Chapter 29 Meniscus Transplantation
Diagnosis, Operative Techniques, and Clinical Outcomes
INDICATIONS
The meniscus provides important functions in the human knee, including load bearing, shock absorption, stability, and joint nutrition, that are vital for the integrity of the articular cartilage. Although many meniscus tears can be successfully repaired, including complex tears that extend into the central avascular region,52,53 not all are salvageable, especially if considerable tissue damage has occurred. Transplantation of human menisci is hypothesized to restore partial load-bearing meniscus function, decrease patient symptoms, and provide some chondroprotective effects.10,25,37,63,70 However, the procedure remains in an evolving state, as investigations of tissue-processing, secondary sterilization, and long-term function continue to evaluate its effectiveness. Clinical studies have shown that meniscus transplantation decreases tibiofemoral joint pain in the short term. However, long-term investigations report that most transplants gradually deteriorate, tear, or shrink in size, thereby losing the ability to provide function, as is described later. Accordingly, the goal is to provide short-term benefits until a more suitable meniscus transplant is clinically available. At best, the transplant provides only partial function, and therefore, strenuous sports and high-impact activities are not advised postoperatively even though many younger patients have the desire to return to unrestricted athletics. Education of the patient and family is required so that all understand and accept these current limitations of the procedure.
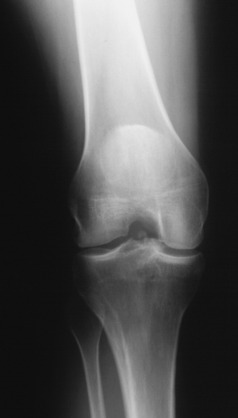
The optimal candidate is a patient under the age of 50 who has had a total meniscectomy, has pain that limits daily activities, and demonstrates early articular cartilage deterioration in the involved tibiofemoral compartment. There should be no radiographic evidence of advanced tibiofemoral joint arthritis. At least 2 mm of tibiofemoral joint space should be visible on 45° weight-bearing posteroanterior (PA) radiographs.50 Arthroscopic examination performed prior to meniscus transplantation confirms that the patient is a suitable candidate. In the most advanced cases, there should be no or only minimal bone exposed on tibiofemoral surfaces. Few treatment options are available for these individuals, especially those younger than 30 years of age, and the goal in the short-term is to decrease pain, increase knee function, allow pain-free activities of daily living, and delay the onset of tibiofemoral arthritis. Normal axial alignment and a stable joint are required. The body mass index (BMI) must be within normal range.
CONTRAINDICATIONS
Patients who have had a meniscectomy are evaluated with 45° PA weight-bearing radiographs and magnetic resonance imaging (MRI)45,46 to determine the status of the joint, articular cartilage, and subchondral bone edema. Advanced knee joint arthritis with flattening of the femoral condyle, concavity of the tibial plateau, and osteophytes that prevent anatomic seating of the meniscus transplant are contraindications. Clinical studies have shown poor results and high failure rates in knees with this amount of joint damage.19,35,46,60
Untreated lower limb malalignment is associated with failed meniscus transplantation8,12,64,65; therefore, the patient must be willing to first undergo a corrective osteotomy. Axial correction is recommended in knees in which the weight-bearing line is less than 45% (varus) or greater than 55% (valgus), representing a 2° to 3° change from normal alignment. Uncorrected knee joint instability, especially anterior cruciate ligament (ACL) deficiency, is also associated with poor outcomes after meniscus transplantation.64 Patients must undergo concurrent or staged ACL reconstruction to restore normal stability to protect the meniscus transplant.
The clinical problem is often encountered involving patients younger than 30 years of age who have undergone meniscectomy years ago, do not have articular cartilage damage, and are asymptomatic. Clinical studies show that eventual deterioration of the meniscectomized tibiofemoral compartment will most likely occur. These patients are advised that there is no optimal or predictable operative procedure to replace meniscus function and that they should decrease or refrain from participating in high-impact, strenuous activities. There are sensitive and accurate MRI cartilage techniques to determine the status of the articular cartilage in the meniscectomized compartment.44,45 When early but definite articular cartilage damage is detected, it can be logically assumed that the joint deterioration will continue over time and the opportunity exists to perform meniscus transplantation. This still represents a difficult choice for the patient in terms of undergoing surgery before the onset of major joint symptoms. In addition, the transplant may not function and further arthroscopic surgery may be required to remove the tissue. Most patients who develop early cartilage damage in the meniscectomized compartment complain of pain with strenuous athletic activities, but not with recreational or daily activities. These patients are not truly asymptomatic and desire to lessen the risk of further joint deterioration to the level at which it will affect lower intensity activities. Patient education and a conservative approach to recommendation of transplantation are important until a more dependable transplant is available.
The presence of a full-thickness femoral condylar defect with bone exposure is a relative contraindication to meniscus transplantation. Concurrent articular cartilage restorative procedures (such as osteochondral grafts or autologous chondrocyte implantation) can be successfully performed with meniscus transplantation18,38 and expand the indications to include knees with these lesions.
CLINICAL BIOMECHANICS
Chondroprotective Effects
The deleterious effects of meniscectomy on knee joint contact pressures and tibiofemoral articular cartilage have been demonstrated in multiple experimental studies.7,25,28,42,63,72,74 Bylski-Austrow and coworkers7 reported that medial meniscectomy caused a decrease in medial compartment contact pressures compared with intact joints of 70% by 4 months postoperatively and 42% by 8 months postoperatively in the goat model. The overall goal of meniscus transplantation is to protect the articular cartilage from subsequent deterioration.
Critical Points CLINICAL BIOMECHANICS
Chondroprotective Effects
Knee Joint Contact Mechanics after Meniscus Transplantation
Effect Fixation and Location of Meniscus Transplants
Szomor and associates63 conducted a study to determine the chondroprotective effects of meniscus allografts and autografts in a large animal model. Medial meniscectomy, medial meniscus autografts, and medial meniscus allografts were performed in 24 sheep. The grafts were placed into the anatomic anterior and posterior horn attachment sites and secured to the tibial plateau with three suture anchors. At 16 weeks postoperative, both the allograft and the autograft knees demonstrated a 34% to 40% reduction in the score for macroscopic damage to the articular cartilage and an approximate 50% reduction in the area of damage to the articular cartilage compared with the meniscectomized knees. However, neither graft provided complete protection, which the investigators hypothesized could have been due to nonisometric positioning and tensioning and graft fixation. Histologic analysis revealed that the allografts had fibrinoid degeneration, areas of hypocellularity, and cloning of meniscus cells.
Kelly and colleagues25 developed a meniscus allograft surgical technique that attempted to restore the anatomic anterior tibial and posterior femoral meniscal attachments in a sheep model. Fixation of the allografts was accomplished through bone tunnels. Lateral meniscus allografts were implanted into 17 animals, and lateral meniscectomies were performed in 24 animals. Gross inspection, histologic analysis, biomechanical testing, MRI, and T2 mapping of the central weight-bearing portion of the lateral tibial plateau performed 2 and 4 months postoperatively demonstrated protective effects of the allografts. Significantly decreased cartilage wear and increased cartilage stiffness were found in the allografted joints compared with the meniscectomized knees. However, at 4 months postoperative, the allografted knees had significantly worse values for these outcome measures than the intact knees. The authors noted the successful utilization of MRI with T2 mapping to detect early articular cartilage degeneration. In summary, experimental studies published to date are short term and show only partial function of the meniscus transplant in terms of contact area measurements.
Knee Joint Contact Mechanics after Meniscus Transplantation
Alhalki and coworkers2 measured the maximum pressure, mean pressure, and contact area of the medial tibial articular surface after medial meniscectomy and implantation of ipsilateral medial meniscus autografts and cryopreserved allografts in 10 cadaveric knees (mean age, 70 yr). The autografts and allografts were implanted using the same technique of bone plug fixation through anterior and posterior horn transtibial tunnels.
The allografts significantly reduced normalized maximum and mean contact pressures by 75% compared with meniscectomized knees. In addition, the maximum pressure was restricted to a small region of the contact area. The authors hypothesized that the reduction of this magnitude could reduce the rate of cartilage wear compared with that in a meniscectomized knee. However, the allografts did not restore normal contact mechanics and demonstrated greater variability in normalized maximum and mean contact pressures than the autografts. The authors concluded that the variability in contact mechanics could have been due to poor matching of the three-dimensional geometry of the allograft to the recipient knee. Dimensions for the allograft were matched from standard anteroposterior (AP) and lateral radiographs in the transverse plane. Studies by Paletta and associates41 and Haut and colleagues21 revealed that measurements made in the transverse plane only weakly predict the cross-sectional shape of the meniscus.
The effect of the size of lateral meniscus allografts (in comparison with native menisci) on tibial plateau contact mechanics was investigated by Dienst and coworkers.14 Allografts that were 17.5% larger than native menisci showed significantly higher contact pressures across the articular cartilage. Although allografts sized 10.5% smaller than native menisci had normal contact forces, increased forces in the meniscal tissue were detected that the authors hypothesized could cause early transplant failure. Allografts sized 10% larger or smaller than native menisci restored contact mechanics close to normal. The authors concluded that the surgeon should select lateral meniscus transplants (LMTs) that are slightly larger than native menisci (rather than smaller) to reduce the risk of early failure.
Paletta and associates41 investigated the effects of lateral meniscectomy, cryopreserved lateral meniscus transplantation with bone plug fixation, and lateral meniscus transplantation without fixation of the anterior and posterior horn attachments. The study involved 10 cadaver knees less than 48 years of age. The lateral meniscal transplants increased total contact area by 42% to 65% compared with meniscectomized knees at all flexion angles (0°, 30°, and 60°). However, there remained a residual 17% to 23% decrease in contact area compared with intact knees. Release of the horn attachments resulted in contact area that was identical to meniscectomized specimens. McDermott and associates28 assessed the effects of lateral meniscal transplantation with and without bone block fixation in eight cadaver knees. These investigators reported no difference between the two methods in peak contact pressures compared with intact knees. The cadaver specimens used in the study were aged 81 to 98 years, and all had moderate to severe degenerative changes. In addition, no formal size matching was performed with the allografts and recipient knees.
Effect Fixation and Location of Meniscus Transplants
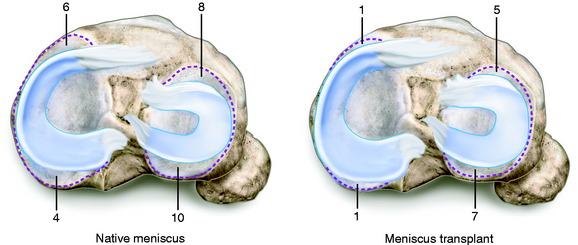
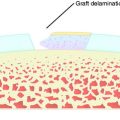
The method of fixation of meniscus transplants to the surrounding tissues is believed to be paramount in subsequent load-bearing function and chondroprotective effects. The goal is to reproduce the normal attachment sites, allowing lateral and medial transplants to remain in their anatomic location and move normally throughout knee motion.47,68 The use of a transplant with bone for fixation incorporated with either a central bone bridge or a two-tunnel technique (as described later in this chapter) is, in the authors’ opinion, required to obtain these goals. Soft tissue meniscus transplants, without bone fixation, are not recommended. Although soft tissue transplants are far easier to prepare and implant surgically, scientific data are inadequate to support that the soft tissue ends of the meniscus implant will heal and provide the circumferential tension in the meniscus that is required for function (Fig. 29-1).
The importance of securing the anterior and posterior horns of an LMT was documented by Chen and colleagues,9 who investigated a variety of surgical methods for meniscus implantation. Using an autograft cadaver model, the study revealed that a transplant that had either a bony bridge or bone plug fixation of both horns produced contact area, peak contact pressure, and average central pressure results similar to those of an intact meniscus. Procedures in which either only one horn was secured or neither horn was secured demonstrated a loss of mechanical function and subsequent expected benefit of the transplant.
Alhalki and coworkers1 compared three fixation methods of medial meniscus autografts in cadaver knees to determine which method restored tibial contact mechanics closest to normal. The experimental design tested bone plug fixation alone, bone plug fixation combined with peripheral suturing of the transplant to the native rim, and suturing of the horns through bone tunnels combined with peripheral suturing of the transplant to the native rim. The study revealed that bone plug fixation produced contact mechanics closest to normal; however, the maximum pressure was significantly greater than that in the intact knee. There was no benefit in adding peripheral sutures to the bone plug fixation model. Importantly, fixation with sutures only did not restore normal contact mechanics and was not recommended by the investigators.
Verma and associates72 measured medial compartment peak pressure, mean pressure, and contact area in eight cadaver knees to determine whether a difference existed between medial meniscus transplants (MMTs) implanted with a bone plug technique and those with a bone trough technique. The data indicated no difference between the two techniques for all three variables, which were restored to values similar to those measured in the intact knees. The authors cited clinical advantages with the trough technique for both medial and lateral meniscus transplantation.
The effect of variations in placement of the posterior horn attachment of an MMT were investigated by Sekaran and colleagues.56 Using a cadaver autograft model, the posterior horn tunnel was placed either in its anatomic position or 5 mm medial or 5 mm posterior to the anatomic location. The study showed that placing the posterior horn tunnel 5 mm medial to its anatomic position caused an increase in normalized maximum pressure, a posterior shift in the location of the centroid of the contact area, and an increase in the normalized mean pressure. Placing the posterior horn tunnel 5 mm posterior was not as detrimental; however, this location resulted in a significant shift in the centroid of contact area. The authors concluded that surgeons should place the posterior horn tunnel as close to its anatomic position as possible, with a tolerance limit of less than 5 mm medial and 5 mm posterior to this location.
CLINICAL EVALUATION
MRI is obtained using proton-density–weighted, high-resolution, fast-spin-echo sequences45,46 to determine the status of the articular cartilage and prior meniscectomized tibiofemoral compartment. Radiographs include AP, lateral at 30° of knee flexion, weight-bearing PA at 45° of knee flexion, and patellofemoral axial views. Axial lower limb alignment is measured using double-limb standing hip-knee-ankle weight-bearing radiographs16 in knees that demonstrate varus or valgus alignment.
Patients complete questionnaires and are interviewed for the assessment of symptoms, functional limitations, sports and occupational activity levels, and patient perception of the overall knee condition according to the Cincinnati Knee Rating System (CKRS).4
PREOPERATIVE PLANNING
Meniscus transplants are obtained from tissue banks accredited by the American Association of Tissue Banks (AATB) and inspected by the U.S. Food and Drug Administration (FDA), in which serologic testing meets or exceeds the standards of these organizations.67 Importantly, donor selection criteria may vary between tissue banks and the surgeon should understand the specific criteria used by the bank chosen to supply the transplant.
A variety of sterilization techniques have been described for meniscus transplants, including none (fresh-frozen), irradiated, cryopreserved, and proprietary chemical techniques. To date, no scientific data exist to select one type of graft processing method over another. Some authors8 advocate combined secondary sterilization using low-dose irradiation (1–2 Mrads) and chemical agents.
Surgeons should be aware that so-called sterilization processes may not prevent contamination and do not guarantee a sterile graft. The authors recommend that grafts be selected that have undergone some form of sterilization to decrease the risk of bacterial infection. Prophylactic antibiotics are administered intravenously before surgery, and patients are carefully monitored postoperatively for any signs of infection. The implications of different processing techniques on graft sterility and donor selection issues, allograft harvesting techniques, and disease testing are beyond the scope of this chapter and have been discussed in detail by others.5,10,67
Although there is no standard protocol at present, AP and lateral radiographs are used to obtain approximate width and length measurements for the meniscus transplant.43 A number of studies have been performed to determine the appropriate sizing method for meniscus transplants.15,21,58,61 Shaffer and coworkers58 found no difference between AP radiographs and MRI in terms of accuracy in measuring actual meniscus width and length. With accuracy defined as no more than a 2-mm difference between actual meniscus dimensions in cadaver specimens and that measured on the films, the accuracy rates were 33% for AP radiographs and 37% for MRI. Stone and associates61 suggested that recipient height, weight, and gender be considered as important matching criteria when selecting meniscus transplants. These investigators measured meniscus and tibial plateau dimensions in 111 patients using MRI and correlated the dimensions with the patients’ height, weight, BMI, and gender. Height correlated well with total tibial plateau width (R = 0.7194), and females generally had smaller meniscus dimensions than males. In addition, patients with a BMI greater than 25 had larger meniscus dimensions than patients with a lower BMI at any given height.
Critical Points PREOPERATIVE PLANNING
Donahue and colleagues15 developed an algorithm for meniscus transplant sizing based on MRI measurements. The authors recommended that tissue banks follow the algorithm, which involves a series of six steps. These include making four transverse and six cross-sectional measurements for each transplant in the bank’s inventory using a three-dimensional coordinate digitizing system, obtaining MRI of the recipient’s uninjured knee and measuring nine parameters for the medial or lateral meniscus, and performing a series of calculations to determine the best match.
The problem still exists that even though an approximate size can be determined preoperatively, in many knees the tibiofemoral joint has undergone degenerative changes that produce subtle alterations in joint geometry leading to permanent alterations in the normal surface stress distribution of the joint surface.7 A meniscus transplant does not have the ability to restore the native or normal state of the meniscectomized compartment. Future studies are required to determine the effect of subtle size and shape mismatch of the transplant on retaining articular cartilage functional properties. A chondroprotective effect of meniscus transplants has yet to be proved. This involves sophisticated questions regarding the chondrocyte function, cartilage collagen, and glycosaminoglycan homeostasis and resultant biomechanical properties.
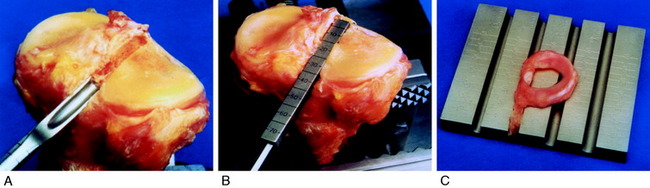
It is preferred that the tissue bank provides a digital photograph of the transplant selected for the patient before surgery. A metric ruler is placed adjacent to the transplant in the photograph to ensure that the specimen is of adequate size and width. Certain medial menisci may have a hypoplastic anterior horn that is narrow, inserting distal to the medial tibial surface (type III6), and are not acceptable for implantation. The middle third of a medial or lateral meniscus may be 8 to 10 mm in width and suitable only for small patients. The lateral meniscus may have reduced anterior-to-posterior length, less than that calculated on the sagittal radiograph, and not be suitable for implantation.
Knees with associated varus osseous malalignment require a staged corrective osteotomy prior to the meniscus transplant procedure. Knees with ligament deficiency require a staged ligament reconstruction. Some studies have advocated concurrent ACL reconstruction and meniscus transplantation.20,57,77 The normal ACL tibial attachment site and the ACL tibial graft tunnel may compromise meniscus transplant tibial fixation. This may occur when the slot technique to be described is selected in patients whose central tibial intercondylar region is not wide enough to accommodate both the meniscus transplant slot and the ACL tibial graft tunnel. Because it is not possible in these knees to use the central slot technique, a two-tunnel procedure is selected for the MMT.
INTRAOPERATIVE EVALUATION
All knee ligament subluxation tests should be performed after the induction of anesthesia in both the injured and the contralateral limbs. The amounts of increased anterior tibial translation, posterior tibial translation, lateral and medial joint opening, and external tibial rotation should be documented. A thorough arthroscopic examination should be conducted, documenting articular cartilage surface abnormalities39 and the condition of the menisci.
OPERATIVE TECHNIQUE: LMT
Critical Points INTRAOPERATIVE EVALUATION
Critical Points OPERATIVE TECHNIQUE: LATERAL MENISCUS TRANSPLANT
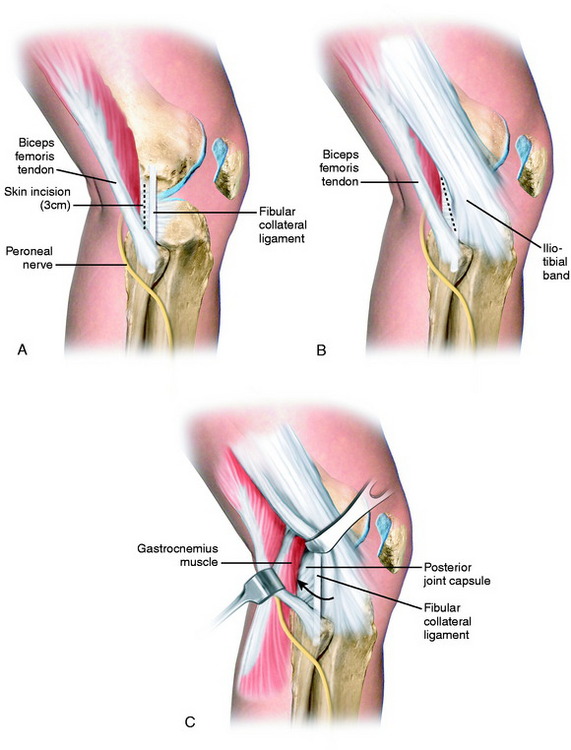
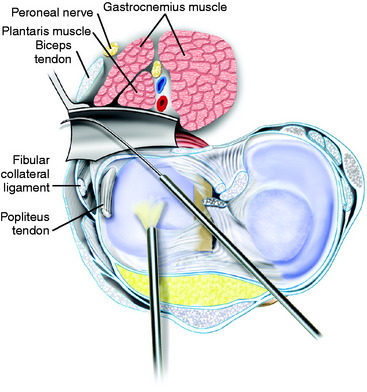
A second 3-cm posterolateral incision is made just behind the fibular collateral ligament (FCL; Fig. 29-2), similar to that described in Chapter 28, Meniscus Tears: Diagnosis, Repair Techniques, and Clinical Outcomes, for inside-out lateral meniscus repairs.29,53 The interval between the short head of the biceps muscle and the iliotibial band is identified and incised. The lateral head of the gastrocnemius is gently dissected with Metzenbaum scissors off the posterior capsule at the joint line just above the fibular head. Care is taken at this point because dissection that extends too far proximal to the joint line would enter the joint capsule. If this occurs, a capsular repair is required to maintain joint integrity during the inside-out meniscal repair procedure.
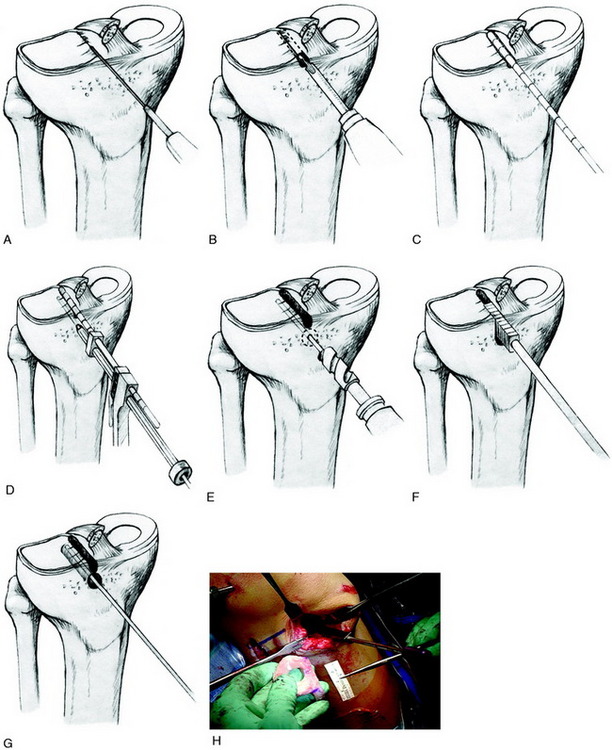
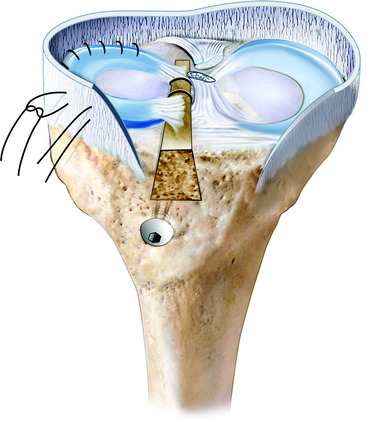
The sequence of steps to prepare the lateral tibial slot is shown in Figure 29-3. The tibial bone slot is 1 to 2 mm wider than the transplant to facilitate implantation. The anterior and posterior horns of the transplant are placed into their normal attachment locations, adjacent to the ACL. It is important to note that a prior ACL reconstruction in which the tibial tunnel was placed in a lateral position may produce a technical problem in creating the tibial slot.
A starter chisel and finishing chisels provide an alternative technique to create and fashion the tibial slot to its final depth and width (Fig. 29-4A). A tibial slot sizing guide is used to check the length and depth (see Fig. 29-4B). A sizing block (see Fig. 29-4C) confirms that the transplant bone bridge is of the correct width and depth.
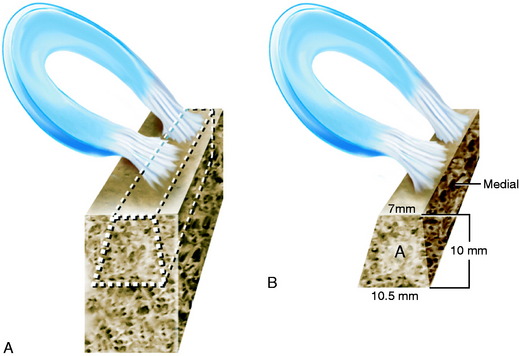
A dovetail technique may also be considered, which has the advantage of providing added stability to the fixation at the tibial bone portion of the transplant (Fig. 29-5). This procedure entails cutting a trapezoidal bone block that includes a more narrow 7-mm bone bridge. This procedure requires additional time to prepare the transplant.
Two fixation methods are available for the central bone attachment. Two 2-0 nonabsorbable sutures may be placed retrograde into the tibial slot, passed over the central bone bridge prior to transplant passage, and tied to a tibial post. The sutures hold the transplant securely in the tibial slot and, along with the peripheral sutures, provide fixation. This is the preferred technique because it is simple and effective. Another option is to place a 7- × 25-mm interference screw composed of an absorbable composite material adjacent medially to the bone bridge.17 A tap is inserted over the guidewire to create a path for the interference screw with the bone bridge held in place manually. This technique is not used if there is tibial bone osteopenia or if a prior ACL graft tunnel exists because inadequate fixation will occur.
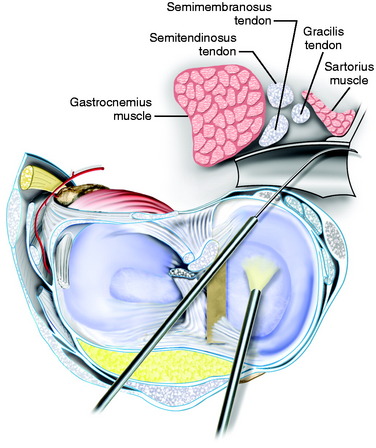
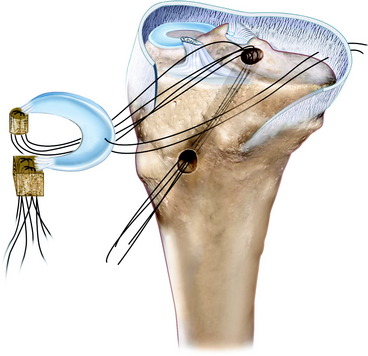
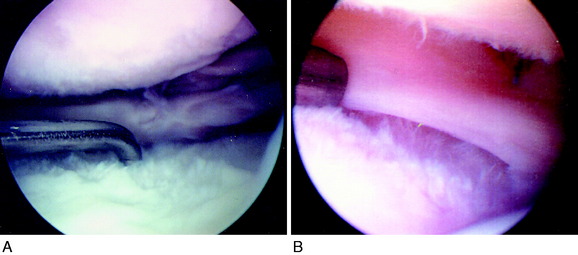
The arthrotomy is closed, and the inside-out meniscal repair completed with multiple vertical divergent sutures that are placed first superiorly to reduce the meniscus (Fig. 29-6) and then inferiorly in the outer third of the transplant. Sutures are not placed in the middle and inner thirds to avoid weakening the transplant owing to its limited healing capability in these regions (Fig. 29-7).
OPERATIVE TECHNIQUE: MMT
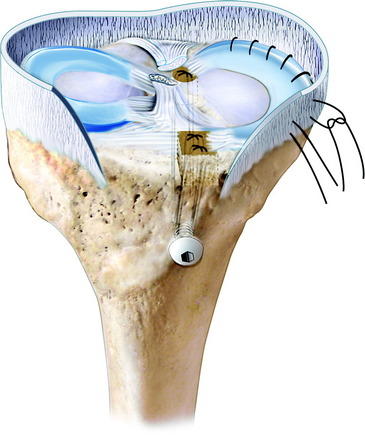
The patient is placed in a supine position on the operating room table with a tourniquet applied with a leg holder, and the table adjusted to allow 90° of knee flexion. The opposite lower extremity is placed in a thigh-high elastic stocking and is padded to maintain mild hip flexion to decrease tension on the femoral nerve. After knee examination and diagnostic arthroscopy, the meniscus bed is prepared by removing remaining meniscal tissue. It is important to preserve, whenever possible, a 3-mm rim to help contain the meniscus and prevent medial extrusion. Although there are techniques for suturing the meniscus implant without bone plugs, the authors prefer to take the added time to secure a bone-meniscus-bone implant and have identified on weight-bearing MRI studies (presented later in this chapter) that this procedure results in a meniscus implant that heals without medial extrusion. The same concept applies to lateral meniscus implants. The authors are not aware of similar clinical MRI studies after meniscus implants without bone attachments to prove that early partial meniscus extrusion is not a problem. Biomechanical studies1,2,9,41 support this concept and have shown that meniscus implants sutured, without additional bony fixation, do not restore normal joint contact pressures, although one study did not agree.28 Any loss of meniscus to its bony attachment may result in loss of function. Sekaran and colleagues56 showed that even a 5-mm malposition in the medial meniscus posterior bone plug adversely affects joint contact pressure. The meniscus bed and synovium are rasped to aid in revascularization of the transplant.
Critical Points OPERATIVE TECHNIQUE: MEDIAL MENISCUS TRANSPLANT
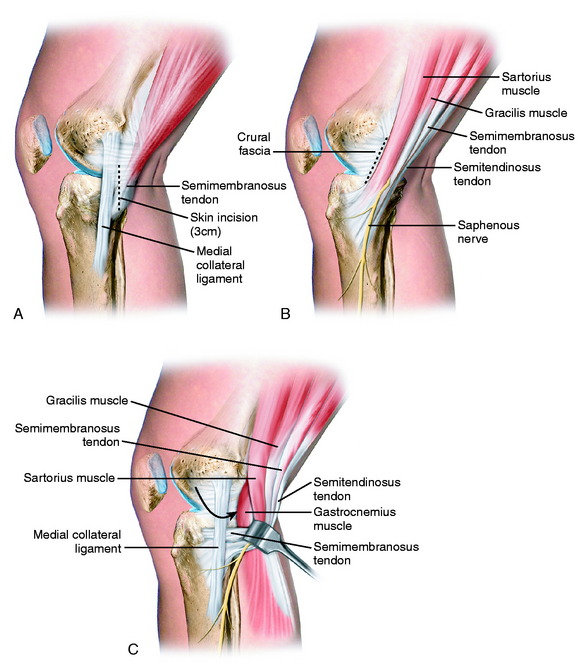
The tourniquet is inflated only for the anteromedial and posteromedial surgical approaches. A 4-cm skin anteromedial incision is made adjacent to the patellar tendon for the anterior arthrotomy. A second 3-cm vertical posteromedial incision is made, similar to that described for inside-out meniscus repairs29 (Fig. 29-8). The fascia is incised anterior to the sartorius muscle, and the pes anserine muscle groups are retracted posteriorly. Great care is taken to identify and avoid injury to the infrapatellar branches of the saphenous nerve. The interval between the semimembranosus tendon and the capsule is dissected. The tendon sheath of the semimembranosus is incised to facilitate exposure. The layer between the medial gastrocnemius tendon and the posterior capsule is separated with blunt dissection. A meniscus retractor is placed in the interval anterior to the gastrocnemius tendon and directly posterior to the meniscus bed and posterior capsule. The two approaches are performed with the tourniquet inflated to 275 mm and usually require less than 15 minutes; otherwise, the tourniquet is not used.
Medial Meniscus Central Bone Bridge Technique
Critical Points OPERATIVE TECHNIQUE: MEDIAL MENISCUS CENTRAL BONE BRIDGE TECHNIQUE
In the dovetail technique, the central bone bridge of the transplant is sized to a width of 7 mm (1 mm less than the dimension at the tibial site) and a depth of 10 mm.17 The dovetail technique requires less central bone resection and, therefore, is more protective of the ACL attachment.
The fixation of the central bone bridge is accomplished with two sutures that are passed through a tunnel in the central tibial slot or with an interference absorbable screw, as already described. The anterior horn of the meniscus is sutured with vertical sutures (2-0 Ethibond) under direct visualization (Fig. 29-9). The anterior arthrotomy is closed and the inside-out vertical divergent sutures are placed, as described, to suture the meniscus to the meniscus bed, removing any transplant undulations and restoring circumferential meniscal tension. A final arthroscopic inspection confirms proper transplant fixation and placement. The central bone bridge of the transplant provides for fixation of the anterior and posterior portions of the transplant and subsequent healing to the host tibia (Fig. 29-10).
Medial Meniscus Two-Tunnel Technique
If it is determined that the central bone bridge technique is not acceptable, the surgeon must prepare separate anterior and posterior bone attachments for the meniscus transplant that will be secured to the normal anatomic attachment sites (Fig. 29-11). The transplant is prepared with a posterior bone plug 8 mm in diameter and 12 mm in length. Although techniques have been described that use only soft tissue fixation of the posterior horn, removing the posterior bone attachment of the meniscus graft to allow easier graft passage, the authors’ opinion is that this provides less secure fixation, does not adequately restore hoop tension, and leads to a higher failure rate. The anterior bone attachment is 12 mm in width, length, and depth. Two 2-0 nonabsorbable sutures are passed retrograde through each bone attachment, with two additional locking sutures placed in the meniscus adjacent to the bone attachment for secure fixation.
Critical Points OPERATIVE TECHNIQUE: MEDIAL MENISCUS TWO-TUNNEL TECHNIQUE
Alternative techniques such as meniscus fixators are not considered because these devices lessen the ability to precisely secure and restore tension to the meniscus transplant. The anterior arthrotomy is opened, and final tensioning and fixation of the anterior horn bone attachment is performed. Additional sutures are required to secure the most anterior third of the meniscus to the capsular attachments, which is performed under direct vision (Fig. 29-12). An alternative method of fixation is to use a 3.5-mm cancellous screw with a washer for fixation of the anterior horn meniscus-bone attachment. After final inspection of the graft with knee flexion and extension and tibial rotation, the operative wounds are closed in a routine fashion.
AUTHORS’ CLINICAL STUDIES
Cryopreserved Meniscus Transplantation
The clinical outcome of 40 consecutive cryopreserved and 96 fresh-frozen irradiated MMTs and LMTs were previously described in detail.35–37,47 A 100% follow-up was obtained in these prospective studies.
Forty cryopreserved meniscus transplants were implanted into 38 patients from November 1995 to March 2000.37 Four of the meniscus transplants failed and were removed before the minimum 2-year follow-up study period; these cases were included in the overall failure rate. Thirty-five patients were followed (36 meniscus transplants; 18 lateral, 16 medial, 1 bilateral) a mean of 40 months (range, 24–69 mo) postoperatively. There were 18 males and 17 females whose mean age at surgery was 30 years (range, 14–49 yr).
Critical Points AUTHORS’ CLINICAL STUDIES: CRYOPRESERVED MENISCUS TRANSPLANTATION
ACL, anterior cruciate ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament.
At the time of the LMT, a concurrent osteochondral autograft transfer of the lateral femoral condyle was done in 13 knees for full-thickness articular cartilage defects. Knee ligament reconstructions were done before the meniscus transplant in 4 knees and at the same time as the transplant in 4 knees. In 6 knees, ACL reconstructions were done using either bone–patellar tendon–bone or semitendinosus-gracilis autografts. A PCL two-strand quadriceps tendon autograft reconstruction33 was done in 1 knee, and both the PCL and the ACL were reconstructed in another.
A total of 29 meniscus transplants (73%) were analyzed with MRI using the research protocol previously described in detail37,47 an average of 35 months (range, 12–67 mo) postoperatively. The films were reviewed and measured by independent orthopaedic surgeons blinded to patient information. The height, width, and displacement of the transplant were determined during full or partial weight-bearing conditions.
A subset of eight meniscus transplants in seven knees were studied 15 to 34 months postoperatively47 in an open configuration Signa SP MRI System (General Electric Medical Systems, Milwaukee, WI). This system is a 0.5-T superconducting magnet in which the windings are located in separate but communicating cryostats. The vertical orientation of the scanner allows the patient to stand between the cryostats with the knee at isocenter (Fig. 29-13). Single-slice sagittal and coronal images were obtained on both knees at 0°, 30°, 60°, and 90° of knee flexion.
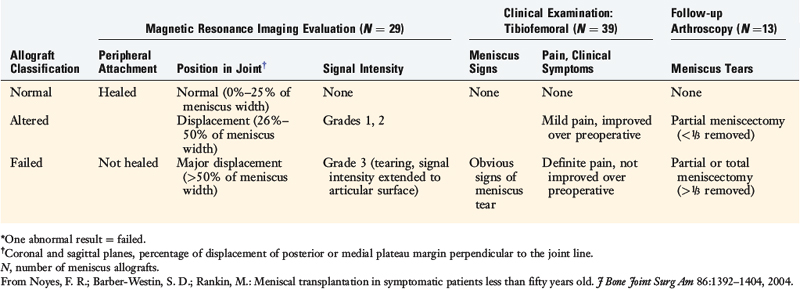
The subjective and functional results were assessed with the CKRS. A classification system of meniscus transplant characteristics was developed on the basis of MRI, clinical examination, follow-up arthroscopy (when performed), and tibiofemoral symptoms (Table 29-1). The International Knee Documentations Committee (IKDC) classification system was used to determine knee ligament graft function.
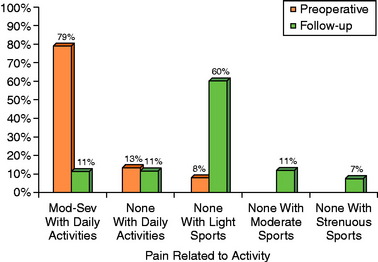
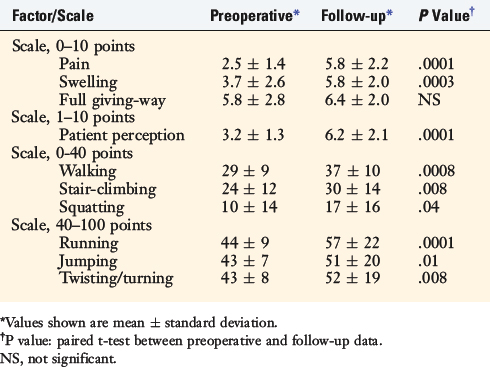
Before surgery, 27 patients (77%) had moderate to severe pain with daily activities, but at follow-up, only 2 (6%) had pain with daily activities (Fig. 29-14; P < .0001). All patients had pain in the meniscectomized tibiofemoral compartment preoperatively, but at follow-up, only 10 (29%) had some component of tibiofemoral pain.
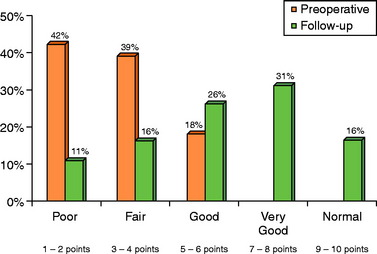
Thirty-three of 35 patients (94%) stated their knee condition had improved on self-assessment ratings (Fig. 29-15). The mean preoperative patient perception score (scale, 1–10) of 3.1 points (range, 1–6 points) improved to a mean of 6.2 points (range, 1–9 points) at follow-up (Table 29-2; P < .0001). Preoperatively, only 1 patient was able to participate in sports without problems. At follow-up, 27 patients (77%) were participating in light, low-impact sports without problems and 1 patient was participating with symptoms against advice (Table 29-3).
TABLE 29-3 Sports Activity Levels of Patients before and after Meniscal Transplantation
| Type of Sport | Preoperative (N) | Follow-up (N) |
|---|---|---|
| Jumping, hard pivoting, cutting | 0 | 1 |
| Running, twisting, turning | 0 | 4 |
| Swimming, bicycling | 7 | 24 |
| None | 31 | 9 |
| Change in sports activities | ||
| Increased level, no symptoms | 0 | 25 |
| Same level, no symptoms | 0 | 2 |
| Decreased level, no symptoms | 1 | 1 |
| Playing with symptoms | 6 | 1 |
| No sports, knee-related reasons | 31 | 8 |
| No sports, non–knee-related reasons | 0 | 1 |
Before the operation, 15 patients suffered symptoms and limitations during work activities (Table 29-4), whereas at follow-up, only 2 patients continued to have problems related to the knee condition at work.
TABLE 29-4 Occupational Levels of Patients before and after Meniscal Transplantation
| Occupational Level | Preoperative (N) | Follow-up (N) |
|---|---|---|
| Disabled | 5 | 3 |
| Very light/light | 12 | 21 |
| Moderate | 2 | 1 |
| Heavy/very heavy | 4 | 5 |
| Student/homemaker | 15 | 8 |
| Change in occupational level | ||
| Increased level, no symptoms | 0 | 5 |
| Same level, no symptoms | 2 | 15 |
| Decreased level, no symptoms | 1 | 5 |
| Working with symptoms | 15 | 2 |
| No work, knee-related reasons | 5 | 3 |
| No work, non–knee-related reasons | 15 | 8 |
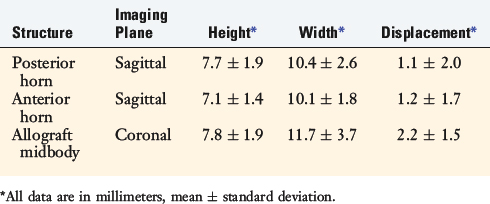
The mean displacement of the 29 meniscus transplants examined with MRI was 2.2 ± 1.5 mm (range, 0–5 mm) in the coronal plane (Table 29-5). Seventeen transplants (59%) had no displacement, 11 had minor displacement, and 1 could not be evaluated.
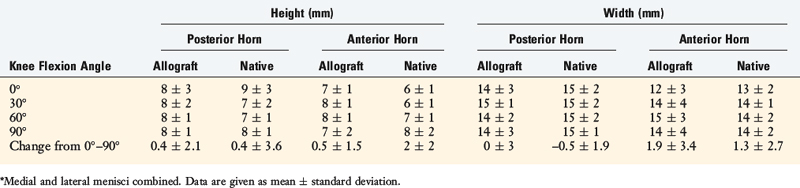
In the subgroup of 8 transplants examined with the standing full weight-bearing MRI protocol, the mean height and width of the anterior and posterior horns of the transplants were similar to those of native menisci (Table 29-6). The millimeters of coronal displacement of motion of the midbody was also similar between the transplants and the native menisci. The anterior horn of the native medial menisci moved an average of 5 mm more (total anterior-to-posterior translation, P < .05) than the transplants. The posterior horn of the native medial menisci and both horns of the native lateral menisci also tended to move more than the corresponding horns of the transplanted menisci (Fig. 29-16), although this could not be confirmed statistically, given the number of menisci studied.
TABLE 29-6 Height and Width Measurements of Eight Meniscus Allografts and Native Menisci* in the Sagittal Plane
Irradiated Meniscus Transplantation
The results of 96 consecutive irradiated meniscus transplants implanted into 82 patients were previously described.36 Twenty-eight menisci in 27 patients required early arthroscopic resection owing to lack of meniscal healing a mean of 10 months (range, 2–20 mo) postoperatively. These 28 menisci were included in the overall failure rate. In addition, 1 patient died of causes unrelated to the knee condition prior to the 2-year follow-up. This left 67 menisci (57 medial, 10 lateral) in 62 patients (63 knees) who all returned for follow-up a mean of 44 months postoperatively (range, 22–111 mo).
Critical Points AUTHORS’ CLINICAL STUDIES: IRRADIATED MENISCUS TRANSPLANTS
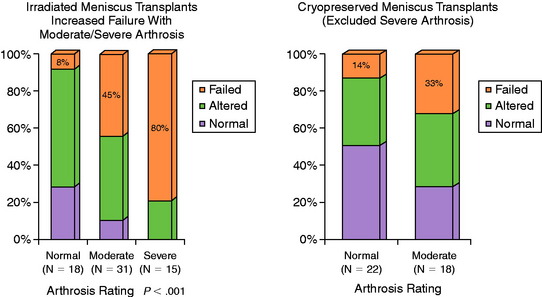
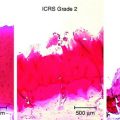
The patients were divided into three groups for analysis of the meniscus transplant. Group 1 had normal to mild articular cartilage arthritis on MRI, group 2 had moderate arthritis, and group 3 had severe arthritis. The meniscus transplant failure rate was 6% (1 of 18 knees) in knees with normal or only mild arthritis on MRI, 45% (14 of 31 knees) in knees with moderate arthritis, and 80% (12 of 15 knees) in knees with advanced arthritis (Fig. 29-17). The relationship between the meniscus transplant failure rate and increasing severity of joint arthritis was significant (P < .001).
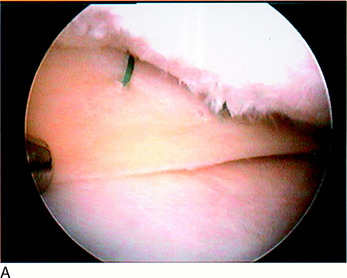
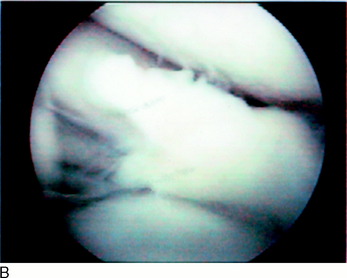
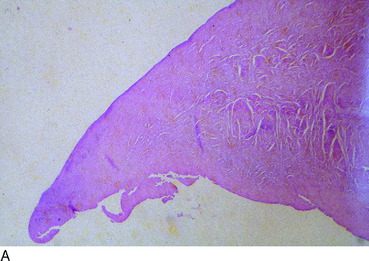
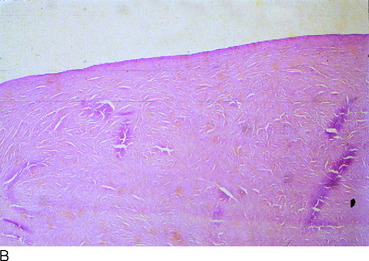
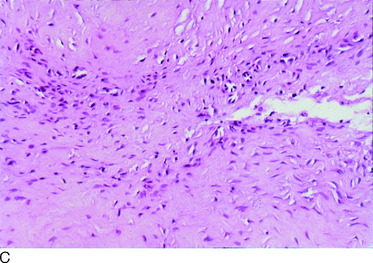
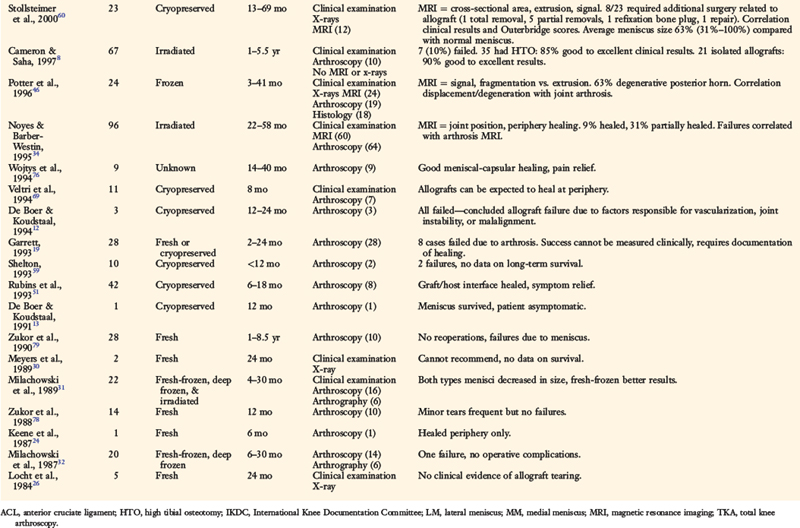
Histologic evaluations were conducted by independent examiners on the 28 meniscus allografts that failed early postoperatively. Nine specimens (5 medial, 4 lateral) that included the peripheral meniscal-capsular junction and an intact meniscal body were critically analyzed (Fig. 29-18). These allografts had been removed a mean of 11 months (range, 2–21 mo) postoperatively and the tibiofemoral and inner-outer orientations were easily identifiable. There was no evidence of a cellular reaction suggestive of a rejection phenomenon in any of the tissues examined. The specimens consistently demonstrated minimal, if any, cellular repopulation of the femoral and tibial surfaces or central core of the meniscus (Fig. 29-19A and B). The predominant cell type was a fibrocyte (see Fig. 29-19C). Remodeling with abnormal collagen orientation was found in 6 specimens. The remodeling phenomenon resulted in a loss of the normal surface radial collagen architecture and a loss of the normal circumferential fibers within the meniscal substance (see Fig. 29-19D).
RESULTS FROM OTHER CLINICAL STUDIES
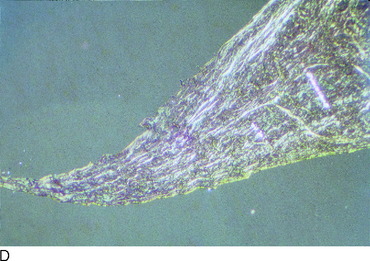
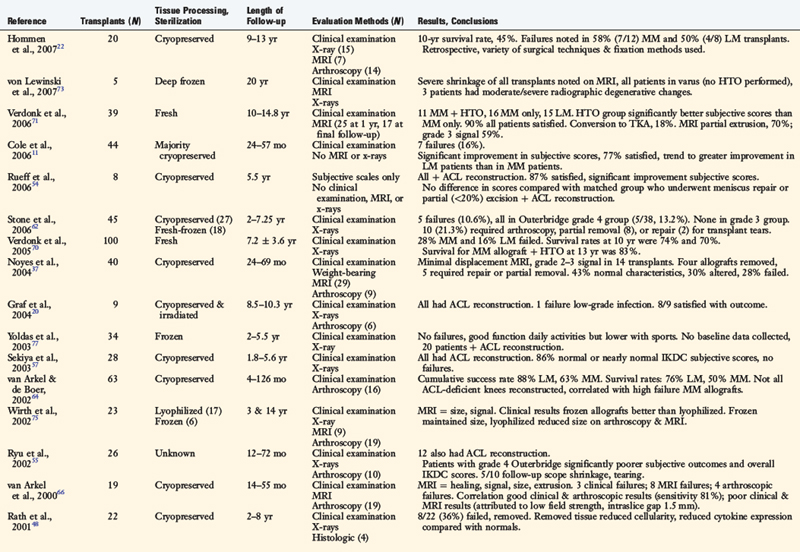
Since 1984, over 30 clinical investigations have reported results of meniscus transplant surgery (Table 29-7).*Differences in tissue processing, secondary sterilization, preservation, operative technique, and rating schemes make comparisons between studies difficult, and others have performed lengthy reviews of these investigations.10,27,49
Other studies of cryopreserved meniscus transplants reveal an approximate failure rate of 30%. Stollsteimer and coworkers60 followed 23 patients who had cryopreserved meniscal transplants 13 to 69 months postoperatively. Eight patients (35%) required a second operation for meniscal symptoms 5 to 28 months postoperatively. Although good pain relief was obtained in 18 knees, MRI in 12 knees showed some shrinkage of the transplants in that the transplants were an average of 63% the size of the contralateral normal menisci. No or only minimal transplant displacement was detected, and minor signal abnormalities were present in 5 knees.
Rath and associates48 followed 22 cryopreserved meniscal transplants for 2 to 8 years postoperatively. Concomitant ACL reconstructions were done in 11 of the 18 patients. Eight menisci (36%) failed and were removed an average of 31 months postimplantation. Even so, all patients except 1 had significant improvements in Short-Form 36-item questionnaire (SF-36) scores. Histologic analysis of the torn transplants demonstrated greater than a 50% reduction in the number of meniscal fibrochondrocytes at the periphery compared with torn native menisci. Hommen and colleagues22 followed 20 cryopreserved meniscus transplants for 9 to 13 years postoperatively and reported a 10-year survival rate of only 45%. The failures were identified from low Lysholm scores (<65 points), no improvement in pain, MRI, and second-look arthroscopy data.
van Arkel and coworkers66 reported on the results of 19 cryopreserved meniscus transplants followed 14 to 55 months postoperatively with MRI, arthroscopy, and clinical examination. The authors reported 16 transplants were successful and 3 failed based on clinical findings. However, MRI criteria revealed 8 failures because 4 transplants had severe shrinkage and 4 transplants had moderate shrinkage. None of the transplants were in a normal position; 11 showed subextrusion, 6 demonstrated extrusion, and 2 had bucket-handle–like appearances. The authors did not provide details on the surgical technique, including whether attachment of the anterior and posterior horns was performed.
Two survival analysis investigations of meniscus transplantation have been published to date. van Arkel and de Boer64 conducted a survival analysis of 63 consecutive cryopreserved meniscal transplants followed 4 to 126 months postoperatively. Persistent pain or mechanical damage (detached or torn transplant) was used to determine transplant failure. The cumulative 10-year survival rates of lateral, medial, and combined transplants in the same knee were 76%, 50%, and 67%, respectively. Failure of lateral transplants occurred an average of 53 months postimplantation and failure of medial transplants occurred a mean of 25 months.
Verdonk and associates70 followed 100 fresh meniscus transplant patients a mean of 7.2 years postoperatively. Endpoints for failure were defined as moderate or severe occasional or persistent pain or poor knee function, based on the Hospital for Special Surgery (HSS) pain and functional scores. The failure rate for MMTs was 28%, occurring a mean of 6.0 ± 8.8 years postoperatively. The failure rate for LMTs was 16%, which occurred at a mean of 4.8 ± 2.8 years postoperatively. The average cumulative survival time (11.6 yr) was identical for medial and lateral transplants. The cumulative survival rates at 10 years were 74.2% for medial transplants and 69.8% for lateral transplants. MMTs done concurrently with HTO had a higher cumulative survival rate of 83.3% at 10 years.
Postoperative MRI signal intensity alterations of meniscus transplants are frequently reported.46,60,66,75 Potter and colleagues46 investigated 29 meniscal transplants with MRI and clinical examination 3 to 41 months postoperatively. Increased signal intensity was detected in the posterior horn in 15 knees and peripheral displacement at the body was noted in 11; all of these knees had moderate or severe chondral degeneration. Histologic analysis demonstrated peripheral cellular repopulation but a central core that was acellular or hypocellular with evidence of disorganized collagen fibers. Knees with mild chondral degeneration had no abnormalities noted in the meniscus transplants and demonstrated superior clinical results compared with those with severe chondral degeneration.
Verdonk and coworkers71 followed 39 fresh meniscus allografts (implanted in 38 patients) from 10 to 14.8 years postoperatively. Isolated MMTs were performed in 16 knees, MMT was performed with HTO (MMT + HTO) in 11 knees, and isolated LMTs were done in 14 knees. Seven knees (18%; 4 MMT, 2 MMT + HTO, 1 LMT) failed to improve and underwent total knee arthroplasty a mean of 6.5 years postoperatively. All subgroups had significant improvement in modified HSS scores at follow-up; the MMT + HTO had significantly higher pain scores compared with the MMT subgroup (P = .017). However, Knee Injury and Osteoarthritis Outcome Score (KOOS) data obtained in 25 patients at follow-up showed substantial disability and symptoms and poor quality of life average scores. Standing PA radiographs obtained at follow-up in 32 knees (82%) revealed no further decrease in tibiofemoral joint space in 13 knees (41%), a grade 1 IKDC decrease in 11 (34%), a grade 2 decrease in 7 (22%), and a grade 3 decrease in 1 (3%). MRI was obtained in 17 knees, which revealed partial extrusion of the allografts in 70%. Grade 3 signal intensity was noted at 1 year postoperative in 7 allografts and in 10 allografts at the final follow-up evaluation. The authors concluded that the operation had a potential chondroprotective effect owing to the absence of further joint space narrowing in 41%.
Whereas most authors exclude patients with significant tibiofemoral compartment arthritis from meniscus transplantation, one report62 described results of this operation in patients with Outerbridge40 radiographic grade 3 (fragmentation > 1.3 cm2, 9 transplants) and grade 4 (erosion to subchondral bone, 38 transplants) degeneration. Stone and associates62 followed 45 patients from 2 to 7.25 years postoperatively. Transplant failure, defined as removal of the transplant, occurred in 5 of the 38 patients with grade 4 arthritis (13.2%) and in none of the knees with grade 3 arthritis. An additional 10 transplants tore after surgery, requiring subsequent arthroscopy and either partial removal (8 transplants) or repair (2 transplants). The authors concluded that the transplants could survive in joints with severe degenerative damage. MRI was not obtained in any knee in this investigation.
CONCLUSIONS
The biology of meniscus healing and remodeling after implantation determines the final outcome regarding potential load-bearing function and chondroprotective effects. The meniscus transplant heals to the peripheral transplant-host rim junction within a short period of time, usually 4 to 6 weeks, providing initial stability of the transplant in the knee joint. Animal3 and human36 studies indicated that an incomplete and disordered remodeling process occurs. This includes minimal cellular repopulation of the central and inner portions of the transplant, disorganization of collagen tissue (which lacks the normal collagen orientation required for load-sharing), and a predominant fibrocyte cellular structure. An increase in water content and a decrease in proteoglycan concentration in meniscus transplants have been documented.23
ILLUSTRATIVE CASES
Case 1
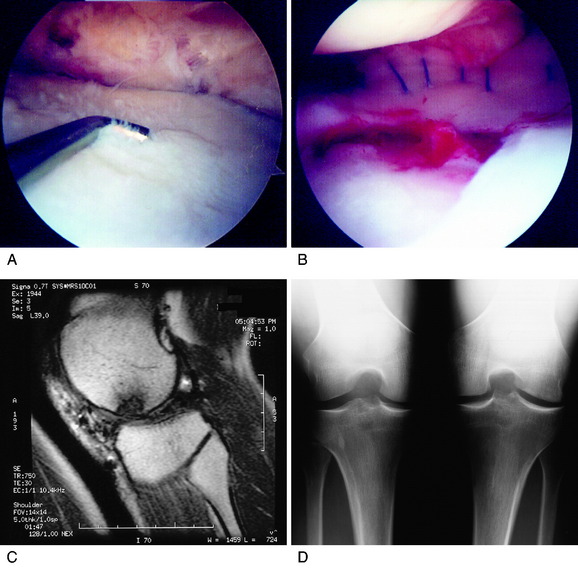
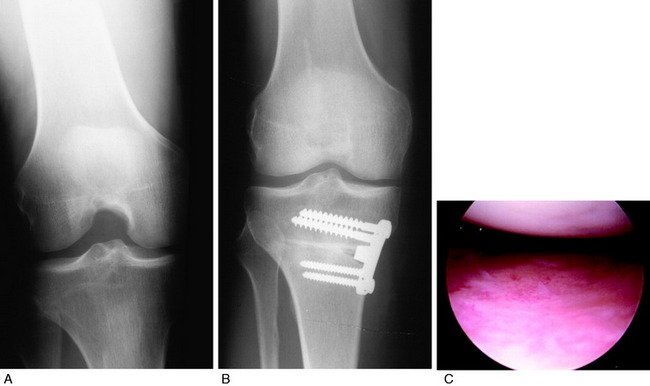
A 21-year-old man presented 2 years after an injury sustained to his left knee playing basketball that had been treated with three partial lateral meniscectomies. The patient had lateral tibiofemoral pain and swelling with all athletic activities and had not been able to return to sports. Physical examination revealed moderate lateral tibiofemoral crepitus, but no associated ligament deficiency or osseous malalignment. Arthroscopy performed before the meniscus transplantation demonstrated no remaining functional lateral meniscal tissue, diffuse grade 2A damage to the lateral femoral condyle, and a 15- x 20-mm grade 2B lesion on the tibial plateau (Fig. 29-20A). The patient was treated with a cryopreserved LMT (see Fig. 29-20B) and an osteochondral autograft transfer of the lateral femoral condyle.
At the most recent follow-up evaluation, 4 years postoperative, the patient had no lateral tibiofemoral compartment pain and had returned to low-impact activities without symptoms. He rated the overall condition of his knee as very good. MRI demonstrated grade 1 signal intensity and no displacement of the transplant (see Fig. 29-20C and D). Using the authors’ strict rating system of meniscus transplant characteristics, the implant was classified as normal.
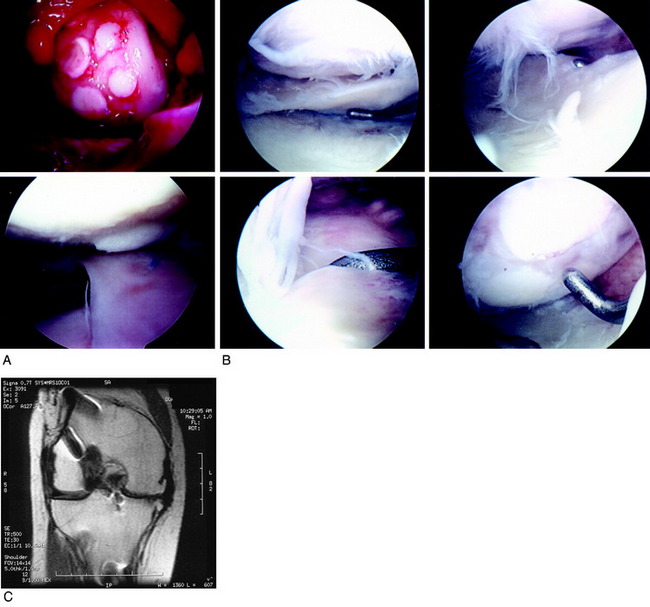
Case 2
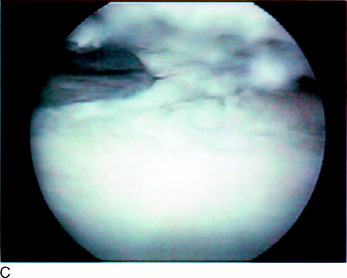
Arthroscopy performed prior to meniscus transplantation demonstrated no remaining functional lateral meniscal tissue (Fig. 29-21A), a grade 3A lesion on the lateral femoral condyle, and grade 2B damage to the tibial plateau. The patient was treated with a cryopreserved LMT (see Fig. 29-21B) and an osteochondral autograft transfer of the lateral femoral condyle.
At the most recent follow-up evaluation, 3 years postoperative, the patient had no lateral tibiofemoral compartment pain and had returned to low-impact activities without symptoms. He had changed his occupation to office work. He rated the overall condition of his knee as very good. MRI demonstrated grade 2 signal intensity, and minor displacement of the transplant (see Fig. 29-21C) was classified as altered. Standing PA radiographs showed no loss of tibiofemoral compartment joint space (see Fig. 29-21D).
Case 3
A 49-year-old woman presented 15 years after an injury to her right knee that had occurred during a fall. She had undergone an ACL allograft reconstruction, two medial meniscectomies, and a microfracture of the medial tibial plateau. She complained of pain, swelling, and partial giving-way with daily activities. Physical examination demonstrated a grade III pivot shift, moderate patellofemoral crepitus, and medial tibiofemoral compartment pain. Arthroscopy performed before meniscus transplantation demonstrated no remaining functional medial meniscal tissue, full-thickness defects of the medial femoral condyle and tibial plateau, and noteworthy fissuring and fragmentation of the patellar undersurface. The patient was treated with a cryopreserved MMT (Fig. 29-22A), an osteochondral autograft transfer of the medial femoral condyle, and a proximal patellar realignment. Seven months later, a revision ACL bone–patellar tendon–bone autograft reconstruction was performed as a staged procedure. The MMT had healed and had a relatively normal appearance arthroscopically (see Fig. 29-22B). However, MRI performed 3 years later showed major displacement of the meniscus transplant and a grade 3 signal intensity (see Fig. 29-22C). The meniscus transplant was classified as failed.
Case 4
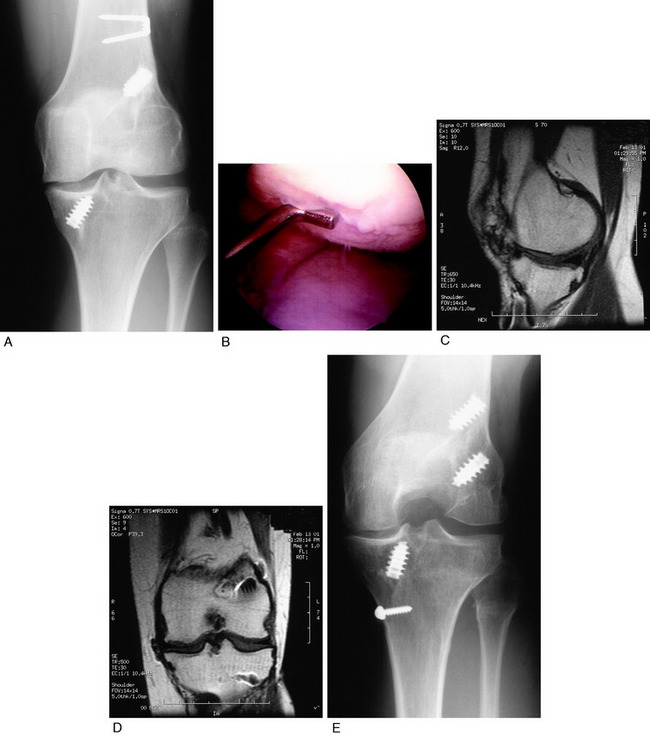
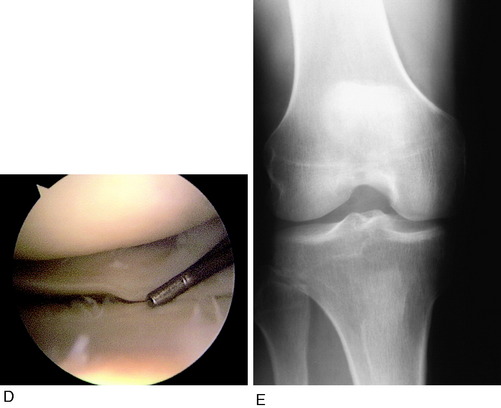
A 32-year-old woman presented with left knee medial tibiofemoral pain, locking, and instability with daily activities of 6 months’ duration. She had undergone a medial meniscectomy 17 years previously and an ACL allograft reconstruction 7 years before her initial evaluation. Physical examination demonstrated 15 mm of increased anterior-to-posterior displacement compared with the contralateral knee on KT-2000 testing, no other ligament deficiencies, a marked varus recurvatum deformity, and a hyperextension gait abnormality. Full standing radiographs showed a weight-bearing line of 19%, a mechanical axis of 5° varus, and moderate narrowing of the medial tibiofemoral compartment (Fig. 29-23A). MRI demonstrated advanced articular cartilage deterioration in the medial tibiofemoral compartment. Owing to the patient’s age, she was not considered a candidate for a unicompartmental knee replacement. The treatment recommendation was to first correct the lower limb varus malalignment and then perform meniscus transplantation and ACL revision. The patient underwent a gait-retraining program (see Chapter 34, Correction of Hyperextension Gait Abnormalities: Preoperative and Postoperative Techniques) to correct the hyperextension abnormality before proceeding to HTO.
A closing wedge osteotomy was performed, with a small 12- to 15-mm area of grade 3A articular cartilage deterioration noted in the medial tibiofemoral compartment at the time of surgery (see Fig. 29-23B). Four months later, an MMT and osteochondral autograft transfer of the medial femoral condyle were performed. An ACL patellar tendon autogenous revision reconstruction was done 3 months later, along with removal of hardware from the osteotomy.
At the most recent follow-up evaluation, 5.5 years post-transplantation, the patient had no symptoms or limitations with daily activities. She rated the overall condition of her knee as good and had no problems with her occupation in engineering. MRI showed an intact meniscus transplant (see Fig. 29-23C and D), still in position in the tibiofemoral joint. There was increased signal intensity noted, and some extrusion of the implant. Standing PA radiographs showed no progression of loss of the medial tibiofemoral joint space (see Fig. 29-23E). She had no increase in anterior tibial translation, a negative pivot shift test, and a normal range of knee motion.
Case 5
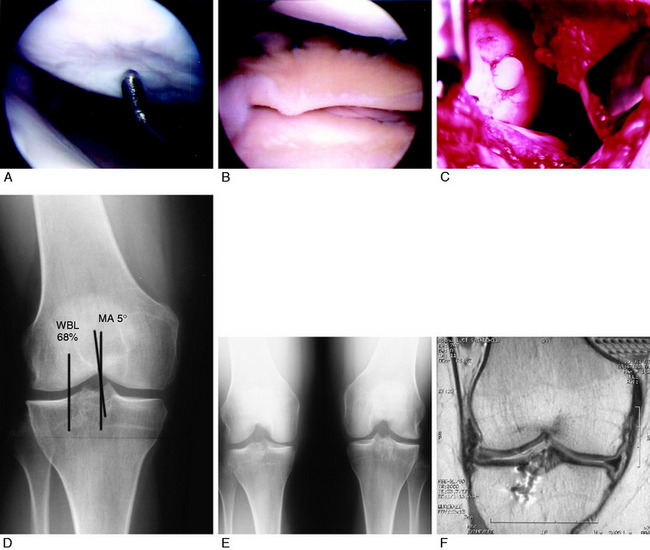
A 16-year-old female presented 3 years after a right lateral meniscectomy for a symptomatic discoid meniscus. She complained of pain and swelling with all sports activities of 6 months’ duration. Her walking tolerance was 1 hour and she was unable to kneel or squat. Physical examination revealed a normal range of knee motion, no ligament deficiencies, moderate pain and crepitation in the lateral tibiofemoral compartment, and an overall valgus alignment. Arthroscopic examination conducted elsewhere 5 months earlier revealed noteworthy articular cartilage deterioration on the lateral tibial plateau. Owing to the patient’s young age and rapid deterioration of the lateral compartment (Fig. 29-24A), she was treated with an LMT (see Fig. 29-24B). In addition, an osteochondral autograft transfer of the lateral femoral condyle was performed for a full-thickness defect that measured approximately 7 x 7 mm (see Fig. 29-24B and C).
Ten years postoperatively, the patient reported no symptoms with her occupation as an emergency room nurse. She had mild tenderness to palpation of the lateral tibiofemoral compartment, but the remainder of the physical examination was normal. Full standing radiographs demonstrated a valgus alignment (see Fig. 29-24D), and the patient was advised that a femoral osteotomy may be required in the future. Standing PA radiographs showed maintenance of the lateral tibiofemoral joint space (see Fig. 29-24E). However, MRI showed a meniscus transplant that was decreased in size, displaced, with grade 2 signal intensity (see Fig. 29-24F). The patient was advised to return for yearly examinations to continue to assess the need for a future femoral osteotomy.
Case 6
A 45-year-old man presented 2 years after a left medial meniscectomy. He had medial joint line pain, catching, and partial giving-way with daily activities that had not been resolved by the procedure. Physical examination showed a normal range of knee motion, no ligament instabilities, and mild medial tibiofemoral crepitus. The patient had significant medial joint line tenderness to palpation. Radiographs showed only minor medial joint space narrowing (Fig. 29-25A) and a varus malalignment, with the weight-bearing line at the 30% point. The patient ambulated with a varus thrust.
An opening wedge osteotomy was first performed to correct the varus osseous malalignment (see Fig. 29-25B). At the time of surgery, the articular cartilage in the medial tibiofemoral compartment had minor fissuring and no subchondral bone exposed (see Fig. 29-25C). Eight months later, an MMT was performed using a central bone bridge technique. The patient sustained a twisting injury 3 months postoperatively and presented with pain in the medial compartment. Arthroscopy was performed to assess the status of the transplant, which was determined to be normal (see Fig. 29-25D).
Four months later, the patient presented with aching pain in the medial tibiofemoral compartment and pain after walking more than 10 minutes. Radiographs revealed a healed HTO and preserved medial joint space (see Fig. 29-25E). The patient also had burning pain and tenderness to light touch along the anterior tibia. Marked atrophy was noted in the lower extremity. Three months later, the patient had not experienced relief from his symptoms, which were determined to be related to the arthritis and not to a complex regional pain syndrome. The patient subsequently underwent total joint replacement, 17 months after the meniscus transplant.
Case 7
A 43-year-old male construction worker presented 4 months after a left medial meniscectomy. The patient complained of medial pain with daily activities and had not been able to return to work. An unloader brace had been prescribed, which provided minimal relief. Physical examination demonstrated normal knee motion, mild pain and crepitation to the medial compartment, no ligament instabilities, a normal lower extremity overall alignment, and moderate patellofemoral pain on compression. At the time of the patient’s meniscectomy, noteworthy deterioration had been detected on the medial femoral condyle. Radiographs demonstrated only minimal narrowing of the medial compartment (Fig. 29-26A). The patient was treated conservatively for 5 months with nonsteroidal anti-inflammatory medications and physical therapy, but his symptoms continued.
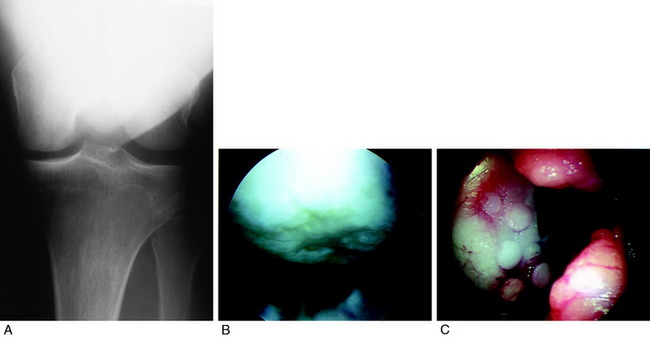
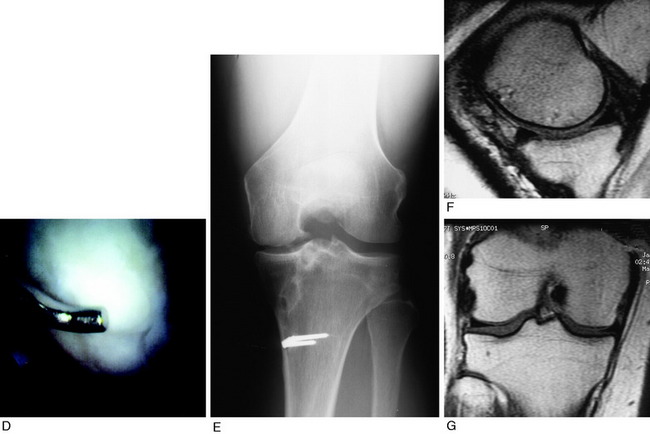
FIGURE 29-26 Case 7.
From Noyes, F. R.; Barber-Westin, S. D.; Rankin, M.: Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am 86:1392–1404, 2004.
Arthroscopy revealed a 20- x 20-mm area of subchondral bone exposure on the medial femoral condyle (see Fig. 29-26B) and extensive fissuring and fragmentation on the undersurface of the patella. An osteochondral autograft transfer was performed on the medial femoral condyle (see Fig. 29-26C). Eight months later, an MMT was performed, at which time excellent healing of the autograft bone plug in the medial femoral condyle was noted (see Fig. 29-26D).
At follow-up, 5 years postoperatively, the patient had minimal pain and had returned to his construction occupation. No problems were incurred with walking on uneven ground or stair-climbing. He had a normal range of motion, no tenderness to palpation to the medial joint line, and no effusion. Radiographs demonstrated preservation of the tibiofemoral compartment (see Fig. 29-26E). MRI revealed an intact transplant, with no displacement or extrusion and no increase in signal intensity (see Fig. 29-26F and G).
Case 8
A 38-year-old man presented 3 months after a falling injury in which he landed directly on his left knee. His history included a lateral meniscectomy at age 16, but he had not experienced knee-related symptoms until his recent injury. The patient had moderate pain and giving-way with activities. Physical examination demonstrated 10 mm of increased posterior tibial translation, 13 mm of increased lateral joint opening, 10° of increased external tibial rotation, tenderness over the medial and lateral joint lines, and moderate crepitus in the lateral tibiofemoral compartment. Radiographs showed narrowing of the lateral compartment (Fig. 29-27A). Stress radiographs revealed 6.5 mm of increased posterior tibial translation compared with the contralateral knee.
A PCL two-strand quadriceps tendon autograft reconstruction, a posterolateral reconstruction, and a lateral meniscus allograft were performed (see Fig. 29-27B). At the latest follow-up evaluation, 5 years postoperative, the patient had no symptoms and rated the overall condition of his knee as good. The KT-2000 showed 5 mm of increased anterior-to-posterior tibial displacement at 20° of knee flexion and 9 mm of increase at 70° of flexion. Physical examination showed no increase in lateral joint opening or external tibial rotation, a normal range of knee motion, no effusion, and no lateral joint line pain.
1 Alhalki M.M., Howell S.M., Hull M.L. How three methods for fixing a medial meniscus autograft affect tibial contact mechanics. Am J Sports Med. 1999;27:320-328.
2 Alhalki M.M., Hull M.L., Howell S.M. Contact mechanics of the medial tibial plateau after implantation of a medial meniscal allograft. A human cadaveric study. Am J Sports Med. 2000;28:370-376.
3 Arnoczky S.P., DiCarlo E.F., O’Brien S.J., Warren R.F. Cellular repopulation of deep-frozen meniscal autografts: an experimental study in the dog. Arthroscopy. 1992;8:428-436.
4 Barber-Westin S.D., Noyes F.R., McCloskey J.W. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati Knee Rating System in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am J Sports Med. 1999;27:402-416.
5 Barbour S.A., King W. The safe and effective use of allograft tissue–an update. Am J Sports Med. 2003;31:791-797.
6 Berlet G.C., Fowler P.J. The anterior horn of the medial meniscus. An anatomic study of its insertion. Am J Sports Med. 1998;26:540-543.
7 Bylski-Austrow D.I., Malumed J., Meade T., Grood E.S. Knee joint contact pressure decreases after chronic meniscectomy relative to the acutely meniscectomized joint: a mechanical study in the goat. J Orthop Res. 1993;11:796-804.
8 Cameron J.C., Saha S. Meniscal allograft transplantation for unicompartmental arthritis of the knee. Clin Orthop Relat Res. 1997;337:164-171.
9 Chen M.I., Branch T.P., Hutton W.C. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12:174-181.
10 Cole B.J., Carter T.R., Rodeo S.A. Allograft meniscal transplantation. Background, techniques, and results. J Bone Joint Surg Am. 2002;84:1236-1250.
11 Cole B.J., Dennis M.G., Lee S.J., et al. Prospective evaluation of allograft meniscus transplantation: a minimum 2-year follow-up. Am J Sports Med. 2006;34:919-927.
12 De Boer H.H., Koudstaal J. Failed meniscal transplantation. A report of three cases. Clin Orthop Relat Res. 1994;306:155-162.
13 De Boer H.H., Koudstaal J. The fate of meniscus cartilage after transplantation of cryopreserved nontissue-antigen–matched allograft. A case report. Clin Orthop Relat Res. 1991;266:145-151.
14 Dienst M., Greis P.E., Ellis B.J., et al. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med. 2007;35:34-42.
15 Donahue T.L., Hull M.L., Howell S.M. New algorithm for selecting meniscal allografts that best match the size and shape of the damaged meniscus. J Orthop Res. 2006;24:1535-1543.
16 Dugdale T.W., Noyes F.R., Styer D. Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248-264.
17 Farr J., Meneghini R.M., Cole B.J. Allograft interference screw fixation in meniscus transplantation. Arthroscopy. 2004;20:322-327.
18 Farr J., Rawal A., Marberry K.M. Concomitant meniscal allograft transplantation and autologous chondrocyte implantation: minimum 2-year follow-up. Am J Sports Med. 2007;35:1459-1466.
19 Garrett J.C. Meniscal transplantation: a review of 43 cases with 2- to 7-year follow-up. Sports Med Arthrosc Rev. 1993;1:164-167.
20 Graf K.W.Jr., Sekiya J.K., Wojtys E.M. Long-term results after combined medial meniscal allograft transplantation and anterior cruciate ligament reconstruction: minimum 8.5-year follow-up study. Arthroscopy. 2004;20:129-140.
21 Haut T.L., Hull M.L., Howell S.M. Use of roentgenography and magnetic resonance imaging to predict meniscal geometry determined with a three-dimensional coordinate digitizing system. J Orthop Res. 2000;18:228-237.
22 Hommen J.P., Applegate G.R., Del Pizzo W. Meniscus allograft transplantation: ten-year results of cryopreserved allografts. Arthroscopy. 2007;23:388-393.
23 Jackson D.W., Simon T.M. Biology of meniscal allograft. In: Mow V.C., Arnoczky S.P., Jackson D.W., editors. Knee Meniscus: Basic and Clinical Foundations. New York: Raven; 1992:141-152.
24 Keene G.C., Paterson R.S., Teague D.C. Advances in arthroscopic surgery. Clin Orthop Relat Res. 1987;224:64-70.
25 Kelly B.T., Potter H.G., Deng X.H., et al. Meniscal allograft transplantation in the sheep knee: evaluation of chondroprotective effects. Am J Sports Med. 2006;34:1464-1477.
26 Locht R.C., Gross A.E., Langer R. Late osteochondral allograft resurfacing for tibial plateau fractures. J Bone Joint Surgery Am. 1984;66:328-335.
27 Matava M.J. Meniscal allograft transplantation: a systematic review. Clin Orthop Relat Res. 2007;455:142-257.
28 McDermott I.D., Lie D.T., Edwards A., et al. The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc. 2008;16:553-560.
29 McLaughlin J.R., Noyes F.R. Arthroscopic meniscus repair: Recommended surgical techniques for complex meniscal tears. Tech Orthop. 1993;8:129-136.
30 Meyers M.H., Akeson W., Convery F.R. Resurfacing of the knee with fresh osteochondral allograft. J Bone Joint Surg Am. 1989;71:704-713.
31 Milachowski K.A., Weismeier K., Wirth C.J. Homologous meniscus transplantation. Int Orthop. 1989;13:1-11.
32 Milachowski K.A., Weismeier K., Wirth C.J., Kohn D. Meniscus transplantation—experimental study and first clinical report. Am J Sports Med. 1987;15:626.
33 Noyes F.R., Barber-Westin S. Posterior cruciate ligament replacement with a two-strand quadriceps tendon–patellar bone autograft and a tibial inlay technique. J Bone Joint Surg Am. 2005;87:1241-1252.
34 Noyes F.R., Barber-Westin S.D. Irradiated meniscus allografts in the human knee. A two- to five-year follow-up study. Orthop Trans. 1995;19:417.
35 Noyes F.R., Barber-Westin S.D. Meniscus transplantation: indications, techniques, clinical outcomes. Instr Course Lect. 2005;54:341-353.
36 Noyes F.R., Barber-Westin S.D., Butler D.L., Wilkins R.M. The role of allografts in repair and reconstruction of knee joint ligaments and menisci. Instr Course Lect. 1998;47:379-396.
37 Noyes F.R., Barber-Westin S.D., Rankin M. Meniscal transplantation in symptomatic patients less than fifty years old. J Bone Joint Surg Am. 2004;86:1392-1404.
38 Noyes F.R., Barber-Westin S.D., Rankin M. Meniscal transplantation in symptomatic patients less than fifty years old: surgical technique. J Bone Joint Surg Am. 2005;87(suppl 1[pt 2]):149-165.
39 Noyes F.R., Stabler C.L. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med. 1989;17:505-513.
40 Outerbridge R.E. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752-757.
41 Paletta G.A., Manning T., Snell E., et al. The effect of allograft meniscal replacement on intra-articular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med. 1997;25:692-698.
42 Pena E., Calvo B., Martinez M.A., et al. Finite element analysis of the effect of meniscal tears and meniscectomies on human knee biomechanics. Clin Biomech (Bristol, Avon). 2005;20:498-507.
43 Pollard M.E., Kang Q., Berg E.E. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684-687.
44 Potter H.G., Foo L.F. Magnetic resonance imaging of articular cartilage: trauma, degeneration, and repair. Am J Sports Med. 2006;34:661-677.
45 Potter H.G., Linklater J.M., Allen A.A., et al. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276-1284.
46 Potter H.G., Rodeo S.A., Wickiewicz T.L., Warren R.F. Imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology. 1996;198:509-514.
47 Rankin M., Noyes F.R., Barber-Westin S.D., et al. Human meniscus allografts’ in vivo size and motion characteristics: magnetic resonance imaging assessment under weightbearing conditions. Am J Sports Med. 2006;34:98-107.
48 Rath E., Richmond J.C., Yassir W., et al. Meniscal allograft transplantation. Two- to eight-year results. Am J Sports Med. 2001;29:410-414.
49 Rodeo S.A. Meniscal allografts—where do we stand? Am J Sports Med. 2001;29:246-261.
50 Rosenberg T.D., Paulos L.E., Parker R.D., et al. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70:1479-1483.
51 Rubins D., Barrett J.P., Hayter R. Arthroscopic meniscal allograft transplantation. Arthroscopy. 1993;9:356-357.
52 Rubman M.H., Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med. 1998;26:87-95.
53 Rubman M.H., Noyes F.R., Barber-Westin S.D. Technical considerations in the management of complex meniscus tears. Clin Sports Med. 1996;15:511-530.
54 Rueff D., Nyland J., Kocabey Y., et al. Self-reported patient outcomes at a minimum of 5 years after allograft anterior cruciate ligament reconstruction with or without medial meniscus transplantation: an age-, sex-, and activity level–matched comparison in patients aged approximately 50 years. Arthroscopy. 2006;22:1053-1062.
55 Ryu R.K., Dunbar V.W., Morse G.G. Meniscal allograft replacement: a 1-year to 6-year experience. Arthroscopy. 2002;18:989-994.
56 Sekaran S.V., Hull M.L., Howell S.M. Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med. 2002;30:74-82.
57 Sekiya J.K., Giffin J.R., Irrgang J.J., et al. Clinical outcomes after combined meniscal allograft transplantation and anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:896-906.
58 Shaffer B., Kennedy S., Klimkiewicz J., Yao L. Preoperative sizing of meniscal allografts in meniscus transplantation. Am J Sports Med. 2000;28:524-533.
59 Shelton W.R. Meniscal allotransplantation: an arthroscopically assisted technique. Arthroscopy. 1993;9:361.
60 Stollsteimer G.T., Shelton W.R., Dukes A., Bomboy A.L. Meniscal allograft transplantation: a 1- to 5-year follow-up of 22 patients. Arthroscopy. 2000;16:343-347.
61 Stone K.R., Freyer A., Turek T., et al. Meniscal sizing based on gender, height, and weight. Arthroscopy. 2007;23:503-508.
62 Stone K.R., Walgenbach A.W., Turek T.J., et al. Meniscus allograft survival in patients with moderate to severe unicompartmental arthritis: a 2- to 7-year follow-up. Arthroscopy. 2006;22:469-478.
63 Szomor Z.L., Martin T.E., Bonar F., Murrell G.A. The protective effects of meniscal transplantation on cartilage. An experimental study in sheep. J Bone Joint Surg Am. 2000;82:80-88.
64 van Arkel E.R., de Boer H.H. Survival analysis of human meniscal transplantations. J Bone Joint Surg Br. 2002;84:227-231.
65 van Arkel E.R.A., De Boer H.H. Human meniscal transplantation. Preliminary results at 2- to 5-year follow-up. J Bone Joint Surg Br. 1995;77:589-595.
66 van Arkel E.R.A., Goei R., de Ploeg I., de Boer H.H. Meniscal allografts: evaluation with magnetic resonance imaging and correlation with arthroscopy. Arthroscopy. 2000;16:517-521.
67 Vangsness C.T.Jr., Garcia I.A., Mills C.R., et al. Allograft transplantation in the knee: tissue regulation, procurement, processing, and sterilization. Am J Sports Med. 2003;31:474-481.
68 Vedi V., Williams A., Tennant S.J., et al. Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81:37-41.
69 Veltri D.M., Warren R.F., Wickiewicz T.L., O’Brien S.J. Current status of allograft meniscal transplantation. Clin Orthop Relat Res. 1994;303:44-55.
70 Verdonk P.C., Demurie A., Almqvist K.F., et al. Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87:715-724.
71 Verdonk P.C., Verstraete K.L., Almqvist K.F., et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14:694-706.
72 Verma N.N., Kolb E., Cole B.J., et al. The effects of medial meniscal transplantation techniques on intra-articular contact pressures. J Knee Surg. 2008;21:20-26.
73 von Lewinski G., Milachowski K.A., Weismeier K., et al. Twenty-year results of combined meniscal allograft transplantation, anterior cruciate ligament reconstruction and advancement of the medial collateral ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15:1072-1082.
74 Wilson W., van Rietbergen B., van Donkelaar C.C., Huiskes R. Pathways of load-induced cartilage damage causing cartilage degeneration in the knee after meniscectomy. J Biomech. 2003;36:845-851.
75 Wirth C.J., Peters G., Milachowski K.A., et al. Long-term results of meniscal allograft transplantation. Am J Sports Med. 2002;30:174-181.
76 Wojtys E.M., Carpenter J.E. Meniscal replacement—early experience. Arthroscopy. 1994;10:337.
77 Yoldas E.A., Sekiya J.K., Irrgang J.J., et al. Arthroscopically assisted meniscal allograft transplantation with and without combined anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2003;11:173-182.
78 Zukor D., Brooks P., Gross A., Cameron J. Meniscal allografts—experimental and clinical study. Orthop Rev. 1988;17:522.
79 Zukor D.J., Cameron J.C., Brooks P.J., et al. The fate of human meniscal allografts. In: Ewing J.W., editor. Articular Cartilage and Knee Joint Function: Basic Science and Arthroscopy. New York: Raven; 1990:147-152.