Chapter 171 Menopause
INTRODUCTION
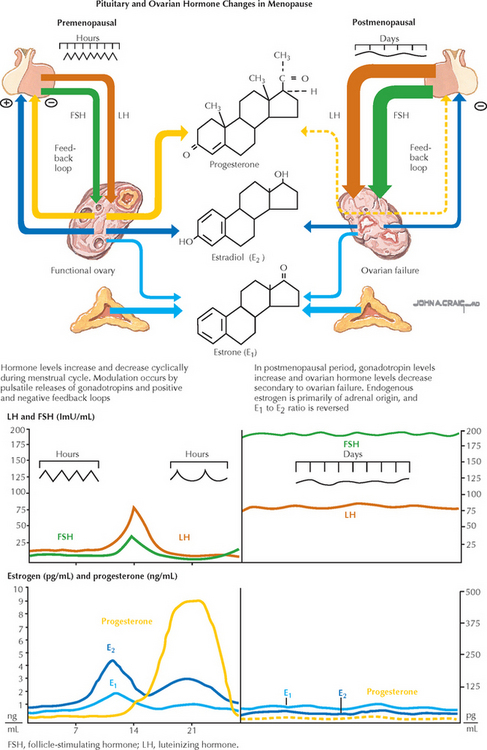
ETIOLOGY AND PATHOGENESIS
CLINICAL CHARACTERISTICS
WORKUP AND EVALUATION
MANAGEMENT AND THERAPY
Nonpharmacologic
Drug(s) of Choice
Alternative Drugs
FOLLOW-UP
Newton KM, Reed SD, LaCroix AZ, et al. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy, or placebo: a randomized trial. Ann Intern Med. 2006;145:869.
Rapp SR, Espeland MA, Shumaker SA, et alWHIMS Investigators. Effect of estrogen plus progestin on global cognitive function in postmenopausal women: The Women’s Health Initiative Memory Study: a randomized controlled trial. JAMA. 2003;289:2663.
Reddy SY, Warner H, Guttuso TJr, et al. Gabapentin, estrogen, and placebo for treating hot flushes: a randomized controlled trial. Obstet Gynecol. 2006;108:41.
Shumaker SA, Legault C, Rapp SR, et alWHIMS Investigators. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: The Women’s Health Initiative Memory Study: a randomized controlled trial. JAMA. 2003;289:2651.
Simon JA, Bouchard C, Waldbaum A, et al. Low dose of transdermal estradiol gel for treatment of symptomatic postmenopausal women: a randomized controlled trial. Obstet Gynecol. 2007;109:588.
Steiner AZ, Xiang M, Mack WJ, et al. Unopposed estradiol therapy in postmenopausal women: results from two randomized trials. Obstet Gynecol. 2007;109:581.
Anderson GL, Limacher M, Assaf AR, et alWomen’s Health Initiative Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: The Women’s Health Initiative randomized controlled trial. JAMA. 2004;291:1701.
Bath PM, Gray LJ. Association between hormone replacement therapy and subsequent stroke: a meta-analysis. BMJ. 2005;330:342. Epub 2005 Jan 7
Cauley JA, Robbins J, Chen Z, et alWomen’s Health Initiative Investigators. Effects of estrogen plus progestin on risk of fracture and bone mineral density: The Women’s Health Initiative randomized trial. JAMA. 2003;290:1729.
Cheong JM, Martin BR, Jackson GS, et al. Soy isoflavones do not affect bone resorption in postmenopausal women: a dose-response study using a novel approach with 41Ca. J Clin Endocrinol Metab. 2007;92:577. Epub 2006 Dec 5
Cushman M, Kuller LH, Prentice R, et alWomen’s Health Initiative Investigators. Estrogen plus progestin and risk of venous thrombosis. JAMA. 2004;292:1573.
Hendrix SL, Wassertheil-Smoller S, Johnson KC, et alWHI Investigators. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006;113:2425. Epub 2006 May 15
Hsia J, Langer RD, Manson JE, et alWomen’s Health Initiative Investigators. Conjugated equine estrogens and coronary heart disease: The Women’s Health Initiative. Arch Intern Med. 2006;166:357.
Magliano DJ, Rogers SL, Abramson MJ, Tonkin AM. Hormone therapy and cardiovascular disease: a systematic review and meta-analysis. BJOG. 2006;113:5.
Manson JE, Allison MA, Rossouw JE, et alWHI and WHI-CACS Investigators. Estrogen therapy and coronary-artery calcification. N Engl J Med. 2007;356:2591.
Nedrow A, Miller J, Walker M, et al. Complementary and alternative therapies for the management of menopause-related symptoms: a systematic evidence review. Arch Intern Med. 2006;166:1453.
Nelson HD. Commonly used types of postmenopausal estrogen for treatment of hot flashes: scientific review. JAMA. 2004;291:1610.
Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295:2057.
Rossouw JE, Anderson GL, Prentice RL, et alWriting Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321.
Rossouw JE, Prentice RL, Manson JE, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007;297:1465.
Wassertheil-Smoller S, Hendrix SL, Limacher M, et alWHI Investigators. Effect of estrogen plus progestin on stroke in postmenopausal women: The Women’s Health Initiative: a randomized trial. JAMA. 2003;289:2673.
American College of Obstetricians and Gynecologists. Use of botanicals for management of menopausal symptoms. ACOG Practice Bulletin 28. Washington, DC: ACOG, 2001.
American College of Obstetricians and Gynecologists. Selective estrogen receptor modulators. ACOG Practice Bulletin 39. Obstet Gynecol. 2002;100:835.
American College of Obstetricians and Gynecologists. Osteo-porosis. ACOG Practice Bulletin 50. Obstet Gynecol. 2004;103:203.
American College of Obstetricians and Gynecologists. Compounded bioidentical hormones. ACOG Committee Opinion 322. Obstet Gynecol. 2005;106:1139.
Cheung AM, Feig DS, Kapral M, et alCanadian Task Force on Preventive Health Care. Prevention of osteoporosis and osteoporotic fractures in postmenopausal women: recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2004;170:1665.
Creasman WT, Hoel D, Disaia PJ. WHI: Now that the dust has settled: a commentary. Am J Obstet Gynecol. 2003;189:621.
Grady D. Clinical practice. Management of menopausal symptoms. N Engl J Med. 2006;355:2338.
Grimes DA, Lobo RA. Perspectives on the Women’s Health Initiative trial of hormone replacement therapy. Obstet Gynecol. 2002;100:1344.
Hickey M, Davis SR, Sturdee DW. Treatment of menopausal symptoms: what shall we do now? Lancet. 2005;366:409.
National Institutes of Health. National Institutes of Health State-of-the-Science Conference statement: Management of menopause-related symptoms. Ann Intern Med. 2005;142:1003. Epub 2005 May 27
Roberts H. Managing the menopause. BMJ. 2007;334:736.
Sahdev A. Imaging the endometrium in postmenopausal bleeding. BMJ. 2007;334:635.
Santoro N. The menopausal transition. Am J Med. 2005;118:8.
Warren MP. Historical perspectives in postmenopausal hormone therapy: defining the right dose and duration. Mayo Clin Proc. 2007;82:219.