Chapter 17 MICROSCOPIC HEMATURIA
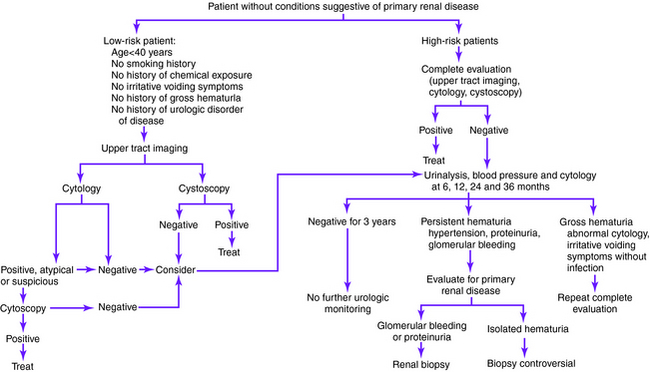
Definitions of microscopic hematuria vary from 1 to more than 10 red blood cells per high-power field on microscopic evaluation of urinary sediment from two of three properly collected urinalysis specimens. The American Urological Association has issued guidelines (Figs. 17-1 and 17-2) for the evaluation of microscopic hematuria in adults and defines clinically significant microscopic hematuria as three or more red blood cells per high-power field. However, each laboratory establishes its own thresholds on the basis of the method of detection used.
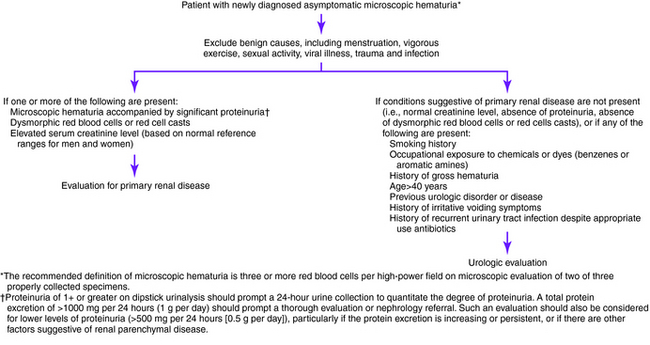
Figure 17-1. Initial evaluation of newly diagnosed microscopic hematuria.
(Adapted from Grossfeld GD, Wolf JS, Litwin MS, et al: Asymptomatic microscopic hematuria in adults: summary of the AUA best practice policy recommendations. Am Fam Physician 2001;63:1145-1154, Figures 1 and 2.)
If a glomerular source is ruled out or considered unlikely, the upper urinary tract should undergo imaging. Excretory urography, ultrasonography, computed tomographic (CT) scanning, or magnetic resonance imaging (MRI) may be used. A CT scan without contrast medium is appropriate as the first test for patients with suspected urinary stone disease. When there is no clinical suspicion of urinary stone disease, CT urography should be performed, first without and then with contrast medium. CT scanning is more expensive than excretory urography and ultrasonography, but it is the best imaging modality for the evaluation of urinary stones, renal and perirenal infections, and associated complications. In addition, with excretory urography and ultrasonography, additional imaging is often necessary for further evaluating cysts. When CT scanning is unavailable, excretory urography or ultrasonography are reasonable alternatives individually or in combination. Ultrasonography is advised in place of CT scanning for patients with renal failure, pregnancy, or hypersensitivity to contrast medium.
Causes of Microscopic Hematuria
• Immunoglobulin A nephropathy
• Hereditary nephritis (Alport syndrome)
• Membranoproliferative glomerulonephritis
• Mesangial proliferative glomerulonephritis
• Mild focal glomerulonephritis of other causes
• Postinfectious glomerulonephritis (endocarditis or viral)
• Poststreptococcal glomerulonephritis
Key Physical Findings
✓ Vital signs, especially blood pressure measurement
✓ Cardiac examination for irregular rhythm, suggestive of atrial fibrillation, or new murmur, suggestive of endocarditis
✓ Abdominal examination for bruits, masses, organomegaly, or aortic aneurysm
✓ Back examination for costovertebral angle tenderness
Suggested Work-Up
| Urinalysis | To evaluate for bacteriuria and pyuria |
| Urine culture | Should be obtained if the urinalysis reveals bacteriuria or pyuria |
| Serum creatinine | To evaluate for renal insufficiency |
| CT urography without and with contrast medium (excretory urography and ultrasonography are alternatives when CT scanning is unavailable or too expensive); ultrasonography is advised in place of CT scanning for patients with renal failure, pregnancy, or hypersensitivity to contrast medium | To evaluate the upper urinary tract for renal-cell carcinoma, transitional cell carcinomas, urolithiasis, cystic disease, and obstructive lesions |
| Cytologic analysis of urine (first void in the morning on 3 consecutive days) | To evaluate for bladder cancer and carcinoma in situ |
| Cystoscopy | Recommended for all persons with asymptomatic microscopic hematuria who are older than 40 years and for those who are younger but have risk factors for bladder cancer |
Ahmed Z, Lee J. Hematuria and proteinuria. Med Clin North Am. 1997;81:641-652.
Cohen RA, Brown RS. Microscopic hematuria. N Engl J Med. 2003;348:2330-2338.
Feld LG, Waz WR, Perez LM, et al. Hematuria. An integrated medical and surgical approach. Pediatr Clin North Am. 1997;44:1191-1210.
Grossfeld GD, Carroll PR. Evaluation of asymptomatic microscopic hematuria. Urol Clin North Am. 1998;25:661-676.
Grossfeld GD, Wolf JS, Litwin MS, et al. Asymptomatic microscopic hematuria in adults: summary of the AUA best practice policy recommendations. Am Fam Physician. 2001;63:1145-1154.
Harper M, Arya M, Hamid R, et al. Haematuria: a streamlined approach to management. Hosp Med. 2001;62:696-698.
Mazhari R, Kimmel PL. Hematuria: an algorithmic approach to finding the cause. Cleve Clin J Med. 2002;69:870-876.
McDonald MM, Swagerty D. Assessment of microscopic hematuria in adults. Am Fam Physician. 2006;73:1748-1754.
Sokolosky MC. Hematuria. Emerg Med Clin North Am. 2001;19:621-632.
Thaller TR, Wang LP. Evaluation of asymptomatic microscopic hematuria in adults. Am Fam Physician. 1999;60:1143-1154.
Yun EJ, Meng MV, Carroll PR. Evaluation of the patient with hematuria. Med Clin North Am. 2004;88:329-343.