Midfoot & forefoot
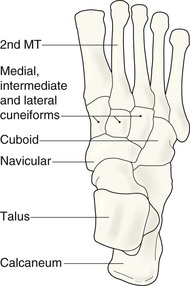
Normal anatomy
The bones of the midfoot form an arch. As a consequence several of the tarsal bones, specifically the three cuneiform bones and the bases of the metatarsals, overlap on both the AP and oblique projections. The individual bones can be separated from one another when the AP and oblique radiographs are examined as a complementary pair.
The cuneiform mortice and the Lisfranc joints
The base of the 2nd metatarsal is held in a mortice created by the three cuneiform bones. This mortice helps to prevent lateral slip of the bases of the metatarsals during weight bearing.
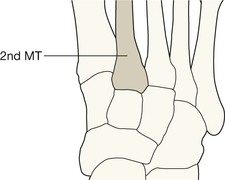
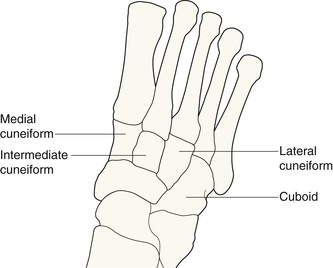
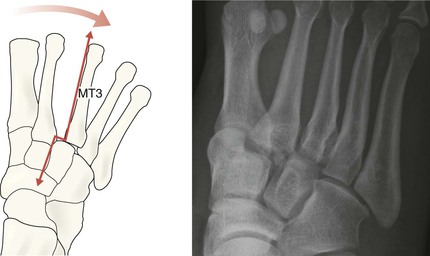
Alignment of 2nd metatarsal and the intermediate cuneiform. May appear “notched”.
Alignment of 3rd metatarsal and the lateral cuneiform. May appear “notched”.
Analysis: the checklists
Analysis of the images will be influenced by the clinical findings such as the precise site of swelling, bruising, tenderness and pain.
The lateral radiograph
Check:
The common fractures
Metatarsals and phalanges
▪ Very common. Some 35% of all foot fractures are metatarsal injuries3. In general, detection of a fracture involving any of the medial four metatarsals is easy.
▪ As many as 70% of all metatarsal fractures involve the 5th metatarsal2.
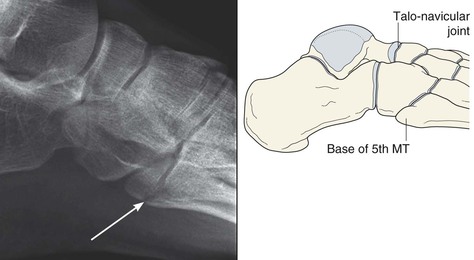
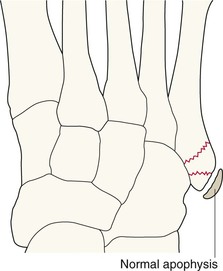
Base of the 5th metatarsal
A fracture of the tuberosity represents an avulsion injury resulting from contraction of the peroneus brevis muscle and the pull of the plantar aponeurosis. It is caused by a plantar flexion–inversion injury.
A patient presenting with a twisted ankle: careful clinical examination of the base of this metatarsal will indicate when radiography of the foot, not the ankle, is necessary.
Fatigue (march/stress) fractures
These injuries are frequently missed, misdiagnosed, mistreated, and misunderstood4.
The 2nd and 3rd metatarsals are most commonly affected.
Radiographs are only abnormal when the fracture is well established. Abnormalities may not be visible for two or more weeks after the onset of symptoms.
If clinical suspicion of a fatigue fracture is high and the initial radiographs appear normal, it is worth considering a radionuclide bone study. Localised increase in uptake of the radiopharmaceutical in the context of a relevant history is diagnostic of a fatigue fracture. Alternatively, in (say) an elite athlete or footballer a similar suspicion would justify an MRI which would quickly confirm or exclude a fatigue fracture.
Infrequent but important fractures
Tarsal bone fractures
Midfoot tarsal bone fractures are uncommon, frequently resulting from high energy trauma. A major injury will be clinically obvious.
Base of the second, 3rd, or 4th metatarsal
Any fracture, whether a major fracture or a very small flake, at any of these sites will signal that there might be a major injury to a tarsometatarsal joint (a Lisfranc joint). See pp. 302–303.
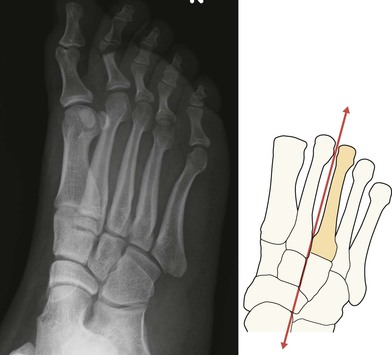
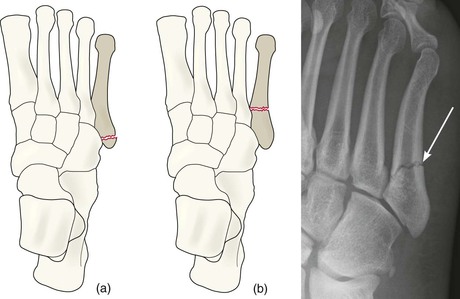
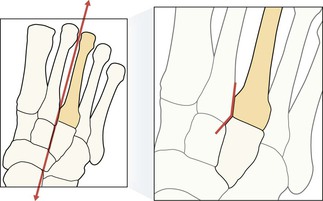
Jones fracture1,2,4–6
Two different fractures involve the proximal shaft of the 5th metatarsal: the very common avulsion injury (p. 298), and the much rarer but clinically important Jones fracture. It is important not to confuse these two fractures.
Jones fractures do not result from a simple avulsion injury.
The Jones fracture was first described by an orthopaedic surgeon, Robert Jones. He sustained the injury and subsequently published his experience7. Descriptions of this fracture in the literature are often confusing.
Clarification: a Jones fracture is a transverse fracture that lies distal to the styloid process of the fifth metatarsal, ie distal to the articulation between the bases of the 4th and 5th metatarsals. Characteristically it is positioned within 1.5 cm of the tuberosity.
A Jones fracture occurs as an acute injury, or, alternatively, following repeated stress affecting this metatarsal. Consequently some Jones fractures are fatigue fractures.
Delayed union or non-union are common problems, especially with a Jones fatigue fracture. In an elite athlete fixation with an intramedullary screw is often required.
Dislocations/subluxations
Direct trauma commonly results in metatarsophalangeal or interphalangeal joint dislocations. These do not cause any difficulty in terms of diagnosis.
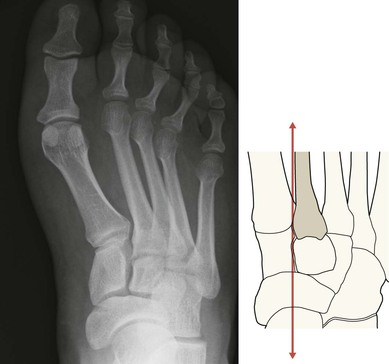
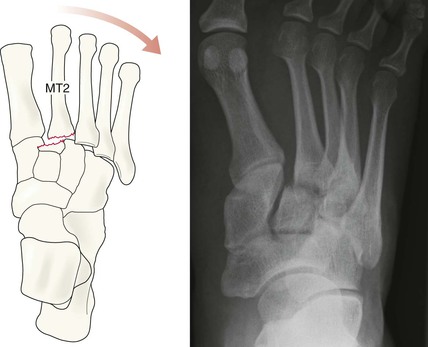
Injury to the tarsometatarsal joints5,8–11
Infrequent but very important. Walking and weight-bearing depend on the accurate alignment of the tarsometatarsal joints (see p. 295). Even a very slight subluxation requires meticulous reduction/management in order to preserve or restore function.
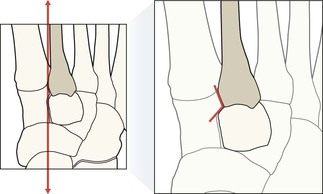
▪ Traumatic subluxations at the bases of the metatarsals (ie Lisfranc injuries) will be overlooked unless the normal alignment of the bones is carefully assessed. The radiographic appearance is often subtle. Always ask two questions:
▪ Subluxation at a Lisfranc joint can occur with or without a fracture.
The reasons why some Lisfranc subluxations are overlooked on the radiographs8–10:
▪ Medical: failure to inspect the radiographs carefully.
▪ Technical: the subluxation may have temporarily reduced because the radiograph is taken with the patient supine and not weight bearing. Apply this rule: whenever there is clinical concern regarding a possible Lisfranc injury and the radiographs appear normal then repeat the radiographs whilst weight bearing. Alternatively, CT or MRI imaging will be diagnostic11.
Pitfalls
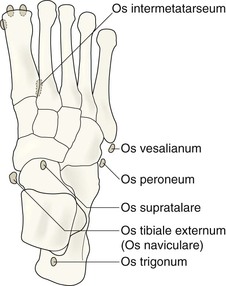
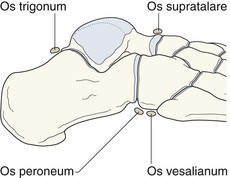
Sesamoids and accessory ossicles
Numerous small bones are present on foot radiographs, and can be erroneously read as fracture fragments.
An unrelated abnormality can cause distraction
Careful history taking and clinical examination is crucial to the correct assessment of the radiographs. Sometimes an unrelated abnormality will distract the unwary.
An error/pitfall8–10 that needs repeated emphasis …
A foot is injured and an injury to a Lisfranc joint is a clinical possibility but the joint appears normal on the radiographs. An injury to the ligaments could still be present if spontaneous reduction of a subluxation has occurred. Remember that the radiographs are obtained as non weight-bearing images and the joint is not under the stress that occurs when the patient is standing. Weight-bearing views (or CT or MRI) should be obtained when there is continuing clinical concern in relation to a Lisfranc joint.