CHAPTER 20 Midhumeral block
Surface anatomy
The main landmarks for the midhumeral block include the junction between the upper one-third and lower two-thirds of the humerus and the brachial artery. This can be approximated as three fingers’ breadth below the anterior axillary fold (Fig. 20.1).
Sonoanatomy
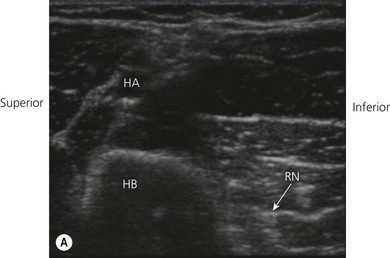
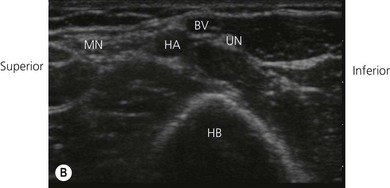
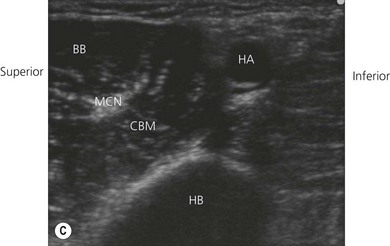
Ultrasound examinations of the brachial plexus through the humeral canal show that ulnar and median nerves are located superficially under the skin. The radial nerve, located beside the humerus, is the most dorsally located nerve of the plexus. The musculocutaneous nerve is situated midway between these two nerves. Images obtained from ultrasound examinations of the brachial plexus through the humeral canal can be illustrated on a graphical synthesis and can be divided into two compartments (Fig. 20.2). A superficial and a dorsal nerve can be found within each compartment. Median and musculocutaneous nerves are located inside the cephalic compartment, whereas the musculocutaneous nerve is located dorsally. Ulnar and radial nerves are located inside the caudal compartment; the radial nerve is located dorsally.
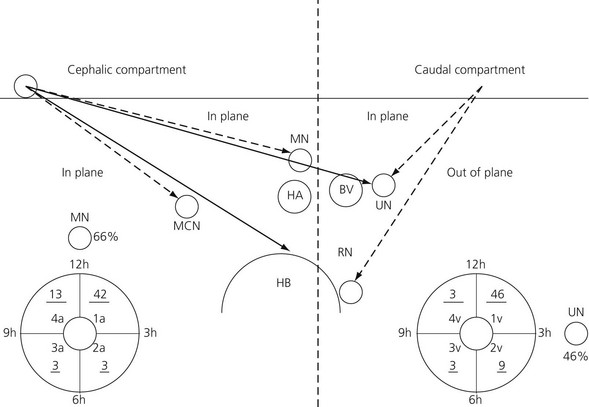
Figure 20.2 Graphical synthesis of the brachial plexus at the level of the humeral canal under ultrasound description. RN: radial nerve; UN: ulnar nerve: MCN: musculocutaneous nerve: MN: median nerve: HA: humeral artery: BV: basilic vein: HB: humerus. The dotted line separates the caudal compartment from the cephalic compartment. The underlined numbers correspond to volunteers. The MN is between 12 and 1 o’clock in 66% of the cases. The UN is situated at the 3 o’clock position in 46% of the cases. The UN and the RN cannot be blocked from a single point of puncture located on the cephalic side of the probe (long line arrows). The 2 points of puncture inside the 2 compartments are mandatory (broken line arrows).1
Technique
Landmark-based approach
The patient is placed supine and the arm abducted at 90°. At the junction between the upper and middle thirds of the arm, a line is drawn over the brachial artery. The needle insertion point is infiltrated with local anesthetic using a 25-G needle. A 50-mm 22-G insulated needle connected to a peripheral nerve stimulator is inserted almost tangentially to the skin, between the brachial artery and the palpating finger, in the direction of the axilla, in order to locate the median nerve (Fig. 20.3). The stimulating current is set at 1.0 mA, 2 Hz, and 0.1 ms. The needle is advanced slowly until the appropriate muscle response is obtained. The needle position is adjusted while decreasing the current to 0.35 mA with maintenance of the muscle response. Stimulation of the median nerve will produce contraction of the flexor carpi radialis and flexor digitorum superficialis of the fingers. Incremental injections of local anesthetic (6–8 mL) are made with repeated aspiration.
After blocking the median nerve, the current is increased to 2 mA, and the needle withdrawn and redirected beneath and medial to the artery (Fig. 20.4). Stimulation of the ulnar nerve induces contraction of the flexor carpi ulnaris muscle. Incremental injection of local anesthetic (6–8 mL) is made with repeated aspiration.
The needle is now withdrawn and, with a high level of stimulation in the subcutaneous position, redirected toward the radial nerve. This nerve is posterior to the artery, close to the humerus (Fig. 20.5). Stimulation of the radial nerve causes contraction of the extensor muscles of the forearm. Incremental injections of local anesthetic (6–8 mL) are made with repeated aspiration.
To block the musculocutaneous nerve, the needle is directed from its initial subcutaneous position beneath the biceps muscle (Fig. 20.6). Stimulation of this nerve induces contraction of the biceps muscle and flexion of the elbow. Incremental injections of local anesthetic (6 mL) are made with repeated aspiration. A final 3 mL is injected medial to the artery to block the medial cutaneous nerves of the arm and the forearm.
Ultrasound-guided approach
The operator stands on the side to be blocked, and with the patient supine and the arm abducted at 90 ° (Fig. 20.7). The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. The humeral canal region is scanned with a 7–13 MHz linear transducer. The ultrasound screen should be made to look like the scanning field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.
With transverse imaging of the humeral canal, in half of the cases, when the point of puncture is situated cephalic to the ultrasound transducer the needle crosses the basilic vein in order to reach the ulnar nerve. Similarly, the radial nerve cannot be blocked through this pathway because the humerus is situated on the pathway of the needle in 58% of cases (Fig. 20.2). It would be possible to introduce the needle on the caudal side of the probe, but in this configuration, movements of the needle are impeded by the upper limb layout.
In this configuration, the radial nerve is initially blocked through an out-of-plane approach. After the transducer has been re-directed anterior to the vessels, the ulnar nerve is blocked within the same point of puncture through an in-plane approach (Fig. 20.8). Nerves from the cephalic compartment are both blocked through an in-plane approach. The deepest nerve is always blocked first; otherwise the injected local anesthetic impedes location of the deepest structures.
Once the needle has approached each individual nerve, 1–2 mL of local anesthetic may be injected to confirm correct needle placement. Local anesthetic appears as a hypoechoic image. Correct needle placement is confirmed by observing solution surrounding each individual nerve (Fig 20.9). Should this not occur, the needle may need to be repositioned, and the procedure repeated. Following confirmation of correct needle placement, 4–6 mL of local anesthetic solution can be injected to achieve blockade of each nerve.
Adverse effects
Clinical pearls
Bouaziz H, Narchi P, Mercier FJ, et al. Comparison between conventional axillary block and a new approach at the midhumeral level. Anesth Analg. 1997;84:1058-1067.
Frizelle HP. Technical note: the humeral canal approach to the brachial plexus. Yale J Biol Med. 1998;71:585-589.
Hickey RM, Hoffman J, Tingle LJ, et al. Comparison of the clinical efficacy of three perivascular techniques for axillary brachial plexus block. Reg Anesth. 1993;18:335-338.
Perlas A, Chan VW, Simons M, et al. Brachial plexus examination and localization using ultrasound and electrical stimulation: a volunteer study. Anesthesiol. 2003;99(2):429-435.