Chapter 6. Methods of treatment
When asked to describe the treatment of any condition, it is a good principle and a safe answer to reply that treatment may be conservative or operative. This is particularly true in orthopaedic surgery, where there are more things to offer the patient than operation. Before selecting the right treatment for the individual patient, the physical requirements of work, home circumstances and motivation, as well as the patient’s likely cooperation with treatment and rehabilitation, all have to be considered.
It must also be remembered that many conditions get better on their own and there is a great temptation for doctors to ‘ascribe to their own skill the kindly work of time’ (John of Salisbury 1180).
Physical therapy
Physiotherapy
An injured limb can be made to work again by a programme of graded exercises to increase the range of joint movement and muscle power using weights, springs and other devices in the ward or gymnasium. Rehabilitation and the supervision of day-to-day progress are essential parts of orthopaedic treatment, but only part of the physiotherapist’s role; a good physiotherapist will also build up the patient’s morale to achieve goals previously thought impossible.
Muscles can be made to contract by applying an intermittent current (faradic stimulation or ‘faradism’) if the patient is unable to contract the muscle voluntarily. Faradism will not work if muscle is denervated, although interrupted direct current and other types of electrotherapy are effective.
Physiotherapists also manipulate the spine and other joints when necessary.
Remedial gymnastics, which once required a separate qualification from physiotherapy, takes the physical rehabilitation of the patient further than routine physiotherapy and is helpful to the young patient with physical or sporting ambitions.
Occupational therapy
The popular concept of occupational therapy is centred on handicrafts such as raffia and wickerwork, but this has little in common with modern occupational therapy, which concentrates on rehabilitating the patient through tasks relevant to work and everyday activities.
Occupational therapy departments include a small kitchen, a bath and a lavatory so that problems can be overcome before the patient leaves hospital, rather than after discharge when there is no help available. The department may also include a small printing press, so that patients can regain fine finger movement while they set type, and a treadle-operated woodworking machine to improve the coordination and strength of the legs, as well as the manual skills of carpentry. Apart from encouraging physical coordination, to produce something useful is tangible evidence of recovery and excellent for morale.
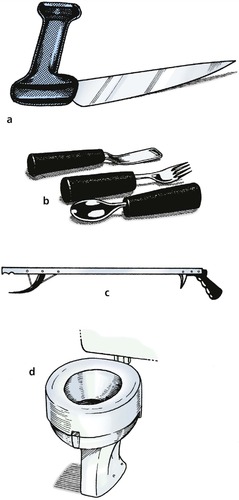
Occupational therapists also provide special cutlery for patients with hand deformities, ‘pickups’ for those who cannot bend and simple gadgets to help with dressing and other activities of daily living (Fig. 6.1).
 |
| Fig. 6.1
(a) Knife for patients with rheumatoid arthritis of the hand. (b) Thick handled cutlery for patients with poor grip. (c) ‘Pick-up’. (d) ‘Doughnut’ to increase the height of the lavatory seat for patients with poor hip movement.
|
Chiropractors and osteopaths
Chiropractors and osteopaths practise manipulation with great skill but do very little else, and generally work outside the hospital system. ‘Manipulative medicine’ is only one component of physiotherapy and is best conducted where there is access to other forms of treatment.
Aids and appliances
Walking aids
Frames
Frames provide a firm base to lean on and are particularly helpful for the elderly, but they are cumbersome, and most patients want to progress rapidly from the frame to crutches. Wheeled frames (‘Rollators’) are useful in hospital but only work on smooth floors (Fig. 6.2).
 |
| Fig. 6.2
(a) Walking frame or ‘pulpit’; (b) ‘quadrupod’ walking stick; (c) wheeled walking frame or ‘Rollator’; (d) two types of walking stick.
|
Crutches
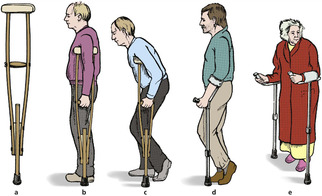
Crutches reduce the load on the lower limbs in patients with fractures or painful joints and help with balance. Three types are in common use (Fig. 6.3).
 |
| Fig. 6.3
(a) Axillary crutch; (b) axillary crutch used correctly; (c) axillary crutch used incorrectly; (d) elbow crutch; (e) gutter crutch.
|
Axillary crutches. The traditional axillary crutch has the great disadvantage that leaning on the upper end presses the radial nerve against the humerus and causes a ‘crutch palsy’. When axillary crutches are used, the elbows should be locked straight; the upper end is not for weight-bearing.
Elbow crutches. To avoid this problem, elbow crutches may be used and are preferable to axillary crutches, but have the disadvantage of being easily broken, particularly by heavy patients.
Gutter crutches. Patients with deformed hands cannot use either axillary or elbow crutches effectively and prefer gutter crutches so they can use their forearms for weight-bearing.
Walking stick
A walking stick reduces the load on an injured limb if it is pushed against the ground when the injured limb is taking weight. Stand on a bathroom scale and press a stick against the floor to see how this happens (Fig. 6.4). Used correctly, a third of the body’s weight can be taken through the stick, but only if the stick is put to the ground at the same time as the injured leg. This usually means holding the stick in the hand opposite the injured limb, but right-handed patients with injuries of the right leg find this difficult.
 |
| Fig. 6.4
Mechanism of action of a walking stick. When the stick is pushed against the floor, the patient’s weight on the limb is reduced, relieving pressure on joints.
|
Appliances
Surgical appliances include splints and braces to support limbs, prostheses to replace absent parts of the body, surgical shoes and spinal supports. Appliances are expensive, although economical by comparison with hospital admission.
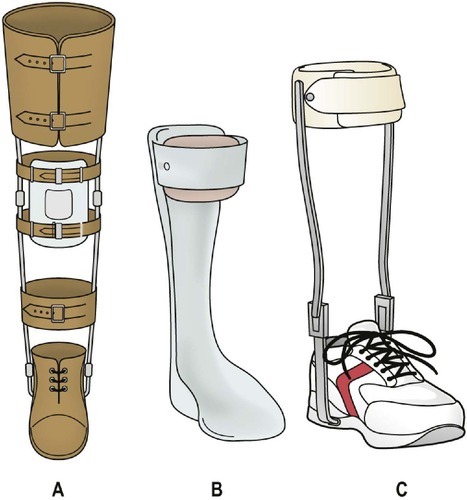
Orthoses
Orthoses, or braces, are used to support limbs (Fig. 6.5). A leg with no active dorsiflexors of the ankle is helped by a device to lift the foot, and an unstable knee is helped by a simple exoskeleton or caliper. The design and development of orthoses has advanced enormously in recent times and many heavy and unsightly devices of the past (Fig. 6.6) can be replaced with lightweight cosmetic orthoses. Close cooperation with the fitter, or orthotist, is essential if the patient is to receive the best appliance for his or her own requirements.
 |
| Fig. 6.5
Modern types of orthosis: (a) weight-relieving caliper; (b) below-knee caliper with T strap; (c) cosmetic drop foot splint.
|
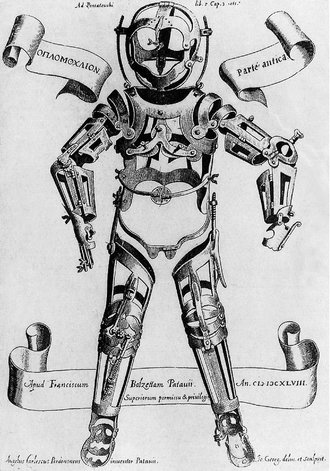 |
| Fig. 6.6
An early orthosis.
From Fabricius ab Aquapendente, Opera Chirurgica (1647), Padua. By kind permission of the Wellcome Institute Library, London.
|
For patients with paraplegia, complex braces can also be made that support the lower limbs well enough to stand, and in some cases walk, unaided (Fig. 6.7).
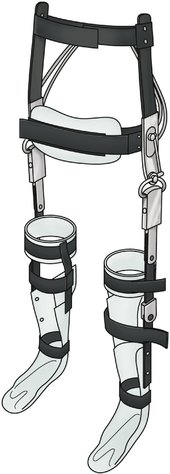 |
| Fig. 6.7
A modern orthosis with padded leather waistband and steel limb supports.
|
Weight reduction
In the past, it was considered important to relieve the weight taken by an injured or diseased limb and many devices existed to achieve this (Fig. 6.8). Protection from full load-bearing is still important for some conditions, particularly healing fractures.
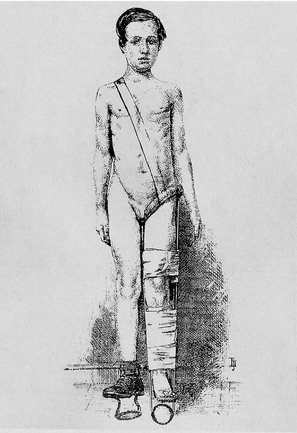 |
| Fig. 6.8
An ischial-bearing, weight-relieving, patten-ended caliper. From Thomas H O (1876) Diseases of the Hip, Knee, and Ankle Joints.
By kind permission of the Wellcome Institute Library, London.
|
Prostheses
Artificial limbs, or ‘exoprostheses’, have also improved in recent years (Fig. 6.9 and Fig. 6.10), and fitting limbs is now a specialty in its own right. This service is provided at Artificial Limb and Appliance Centres (ALACs), which are established regionally and are not available in every city.
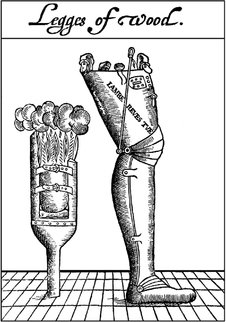 |
| Fig. 6.9
An early artificial limb.
From A Discourse of the Whole Art of Chirurgerie (1612). By kind permission of the Wellcome Institute Library, London.
|
 |
| Fig. 6.10
A modern socket (without waistband).
|
Everyday problems of maintaining artificial limbs, including repair and replacement of the limb, and practical problems such as pressure sores on the stump are best managed by these centres and it is always worth discussing difficulties with the appropriate specialist at the limb centre. The limb centre can also help by explaining the practical problems of amputation with the patient before operation, which not only helps the patient adjust to the inevitable problems but also helps the surgeon choose the right prosthesis for the individual and ensure that the stump is as good as can be achieved.
Prostheses for the upper limb present a number of different problems. A working prosthesis to replace the hand usually includes a hook of some type if it is to be of practical use; these can be unsightly. Cosmetic substitutes for the hand are seldom functional. Many patients have two prostheses, one for the working day and another for social occasions where appearance is more important than function.
The design and selection of prostheses is a subject in itself.
Spinal supports
Spinal supports were once used extensively for tuberculosis and other infections. These diseases are now uncommon and have been replaced by low back pain as the commonest indication for a lumbosacral support (Fig. 6.11). Spinal supports restrict movement of the lumbar spine and should be prescribed sparingly, especially in obese patients, who can expect little support from a lumbosacral corset that cannot get near the pelvis because of fat.
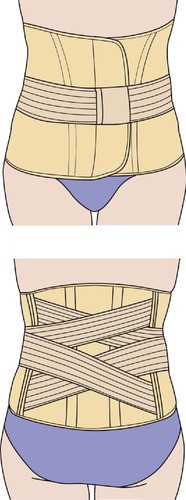 |
| Fig. 6.11
A lumbosacral support.
|
Collars
Collars to support the neck are used after trauma and for patients with acutely painful necks. Do not use the term ‘cervical collar’: a collar cannot be worn anywhere else.
Footwear
Surgical shoes or boots are prescribed for patients with foot deformities. Normal shoes are designed for normal feet and patients with abnormal feet are sometimes disabled only because they cannot find shoes that fit. Many patients with quite severe deformities can cope in soft shoes such as trainers, but specially made shoes will be needed if these are unsatisfactory. There are several types of appliance (Fig. 6.12):
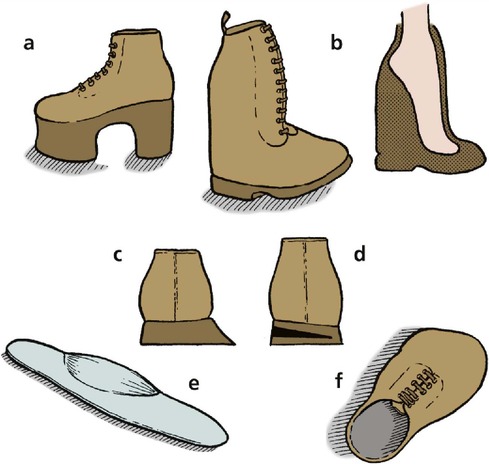 |
| Fig. 6.12
Modifications to shoes and footwear: (a) raised sole and heel; (b) boot to accommodate fixed equinus deformity; (c) float to heels; (d) wedge to heel; (e) an insole; (f) surgical shoe for foot deformity.
|
• Boots with a firm ankle support for patients with unstable ankles.
• Floats to the sole and heel for feet that tend to roll over.
• Insoles: soft insoles are helpful for patients with prominent metatarsal heads; firm moulded insoles support flat feet.
• Raises to the sole or heel to compensate for limb inequality.
These simple devices may be enough to make operation unnecessary.
Community services
Social services
Many patients have been helped more by social services or modifications to their home than by hospital treatment. Elderly patients unable to fend for themselves may need a home help to assist with housework and shopping rather than a total hip replacement, and the insuperable problem of climbing stairs can sometimes be solved by fitting a stout handrail.
These aspects of patient care cannot be ignored just because they happen outside hospital.
Warden-controlled accommodation is suitable for many elderly or infirm patients and allows them to live an independent existence in a home of their own. As the age of the population increases, small developments of single-storey accommodation designed specifically for the elderly are seen more often.
Those who cannot cope with warden-controlled accommodation need long-term residential care. Such accommodation may be provided either by local authorities or by private individuals but is under great pressure and the level of care offered is very variable.
If a patient is to be cared for by the family it is important to consider before discharge the impact such arrangements will have upon the rest of the family. Home visits from social workers, occupational therapists and the local health visitor are very helpful.
Resettlement
Patients who cannot be restored to their former work need to be resettled or retrained. A man engaged in heavy manual work and unable to lift after a back injury must find another job; a builder’s labourer with a stiff foot needs work that does not involve walking over rough ground. These problems commonly occur in patients with little academic aptitude and the selection of a new job can be difficult.
Advising a patient to give up his or her work and undergo retraining involves a great deal of thought and sympathetic assessment to determine the patient’s own particular skills (Fig. 6.13). This is best done in a resettlement or retraining centre, contacted through the local Disablement Resettlement Officer. It is not uncommon to find that a resettled patient can earn more in the new job and enjoys it better. On the other hand, ‘outdoor people’ are always unhappy at the prospect of working indoors, seated at a bench doing repetitive manual tasks, and need much encouragement.
 |
| Fig. 6.13
A skill centre for retraining injured patients.
By kind permission of Skills Training Agency, Sheffield.
|
Rehabilitation centres
Rehabilitation of the severely injured patient requires a coordinated approach and a sense of direction, which is missing when the patient is an outpatient receiving a little physiotherapy here and some occupational therapy there while they wait their turn for industrial retraining. Combining all these facilities under one roof, where patients receive more concentrated and continuous treatment than an ordinary hospital can offer, makes the task of rehabilitation a full-time occupation. This can achieve results not possible if patients are at home dwelling on their problems.
Drugs
Non-steroidal anti-inflammatory drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs are used for the conservative management of joint disease. Many such drugs are available and there is little to choose between them, but patients often do not react predictably. One patient may be completely relieved by a drug that has no effect on a patient with the same condition, and several may have to be tried before finding one that ‘suits’ the individual.
NSAIDs are the first line of treatment for most joint pains but they are not a panacea. They may not be effective and they have complications, of which the commonest is gastrointestinal irritation. Newer types (COX-2 inhibitors) may reduce this risk, but they can have their own complications, e.g. sudden cardiac death. They may also impair renal function if given for long periods. Urea and electrolytes should be measured before operation in patients who have been taking NSAIDs.
Steroids
Steroids, gold, hydroxychloroquine, sulfasalazine, methotrexate and penicillamine are all used in the management of rheumatoid arthritis. Patients requiring such treatment are better treated by rheumatologists than by orthopaedic surgeons. Great care should be taken when using methotrexate because of potential fatal blood dyscrasias.
Colchicine
Colchicine is effective in acute attacks of gout but a larger dose of a non-steroidal anti-inflammatory is also effective and causes fewer side-effects.
Antibiotics
Antibiotics are used prophylactically before implant procedures, such as joint replacement, and in the treatment of joint infections. They are also used to treat both acute and chronic infections, including osteomyelitis.
Prophylactic antibiotics
An appropriate prophylactic regimen for joint replacement is flucloxacillin 500–1000 mg, given intravenously in the anaesthetic room and continued for three doses thereafter. It is also acceptable to give 1 g 6-hourly for 24 h. It is important that the antibiotic is given before the incision is made so that there is a high blood level at the wound site.
If the patient is sensitive to penicillin, cephalosporins may be adequate but 10% of patients with penicillin sensitivity are also sensitive to cephalosporins. In those patients over the age of 60 there is high incidence of Clostridium difficile infection with the use of cephalosporins. A single intravenous dose of vancomycin is an alternative but the levels of this should be monitored.
Therapeutic antibiotics
In acute infections, the correct choice of antibiotics varies from place to place. Flucloxacillin 500 mg four times daily with ampicillin 500 mg four times daily, intravenously or orally, is a good ‘best guess’ for treatment in children before the laboratory results are known. The dose can be increased to 1 g of each drug in adults.
Anticoagulants and deep vein thrombosis
Deep vein thrombosis of some degree occurs in up to 60% of patients over the age of 40 after orthopaedic operations. The majority are ‘silent’; i.e. they are not apparent clinically.
Death from pulmonary embolus occurs in about 0.5% of patients following hip or knee replacement and is a constant anxiety. The risks following orthopaedic operations are far greater than those after other procedures, partly because of the trauma to the tissues surrounding the deep veins and partly because of difficulties in moving injured limbs in order to maintain venous flow.
Prophylactic anticoagulation
There is no agreement on prophylactic measures for anticoagulants after orthopaedic procedures. There are several reasons for this:
1. Prophylactic anticoagulants may reduce the incidence of deep vein thrombosis after operation but this is not the same as reducing the incidence of fatal pulmonary embolus.
2. Anticoagulants can cause their own complications. These include increased blood loss both before and after operation. Wound haematomas predispose to infection and delayed wound healing, and the complications of the additional blood replacement following increased blood loss may outweigh its benefits.
3. The incidence of pulmonary embolus is so low that huge numbers of patients must be studied before a statistically valid conclusion can be drawn.
Various methods of prophylaxis have been used, including elastic support stockings, faradic stimulation of the opposite limb during surgery, intermittent compression of the calf during operation, low dose warfarin and subcutaneous heparin. None has been shown to be completely effective. Low molecular weight heparin may decrease the risk of complications associated with anticoagulation.
If a deep vein thrombosis is suspected, an ultrasound of the superficial and deep veins is done initially. A venogram may be used when in doubt but this is invasive and often painful for the patient. The d-dimer blood test is also sensitive in predicting a thrombosis. Patients with large thrombi in proximal veins require full anticoagulation as there is a great risk of these clots breaking off and ending in the lung.
Established deep vein thrombosis
Anticoagulants are required in patients with established deep vein thrombosis. Full therapeutic anticoagulation is best conducted by the haematologist and should be continued after discharge for at least 6 months.
Intra-articular steroids
Intra-articular steroids should only be given when a diagnosis has been confirmed. They should not be given without careful thought and are more generally used by rheumatologists than by orthopaedic surgeons. They are most effective in patients whose disease is well controlled by drugs.
Hydrocortisone acetate 25 mg is a useful preparation for injection into painful areas, particularly at the bone–muscle or ligament–bone interface. Other preparations, e.g. triamcinolone, are used for intra-articular injection, but when injected subcutaneously they can cause fat necrosis and therefore skin atrophy. They should not be used for subcutaneous injection.
Operative management
There are more different operations in orthopaedic surgery than in any other surgical specialty.
Operations on tendons
Tendons can be (Fig. 6.14):
• Cut – tenotomy.
• Made longer – tendon lengthening.
• Moved – tendon transposition (transfer).
• Released – tenolysis.
• Fixed to bone to stabilize joints – tenodesis.
• Repaired.
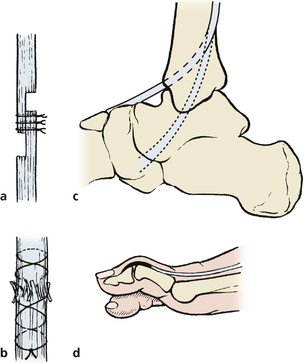 |
| Fig. 6.14
(a) Tendon lengthening; (b) repair of tendon injuries; (c) tendon transfer; (d) tenodesis.
|
Tenotomy
Dividing a tendon is a simple way to stop a muscle working and can be done either percutaneously, through a short stab incision, or by open operation.
Example: the adductor spasm of cerebral palsy can be relieved by subcutaneous adductor tenotomy.
Tendon lengthening
Tendons can be lengthened either by making a Z-shaped cut and joining the two ends together or by cutting the two halves of the tendon and allowing them to slide over each other inside the tendon sheath. Tendon lengthening relieves a fixed deformity without defunctioning the muscle altogether, as a tenotomy does.
Example: the Achilles tendon can be lengthened to reduce the equinus deformity of talipes.
Tendon transposition
A tendon can be transposed from its normal insertion to another so that the line of action of the muscle is altered, or power restored to a denervated muscle group.
Example: drop foot from common peroneal palsy can be relieved by transposing the tibialis posterior from the back of the leg to the front so that it acts as a dorsiflexor.
Tendon release (tenolysis)
Tendons which run through fibrous sheaths may become inflamed where they enter the fibrous tunnel or adherent to the sheath after trauma.
Tenodesis
Tendons can be converted to ligaments and used to stabilize unstable joints by attaching the tendon to bone immediately above the joint upon which it acts.
Example: a fixed flexion deformity of the big toe caused by unopposed action of the flexor hallucis longus can be controlled by fixing the tendon of extensor hallucis to the neck of the first metatarsal to create a ‘dorsal ligament’.
Tendon repair
Tendons can be repaired if they are torn or divided.
Example: repair of a ruptured Achilles tendon.
Operations on bones
Bones can be (Fig. 6.15):
• Cut – osteotomy.
• Joined – osteosynthesis.
• Grafted.
• Lengthened.
• Smoothed – exostectomy.
• Drained.
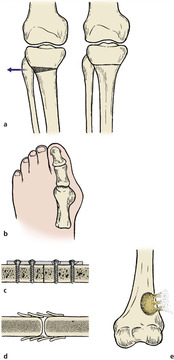 |
| Fig. 6.15
(a) Osteotomy to correct malalignment; (b) exostectomy to remove bony prominences; (c) osteosynthesis with plate and screws; (d) bone grafting; (e) decompression of bone abscess.
|
Osteotomy
An osteotomy is done either to correct deformity or to alter the stresses on a joint. An osteotomy is a surgical fracture and must unite like a fracture, but the site of the ‘fracture’ is carefully selected and the operation done so that the bone has the best chance of uniting uneventfully.
Example: tibial osteotomy to relieve the pain of osteoarthritis at the knee by correcting the varus deformity that follows wear of the medial compartment (p. 407).
Osteosynthesis
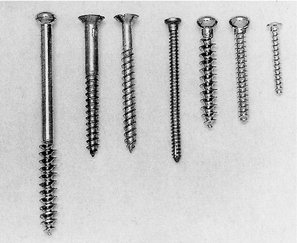
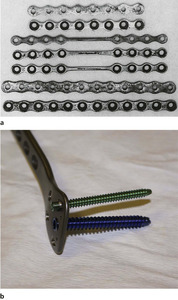
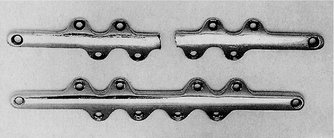
Fractured or osteotomized bones can be joined together using plates, screws or nails (Fig. 6.16 and Fig. 6.17) (p. 132). Fixation devices do not make bones unite; they only hold the bones together in the correct position while natural bony union occurs. If this does not happen, even the strongest metal plates and screws will eventually break or pull out of the bone (Fig. 6.18 and Fig. 6.19).
 |
| Fig. 6.16
Different types of screw. From left to right: ASIF cancellous lag screw; ordinary wood screw with tapered shank; chipboard screw with parallel-sided shank; self-tapping bone screw with fluted self-tapping tip; ASIF cancellous screw; ASIF cortical screw; ASIF small fragment screw (compare with Fig. 9.22).
|
 |
| Fig. 6.17
Different types of plate. (a) Very old plates. Note the pitting and corrosion and the very flimsy design. These plates were not strong enough for rigid fixation. (b) Modern locking plate with screws.
|
 |
| Fig. 6.18
An old tibial plate which has broken.
|
 |
| Fig. 6.19
(a), (b) Fractured internal fixation. The screw used to fix a fractured olecranon has itself fractured because the fragments did not unite.
|
Example: internal fixation of unstable fractures (p. 81).
Bone grafting
There are three types of grafted tissue:
1. Autograft – from elsewhere in the patient.
2. Allograft – from another human.
3. Xenograft – from another species.
Autografts. Autografts are used to encourage bone union or replace lost bone. In the past, a strip of cortical bone was taken from a site such as the tibia and screwed across a fracture site as a ‘cortical inlay graft’ to hold the ends together. Although a neat surgical exercise, the bone was being used as an internal fixation device and not as living tissue. Modern metal plates are far stronger than devitalized cortical bone and have largely replaced the cortical bone graft.
Instead, slivers or chips of cancellous bone, which contain osteoblasts and bone marrow, are taken from a site such as the iliac crest and laid around the bone, without disturbing the fracture site, to induce ossification. This technique uses bone as a biological agent and does not have an analogy in other branches of surgery.
Example: cancellous bone from the iliac crest is placed between the transverse processes and the sacrum in an intertransverse lumbosacral fusion.
Allograft bone is likely to be used more frequently as practical problems are overcome. The allograft must be stored sterile and has a limited shelf life that varies according to the method of preservation. When whole bone segments are used, a large range of sizes for both left and right sides must be kept.
Achilles tendon, patellar tendon and tibialis posterior tendon can be used to replace the anterior cruciate ligament and other ruptured ligaments.
A particular anxiety, common to all donor materials, is the possible transmission of infections, e.g. the hepatitis virus and HIV. This is a justifiable fear because patients have contracted AIDS in this way. Freeze-drying and irradiation have been claimed to reduce the risk of disease transmission but this may be at the expense of the mechanical properties of the graft.
Xenografts. Xenografts (tissue from another species) are treated to remove protein and fat, leaving only the mineralized structure intact. These grafts are essentially foreign bodies which act as a skeleton for creeping substitution rather than a true osteogenic bone graft. They have little, if any, osteogenic potential but are useful to fill spaces and hold osteotomies open.
More recently, bone morphogenic proteins (BMP) have been used with encouraging results. These stimulate the natural healing mechanism.
Other materials. Inert sponges of many materials containing calcium have been used as scaffolds for creeping substitution. Among the most recent to be offered for general use is coral, which has been machined to exact sizes, sterilized and packed ready for insertion. (‘Full fathom five thy father lies; Of his bones are coral made;’ William Shakespeare, The Tempest, Act I, Scene 2.)
Lengthening bones
Bones can be lengthened in a number of ways. A variety of techniques have been used in the past, including periosteal stripping, implantation of a foreign substance, alteration in the blood supply, sympathectomy, bioelectrical stimulation, hormone therapy and surgery. Unfortunately many of these techniques were unreliable. The use of growth hormone in particular led to tragedy as some of the hormone was obtained from human pituitary glands and was contaminated with the Creutzfeldt–Jakob disease (CJD) agent; a few of the patients treated in this way have contracted this disease.
Operations are more reliable. Simple division of the bone in a step cut fashion with subsequent distraction of the two bone ends and refixation at the desired length is possible, but only small segments can be lengthened at a time. The lengthened segment of bone is also weaker than normal and recovery may be prolonged.
In the immature skeleton a bone can be lengthened by stretching the growth plate (physeal distraction). This is achieved by the application of an external fixator across the growth plate and slowly distracting the physis. The degree of lengthening achieved is variable and the technique is limited to those patients with an open physis and potential for growth. Complications are frequent and the results are often unpredictable.
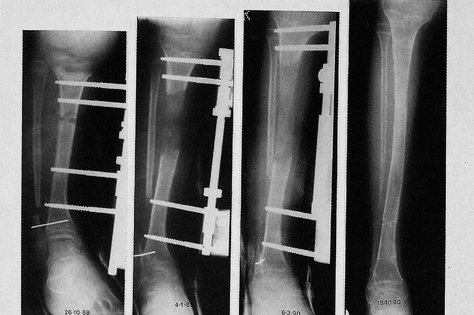
An easier and more reliable method is by callotasis. In essence this consists of cutting the bone (corticotomy) and progressive stretching of the healing callus that forms. After approximately 7–10 days following the corticotomy, the callus is stretched at a rate of approximately 1 mm per day. Distraction is achieved using either a monolateral external fixator or a ring fixator (see Fig. 9.20b). Once the desired length has been achieved the fixator is clamped and the bone is allowed to consolidate (Fig. 6.20). Patients can walk on the limb with the fixator in situ until the bone has remodelled and strengthened. There is always concern for the soft tissues, nerves and blood vessels while the distraction of the bone is in progress. Meticulous care of the pin sites is needed and patients should be prepared for a prolonged period of treatment. Patients should also be advised not to smoke while treatment is in progress because smoking interferes with ossification.
 |
| Fig. 6.20
X-rays of limb lengthening using callotasis.
|
Exostectomy
Exostoses and other lumps can be levelled, preferably making a slight depression at the site of the original bump so that the fibrous tissue which forms at the site of operation lies in the depression.
Example: levelling an exostosis on the dorsum of the foot.
Draining infection
In days gone by, bone infection was a common problem and orthopaedic surgeons spent much of their time letting pus out of abscesses and removing sequestra. These operations are, thankfully, seldom required now but it is still occasionally necessary to perform a sequestrectomy and unroof infected bone cavities (p. 312).
Example: drilling acute osteomyelitis (p. 312).
Operations on joints
Joints can be
• Stiffened – arthrodesis.
• Opened – arthrotomy.
• Refashioned – arthroplasty.
• Subjected to excision of the synovium – synovectomy.
• Mobilized – arthrolysis.
• Looked into – arthroscopy.
• Aspirated.
• Manipulated.
Arthrodesis
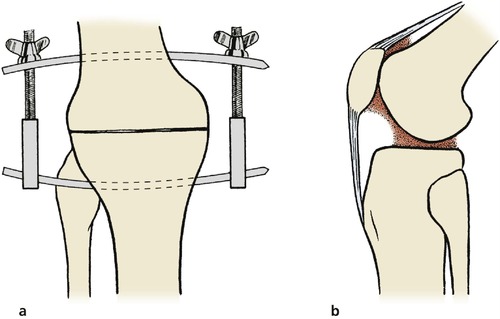
Stiffening a joint, or arthrodesis, is achieved by removing the articular surfaces of the joint and holding the bone ends together so that they unite like a fracture. The operation is indicated for irreparable damage or instability of a joint and will produce a sound and painless limb that lasts a lifetime, but the loss of movement is a serious disadvantage in large joints such as the hip and knee (Fig. 6.21, Fig. 6.22 and Fig. 6.23).
 |
| Fig. 6.21
(a) Compression arthrodesis; (b) adhesions within joints can be released by arthrolysis.
|
 |
| Fig. 6.22
Anteroposterior (a) and lateral (b) views of an arthrodesis of the wrist using ASIF internal fixation. The radiograph was taken immediately after operation and the drain is still in position.
|
 |
| Fig. 6.23
An arthrodesed hip.
|
The effect of arthrodesis is usually irreversible but can be predicted by immobilizing the joint in plaster, after which the patient may decide that a painful joint that moves a little is preferable to a painless limb that will not move at all.
Arthrodesis should not be performed if there is a chance of other joints becoming stiff. A patient can manage with one arthrodesed hip but to manage with two is extremely difficult. If both hip and knee are arthrodesed in the same limb, problems are inevitable: hold your own hip and knee stiff and try to imagine the difficulties yourself.
Example: arthrodesis of the proximal interphalangeal joint of the second toe for hammer toe (p. 440).
Arthrotomy
Any operation that opens a joint is an arthrotomy but the term is usually applied to an exploratory arthrotomy. With arthroscopy and other modern investigative techniques, exploratory arthrotomy is seldom performed alone and is largely obsolete.
Arthroplasty
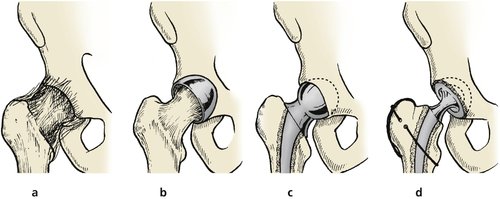
Any operation that creates or reshapes a joint is an arthroplasty. There are several types (Fig. 6.24).
 |
| Fig. 6.24
Different types of arthroplasty using the hip as an example: (a) excision arthroplasty; (b) interposition arthroplasty; (c) hemiarthroplasty; (d) total hip replacement.
|
Excision arthroplasty. Excision arthroplasty, in which the bone surfaces are removed and the space between them is allowed to fill with fibrous tissues, is the simplest and sometimes the most satisfactory arthroplasty, but leaves an unstable joint.
Example: excision arthroplasty of the hip (Girlestone’s procedure) as a salvage procedure for failed total hip replacement (p. 403).
Interposition arthroplasty. Rather than leave the two bone surfaces of an excision arthroplasty exposed, a prosthetic or organic material can be laid between the two. A stainless steel cup or mould was inserted in the hip joint before the advent of total hip replacement and a similar operation was performed at the knee.
Replacement hemiarthroplasty. If one surface of a joint is replaced with an artificial material such as metal, the operation becomes a replacement hemiarthroplasty, or simply a hemiarthroplasty.
Example: fractures of the femoral neck may be treated by replacing the femoral head with a metal prosthesis. This is satisfactory but the hard metal of the prosthesis may erode the acetabulum.
Total joint replacement. A metal prosthesis will erode bone affected by osteoarthritis or other disease. Because of this, it is usual to replace both joint surfaces in osteoarthritis and perform a total joint replacement, one of the most successful operations in orthopaedic surgery (Fig. 6.25).
 |
| Fig. 6.25
Postoperative hip X-ray.
|
Problems arise if the hip becomes infected or the components loosen, when it may be necessary to remove the artificial material and convert the total hip replacement to an excision arthroplasty.
Example: total hip replacement for osteoarthritis (p. 395).
Synovectomy
Synovium affected by rheumatoid arthritis or any other chronic inflammation may need to be removed. Without synovium, the joint develops a new lining which differs slightly from the original.
Example: synovectomy of the elbow for rheumatoid arthritis.
Arthrolysis
For a joint to function normally the bone surfaces must be free to slide over each other and the synovial cavity must be free of adhesions. If there has been bleeding or infection in the knee, fibrous adhesions will form between the two synovial surfaces and between articular cartilage and synovium, restricting movement severely. Division of the adhesions restores joint movement but they can reform (see Fig. 6.21b).
Example: mobilization of the knee following trauma.
Arthroscopy
Joints can be looked into with a telescope, an invasive procedure usually done under general anaesthetic (Fig. 6.26).
 |
| Fig. 6.26
Arthroscopy of the knee.
|
Aspiration
Joints can be aspirated; i.e. fluid can be drawn out of them: (1) to relieve the tension of a haemarthrosis; (2) to remove fluid for culture; (3) to remove synovial fluid for examination.
Aspiration requires little more skill than any ordinary injection but full sterile precautions must be taken to prevent infection. The aspiration can be done under local anaesthetic, provided that joint capsule, synovium and skin are infiltrated.
Example: diagnostic aspiration of a painless joint effusion.
Manipulation under anaesthetic
Joints can be manipulated under anaesthetic to break down adhesions or assess movement. Manipulation is helpful in restoring movement after haemarthrosis or joint replacement; however, over-enthusiastic manipulation of a joint can tear ligaments or break the bone.
Example: manipulation of a stiff joint after a fracture.
Operations on ligaments
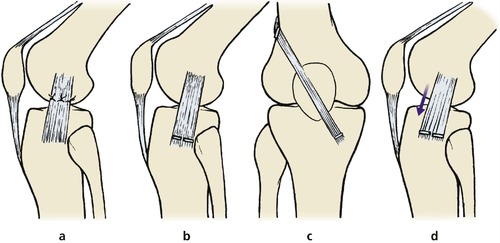
Ligaments can be (Fig. 6.27):
• Repaired when torn.
• Replaced or reconstructed.
• Shortened – plication or capsulorrhaphy.
 |
| Fig. 6.27
Operations on ligaments: (a) repair; (b) reattachment; (c) replacement with tendon or prosthesis; (d) advancement of ligament attachment.
|
Repair
Ligaments are strong and complex structures. If a ligament is even a millimetre too long, the joint that it controls may be unstable; if it is a millimetre too short, joint movement will be restricted. Even if the ligament can be accurately resutured so that it is a perfect length and in perfect position, the chances that the repaired ligament will have the same ‘stretchiness’ as the original are slight. Because of this, repairing ruptured ligaments is not generally successful.
Example: repair of the ulnar collateral ligament of the first metacarpophalangeal joint (p. 232).
Replacement or reconstruction
Because of the difficulty of repair, ligaments are sometimes replaced with a length of tendon (p. 421) or prosthetic material, but none of these procedures is entirely satisfactory.
Example: reconstruction of the anterior cruciate ligament of the knee for instability.
Plication and capsulorrhaphy
Ligaments can be tightened by advancing the attachment to bone or plicating the joint capsule to restrict movement.
Operations on nerves
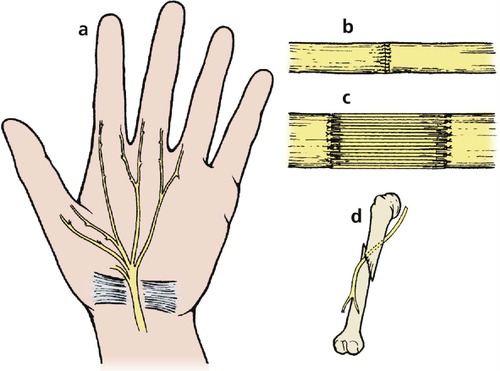
Nerves can be (Fig. 6.28):
• Decompressed.
• Repaired.
• Freed – neurolysis.
• Grafted.
 |
| Fig. 6.28
Operations on nerves: (a) decompression of compressed nerve; (b) repair by suture of the perineurium; (c) cable grafting of large defects; (d) neurolysis. Tethering of the nerve to bone or other tissues can be released by operation.
|
Decompression
The most commonly performed operation on nerves is decompression for dysfunction caused by outside pressure.
Example: decompression of the median nerve at the wrist for carpal tunnel syndrome (p. 387).
Repair
Nerves divided by injury can be repaired (p. 141).
Example: repair of the median nerve at the wrist following a laceration.
Neurolysis
Nerves can become involved in dense scar tissue, which interferes with function.
Example: mobilization of the median or ulnar nerve following a laceration of the wrist.
Grafting
Large gaps in a nerve can be replaced with a cable graft made from cutaneous nerves. These operations are unreliable but are sometimes an attractive alternative to accepting a serious disability.
Example: replacement of the upper cord of the brachial plexus with a graft made from the sural nerve.
Operations on skin
Skin can be:
• Repaired.
• Grafted.
• Changed in shape – plastic surgery.
Repair and grafting are dealt with in Chapter 9.
Plastic operations
Small areas of skin can be changed in shape to release tension, but complex plastic procedures are better done by plastic surgeons. If you find these procedures difficult to understand, try cutting out the patterns in Figure 6.29 on a separate piece of paper and move the flaps to see the effect.
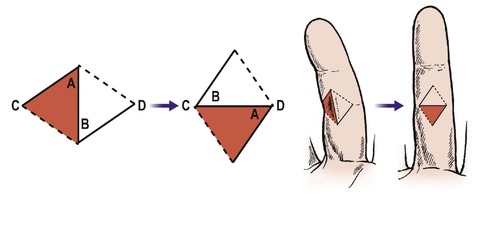 |
| Fig. 6.29
Z-plasty. A Z-plasty can change the shape of a piece of skin and the direction of the contracture.
|
Example: Z-plasty for Dupuytren’s contracture (p. 88).
Case reports
The way in which the different services are necessary for the management of orthopaedic patients is illustrated by comparing the fate of three imaginary 78-year-old women of identical size and weight who had identical fractures treated by identical operations on the same day.
Patient A (Fig. 6.30a)
This patient is a bright and active woman without relatives who fended well for herself before operation and lived alone in a bungalow (1). Her operation was uneventful and the next day, rather against her will, she sat out of bed. The following day, again under protest, she began to walk with a walking frame (3) and within 2 weeks had discarded the frame and was using elbow crutches. While in hospital, the occupational therapist made certain that the patient was able to wash and dress herself, use the lavatory, and prepare a meal while still using crutches (4). A few simple aids were necessary to help her dress but with practice she was well able to cope.
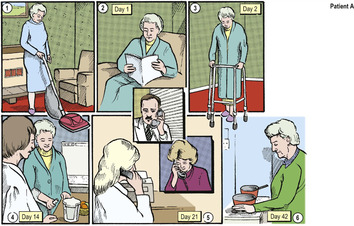 |
| Fig. 6.30a
Postoperative management – early mobilization.
|
The social worker visited the patient in hospital and arranged that after discharge a home help would assist with housework, and that ‘meals on wheels’ would call so that she would have at least one hot meal every few days even if she could not cook her own. The community nurse visited her and arranged for the health visitor to call after discharge. The patient’s family doctor was notified of the time and date of her discharge and a telephone call to the patient’s neighbours ensured that the house was heated and that fresh food was available when she arrived home (5). She was visited at home by the health visitor later on the day of discharge and by her family doctor the following day.
The patient discarded her crutches 6 weeks after operation (6) and a few weeks later was again looking after herself without assistance.
Patient B (Fig. 6.30b)
Also a bright 78-year-old woman living in a bungalow (1). The postoperative X-ray of this patient was so good that the surgeon decided she really did not need much physiotherapy or occupational therapy. The patient felt tired after operation and her kind surgeon felt so sorry for her that he let her stay in bed for a full week (2). Thereafter she spent longer and longer every day sitting out of bed (3) until about 3 weeks after operation, when she was given a pair of crutches and taken home by ambulance late one afternoon (4). Her home was unheated and the only food in the house, which was bought before her operation, had gone bad. The family doctor and health visitor did not know she was going home and none of the neighbours saw the ambulance arrive. The patient was unable to feed herself and could neither attract attention nor get herself to bed. The following day, neighbours noticed that a light was on and found the patient unconscious in an armchair (5). She was readmitted to hospital (6) with hypothermia and after intensive rehabilitation in the geriatric department made an excellent recovery, but she might not have been so fortunate.
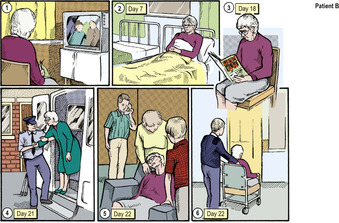 |
| Fig. 6.30b
Postoperative management – delayed mobilization.
|
Patient C (Fig. 6.30c)
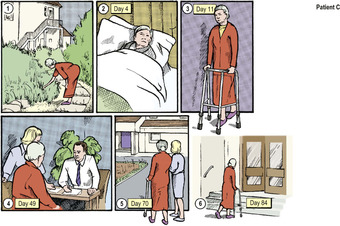 |
| Fig. 6.30c
Postoperative management.
|
Moral
The only straightforward part in the management of these three patients’ injuries was the operation. The doctor who believes that his or her responsibilities stop when the patient leaves the operating theatre should not take up orthopaedic surgery.