulnerable to the effects of stress and trauma. This has implications for the later development of dementia. The prefrontal cortex is important for working memory, and executive functions such as reasoning, emotional regulation, immune modulation and extinction of learning. The prefrontal cortex also plays a key role in modulating the stress response48 but it too tends to atrophy through stress. The amygdala, on the other hand, which mediates the physiological and behavioural fear response, shows growth in response to persistent stress. Other parts of the brain have also been shown to be involved in the stress and fear responses.
States of mind such as those induced by mindfulness meditation are associated with changes in brain activity, specifically activation of the left frontal lobe, which is associated with better mood and improved immunity.49 A predominance of left-sided anterior prefrontal activation is associated with positive affect and optimism. Other studies also link meditation to specific changes in brain activity associated with attention regulation and control of the autonomic nervous system.50 Long-term meditation is now thought to have effects on brain structure and to slow age-related neuronal loss,51 particularly in brain regions associated with attention, interoception and sensory processing. These were significantly thicker in meditators than in matched controls. Meditation ‘might offset age-related cortical thinning’ and provide ‘evidence for … cortical plasticity’, probably a result of down-regulation of the stress hormones associated with allostatic load and implicated in acceleration of brain ageing.
THE PLACEBO RESPONSE
Conditions that seem to be most subject to the placebo effect are those most influenced by emotion, perception and interpretation. Hence, the placebo effect for antidepressants, anxiolytic agents and analgesics is extremely high. To illustrate, reviews of the published research data suggest that the level of placebo effect of antidepressants is 60–80%; that is, only 20–40% of the clinical effect can be attributed to the chemical. More recent reviews, which include unpublished as well as published data, suggest that antidepressants are no better than placebo for mild–moderate depression and only marginally better than placebo even for severe depression.52,53 This is not surprising if one considers that fMRIs on patients receiving antidepressants show that brain activation in those receiving the drug is almost identical to that of those who receive a placebo.39 Recovery from depression through cognitive therapies is via different neurological pathways than those activated by drugs. In the future it may be possible to use patients’ brain scans to identify those who are more likely to respond to drug or cognitive therapies.42,54 fMRI also shows that giving a placebo to a person in pain leads to a different cascade of neuron-chemical changes than those associated with mood regulation—rather, one associated with pain pathways.55 Explanations for such phenomena are difficult unless one takes a more metaphysical view of the relationship between mind, brain and biology.
Surgical techniques are rarely subjected to placebo-controlled trials but when they are, the results are interesting. For example, a trial on arthroscopic knee surgery for osteoarthritis found that ‘the outcomes after arthroscopic lavage or arthroscopic debridement were no better than those after a placebo procedure’.56
THE EXPERIENCE OF PAIN
Empathy, or experiencing another’s pain, has biological correlates. Again, under fMRI, empathy has been shown to be associated with similar changes in brain activity to those in the loved one actually experiencing the pain. Although the body is not registering physical pain, in empathy a person ‘suffers’ emotionally as they would if they were experiencing physical pain.57 ‘Stress’ also affects acute and chronic pain perception. Chronic pain syndromes are very common in individuals with anxiety, depression, poor coping and high levels of helplessness and hopelessness. Equally, it is often difficult to identify somatic disease in such conditions as burnout, multiple chemical sensitivity, chronic musculoskeletal pain, chronic low back pain, chronic fatigue syndrome and fibromyalgia. In chronic pain syndromes, evidence suggests that neural loops become sensitised to register the experience of pain with minimal stimuli. They are maintained by ‘sustained attention and arousal’ in that the person is constantly vigilant for, and reactive to, pain messages.58,59 It may be through the reversal of such effects that practices such as mindfulness, which reduce arousal and reactivity and refocus attention, have excellent long-term effects in the management of chronic pain.60
The comorbidity of chronic pain and depression may be partly explained by the fact that pain alters the hippocampus and gene expression, and reduces neurogenesis. In total, this adds up to the sensitisation of the nervous and limbic systems, in depressed patients.61
Chronic pain conditions are responsive to a range of mind–body interventions. For example, a study62 of irritable bowel patients found that 71% initially responded to hypnosis and, of these, 81% maintained their improvement in the longer term. This correlated with improvements in quality of life, anxiety or depression scores, and led to a reduction in consultation rates and medication use. These benefits were still demonstrable after 5 years.
THE EFFECTS OF STRESS REDUCTION
Stress affects immune function (see section on psychoneuroimmunology, later in this chapter), slows wound healing63,64 and alters genetic function, damage and repair (see section on genetic expression, later in this chapter). The implications are enormous.
The relaxation response, on the other hand, reverses the harmful effects of the inappropriate activation of the stress response. The ‘relaxation response’ was first coined by Professor Herbert Benson of Harvard University.65 Although it can be fostered in a variety of ways, the effects are similar: a relaxed physical condition and a focused and alert mental state. This state of body and mind is sometimes called ‘restful alertness’.
Some of the physical and psychological effects of stress that can be reversed through stress reduction techniques are listed in Boxes 8.1 and 8.2.66 Overall there is a restoration of physiological balance or homeostasis. This movement towards balance, efficiency and health is natural and will take place automatically if it is not interfered with. Similarly, the mind will return to happiness and contentment if it is allowed.
BOX 8.1 Physiological benefits of relaxation and stress reduction
Some insurance companies are interested in the health benefits of stress reduction and meditation. This interest is based on the findings of some large audits. One compared 600,000 non-meditators to 2000 meditators.108 The findings demonstrated reduced illness rates and medical care utilisation in every disease category. For example, there was an 87% reduction in heart disease and a 55% reduction in tumours among those who meditated compared with those who didn’t. Follow-up over an 11-year period showed further improvements, with an overall 63% reduction in healthcare costs (that is, 63 cents in the health dollar saved), with less than one-eleventh the number of hospital admissions for cardiovascular disease, one-third the number for cancer and one-sixth the number for mental disorders and substance abuse, in meditators compared with non-meditating controls.109 These studies did not control for all lifestyle and personality factors, and so self-selection and healthy lifestyle change would have contributed to the results along with direct physiological benefits. On the strength of the evidence, some insurance companies in the United States and Europe offer substantial reductions in life insurance premiums of up to 30% for those who regularly practise an approved form of meditation, in this case transcendental meditation (TM).
PSYCHONEUROIMMUNOLOGY
Although the notion that the mind affects our resistance to disease dates back thousands of years, PNI began to gain credence in the mid-1970s. Communication between the CNS and the immune system takes place via ‘hard wiring’ (nerves) and a ‘postal system’ (blood-borne hormones and neurotransmitters). By these two means the CNS communicates with every element of our immune defences in a bi-directional feedback system.111,112 Over 70 neurotransmitter receptors have been found on the surface of white blood cells. Especially important in the feedback loop are the limbic system in the brain, primarily concerned with emotion, and the prefrontal lobes. A predominance of left-prefrontal lobe activity is associated with better mood, optimism, intense positive emotion response to emotionally positive stimuli and an ability to minimise negative affect in daily life.113–115 This correlates with greater natural killer (NK) cell activity. Predominantly right-brain active people experience lower mood, more pessimism and intense negative emotion in response to emotionally negative stimuli. The right prefrontal lobe is more important for antibody and immunoglobulin response.116
The ‘chemistry of thought’ is not localised to the brain, because the same neurotransmitter receptors are found in virtually every tissue in which they are sought. This goes a long way to explaining how emotional states such as stress, anxiety and depression cause distant physiological effects and affect susceptibility to disease. Also important is the fact that drugs that have psychoactive properties are also found to affect immune function and have clinically relevant side effects on immunity. Furthermore, the blood–brain barrier is made more porous by stress117 and PNI mechanisms may play a role in the development of psychiatric disorders.3
There are many ways of measuring immune status. The commonly used measures of immunity are simply the number and types of immune cells—this indicates ‘how large the army is’ but tells us little about how well it is functioning. Tests of immune cell function are more specialised and expensive but are designed to give a more important indicator of how well the cells are performing their designated roles.118 Such tests include measuring white blood cell ‘proliferation’ in response to an antigenic challenge and measuring how well NK cells kill tumour cells through a cytotoxic activity assay. These tests are performed in vivo. Other tests are performed in vitro by measuring the body’s ability to stimulate antibodies or the delayed-type hypersensitivity response (allergic response). Negative emotional states have a negative effect on immunity largely by affecting how well immune cells carry out their core functions, such as lymphocyte proliferation in response to infection119 or by inhibiting NK cell activity,120 rather than having major effects on cell numbers. In terms of day-to-day health, the size of the army, though important, may be of secondary importance to how well that army is performing. For these reasons compromised immune function due to stress is harder to pick up on standard blood tests, which give cell counts but tell us little about how well those cells are functioning.
Immune cells discriminate ‘self’ from ‘non-self’ and do not attack self unless that cell has become a threat, as in cancer, or it has become infected by a virus. Immune dysfunction occurs when immune cells lose their ability to discriminate between self and non-self, attacking healthy tissue inappropriately or not attacking things that should be attacked. The former, through inflammatory mechanisms, leads to autoimmune and inflammatory diseases, and the latter, through immunosuppression, predisposes to infections and cancer. During high-stress periods there is a shift towards the type-2 immune response and type-2-mediated conditions (infections, latent viral expression, allergic conditions and autoimmune conditions).121 This inappropriate response is called immune ‘dysregulation’ and partially explains the increased incidence or relapse of such illnesses during high-stress periods (Box 8.3).
Immune cells mirror emotional states122 and emotional states are associated with a variety of disease states, whether as a result of an accumulation of many small stressors or the impact of large ones. An accumulation of small daily stressors can be as detrimental to health as major stressors, if not more so.123 Changes in immune cell numbers and function start to occur within five minutes of an event that is perceived to be stressful.124 Depending on the reaction to the stressor, that effect can remain for up to 72 hours afterwards.125 If a person perceives that they have some control over the situation or control over their response to the situation, then they are partially protected from the stress and its consequent immunosuppressive effects. People who perceive that they have no control over the event or their response to it, especially if they are anxious to be in control, experience prolonged negative effects on immune function.
Acute stress alters quantitative and functional components of cellular immunity, and individuals vary markedly in the magnitude of their response. These differences can be predicted by individual variability in perception and consequent stress-induced hypothalamic-pituitary-adrenal-axis (HPA-axis) and SNS activation. Those who have higher SNS reactivity to stress (increased blood pressure, heart rate, catechol secretion) have the greatest disturbance to immunity and susceptibility to infection in response to stressful events. These variations are of clinical significance.126 High cortisol reactors with high levels of life events have approximately double the incidence of verified upper respiratory infection than high reactors with low levels of life events and low reactors irrespective of their life event scores.127 This has been further illustrated in studies measuring the stress levels of medical interns and their correlation with immunity.128
Salivary immunoglobulin A (S-IgA) is the first line defence against infection in the respiratory gastrointestinal and urinary systems, and is one of the easiest markers of immune competence to measure. Low levels of S-IgA are associated with increased risk of infection129,130 and have been found to be reduced by stressful life events such as exam pressure, social isolation,131 grief,132 anxiety133 and the ‘need to have power and to influence others’.134 Positive emotional states, however, are associated with immunoenhancement.135,136 S-IgA can be increased or decreased for 4–5 hours even by inducing positive (e.g. care and compassion) or negative (e.g. anger and frustration) emotions for only 5 minutes.137 Mental and emotional states also influence the speed of wound healing due to the effects on interleukins and cytokines.138
In response to ‘standardised stressors’ some people experience immunoenhancement and others immunosuppression, depending on the person’s perception of the event. Studies of life stress and its impact on cancer incidence have had similar findings. In determining the impact of stress upon health it is important to take into account the individual’s perception and coping style. Those with positive perceptions and coping styles consistently experience immunoenhancement, including improved NK cell activity and S-IgA, and those with negative perceptions and coping styles consistently experience immunosuppression.139–141 Furthermore, those who have higher SNS reactivity to stress as measured by increased blood pressure, heart rate and catechol secretion also seem to have the greatest disturbance to immunity when under stress.142 Immune change is also predicted by brain activity.143
Lifestyle factors can also influence immune function significantly (see Table 8.1).144 A healthy lifestyle helps our immune function to operate at an optimal level. No lifestyle factor is innately ‘good’ unless it is at the right level. For example, exercise prior to infection can enhance immunity and be protective against becoming ill, but high-intensity exercise after infection can worsen the infection and the symptoms. Very intense or prolonged exercise, because of the effects on allostatic load, can reduce immunity and predispose to infections. Elite athletes, for example, tend to have poor immunity.145 So too much and too little exercise are both associated with poor immunity, as are too much and too little sleep. Being employed is good for health but too little or too much work is associated with poor health.146
TABLE 8.1 Lifestyle and effect on natural killer cell activity144
| Behaviour | Advantage in NK activity (%) |
|---|---|
| Exercise | 47 |
| Managing stress | 45 |
| Enough sleep | 44 |
| Balanced meals | 37 |
| Not smoking | 27 |
| Eating breakfast | 21 |
| Working moderate hours | 17 |
| Avoiding alcohol | 0 |
An unhealthy lifestyle is promoted by stress147 and depression,148 and therefore effective stress management is a prerequisite for sustained healthy lifestyle change.149 Meditation,150 psychological interventions such as CBT,151,152 a positive attitude and humour153 are all powerful immune system stimulants in that they help to reverse the immunosuppressive effect of stress.
The abovementioned fluctuations in immune function are significant factors in susceptibility to infection.154 The likelihood of contracting a clinical infection when exposed to a virus is directly proportional to the level of stress that the host was experiencing not just at the time of exposure but during the preceding months. The severity of a viral illness, such as influenza, is greater with higher stress levels.155 There is also a strong link between high stress and relapse for chronic infections such as herpes viruses,156 HIV and shingles. Such viruses lie dormant and are more able to reactivate when the immune system is depleted. Data show that stress and social connectedness are important factors affecting the rate of progression of HIV to AIDS.157 Those who were experiencing above-average levels of stress and had below average levels of social support were 2–3 times more likely to progress to AIDS over a 5-year follow-up. For every one severe stressor per 6-month study interval, the risk of early disease progression to AIDS was doubled.158 Such observations indicate the importance of offering psychological interventions as a part of standard care. For example, giving CBT to HIV-positive men reduced depression and anxiety, and these changes were paralleled by reductions in stress hormones, improvements in white cell counts159 and elevation of DHEA (dehydroepiandrosterone),160 which is also an important hormone in patients with chronic fatigue syndrome.
Studies of medical students152 during the exam period reveal profound immunosuppression, with lowered NK-cell activity, a 90% reduction in gamma interferon and lowered response of T-cells, which corresponds with the tendency to succumb to illness during or just after exams. Students who learn and practise relaxation techniques show significantly better immune function and less illness in exam periods. Even keeping a journal about significant life events is associated with improved immune function and fewer doctor visits for infectious disease.161 Carers have been found to exhibit immune suppression proportional to the level of distress they feel.162 The degree of immunosuppression observed in those going through a stressor such as marital separation is proportional to the amount of negative emotion and difficulty the person experiences in letting go.
AUTOIMMUNE AND INFLAMMATORY ILLNESSES
Mediators of inflammation play an important role in many illnesses. Cytokines can be typed as type 1 (e.g. γ-interferon) or type 2 (e.g. interleukin-10). A high ratio of type 1 to type 2 leads to what is called a ‘type-1 response’ and a low ratio leads to a ‘type-2 response’. It has been shown that during high-stress periods there is a shift towards the type-2 response, which partially explains the increased incidence of type-2-mediated conditions including infections, latent viral expression, allergic conditions and autoimmune conditions during high-stress periods.163 Thus, psychological state not only regulates the level of immune response but also the type of response. This inappropriate immune response is called immune ‘dysregulation’. Autoimmune diseases are associated with immune dysregulation, whether the response is directed to the joints in rheumatoid arthritis or the myelin sheath in multiple sclerosis. Even coronary heart disease has a significant inflammatory component. PNI offers potential explanations of the mechanisms by which stressful life events and unsupportive social environments can trigger and exacerbate a variety of autoimmune diseases.164–166
For example, stress is associated with increased inflammation, pain and disease activity in rheumatoid arthritis patients.167 Those with supportive relationships and better coping skills are noted to have lower levels of inflammatory hormones such as interleukins.168 ‘Irrational beliefs [that are stress-inducing] are associated with increased inflammation process, among apparently healthy individuals.’169 There are also established links between major depression, early life stress and adverse health outcomes in inflammatory diseases.170 Systemic lupus erythematosus (SLE) is also significantly affected by life stress,171 as is multiple sclerosis.172 From a clinical perspective, the important point is that the comprehensive treatment of any inflammatory or autoimmune illness requires the management of life stress, but unfortunately such interventions are too often ignored or seen as being of peripheral importance. Innovative studies, such as the following, have shown significant promise:
ALLERGIES
As with immunosuppression, it is possible to classically condition allergies by pairing a stimulus with exposure to the allergen.176 At present it is not known whether they can be un-conditioned. Unhealthy lifestyle and poor physical and mental health practices have been implicated in the aggravation of allergies.177 The reverse hypothesis—that stress reduction reduces allergies—is still to be comprehensively tested, but some evidence suggests that it can play a role. For example, the treatment of atopic dermatitis was more successful and required fewer topical steroids when it was combined with relaxation therapy, CBT and an education program.178 It has been further demonstrated that stress is an important prognostic factor for response to immunotherapy.179
STRESS AND IMMUNISATION
The efficacy of vaccination such as with the hepatitis B or influenza vaccines is affected by stress. Those who are stressed prior to vaccination have significantly worse antibody and T-cell response,180,181 and reducing stress has been demonstrated to improve response to flu vaccination.49
PSYCHOGENETICS
Studies on animals and humans182,183 have revealed that psychological stress can induce DNA damage and chromosomal aberrations. Mental state can not only increase the number of genetic mutations, but can also impair the body’s ability to repair damage.184 DNA damage is particularly important in the genesis of cancer,185 which is also affected by genetically modulated cell replication, cell death (apoptosis) and cancer suppressor genes. Damage to these genes can lead to cancer.
DNA repair capacity (DRC) is a measure of the cell’s ability to repair damage. Stresses, such as coping with trauma, while increasing oxidative damage to DNA, also stimulate compensatory DNA repair mechanisms.186 During periods of high stress, such as during exams, compared to periods of low stress, such as after vacations, there is an increase in DRC in most people,187 implying an adaptive response to increased DNA damage. Those with higher and more consistent stress and mood disturbance have high DNA damage but no increase, or even a reduction, in DRC in high-stress periods, suggesting that the response has been impaired in some way. The implications may be significant. For example, studies comparing DRC in women with and without breast cancer showed that the DRC of those with cancer was lower than that in the control group.188 A 1% decrease in DRC corresponded to a 22% increase in breast carcinoma risk, with younger breast cancer patients having a more significant reduction in DRC. Thus, DRC may be a useful marker in predicting susceptibility.
Psychological state affects genetic expression in other ways. A genetic predisposition to an illness—such as addictive behaviours,189 cardiovascular reactivity,190 depression,191 schizophrenia192 and asthma193—is commonly activated by stress. Rather than saying that stress is the cause of the illness, it might be more accurate to say that it is a common trigger for many disease processes. In schizophrenia, for example, the ‘normal in-growth of dopamine fibres during late adolescence and their formation of aberrant connections with abnormal intrinsic cortico-limbic circuits could “trigger” the onset of symptoms in those who carry the constitutional vulnerability for schizophrenia’. In terms of genetic tendency to addictive behaviours, ‘stresses, such as drug use and social adversity, in adolescence or early adult life may propel the neuro-developmentally impaired individual over a threshold into frank psychosis’.194 Drug-seeking behaviour can be triggered by various factors, including ‘priming injections’, drug-associated environmental stimuli and stress. Drug-associated stimuli and stress may activate this system via neural circuits from the prefrontal cortex, amygdala and HPA-axis.
Psychological and social factors also significantly affect the rate of genetic ageing. Telomeres can be used as a marker of genetic age. A study of healthy premenopausal women found that psychological stress, in terms of both perception and chronicity, is significantly associated with higher oxidative stress, lower telomerase activity (the enzyme that repairs telomeres) and shorter telomere length. Women with the highest levels of perceived stress compared with low-stress women had telomeres shorter on average by the equivalent of 9–17 years of additional ageing.195 This has many implications for understanding how stress promotes earlier onset of age-related diseases. Mental illness is a major risk factor for CVD. Part of this may be associated with accelerated genetic ageing. Telomere shortness and low telomerase activity are associated with exaggerated autonomic reactivity (allostatic load) to acute mental stress and elevated nocturnal catechol secretion. Low telomerase activity is also associated with risk factors for CVD—smoking, lipids, high blood pressure, high fasting glucose and greater abdominal adiposity (metabolic syndrome).196
The inherited disposition to depression can be activated by the interaction between heredity and upbringing. Developmentally, this is crucial for risk later in life. Childhood trauma (CT) and genetic factors contribute to the pathophysiology of depression, and experience of at least one type of CT is reported by 80% of adults with depression. The common traumas include physical neglect, emotional abuse and emotional neglect. There is an earlier age of onset of depression in those with CT and earliest onset in those with highest CT.197 Children raised in deprived environments can consequently have severe cognitive and behavioural difficulties and poor response to stress lasting into adulthood. These changes are associated with ongoing alterations in gene expression, ‘environmental programming’ and downstream effects on the HPA axis.198
PERSONALITY AND ILLNESS
Research in this field is inherently difficult due to the varying personality classifications and interpretations. Classifying personality types by clustering groups of traits together can be simplistic and risks ignoring the infinite variation and subtlety of human character and psychology. For example, studies of type A (hard-driving, ambitious, aggressive etc) personalities give inconsistent findings. Some suggest it is a risk factor for heart disease, but others do not.199 More recent and decisive studies have concentrated more on individual traits, such as anger or hostility, rather than combining a number of traits. This may make more sense, as personality traits are blended differently in every individual and traits can be interpreted differently. One person might be ambitious or hard-driving, for example, but in a very compassionate and altruistic way, whereas another may be self-centred. Assertiveness can be useful or destructive, depending on which aspect of our nature is asserting itself. A person with emotional intelligence may experience anger but will be able to determine whether it is worth expressing or not.
Be that as it may, some research has demonstrated that particular personality types may be predisposed to particular types of illnesses. For example, the personality types listed below have been implicated, with differing incidences, in cancer, coronary heart disease (CHD) and overall mortality when individuals with these personality types were followed over 10 years.200
Establishing an unambiguous causal relationship between personality and illness is inherently difficult. Other lifestyle factors may not be controlled. Testing the hypothesis that altering personality traits alters future risk of disease is also difficult. Some research has suggested that minimising unhelpful personality traits and communication patterns and enhancing better ones has a positive long-term effect on physical and psychological health.201,201 Cancer-prone and heart-disease-prone individuals given ‘autonomy training’ over 6 months had far lower all-cause and cause-specific mortality than the control group. This suggests that as personality markers change, so too does the disease profile.
Other studies on patients with established and severe CHD202 show that those with a ‘type D’ personality are nearly five times more likely to have another acute myocardial infarction (AMI) in the next 6–10 years. Type D personality is made up of two main elements: a high level of negative affect (anxiety, anger, worry etc) and a tendency to withhold the expression of these emotions. Emotional stress and its suppression have also been found to increase the number of ischaemic episodes by a factor of 2.2, even when controlled for other factors.203 Among emotions, chronic anger and hostility seem to be most unhealthy, not just for CHD risk but also possibly for cancer risk204,205 and survival.206 Other studies have given conflicting results.207 Part of the discrepancy is explained by the fact that many studies do not control as stringently for individual perception and coping style. People perceive the same events differently. For example, two people undergoing divorce will respond differently. For one it may be a relief of stress and for another a trauma, and in each case the physiological, endocrine and immune response will react to the perception of the event rather than the event itself. Therefore, the former is at minimal increased risk of illness, whereas the latter has a much higher risk.
MIND–BODY INTERVENTIONS
Almost any therapy that affects a person’s mental and emotional states, because it will have consequent effects on their physical state, could be considered a mind–body therapy. For example, various meditative techniques have been found to be helpful for a range of conditions as diverse as epilepsy, premenstrual syndrome, menopausal symptoms, mood and anxiety disorders, and coping with serious illnesses, with few or no significant adverse events reported.208 Yoga therapy also has a range of benefits.209 Mind–body techniques will be helpful as adjuncts or alternatives in a far wider range of illnesses and symptoms but evidence on their efficacy sometimes lags behind community and practitioner experience. It is important that a GP who wishes to use mind–body strategies in the consulting room has adequate training. Although largely safe, their efficacy can be diminished and the potential for adverse events increased when used by inexperienced practitioners.
Techniques that can be included in the classification of mind–body therapies are described below.
Mindfulness-based therapies
A range of therapies use mindfulness principles, including mindfulness-based stress reduction (MBSR),210 mindfulness-based cognitive therapy (MBCT),211 as well as acceptance commitment therapy (ACT) and dialectic behaviour therapy (DBT). There is a high level of clinical and research interest in mindfulness-based therapies because of promising outcomes in mental health212 and neurosciences. Mindfulness uses meditative practices in conjunction with a range of cognitive strategies.213
Autogenic training and hypnosis
Autogenic training and hypnosis are often associated with trance states. Like meditation training, they also involve focal awareness—for example, concentrating on a swinging pendulum. Unlike meditative practices, they involve the induction of a condition in which critical faculties are suspended and the ‘limits of … a person’s … usual frame of reference and beliefs temporarily altered … making him/her … receptive to other patterns of association and modes of mental functioning’.214 It can also use concentration on ‘heaviness’ or ‘warmth’ and uses power of suggestion. It can be induced by others or self-induced. There is clear evidence that these techniques can be useful for a variety of conditions.
Affirmations
Affirmations use a statement to ‘un-condition’ an unhelpful thought pattern and replace it with a more positive one. They are specific and goal-directed. The statement works best if it is short, true and repeated many times a day until it becomes automatic. Affirmations can be incorporated with deep relaxation, but to be effective the thought needs to be supported and reinforced by action.
PRACTISING MINDFULNESS MEDITATION
Mindfulness is about raising awareness and as such it is also about learning to concentrate, in a restful way. There are few contraindications to mindfulness-based practices but acute psychosis and intoxication are probably two. There is, however, some recent evidence that mindfulness-based approaches taught during remission may be useful in improving functioning and reducing some symptoms in patients with psychosis.215 Caution should also be exercised for the inexperienced, to avoid moving on to intensive practice too soon.
THE BODY SCAN
Initially, be conscious of the whole body and let it settle. Now, progressively become aware of each individual part of the body, starting with the feet and then moving to the legs, stomach, back, hands, arms, shoulders, neck and face. Take your time. The object of this practice is to let the attention rest with each part, simply noticing what is happening there, what sensations are taking place, moment by moment. Practise cultivating an attitude of impartial awareness, that is, not having to judge the experiences as good or bad, right or wrong. Simply accept them as they are. There is no need to change your experience from one state to another or to ‘make something happen’. Observing the mind judge, criticise or become distracted, for example, are simply mental experiences to observe non-judgmentally as they come and go. As often as the attention wanders from an awareness of the body, simply notice where the attention has gone and gently bring it back to an awareness of the body. It is not a problem if thoughts come in or the mind becomes distracted.
Benson-Henry Institute for Mind Body Medicine. http://www.massgeneral.org/bhi/default.aspx.
Center for Mindfulness in Medicine, Health Care and Society, University of Massachusetts Medical School. http://www.umassmed.edu/content.aspx?id=41252.
Centre For Mindfulness Research And Practice, Bangor University. http://www.bangor.ac.uk/mindfulness/.
Mind and Life Institute. http://www.mindandlife.org/.
What is complementary and alternative medicine? NCCAM background on mind-body medicine. http://nccam.nih.gov/health/whatiscam/mind-body/mindbody.htm.
Ader R. Psychoneuroimmunology. Burlington: Elsevier, 2007.
Doige N. The brain that changes itself. New York: Penguin, 2007.
Harrington A. The cure within: a history of mind-body medicine. New York: Random House, 2008.
Hassed C. Know thyself: the stress release program. Melbourne: Michelle Anderson Publishing, 2002.
Hassed C. The essence of health: the seven pillars of wellbeing. Sydney: Ebury Press, 2008.
Segal Z, Williams M, Teasdale J. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press, 2002.
Siegal D. The mindful brain. New York: WW Norton, 2007.
Watkins A. Mind-body medicine: a clinician’s guide to psychoneuroimmunology. New York: Churchill Livingstone, 1997.
Williams M, Teasdale J, Segal Z, et al. The mindful way through depression: freeing yourself from chronic unhappiness. New York: Guilford Press, 2007.
1 World Health Organization. Online. Available: www.who.int/en/.
2 Astin J. Why patients use alternative medicine: results of a national study. JAMA. 1998;280(9):784-787.
3 Muller N, Ackenheil M. Psychoneuroimmunology and the cytokine action in the CNS: implications for psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 1998;22(1):1-33.
4 Porter RJ, Gallagher P, Watson S, et al. Corticosteroid-serotonin interactions in depression: a review of the human evidence. Psychopharmacology (Berl). 2004;173(1/2):1-17.
5 Brown MA, Buddle ML, Martin A. Is resistant hypertension really resistant? Am J Hypertens. 2001;14(12):1263-1269.
6 McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann NY Acad Sci. 2004;1032:1-7.
7 Dunn AJ, Swiergiel AH, de Beaurepaire R. Cytokines as mediators of depression: what can we learn from animal studies? Neurosci Biobehav Rev. 2005;29(4/5):891-909.
8 Rutz W. Rethinking mental health: a European WHO perspective. World Psychiatry. 2003;2(2):125-127.
9 Miller M, Rahe R. Life changes scaling for the 1990s. J Psychosom Res. 1997;43(3):279-292.
10 Ustun TB, Ayuso-Mateos JL, Chatterji S, et al. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386-392.
11 Mathers CD, Vos ET, Stevenson CE, et al. The Australian Burden of Disease Study: measuring the loss of health from diseases, injuries and risk factors. Med J Aust. 2000;172(12):592-596.
12 Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
13 McKelvey R, Pfaff J, Acres J. The relationship between chief complaints, psychological distress, and suicidal ideation in 15–24-year-old patients presenting to general practitioners. Med J Aust. 2001;175:550-552.
14 Jureidini JN, Doecke CJ, Mansfield PR, et al. Efficacy and safety of antidepressants for children and adolescents. BMJ. 2004;328(7444):879-883.
15 Vitiello B, Swedo S. Antidepressant medications in children. N Engl J Med. 2004;350(15):1489-1491.
16 Hallfors DD, Waller MW, Bauer D, et al. Which comes first in adolescence—sex and drugs or depression? Am J Prev Med. 2005;29(3):163-170. a p 163.
17 Young R, Sweeting H, West P. Prevalence of deliberate self-harm and attempted suicide within contemporary Goth youth subculture: longitudinal cohort study. BMJ. 2006;332(7549):1058-1061.
18 Martino SC, Collins RL, Elliott MN, et al. Exposure to degrading versus nondegrading music lyrics and sexual behavior among youth. Pediatrics. 2006;118(2):e430-e441.
19 Bressan RA, Crippa JA. The role of dopamine in reward and pleasure behaviour—review of data from preclinical research. Acta Psychiatr Scand Suppl. 2005;427:14-21.
20 Brake WG, Zhang TY, Diorio J, et al. Influence of early postnatal rearing conditions on mesocorticolimbic dopamine and behavioural responses to psychostimulants and stressors in adult rats. Eur J Neurosci. 2004;19(7):1863-1874.
21 Kjaer TW, Bertelsen C, Piccini P, et al. Increased dopamine tone during meditation-induced change of consciousness. Brain Res Cogn Brain Res. 2002;13(2):255-259.
22 Covey LS, Glassman AH, Stetner F. Depression and depressive symptoms in smoking cessation. Compr Psychiatry. 1990;31:350-354.
23 Breslau N, Peterson EL, Schultz LR, et al. Major depression and stages of smoking. A longitudinal investigation. Arch Gen Psychiatry. 1998;55:161-166.
24 Hurt RD, Sachs DP, Glover ED, et al. A comparison of sustained-release bupropion and placebo for smoking cessation. N Engl J Med. 1997;337(17):1195-1202.
25 Hall SM, Muñoz RF, Reus VI. Cognitive-behavioral intervention increases abstinence rates for depressive-history smokers. J Consult Clin Psychol. 1994;62:141-146.
26 Small DM, Zatorre RJ, Dagher A, et al. Changes in brain activity related to eating chocolate: from pleasure to aversion. Brain. 2001;124(9):1720-1733.
27 Kim SW, Grant JE, Adson DE, et al. Double-blind naltrexone and placebo comparison study in the treatment of pathological gambling. Biol Psychiatry. 2001;49(11):914-921.
28 Epiquote. Epictetus. Online. Available: http://en.wikiquote.org/wiki/Epictetus.
29 Sims J. The evaluation of stress management strategies in general practice: an evidence-led approach. Br J Gen Pract. 1997;47(422):577-582.
30 Taylor SE, Klein LC, Lewis BP, et al. Biobehavioural responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev. 2000;107(3):411-429.
31 Girdler SS, Jamner LD, Shapiro D. Hostility, testosterone and vascular reactivity to stress: effects of sex. Int J Behav Med. 1997;4:242-263.
32 Holstrom R. Female aggression among the great apes: a psychoanalytic perspective. In: Bjorkqvist K, Niemela P., editors. Of mice and women: aspects of female aggression. San Diego, CA: Academic Press; 1992:295-306.
33 Uvans-Moberg K. Oxytocin-linked antistress effects—the relaxation and growth response. Acta Psychiatr Scand. 1997;640(Suppl):38-42.
34 Altemus M, Deuster A, Galliven E, et al. Suppression of hypothalamic-pituitary-adrenal axis response to stress in lactating women. J Clin Endocrinol Metab. 1995;80:2954-2959.
35 Willcock SM, Daly MG, Tennant CC, et al. Burnout and psychiatric morbidity in new medical graduates. Med J Aust. 2004;181(7):357-360.
36 Hallowell EM. Overloaded circuits: why smart people underperform. Harv Bus Rev. 2005;83(1):54-62. 116.
37 Biggs J. Student approaches to learning and studying. Australian Council for Educational Research: Melbourne, 1987.
38 Bullimore D. Study skills and tomorrow’s doctors. WB Saunders: Edinburgh, 1998.
39 Mayberg HS, Arturo Silva J, Branna SK, et al. The functional neuroanatomy of the placebo effect. Am J Psychiatry. 2002;159(5):728-737.
40 Wager TD, Rilling JK, Smith EE. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303(5661):1162-1167.
41 Goldapple K, Segal Z, Garson C. Modulation of cortical–limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry. 2004;61(1):34-41.
42 Mayberg HS. Modulating dysfunctional limbic-cortical circuits in depression: towards development of brain-based algorithms for diagnosis and optimised treatment. Br Med Bull. 2003;65:193-207.
43 Eriksen HR, Ursin H. Subjective health complaints, sensitization, and sustained cognitive activation (stress). J Psychosom Res. 2004;56(4):445-448.
44 Ursin H, Eriksen HR. Sensitization, subjective health complaints, and sustained arousal. Ann NY Acad Sci. 2001;933:119-129.
45 Rugulies R. Depression as a predictor for coronary heart disease. a review and meta-analysis. Am J Prev Med. 2002;23(1):51-61.
46 Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease: a meta-analysis. Arch Int Med. 1996;156(7):745-752.
47 Pawlak R, Margarinos AM, Melchor J, et al. Tissue plasminogen activator in the amygdala is critical for stress-induced anxiety-like behaviour. Nat Neuroscience. 2003;6(2):168-174.
48 Wang J, Rao H, Wetmore GS, et al. Perfusion functional MRI reveals cerebral blood flow pattern under psychological stress. Proc Natl Acad Sci USA. 2005;102(49):17804-17809.
49 Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65(4):564-570.
50 Lazar SW, Bush G, Gollub RL, et al. Functional brain mapping of the relaxation response and meditation. Neuroreport. 2000;11(7):1581-1585.
51 Lazar SW, Kerr CE, Wasserman RH, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16(17):1893-1897.
52 Kirsch L, Moore TJ, Scoboria A, et al. The emperor’s new drugs: an analysis of antidepressant medication data submitted to the US Food and Drug Administration. Prev Treat. 5(1), 2002. ArtID 23. Online. Available: http://journals.apa.org/prevention/volume5/pre0050023a.html
53 Kirsch I, Deacon BJ, Huedo-Medina TB, et al. Initial severity and antidepressant benefits: a meta-analysis of data submitted to the. Food and Drug Administration PLoS Medicine. 2008;5(2):e45. 10.1371/journal.pmed.0050045.
54 Goldapple K, Segal Z, Garson C, et al. Modulation of cortical–limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry. 2004;61(1):34-41.
55 Wager TD, Rilling JK, Smith EE, et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303(5661):1162-1167.
56 Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347(2):81-88.
57 Singer T, Seymour B, O’Doherty J, et al. Empathy for pain involves the affective but not sensory components of pain. Science. 2004;303(5661):1157-1162.
58 Eriksen HR, Ursin H. Subjective health complaints, sensitization, and sustained cognitive activation (stress). J Psychosom Res. 2004;56(4):445-448.
59 Ursin H, Eriksen HR. Sensitization, subjective health complaints, and sustained arousal. Ann NY Acad Sci. 2001;933:119-129.
60 Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163-190.
61 Duric V, McCarson KE. Persistent pain produces stress-like alterations in hippocampal neurogenesis and gene expression. J Pain. 2006;7(8):544-555.
62 Gonsalkorale WM, Miller V, Afzal A, et al. Long-term benefits of hypnotherapy for irritable bowel syndrome. Gut. 2003;52(11):1623-1629.
63 Glaser R, Kiecolt-Glaser J, Marucha P, et al. Stress-related changes in pro-inflammatory cytokine production in wounds. Arch Gen Psychiatry. 1999;56(5):450-456.
64 Kiecolt-Glaser J, Marucha PT, Malarkey WB. Slowing of wound healing by psychological stress. Lancet. 1995;346:1194-1196.
65 Benson H. The relaxation response. New York: HarperCollins, 2000.
66 Murphy M, Donovan S. The physical and psychological effects of meditation. A review of contemporary research with a comprehensive bibliography 1931–1996. Sausalito, California: Institute of Noetic Sciences, 1997.
67 Kesterton J. Metabolic rate, respiratory exchange ratio and apnoeas during meditation. Am J Physiol. 1989;256(3):632-638.
68 Benson H. The relaxation response and norepinephrine: a new study illuminates mechanisms. Aust J Clin Hypnotherapy Hypnosis. 1989;10(2):91-96.
69 Mills P, Schneider R, Hill D, et al. Beta-adrenergic receptor sensitivity in subjects practicing TM. J Psychosom Res. 1990;34(1):29-33.
70 Delmonte M. Physiological responses during meditation and rest. Biofeedback Self-regulation. 1984;9(2):181-200.
71 Vyas R, Dikshit N. Effect of meditation on respiratory system, cardiovascular system and lipid profile. Indian J Physiol Pharmacol. 2002;46(4):487-491.
72 Surwit RS, van Tilburg MA, Zucker N, et al. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care. 2002;25(1):30-34.
73 Bagga O, Gandhi A, Bagga S. A study of the effect of TM and yoga on blood glucose, lactic acid, cholesterol and total lipids. J Clin Chem Clin Biochem. 1981;19(8):607-608.
74 Echenhofer F, Coombs M. A brief review of research and controversies in EEG biofeedback and meditation. J Transpers Psychol. 1987;19(2):161-171.
75 Deepak KK, Manchanda SK. Maheshwari MC. Meditation improves clinico-electroencephalographic measures in drug-resistant epileptics. Biofeedback Self-regulation. 1994;19(1):25-40.
76 Bujatti M, Riederer P. Serotonin, noradrenaline, dopamine metabolites in TM technique. J Neural Transm. 1976;39:257-267.
77 Jevning R, Anand R, Biedebach M, et al. Effects on regional cerebral blood flow of TM. Physiol Behav. 1996;59(3):399-402.
78 Doraiswamy PM, Xiong GL. Does meditation enhance cognition and brain longevity? Ann NY Acad Sci. 2007; 28 Sep. [Epub ahead of print]
79 Werner OR, Wallace RK, Charles B, et al. Long-term endocrine changes in subjects practicing the TM and TM-siddhi program. Psychosom Med. 1986;48(1/2):59-65.
80 Jedrczak A, Toomey M, Clements G, et al. The TM–siddhi program, age, and brief tests of perceptual motor speed and non-verbal intelligence. J Clin Psychol. 1986;42(1):161-164.
81 Brown D, Forte M, Dysart M, et al. Visual sensitivity and mindfulness meditation. Percept Mot Skills. 1984;58:775-784.
82 Carlson LE, Speca M, Patel KD, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65(4):571-581.
83 Coehlo R, Silva C, Maia A, et al. Bone mineral density and depression: a community study in women. J Psychosom Res. 1999;46(1):29-35.
84 Kabat-Zinn J, Burney R, Lipworth L. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163-190.
85 Wilson AF, Honsberger R, Chiu JT, et al. Transcendental meditation and asthma. Respiration. 1975;32:74-80.
86 Cerpa H. The effects of clinically standardised meditation on type 2 diabetics. Dissertation Abstr Int. 1989;499(8b):3432.
87 Schneider RH, Alexander CN, Staggers F, et al. Long-term effects of stress reduction on mortality in persons ≥ 55 years of age with systemic hypertension. Am J Cardiol. 2005;95(9):1060-1064.
88 Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatry. 1992;149:936-943.
89 Eppley KR, Abrams AI, Shear J, et al. Differential effects of relaxation techniques on trait anxiety: a meta-analysis. J Clin Psychol. 1989;45(6):957-974.
90 Teasdale J, Segal Z, Williams J. How does cognitive therapy prevent depressive relapse and why should attention control (mindfulness) training help? Behav Res Ther. 1995;33(1):25-39.
91 Bujatti M, Riederer P. Serotonin, noradrenaline, dopamine metabolites in TM technique. J Neural Transm. 1976;39(3):257-267.
92 Kornfield J. Intensive insight meditation: a phenomenonological study. J Transpers Psychol. 1979;11(1):48-51.
93 Baer RA, Smith GT, Lykins E, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329-342.
94 Kutz I, Lerserman J, Dorrington C, et al. Meditation as an adjunct to psychotherapy. An outcome study. Psychother Psychosom. 1985;43(4):209-218.
95 Gelderloos P, Walton KG, Orme-Johnson DW, et al. Effectiveness of the TM program in preventing and treating substance misuse: a review. Int J Addict. 1991;26:293-325.
96 Mason L, Alexander C, Travis F, et al. Electrophysiological correlates of higher states of consciousness during sleep in long-term practitioners of the TM program. Sleep. 1997;20(2):102-110.
97 Simpson TL, Kaysen D, Bowen S, et al. PTSD symptoms, substance use, and vipassana meditation among incarcerated individuals. J Trauma Stress. 2007;20(3):239-249.
98 Gaylord C, Orme-Johnson D, Travis F. The effects of the transcendental meditation technique and progressive muscle relaxation on EEG coherence, stress reactivity, and mental health in black adults. Int J Neurosci. 1989;46(1/2):77-86.
99 Wallace RK, Orme-Johnson DW, Mills PJ, et al. Academic achievement and the paired Hoffman reflex in students practicing meditation. Int J Neurosci. 1984;24(3/4):261-266.
100 Carrington P, Collings G, Benson H, et al. The use of meditation and relaxation techniques for the management of stress in a working population. J Occup Med. 1980;22(4):221-231.
101 Slagter HA, Lutz A, Greischar L, et al. Mental training affects distribution of limited brain resources. PLoS Biology. 2007;5(6):e138. 10. 1371/journal.pbio.0050138, Online. Available:
102 Paul G, Elam B, Verhulst SJ. A longitudinal study of students’ perceptions of using deep breathing meditation to reduce testing stresses. Teach Learn Med. 2007;19(3):287-292.
103 Verma IC, Jayashankarappa BS, Palani M. Effect of transcendental meditation on the performance of some cognitive psychological tests. Indian J Med Res. 1982;77(Suppl):136-143.
104 Shah AH, Joshi SV, Mehrotra PP, et al. Effect of Saral meditation on intelligence, performance and cardiopulmonary functions. Indian J Med Sci. 2001;55(11):604-608.
105 Delmonte M, Kenny V. Conceptual models and functions of meditation in psychotherapy. J Contemp Psychother. 1987;17(1):38-59.
106 Hansen E, Lundh LG, Homman A, et al. Measuring mindfulness: pilot studies with the Swedish versions of the Mindful Attention Awareness Scale and the Kentucky Inventory of Mindfulness Skills. Cogn Behav Ther. 2009;38(1):2-15.
107 Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment. 2004;11(3):191-206.
108 Orme-Johnson D. Medical care utilisation and the transcendental meditation program. Psychosom Med. 1987;49:493-507.
109 Orme-Johnson D, Herron R. An innovative approach to reducing medical care utilisation and expenditures. Am J Manag Care. 1997;3:135-144.
110 Salk J. Dossey L, editor. Meaning and medicine. New York: Bantam, 1991.
111 Bovberg DH. Psychoneuroimmunology: implications for oncology? Cancer. 1991;67:828-832.
112 Ader R. Psychoneuroimmunology. Sydney: Elsevier, 2007.
113 Wheeler RE, Davidson RJ, Tomarken AJ. Frontal brain asymmetry and emotional reactivity: a biological substrate of affective style. Psychophysiology. 1993;30(1):82-89.
114 Tomarken AJ, Davidson RJ. Frontal brain activation in repressors and nonrepressors. J Abnorm Psychol. 1994;103(2):339-349.
115 Tomarken AJ, Davidson RJ, Wheeler RE, et al. Psychometric properties of resting anterior EEG asymmetry: temporal stability and internal consistency. Psychophysiology. 1992;29(5):576-592.
116 Kang DH, Davidson RJ, Coe CL, et al. Frontal brain asymmetry and immune function. Behav Neurosci. 1991;105(6):860-869.
117 Covelli V, Maffione AB, Nacci C, et al. Stress, neuropsychiatric disorders and immunological effects exerted by benzodiazepines. Immunopharmacol Immunotoxicol. 1998;20(2):199-209.
118 Cohen S, Herbert T. Health psychology: psychological factors and physical disease from the perspective of human psychoneuroimmunology. Ann Rev Psychol. 1996;47:113-142.
119 Knapp P, Levy E, Giorgi R, et al. Short-term immunological effects of induced emotion. Psychosom Med. 1992;54:133-148.
120 Jemmott J, Hellman C, McClelland D, et al. Motivational syndromes associated with natural killer cell activity. J Behav Med. 1990;13:53-73.
121 Marshall G, Agarwal SK, Lloyd C, et al. Cytokine dysregulation associated with exam stress in healthy medical students. Brain Behav Immun. 1998;12(4):297-307.
122 Hassed C. Psychoneuroimmunology: a Platonic view of the immune system. Aust Fam Physician. 1999;28(9):950-951.
123 Jandorf L, Deblinger E, Neale J, et al. Daily vs major life events as predictors of symptom frequency: a replication study. J Gen Psychol. 1986;113:205-218.
124 Herbert T, Cohen S, Marsland A, et al. Cardiovascular reactivity and the course of immune response to an acute psychological stressor. Psychosom Med. 1994;56:337-344.
125 Sieber W, Rodin J, Larson L, et al. Modulation of human natural killer cell activity by exposure to uncontrollable stress. Brain Behav Immun. 1992;6:141-156.
126 Marsland AL, Bachen EA, Cohen S, et al. Stress, immune reactivity and susceptibility to infectious disease. Physiol Behav. 2002;77(4/5):711-716.
127 Cohen S, Hamrick N, Rodriguez MS, et al. Reactivity and vulnerability to stress-associated risk for upper respiratory illness. Psychosom Med. 2002;64(2):302-310.
128 Tendulkar AP, Victorino GP, Chong TJ, et al. Quantification of surgical resident stress ‘on call’. J Am Coll Surg. 2005;201(4):560-564.
129 Rossen R, Butler W, Wladman R. The protein in nasal secretion. JAMA. 1970;211:1157-1161.
130 Jemmot J, McClelland D. Secretory IgA as a measure of resistance to infectious disease. Behav Med. 1989;15:63-71.
131 Jemmott J, Magloire K. Academic stress, social support and S-IgA. J Pers Soc Psychol. 1988;55:803-810.
132 He M. A prospective controlled study of psychosomatic and immunologic changes in recently bereaved people. Chin J Neurol Psychiatry. 1993;24:90-93.
133 Annie C, Groer M. Childbirth stress—an immunology study. J Obstet Gynecol Neonatal Nurs. 1991;20:391-397.
134 McClelland D, Floor E, Davidson R, et al. Stressed power motivation, sympathetic activation, immune function and illness. J Hum Stress. 1980;6:11-19.
135 Labott S, Ahleman S, Wolever M, et al. The physiological and psychological effects of the expression and inhibition of emotion. Behav Med. 1990;16:182-189.
136 Dillon K, Minchoff B, Baker K. Positive emotional states and enhancement of the immune system. Int J Psychiatry Med. 1986;15(1):13-16.
137 Rein G, Atkinson M, McCraty M. The physiological and psychological effects of compassion and anger. J Advancement Med. 1995;8(2):87-105.
138 Christian LM, Graham JE, Padgett DA, et al. Stress and wound healing. Neuroimmunomodulation. 2006;13(5/6):337-346.
139 Jemmott J, Borysenko J, Borysenko M, et al. Academic stress, power motivation, and decrease in secretion rate of salivary secretory immunoglobulin A. Lancet. 1983;1(8339):1400-1402.
140 Marsland A, Manuck S, Fazzari T, et al. Stability of individual differences in cellular immune response to stress. Psychosom Med. 1995;57:295-298.
141 Boyce WT, Chesney M, Alkon A, et al. Psychobiologic reactivity to stress and childhood respiratory illnesses: results of two prospective studies. Psychosom Med. 1995;57(5):411-422.
142 Manuck S, Cohen S, Rabin B, et al. Individual differences in cellular immune response to stress. Psychol Sci. 1991;2:111-115.
143 Liang SW, Jemerin JM, Tschann JM, et al. Life events, frontal electroencephalogram laterality, and functional immune status after acute psychological stressors in adolescents. Psychosom Med. 1997;59(2):178-186.
144 Kusaka Y, Londou H, Morimoto K, et al. Healthy lifestyles are associated with higher natural killer cell activity. Prev Med. 1992;21:602-615.
145 Malm C, Celsing F, Friman G. Immune defense is both stimulated and inhibited by physical activity. Lakartidningen. 2005;102(11):867-868. 870, 873.
146 Sokejiana S, Kagamimori S. Working hours as a risk factor for acute myocardial infarction in Japan: case control study. BMJ. 1998;317(7161):775-780.
147 Pelletier KR. Mind–body health: research, clinical, and policy applications. Am J Health Promot. 1992;6(5):345-358.
148 Glassman A, Helzer J, Covery L, et al. Smoking, smoking cessation, and major depression. JAMA. 1990;264:1546-1549.
149 Sutherland JE. The link between stress and illness: do our coping methods influence our health? Postgrad Med. 1991;89(1):159-164.
150 Magarey C. Meditation and health. Patient Management. 1989;May:89-101.
151 Crepaz N, Passin WF, Herbst JH, et al. Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychol. 2008;27(1):4-14.
152 Kiecolt-Glaser JK, Glaser R. Psychoneuroimmunology: can psychological interventions modulate immunity? J Consult Clin Psychol. 1992;60(4):569-575.
153 Kiecolt-Glaser JK, McGuire L, Robles TF, et al. Psychoneuroimmunology and psychosomatic medicine: back to the future. Psychosom Med. 2002;64(1):15-28.
154 Cohen S, Tyrrell DA, Smith AP. Psychological stress and the common cold. N Eng J Med. 1991;325:606-612.
155 Cohen S, Doyle WJ, Skoner DP. Psychological stress, cytokine production, and severity of upper respiratory illness. Psychosom Med. 1999;61(2):175-180.
156 Glaser R, Kiecolt-Glaser J, Speicher C, et al. Stress, loneliness and changes in herpes-virus latency. J Behav Med. 1985;8(3):249-260.
157 Leserman J, Jackson E, Petitto J, et al. Progression to AIDS: the effects of stress, depressive symptoms and social support. Psychosom Med. 1999;61(3):397-406.
158 Evans D, Leserman J, Perkins D, et al. Severe life stress as a predictor of early disease progression in HIV infection. Am J Psychiatry. 1997;154:630-634.
159 Antoni MH, Cruess DG, Cruess S, et al. Cognitive-behavioral stress management intervention effects on anxiety, 24-hr urinary norepinephrine output, and T-cytotoxic/suppressor cells over time among symptomatic HIV-infected gay men. J Consult Clin Psychol. 2000;68(1):31-45.
160 Cruess DG, Antoni MH, Kumar M, et al. Cognitive-behavioral stress management buffers decreases in dehydroepiandrosterone sulfate (DHEA-S) and increases in the cortisol/DHEA-S ratio and reduces mood disturbance and perceived stress among HIV-seropositive men. Psychoneuroendocrinology. 1999;24(5):537-549.
161 Kiecolt-Glaser J, Glaser R. Stress and the immune system: human studies. Ann Rev Psychiatry. 1991;11:169-180.
162 Kiecolt-Glaser J, Dura J, Speicher C, et al. Spousal caregivers of dementia victims: longitudinal changes in immunity and health. Psychosom Med. 1991;53:345-362.
163 Marshall G, Agarwal S, Lloyd C, et al. Cytokine dysregulation associated with exam stress in healthy medical students. Brain Behav Immun. 1998;12(4):297-307.
164 O’Leary A. Stress, emotion, and human immune function. Psychol Bull. 1990;108(3):363-382.
165 Homo-Delarche F, Fitzpatrick F, Christeff N, et al. Sex steroids, glucocorticoids, stress and autoimmunity. Steroid Biochem Molec Biol. 1991;40:619-637.
166 De Vellis R, De Vellis B, McEvoy H, et al. Predictors of pain and functioning in arthritis. Health Educ Res: Theory Pract. 1986;1:61-67.
167 Zautra A, Hoffman J, Potter P, et al. Examination of changes in interpersonal stress as a factor in disease exacerbations among women with rheumatoid arthritis. Ann Behav Med. 1997;19(3):279-286.
168 Zautra AJ, Hoffman JM, Matt KS, et al. An examination of individual differences in the relationship between interpersonal stress and disease activity among women with rheumatoid arthritis. Arthritis Care Res. 1998;11:271-279.
169 Papageorgiou C, Panagiotakos DB, Pitsavos C, et al. Association between plasma inflammatory markers and irrational beliefs: the ATTICA epidemiological study. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(8):1496-1503.
170 Pace TW, Mletzko TC, Alagbe O, et al. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. Am J Psychiatry. 2006;163(9):1630-1633.
171 Da Costa D, Dobkin P, Pinard L, et al. The role of stress in functional disability among women with systemic lupus erythematosus: a prospective study. Arthritis Care Res. 1999;12(2):112-119.
172 Coyle P. The neuroimmunology of multiple sclerosis. Adv Neuroimmunol. 1996;6(2):143-154.
173 Kabat-Zinn J, Wheeler E, Light T, et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA). Psychosom Med. 1998;60(5):625-632.
174 Smyth JM, Stone AA, Hurewitz A, et al. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. A randomised trial. JAMA. 1999;281:1304-1309.
175 Young LD. Psychological factors in rheumatoid arthritis. J Consult Clin Psychol. 1992;60(4):619-627.
176 Gauci M, Husband A, Saxarra H, et al. Pavlovian conditioning of nasal tryptase release in human subjects with allergic rhinitis. Physiol Behav. 1994;55(5):823-825.
177 Shirakawa T, Morimoto K. Lifestyle effect on total IgE. Lifestyles have a cumulative impact on controlling total IgE levels. Allergy. 1991;46(8):561-569.
178 Ehlers A, Stangier U, Gieler U. Treatment of atopic dermatitis: a comparison of psychological and dermatological approaches to relapse prevention. J Consult Clin Psychol. 1995;63(40):624-635.
179 Ippoliti F, De Santis W, Volterrani A, et al. Psychological stress affects response to sublingual immunotherapy in asthmatic children allergic to house dust mite. Pediatr Allergy Immunol. 2006;17(5):337-345.
180 Glaser R, Kiecolt-Glaser JK, Bonneau RH, et al. Stress-induced modulation of the immune response to recombinant hepatitis B vaccine. Psychosom Med. 1992;54:22-29.
181 Kiecolt-Glaser JK, Glaser R, Gravenstein S, et al. Chronic stress alters the immune response to influenza virus vaccine in older adults. Proc Nat Acad Sci. 1996;93:3043-3047.
182 Adachi S, Kawamura K, Takemoto K. Oxidative damage of nuclear DNA in liver of rats exposed to psychological stress. Cancer Res. 1993;53(18):4153-4155.
183 Fischman H, Pero R, Kelly D. Psychogenic stress induces chromosomal and DNA damage. Int J Neurosci. 1996;84(1/4):219-227.
184 Kiecolt-Glaser J, Glaser R. Psychoneuroimmunology and immunotoxicology: implications for carcinogenesis. Psychosom Med. 1999;61(3):271-272.
185 Levine A. The tumour suppressor genes. Ann Rev Biochem. 1993;62:623-651.
186 Oldham KM, Wise SR, Chen L, et al. A longitudinal evaluation of oxidative stress in trauma patients. J Paren Enteral Nutr. 2002;26(3):189-197.
187 Cohen L, Marshall G, Cheng L, et al. DNA repair capacity in healthy medical students during and after exam stress. J Behav Med. 2000;23(6):531-545.
188 Ramos JM, Ruiz A, Colen R, et al. DNA repair and breast carcinoma susceptibility in women. Cancer. 2004;100(7):1352-1357.
189 Self D, Nestler E. Relapse to drug seeking: neural and molecular mechanisms. Drug Alcohol Depend. 1998;51(1/2):49-60.
190 Cui Y, Gutstein W, Jabr S, et al. Control of human vascular smooth muscle cell proliferation by sera derived from ‘experimentally stressed’ individuals. Oncol Rep. 1998;5(6):1471-1474.
191 Lopez J, Chalmers D, Little K, et al. Regulation of serotonin 1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: implications for the neurobiology of depression. Biol Psychiatry. 1998;43(8):547-573.
192 Benes F. The role of stress and dopamine-GABA interactions in the vulnerability for schizophrenia. J Psychiatr Res. 1997;31(2):257-275.
193 Mrazek DA, Klinnert M, Mrazek PJ, et al. Prediction of early-onset asthma in genetically at-risk children. Pediatr Pulmonol. 1999;27(2):85-94.
194 Howes OD, McDonald C, Cannon M, et al. Pathways to schizophrenia: the impact of environmental factors. Int J Neuropsychopharmacol. 2004;7(Suppl 1):S7-S13.
195 Epel ES, Blackburn EH, Lin J, et al. Accelerated telomere shortening in response to chronic stress. Proc Natl Acad Sci USA. 2004;101(49):17312-17315.
196 Epel ES, Lin J, Wilhelm FH, et al. Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinol. 2006;31(3):277-287.
197 Moskvina V, Farmer A, Swainson V, et al. Interrelationship of childhood trauma, neuroticism, and depressive phenotype. Depress Anxiety. 2007;24(3):163-168.
198 Meaney MJ, Szyf M. Maternal care as a model for experience-dependent chromatin plasticity? Trends Neurosci. 2005;28(9):456-463.
199 Rozanski A, Blumenthal J, Kaplan J. Impact of psychosocial factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192-2217.
200 Eysenck HJ, Grossarthy-Maticek R. Creative novation behaviour therapy as a prophylactic treatment for cancer and coronary heart disease: Part 2 Effects of treatment. Behav Res Ther. 1991;29:17-31.
201 Eysenck HJ. Psychological factors, cancer and ischaemic heart disease. BMJ. 1992;305:457-459.
202 Denollet J, Brutsaert DL. Personality, disease severity, and the risk of long-term cardiac events in patients with a decreased ejection fraction after myocardial infarction. Circulation. 1998;97:167-173.
203 Gullette EC, Blumenthal JA, Babyak M, et al. Effects of mental stress on myocardial ischaemia during daily life. JAMA. 1997;277:1521-1526.
204 Kune G, Kune S, Watson LF, et al. Personality as a risk factor in large bowel cancer: data from the Melbourne Colorectal Cancer Study. Psychol Med. 1991;21:29-41.
205 Chen C, David A, Nunnerley H, et al. Adverse life events and breast cancer: a case control study. BMJ. 1995;311:1527-1530.
206 Watson M, Haviland J, Greer S, et al. Influence of psychological response on survival in breast cancer: a population-based study. Lancet. 1999;354:1331-1336.
207 Protheroe D, Turvey K, Horgan K, et al. Stressful life events and difficulties and onset of breast cancer: case control study. BMJ. 1999;319:1027-1030.
208 Arias AJ, Steinberg K, Banga A, et al. Systematic review of the efficacy of meditation techniques as treatments for medical illness. J Altern Complement Med. 2006;12(8):817-832.
209 Khalsa SB. Yoga as a therapeutic intervention: a bibliometric analysis of published research studies. Indian J Physiol Pharmacol. 2004;48(3):269-285.
210 Kabat-Zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Delacorte, 1990.
211 Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press, 2002.
212 Teasdale JD, Segal ZV, Williams JMG, et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68:615-623.
213 Hassed C. Know thyself. Melbourne: Michelle Anderson Publishing, 2002.
214 Erickson M, Rossi E. Experiencing hypnosis. New York: Irvington, 1981.
215 Chadwick P, Hughes S, Russell D, et al. Mindfulness groups for distressing voices and paranoia: a replication and randomized feasibility trial. Behav Cogn Psychother. 2009;37(4):403-412.