Chapter 28 Meniscus Tears
Diagnosis, Repair Techniques, and Clinical Outcomes
INDICATIONS
The importance of the menisci in the human knee is well understood and documented. The menisci occupy 60% of the contact area between the tibial and the femoral cartilage surfaces and transmit greater than 50% of joint compression forces. After meniscectomy, the tibiofemoral contact area decreases by approximately 50% and the contact forces increase two- to threefold.2,45,66,71,83,139 Meniscectomy frequently leads to irreparable joint damage, including articular cartilage degeneration, flattening of articular surfaces, and subchondral bone sclerosis. Poor long-term clinical results have been reported by many investigators after partial and total meniscectomy.* For instance, Scheller and coworkers122 followed 75 knees that underwent partial lateral meniscectomy 5 to 15 years postoperatively and noted that 78% had Fairbank’s signs of radiographic deterioration. Rockborn and Messner114 noted a 50% rate of radiographic osteoarthritis in 30 patients who underwent meniscectomy a mean of 13 years postoperatively. Roos and associates119 followed 82 knees that underwent medial meniscectomy and 25 knees that underwent lateral meniscectomy a mean of 21 years postoperatively and reported that nearly one half had advanced radiographic osteoarthritis compared with a control group. These authors reported that the relative risk of developing osteoarthritis was 3.6 after partial meniscectomy and 7.1 after total meniscectomy. Problems do exist in many meniscectomy natural history studies such as including both partial and total meniscectomy in the same cohort; not assessing the effects of patient body weight, activity level, and overall lower limb alignment on the functional result; failure to include weight-bearing posteroanterior (PA) radiographs in the assessment; and lack of a carefully defined control group for comparison. Still, preservation of meniscal tissue and function remains paramount for long-term joint function.
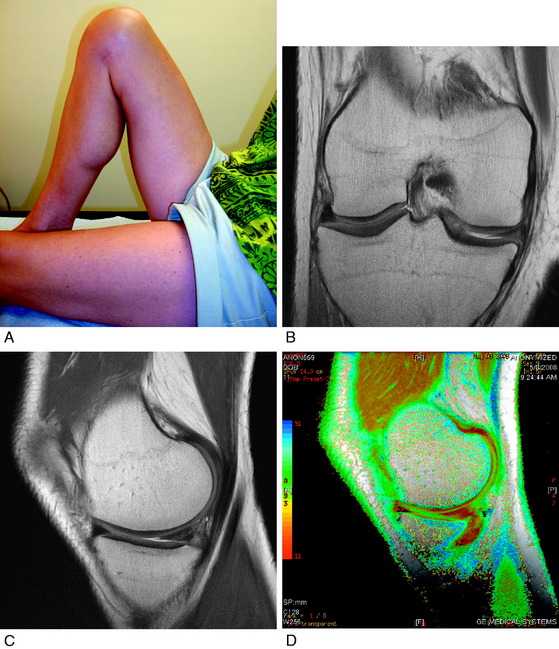
Candidates for meniscal repair are active patients younger than 60 years of age. Trauma is one of the most common etiologies of meniscus tears. For example, meniscus tears occur in 40% to 60% of patients with anterior cruciate ligament (ACL) ruptures.76,98 The majority of these tears extend into the middle third avascular region and are amendable to a meticulous inside-out suture repair. Magnetic resonance imaging (MRI) provides important information regarding the type of meniscus tear and potential for repair to preserve function.44 In knees in which repair is deemed possible, it is important to restrict strenuous activities and athletics until surgery to avoid further damage to the joint and meniscus.
Complications and deteriorating results have been reported by others after the use of all-inside meniscus fixation devices72,74,78,87,125,136 which have reduced failure, stiffness, and displacement properties compared with vertical sutures.25,110 The lack of prospective, randomized level I clinical studies precludes definitive recommendations for the various devices currently available.42,78 Therefore, this chapter focuses on suture repair techniques for various types of meniscus tears.
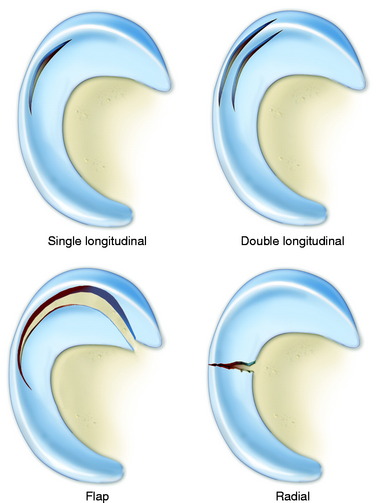
Meniscus tears are classified according to location, type of tear, and integrity and damage to meniscal tissue and the meniscus attachment sites.123 This classification, along with meticulous arthroscopic inspection of the tear site, allows the surgeon to determine whether a tear is reparable. The meniscus body is divided into thirds: inner, middle, and outer. Tears located at the peripheral attachment sites (meniscofemoral and meniscotibial) are referred to as outer third tears. Single longitudinal tears are usually located in the outer third region or at the peripheral attachments (Fig. 28-1). These tears are classified as red-red because both portions have an internal blood supply and are repaired in all cases with high success rates expected.
Repairs of complex tears and tears that extend into the middle third region are evaluated on an individual basis. Tear patterns in this region include single longitudinal, double longitudinal, triple longitudinal, horizontal, radial, and flap. The rationale for repair of these tears is that removal results in essentially a total meniscectomy because a substantial amount of meniscal tissue is resected (Fig. 28-2). This is especially concerning in younger patients in their 2nd to 4th decades of life and in all athletically active individuals. These tears are often reparable with reasonable success rates, as described later in this chapter.
CONTRAINDICATIONS
Meniscus tears located in the inner third region are not reparable and require débridement. Chronic degenerative tears usually have tear components in multiple planes and are classified as complex. The surgeon must carefully assess the tear pattern and determine the amount and integrity of meniscal tissue that is present. Many of these tears are not reparable (Fig. 28-3). A large flap tear may be reduced and approximated, and if the tissue has adequate integrity, repair is considered in active patients. Chronic degenerative tears in which poor tissue quality is encountered require débridement. The tissue may be thickened or abnormally firm and altered in shape or length. Horizontal tears frequently involve displacement of the meniscus from the joint such that a repair of the horizontal flaps would not result in restoration of meniscus function.
CLINICAL BIOMECHANICS
Meniscus Function
Under static-loading conditions, the menisci assume a significant load-bearing function in the tibiofemoral articulation.2,26,45 At least 50% of the compressive load of the knee joint is transmitted through the menisci in 0° of extension, and approximately 85% of the load is transmitted at 90° of flexion.2 The presence of the menisci increases the contact area to 2.5 times the size of a meniscectomized joint. The larger contact area provided by the menisci reduces the average contact stress (force/unit area) acting between the joint surfaces. Removal of as little as 15% to 34% of a meniscus increases contact pressures by more than 350%.124
Lee and colleagues75 evaluated the biomechanical effects of serial meniscectomies in the posterior segment of the medial meniscus. Compared with the intact state, the medial contact area decreased from 20% (after removal of 50% of the posterior segment of the medial meniscus) to 54% (total meniscectomy). Medial contact stress increased from 24% (50% meniscectomy) to 134% (total meniscectomy). Medial peak contact stress increased from 43% (50% meniscectomy) to 136% (total meniscectomy). The peripheral portion of the medial meniscus provides a greater contribution to increasing contact area and decreasing contact stresses than the central portion. Peak contact stresses increase proportionally with the amount of meniscus removed.
Medial meniscectomy performed after sectioning of the ACL results in increased anterior translation at 20° of knee flexion compared with that measured in knees with an intact ACL.77 Thus, the loss of the medial meniscus after an ACL rupture is problematic, especially in varus-angulated knees. In knees with posterior cruciate ligament (PCL) ruptures, the increase in posterior tibial translation allows a change in tibiofemoral contact in which the menisci posterior horns have a reduced weight-bearing function. This is sometimes referred to as a “PCL meniscectomy.” The effect is greater for the medial compartment in which the middle and anterior thirds of the medial meniscus have less weight-bearing function than the lateral meniscus.
The menisci remain in constant congruity to the tibial and femoral articular surfaces throughout knee flexion and extension135,146 and are thus believed to contribute to stability to the knee joint.92 The lateral meniscus provides concavity to the lateral tibiofemoral joint owing to the normal posterior convexity of the lateral tibial condyle, allowing the stabilizing effect of joint weight-bearing forces to reduce lateral compartment anterior and posterior translations.82 Total lateral meniscectomy results in a 45% to 50% decrease in total contact area and a 235% to 335% increase in peak local contact pressure.103
Loss of the medial meniscus results in a smaller, more medial displacement of the center of pressure. Load is subsequently transmitted through the articular cartilage and subchondral bone to the underlying cancellous bone through this more central route, thus stress-shielding the proximal aspects of the medial tibial cortex. The deleterious effects of meniscectomy on tibiofemoral compartment articular cartilage have been demonstrated in multiple experimental studies.65,104,132,145 For these reasons, it is paramount to preserve meniscal function, if possible, in knees with varus osseous malalignment.
In addition, the menisci provide shock absorption to the knee joint during walking and are theorized to assist in overall lubrication of the articular surfaces.92,141
Meniscus Suture Repair Biomechanics
Various suture repair techniques and suture materials have been tested experimentally to determine initial fixation strength and performance under cyclical loading.13,106 Suture techniques have also been compared with several meniscus repair devices.* Post and coworkers106 compared the pull-out strength of vertical mattress, horizontal, and knot-end sutures in a porcine model using either 2-0 Ethibond, 0-polydioxanone sutures (PDS), or 1-PDS suture material. The vertical mattress technique with 1-PDS suture had significantly greater (P < .05) mean load-to-failure values than any other combination (146 ± 17 N). This was followed by the vertical mattress technique with 0-PDS suture material (116 ± 28 N). The vertical mattress technique had significantly greater mean load-to-failure values than the horizontal mattress technique, regardless of suture type (P < .0001). There was no difference in the relative strength between horizontal and knot-end suture techniques.
Asik and coworkers13 compared the failure strengths of vertical, vertical mattress, vertical loop, horizontal mattress, and knot-end suture techniques in a bovine model. Each group consisted of four medial menisci, and 1-Prolene suture material was used in all specimens. The vertically oriented sutures showed significantly higher initial fixation strengths (mean, ∼131 N) compared with the knot-end (64 N; P < .001) and horizontal (98 N; P < .001) techniques. In another study, Asik and Sener12 compared the mean load to failure of a variety of meniscus repair devices with that of horizontal and vertically oriented sutures in a bovine model. The strongest repair method was the vertical sutures with 0 PDS (mean, 104.7 N). The mean failure strengths of all of the devices were lower than both suturing techniques (range, 9.8 N for the Arthrex dart to 51.4 N for the T-Fix device).
Miller and associates88 assessed healing rates and chondral injuries of three all-inside devices in a goat model 6 months after implantation. A 15-mm longitudinal tear was created in the peripheral 25% of the posterior-central horn and then repaired with either two Meniscal Fasteners (Mitek, Ethicon, Westwood, MA), two 10-mm BioStingers (Linvatec, Largo, FL), or two 10-mm Clearfix Meniscal Screws (Mitek). A group of goats that had undergone repair with two vertical mattress sutures for a similar lesion was used for control.89 The authors reported that the suture group had a significantly higher rate of healing (93% completely healed, 7% no healing) than all three of the device groups (P < .01), which ranged from 43% to 54% complete healing and from 0% to 25% no healing. In addition, significant chondral injury was observed in the majority of animals in all three device groups.
Several investigations compared the biomechanical properties of meniscus arrows with those of vertical and horizontal sutures.4,12,16,24,37,110,126,143 Vertical sutures are superior to both horizontal sutures and meniscus arrows in mean load-to-failure values.12,42,143 Dervin and colleagues37 reported that the meniscus arrow had approximately one half the failure strength of vertical sutures (30 N and 58 N, respectively; P < .001). Song and Lee126 found that the maximum tensile strength of the meniscus arrows was significantly lower (38 N) than both vertical (114 N) and horizontal (75 N) sutures (P < .05). Walsh and coworkers143 reported that the meniscus arrow and meniscus staple had significantly lower mean force-at-failure values (44.3 N and 17.8 N, respectively) than vertical suture (73.9 N; P < .005).
Rankin and associates110 used a bovine model to compare vertical sutures, horizontal sutures, meniscus arrows, and T-Fix repairs in which three sutures or devices were used for each repair. Vertical sutures were stronger than all other repair methods and showed the smallest average residual displacement (0.21 mm). The force required to generate 2 mm of tear displacement was greatest for the vertical sutures and least for the arrow (143 N and 43.6 N, respectively; P < .0001). The superior strength of vertical sutures is believed to be due to the perpendicular orientation to the circumferential collagen bundles of the meniscus.110
Becker and colleagues21 compared the biomechanical behavior of several biodegradable implants for meniscus repair with that of vertical and horizontal mattress sutures in response to cyclical loading and load-to-failure testing. Seventy lateral menisci were removed from patients aged 52 to 60 years prior to total knee replacement. One suture or device was used for each repair. The pull-out strength of the vertical and horizontal sutures was superior to those of the implants. Superior stiffness during load-to-failure testing and lower displacement under cyclical loading were found for the vertical sutures compared with horizontal sutures and all implants.
Nyland and associates100 evaluated displacement (repair site gapping) of all-inside vertically or horizontally placed FasT-Fix (Smith & Nephew, Endoscopy Division, Andover, MA) devices to horizontally placed RapidLoc devices (Mitek Surgical Products, Westwood, MA) under cyclical loading conditions in human cadavers (mean age, 65 ± 7.7 yr). Two implants placed 5 mm apart were used for each repair. The vertical FasT-Fix group had significantly less displacement after 500 cycles than the other two groups (P < .01) and greater stiffness.
Meniscus Repair Healing
There are few published experimental studies on the strength of a healing meniscus suture repair (without cell-based therapy or growth factors) subjected to tensile loads. Newman and associates94 measured the mechanical behavior of canine joints after repair of peripheral and radial meniscus tears. Contralateral limbs served as controls. The peripheral tears were repaired with four vertically oriented sutures, and the radial tears were repaired with two horizontally oriented sutures. Thirteen weeks later, the peripheral repairs demonstrated no statistically significant differences between the repaired and the control limb in compressive force-displacement behavior, input energy, and ratio of dissipated to input energy. All of the peripheral repairs healed, with no gapping at the repair site. However, the radial repairs showed significant differences in the structural and material properties compared with the control limb. These repairs healed with 3- to 5-mm-wide fibrovascular scars, and 10 of 17 (59%) specimens failed to refill the gap completely to the inner meniscal rim. The authors concluded that the mechanical function was restored after peripheral repairs, but not after radial repairs in this animal model.
In a rabbit model, Roeddecker and colleagues117 studied tissue strength after repair of longitudinal meniscal lesions located in the central third region. A 3-mm lesion was created and then either left alone, repaired using one suture, or repaired with a fibrin sealant. The contralateral limb was used as a control. After 6 weeks, the mean relative strength of the healing tissues were 26% (suture) and 42.5% (fibrin glue) of the control values. These strength values remained similar after 13 weeks.
CLINICAL EVALUATION
The presence of tibiofemoral joint line pain on joint palpation is a primary indicator of a meniscus tear. Other clinical signs include pain on forced flexion, obvious meniscal displacement during joint compression and flexion and extension, lack of full extension, and a positive McMurray test.84 All ligament stability tests are performed and compared with the opposite knee joint. MRI may be obtained using a proton-density–weighted, high-resolution, fast-spin-echo sequence107,108 to determine the status of the articular cartilage and menisci. This evaluation is useful in knees with suspected degenerative tears142 and chronic ACL ruptures and to determine whether a meniscus cyst is present. A recent investigation that examined the ability of MRI to predict reparability of longitudinal full-thickness meniscus lesions reported high sensitivity and specificity rates (overall, 94% and 81%, respectively).95
LaPrade and Konowalchuk73 described a figure-four test that attempts to replicate symptoms in patients with tears of the lateral meniscus popliteomeniscal attachments. The patient is placed supine, the knee flexed to approximately 90°, the foot placed over the contralateral knee, and the hip externally rotated. A varus loading at the knee joint increases tensile loading in the damaged posterolateral soft tissue meniscal attachments. The primary symptom from popliteomeniscal tears is lateral compartment pain with activities, especially turning and twisting with sports. MRI is frequently negative. The authors described an open approach to repair the popliteomeniscal attachments. However, these peripheral tears are amendable to an inside-out repair technique, as is described later.
Radiographs taken during the initial examination include lateral at 30° of knee flexion, weight-bearing PA at 45° of knee flexion, and patellofemoral axial. Axial lower limb alignment is measured using full standing hip-knee-ankle weight-bearing radiographs in knees that demonstrate varus or valgus alignment.38 Knees that have deficiency of the posterolateral structures may require lateral stress radiographs. Posterior stress radiographs may be used in patients with PCL ruptures.
Patients complete questionnaires and are interviewed to rate symptoms, functional limitations, sports and occupational activity levels, and patient perception of the overall knee condition according to the Cincinnati Knee Rating System.19
INTRAOPERATIVE EVALUATION
A thorough arthroscopic examination is conducted, documenting articular cartilage surface abnormalities.99 A probe inserted from the medial infrapatellar portal is used to tension the meniscus to determine the integrity of the peripheral rim and the anterior and posterior attachments. The probe is placed underneath the meniscus to visualize the entire undersurface (see Fig. 28-2). Flap tears that otherwise may not be evident may be discovered during this examination.
A 30° or 70° arthroscope is used in the anteromedial portal to examine the posteromedial meniscal region. The anteromedial portal is purposely placed immediately adjacent to the medial border of the patellar tendon. The arthroscope sheath with a blunt obturator is passed along the lateral aspect of the medial femoral condyle distal to the PCL attachment into the posteromedial compartment. The meniscal-synovial junction, the peripheral edge of the meniscus, the opening of a synovial cyst, and the posterior articular surface of the medial femoral condyle are inspected. A nerve hook is passed from the anteromedial portal and brought over the top of the meniscus into the posteromedial compartment. The peripheral attachment of the posterior horn of the medial meniscus frequently cannot be completely visualized unless this view is obtained.27
Critical Points INTRAOPERATIVE EVALUATION
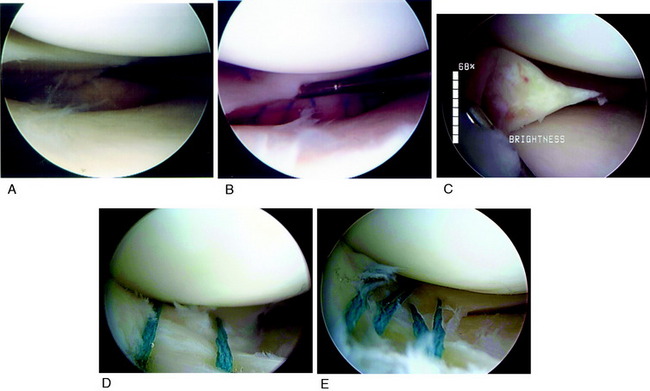
The arthroscopic examination in patients with lateral and posterolateral joint pain may not reveal obvious tears of the posterosuperior meniscus attachments. There may be observable tears in the inferior meniscus tissues about the popliteal hiatus and meniscotibial attachments (Fig. 28-4). There is frequently enlargement of the popliteal hiatus and subtle interstitial tearing of the meniscotibial posterior horn attachments that allow the posterior horn to be abnormally elevated and displaced anteriorly into the lateral compartment. These displacement tests of the posterior horn are performed at 60° to 70° of flexion using a figure-four position because the increased joint gap allows a nerve hook to easily displace the posterior horn and demonstrate the abnormal slackness of the attachments. The authors have frequently encountered athletes who have had a prior negative arthroscopic examination and MRI who have demonstrable posterior horn popliteomeniscal attachment tears that require suture repair.
OPERATIVE TECHNIQUE
Patient Preparation
The patient is placed in the supine position on the operating table so that the affected leg is elevated (Fig. 28-5). The foot of the surgical bed is adjusted to allow 90° of knee flexion. A tourniquet and leg holder are used, but the tourniquet is inflated only for the initial exposure. The leg holder is placed at the middle of the thigh, which allows an assistant to open the tibiofemoral compartment under maximum tension for visualization and meniscus surgery. The extremity is draped free to allow easy positioning during surgery. Standard medial and lateral patellar arthroscopic portals, placed directly adjacent to the patellar tendon, are used for the diagnostic arthroscopy. A common mistake is to place the arthroscopic portals too far medially or laterally over the femoral condyles, where instrument passage damages the femoral articular cartilage. The safe area for instrument passage is with the portal just medial and lateral to the patellar tendon with passage into the femoral notch region.
Critical Points OPERATIVE TECHNIQUE
Exposure for Medial Meniscus Repair
Medial Meniscus Suture Repair Techniques
Multiple 2-0 Braided Polyester Nonabsorbable Sutures Used on 10-Inch Straight Cutting Needle
Exposure for Medial Meniscus Repair
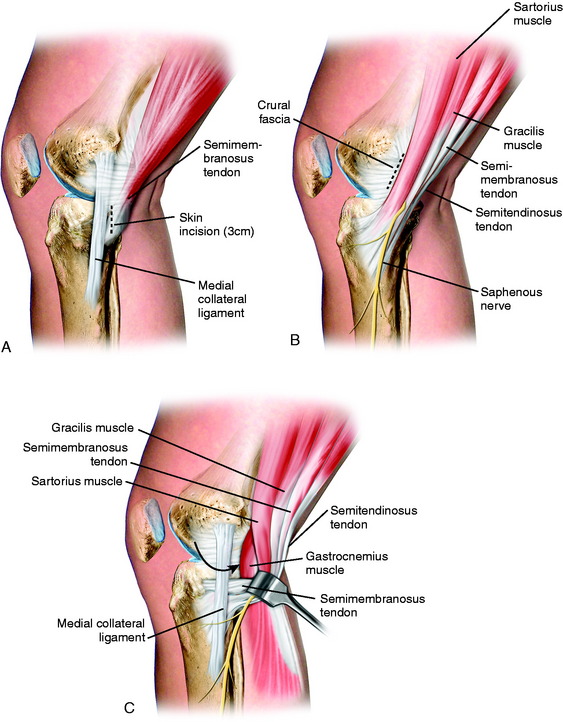
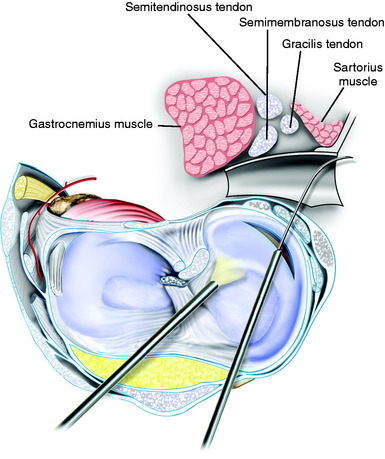
With the surgeon seated, using a headlight, and the sterile prepared foot in the surgeon’s lap, the knee is flexed to 60° and a 3-cm vertical skin incision is made just posterior to the superficial medial collateral ligament (SMCL; Fig. 28-6). The tourniquet is inflated for the surgical exposure. The incision is centered just below the joint line (one third above, two thirds below) to allow retrieval of sutures. Avoid placing the incision too posterior in order to protect the saphenous vein and nerve. The subcutaneous dissection proceeds from the superior aspect of the wound down to the fascia. Care must be taken in the inferior aspect of the wound to avoid damage to the saphenous vein and nerve. Two retractors are used to provide visualization of the next layer of structures, the crural fascia and sartorius.
Blunt dissection with an index finger allows development of a plane between the medial gastrocnemius tendon and the posterior capsule. A Henning retractor or spoon is inserted, allowing safe suture placement and needle retrieval (Fig. 28-7). The anesthesiologist is asked to provide muscle relaxation so that the gastrocnemius and semimembranosus muscles can be retracted. If the exposure is inadequate at this point, an alternative approach is to further dissect the semimembranosus tendon, which is elevated proximally to gain exposure just distal to the tendon. This is a less ideal approach because it is necessary to avoid placing sutures through the semimembranosus tendon just above its tibial attachment site.
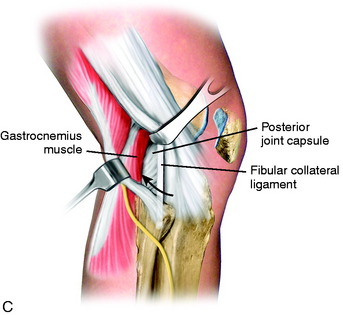
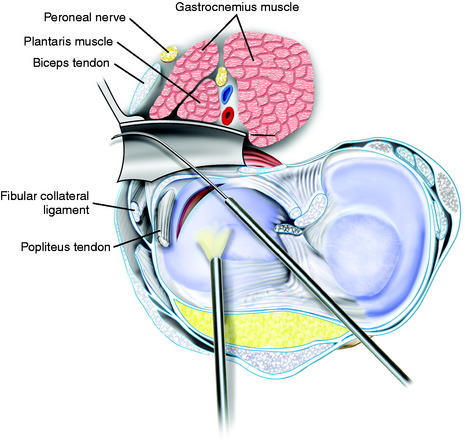
Exposure for Lateral Meniscus Repair
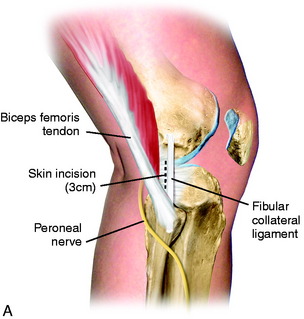
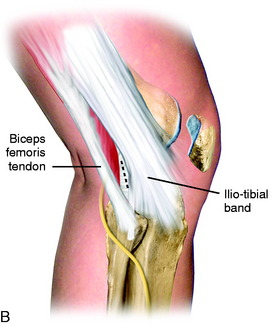
The tourniquet is inflated and the surgeon seated using a headlight with the sterile prepared foot in the surgeon’s lap. The knee is flexed to 60° and a 3-cm skin incision is made just behind the fibular collateral ligament (FCL; Fig. 28-8). The incision is centered just below the joint line (one third above, two thirds below) to allow retrieval of sutures. The interval between the biceps tendon insertion and the iliotibial band is identified and incised, staying superior to the biceps short head muscle fibers. The fascia overlying the posterolateral structures and FCL is gently dissected and peeled from superior to the fibular head. This is performed by applying tension with forceps to the incised fascia and using a thin-blade scissors to peel and strip the fascial tissues to the head of the fibula, protecting the FCL. The retractors are positioned between the biceps tendon and the iliotibial band. The deep layer consists of the posterior capsule and the lateral gastrocnemius tendon. The gastrocnemius tendon has a normal proximal attachment to the posterior capsule, making it necessary to gently dissect the tendon with scissors off the posterior capsule at the joint line. The peroneal nerve inferior to the biceps tendon is palpated and protected, but is not dissected.
The surgeon must be careful to remain posterior to the FCL and other posterolateral structures. The key step is to initially enter the space anterior to the lateral gastrocnemius tendon just above the fibular head. This avoids penetrating and opening the posterior capsule. The space between the posterolateral capsule and the lateral gastrocnemius tendon is further developed bluntly with the index finger. A Henning retractor is used to push the neurovascular bundle medially (Fig. 28-9). The inferior lateral geniculate artery may be visualized in the inferior aspect of the exposure and may be damaged and require electrocoagulation (which is avoided if possible to maintain the vascular supply to the lateral meniscus). The retractor must always be positioned anterior to the gastrocnemius muscle and tendon and directly posterior to the posterior capsule and posterior meniscus bed. The retractor blocks the suture needles from passing too posterior and potentially injuring the common peroneal nerve. During the meniscus suture steps, the surgeon should frequently check the position of the retractor to always ensure that it is anterior to the gastrocnemius muscle. If the retractor is mistakenly placed posterior to the gastrocnemius muscle, the peroneal nerve may be injured.
Suture Repair Techniques
Multiple 2-0 braided polyester nonabsorbable sutures (Ticron, Davis and Geck Co., Danbury, CT; or Ethibond, Ethicon Inc., Somerville, NJ) are used on a 10-inch straight cutting needle to repair all meniscus tears. The sutures are inserted through the superior and inferior meniscal surfaces in an interrupted vertical fashion to close the meniscus tear both superiorly and inferiorly. The vertical placement is used owing to its higher failure strength than that of horizontally placed sutures.111 In addition, the vertical suture orientation mimics the function of the radial collagen fibers within the meniscus, which can improve its load-carrying capacity.29
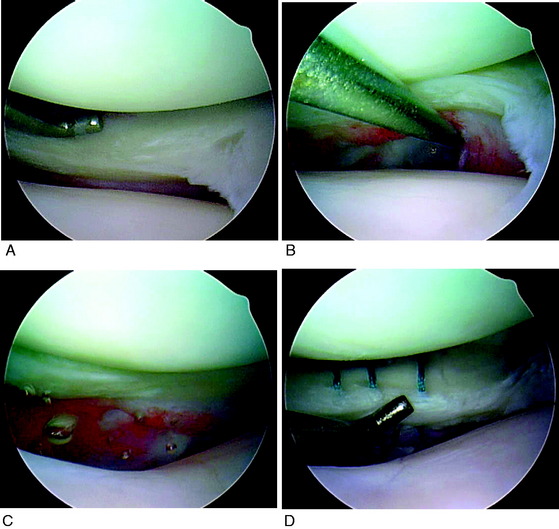
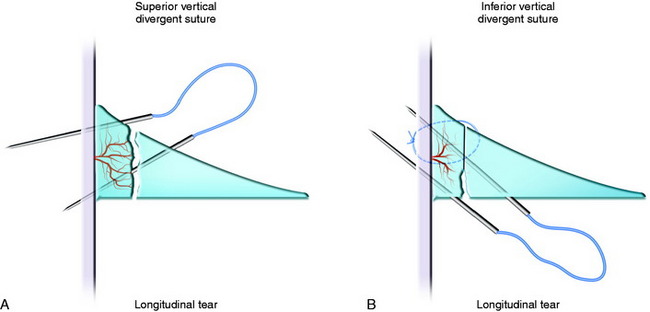
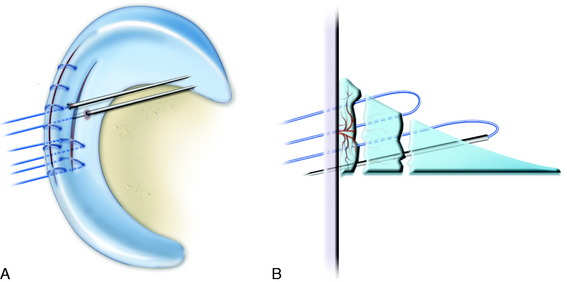
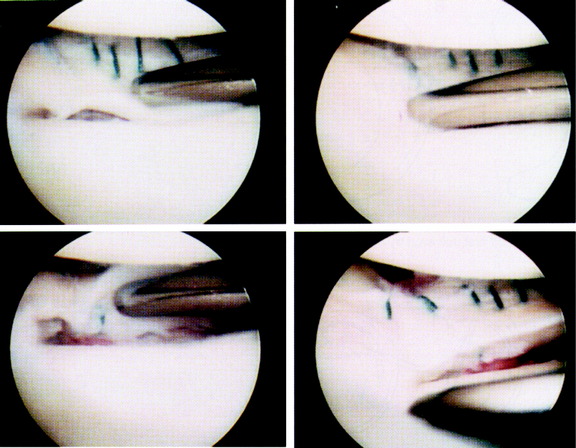
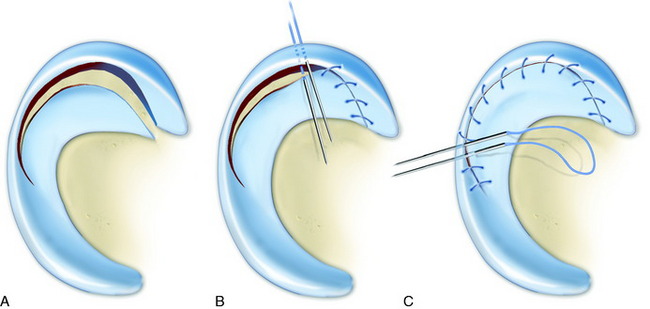
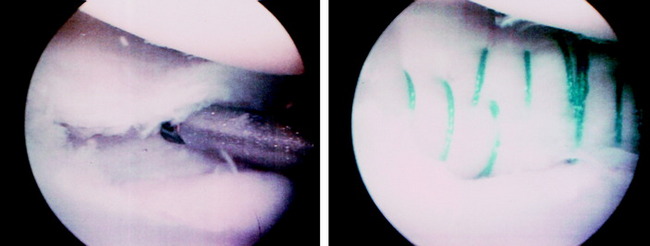
Single and Double Longitudinal Tears
A double-stacked suture technique is used for single and double longitudinal meniscus tears. This technique consists of two layers of sutures (Figs. 28-10 and 28-11) placed at 3- to 4-mm intervals along the length of the tear. The first layer of sutures is placed superiorly to anchor the meniscus to its bed and prevent superior migration of the meniscus during the repair. The cannula is used to hold and reduce the torn meniscus on the tibia.
The first pass of the double-armed suture is placed in the meniscal-synovial junction (periphery) of the intact portion of the meniscus. The second pass of the double-armed suture is placed through the torn portion of the meniscus in a vertical plane so that it bridges the tear (Fig. 28-12). The inferior sutures are placed next in a vertical plane, crossing the tear in the same manner as the superior sutures. The sutures are brought out through the accessory incision and tied directly over the posterior meniscal attachment and capsule. The sutures are tied as they are passed to determine the apposition of the tear surfaces. The tension in each suture is confirmed arthroscopically after the knot is tied. This double-stacked technique provides stable fixation of the meniscal tear on both sides and entirely closes the meniscus gap at the repair site (Fig. 28-13).
Critical Points OPERATIVE TECHNIQUES
Single and Double Longitudinal Tears
Flap Tears
Repair of Lateral Popliteomeniscal Fascicles and Attachments
Techniques to Stimulate Healing of Meniscus Repairs
Radial Tears
Horizontal sutures are placed at 2- to 4-mm intervals along the tear to repair radial meniscus tears. The inner sutures are placed first and securely tied, followed by sutures located in the periphery (Fig. 28-14). Three to four sutures are used on the superior surface, and one or two sutures are used on the inferior surface. The initial sutures are placed first through the body using the needle to place the meniscus toward the tear site, followed by needle passage through the meniscus bed. This allows the tear site gap to be closed. Only radial tears that extend to the outer third of the meniscus body are repaired, because those that are confined to the inner and middle zones have a poor blood supply and will not heal. A radial tear that extends to the meniscus rim compromises the hoop stress and is equivalent to a total loss of meniscus function. Occasionally, the edges of the radial tear are degenerative with poor suture-holding capability and repair is not possible. Traumatic radial tears have a better chance of healing. The goal is to retain partial meniscus function, if possible, because it is rare to have successful healing of a tear in the inner aspect of the meniscus. Because only a limited number of sutures are used, the holding strength is low and a period of non–weight-bearing for 4 weeks is required to prevent disruption of the repair site. The patient is advised that this type of repair has a guarded prognosis in terms of providing function. The repair may heal, but the meniscus tear edges separate in the healing process with the interval replaced with poorly organized fibrous tissue with an elongated meniscus structure that displaces from the joint.
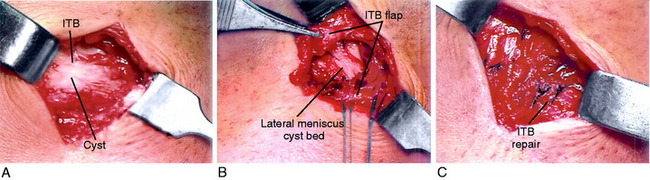
Lateral Radial Tears Associated with a Cyst
Because partial meniscectomy and cyst excision may remove a substantial portion of the meniscus body and disrupt its peripheral rim, a cyst should be excised through a limited open lateral exposure (Fig. 28-15). This is followed by repair of the peripheral rim of the meniscus using an open technique. Then, the radial tear and any associated horizontal tears may be repaired using the arthroscopic techniques described previously. It is not recommended to evacuate the cyst through the intra-articular radial tear site because this damages meniscus tissues and prevents repair. A lateral meniscus cyst is commonly associated with combined radial and horizontal tears that are not reparable; however, this is difficult to determine preoperatively. The mistake is to excise the meniscus in a patient 50 years of age or younger in whom a repair is possible to preserve some meniscus function where progression to lateral compartment arthritis occurs in a short time, particularly in a valgus-aligned lower extremity.
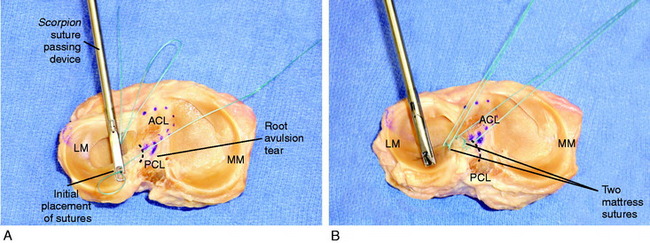
Meniscus Attachment Root Tears
An important reparable meniscus tear is one in which the posterior horn is torn directly at its posterior attachment, producing a complete loss of meniscus function as it displaces under weight-bearing loads. Instruments used in shoulder rotator cuff tears can be used to pass two mattress-type sutures for firm fixation of the meniscus (Fig. 28-16). Alternatively, a suture lasso instrument can be passed through a small tibial tunnel. The suturing instrument is passed twice through the medial or lateral portal using a cannula. The mattress suture is performed rather than a single throw of the suture to increase holding strength. A leg holder is required to allow sufficient joint opening for passing and using the suture device, particularly for medial meniscus root tears. Without suturing, the tear results in complete loss of meniscus function. A 4- to 5-mm tibial tunnel using an ACL tibial guide is placed directly at the attachment site. The sutures are tied over a tibial post. Weight-bearing is restricted for 4 weeks.
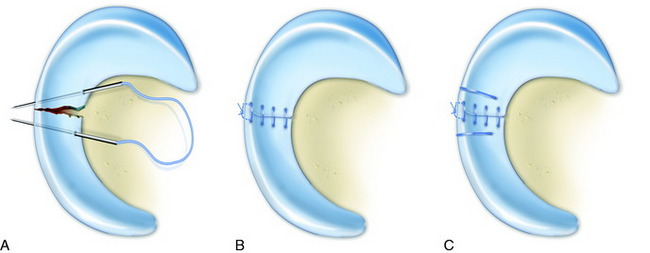
Flap Tears
Two sets of sutures are required to repair flap tears (Fig. 28-17). Tension sutures are inserted first through the flap and then into the intact meniscal rim to anchor and reduce the flap into its anatomic bed. This restores the longitudinally running fibers of the meniscus and is performed in a manner similar to that for a radial tear repair. With the meniscus reduced, the remaining tear is repaired in the same fashion as a longitudinal tear, with superior and inferior vertical divergent sutures. The radial portion of the flap tear may only partially heal; however, the more peripheral longitudinal tear may heal, retaining partial meniscus function. Flap tears that represent 75% of the meniscus with the tear at the periphery or red-white junction are amenable for repair. Smaller flap tears 10 to 12 mm in length that occupy the red-white and white-white zones are not repaired.
Techniques to Stimulate Healing of Meniscus Repairs
The initial vascular response of the meniscus to injury and tearing is characterized by the formation of a fibrin clot that is rich in inflammatory cells. This clot acts as a scaffold through which cells from the synovial membrane adjacent to the meniscus migrate.7,8 The meniscal fibrochondrocytes may add to the intrinsic healing process.
Several experimental studies have investigated techniques to stimulate meniscus healing, including trephination or vascular ingrowth,8,46,149,150 abrasion of the meniscal-synovial region,51,93,112 grafting of the synovial pedicle,47 incorporation of a fibrin clot,93,112 and use of growth factors and cell-based therapy.* Although trephination, or creation of vascular access channels, has been demonstrated experimentally to promote healing, the creation of these channels disrupts the normal peripheral structure of the meniscus. Investigations of growth factors and cell-based therapies have all been experimental to date, with no published clinical trials to document the potential effectiveness.
The incorporation of a fibrin clot52 at the repair site is theoretically beneficial because it provides a scaffold to support the reparative cells and provide chemotactic and mitogenic stimuli.144 The absence of a well-defined fibrin clot in the initial healing period along with a limited vascular supply may be the most important factors limiting meniscus healing in tears located in the middle third region. The problem is that a fibrin clot inserted between the tear edges of the meniscus prevents meticulous suturing of the tear both superiorly and inferiorly. A fibrin clot may be beneficial in horizontal tears in which the clot may be placed between the superior and the inferior tear sites. The clot is prepared with a glass stirring rod. The clot is passed into the knee joint through a cannula, guided by a loop of suture placed around the clot from previously passed meniscus suture needles.
Ritchie and coworkers112 found that abrasion of the parameniscal synovium was more effective than the incorporation of a fibrin clot in central meniscus repairs. Synovial abrasion stimulates vessels and mesenchymal cells to form a proliferate vascular pannus that migrates into the repair site.35,50,123
Several studies have demonstrated that an ACL reconstruction performed concomitantly with meniscal repair increases the success rate because the reconstruction protects the meniscus repair site owing to the restored knee stability and provides the beneficial healing effects of the postoperative hemarthrosis.33,36,60,91,134 In the majority of meniscus repairs done without concomitant ACL reconstruction, the meniscal-synovial junction is abraded and a micropick used in the intercondylar notch region to produce bleeding that promotes adherence of platelets and fibrin at the repair site. The meticulous suture placement described in this chapter stabilizes the tear and prevents gap formation at the repair site, allowing the subsequent repair process to progress.
AUTHORS’ CLINICAL STUDIES
Arthroscopic Assessment of Meniscus Repairs in the Outer and Middle Third Regions
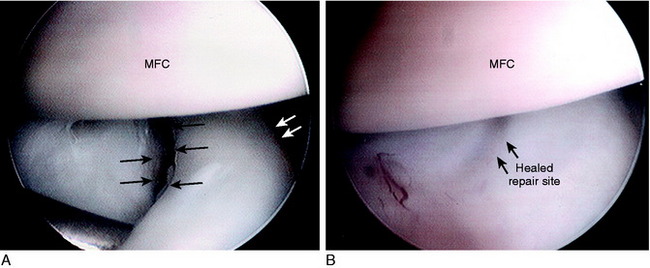
An investigation was conducted on 66 patients who underwent a concomitant meniscus repair and ACL reconstruction, then follow-up arthroscopy 6 to 25 months postoperatively.31 There were a total of 79 meniscus repairs; 51 were done for tears located in the outer third region (periphery) and 28 were done for complex tears that extended into the middle third avascular region. Follow-up arthroscopy was indicated for symptoms related to either tibial hardware or tibiofemoral joint pain.
Repairs of tears located in the outer third region were classified as completely healed in 94%, partially healed in 4%, and failed in 2% (Table 28-1). Repairs of tears that extended into the avascular region were classified as completely healed in 54%, partially healed in 32%, and failed in 14%. The other factors analyzed in this study had no significant effect on the healing rates.
Outcome of 198 Meniscus Repairs in the Middle Third Region
The clinical outcome of 198 meniscus tears that extended into the middle third region, or that had a rim width of 4 mm or greater, was determined in a prospective study.121 Either a clinical examination a minimum of 2 years postoperatively or follow-up arthroscopy were used for inclusionary criteria. The 198 meniscus repairs were performed in 177 patients. Of these, 180 repairs (91%) were evaluated with a clinical examination a mean of 42 months (range, 23–116 mo) postoperatively. In addition, 91 repairs (46%) were evaluated with a follow-up arthroscopic examination a mean of 18 months (range, 2–81 mo) after the initial repair.
Critical Points AUTHORS’ CLINICAL STUDIES: OUTCOME OF 198 MENISCUS REPAIRS IN MIDDLE THIRD REGION
The overall reoperation rate for tibiofemoral symptoms was 20% (39 meniscus tears). All patients who had tibiofemoral pain underwent follow-up arthroscopy. The reoperation rates according to the type of tear are shown in Table 28-2. The limited number of meniscal tears in the individual classification categories precludes specific conclusions on the outcome for each tear pattern. Of the 39 menisci examined, 2 were classified as healed, 13 as partially healed, and 24 as failed. The reoperation rates for tibiofemoral joint symptoms were 12% for single longitudinal tears, 28% for double longitudinal tears, and 27% for the most difficult complex multiplanar tears.
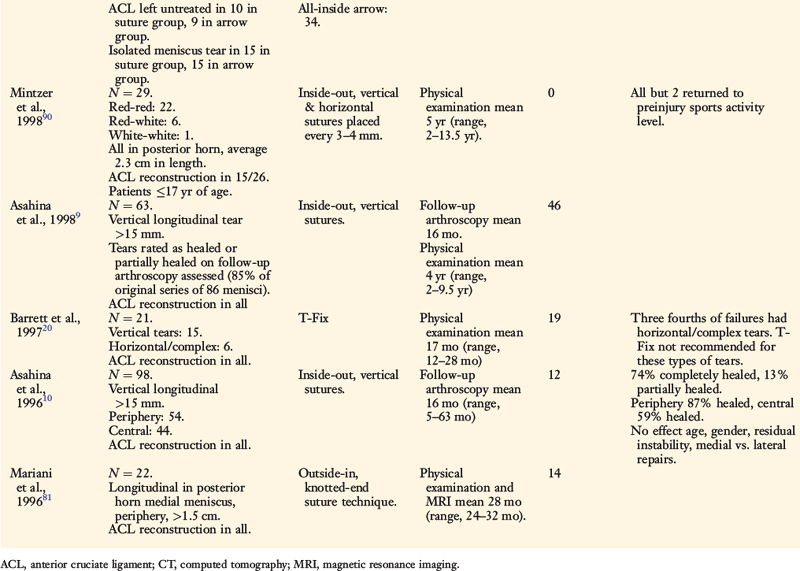
TABLE 28-2 Reoperation Rates for Meniscal Repairs due to Tibiofemoral Joint Symptoms
| Type of Meniscus Tear | Total Number of Meniscus Tears in Study | Number Requiring Repeat Arthroscopy |
|---|---|---|
| Single longitudinal | 92 | 11 (12%) |
| Double longitudinal | 40 | 11 (28%) |
| Complex multiplanar | 26 | 7 (27%) |
| Radial | 15 | 4 (27%) |
| Horizontal | 14 | 4 (29%) |
| Flap | 9 | 2 (22%) |
| Triple longitudinal | 2 | 0 |
| Total | 198 | 39 (20%) |
The effect of six factors on healing rates of meniscal repairs was evaluated (Table 28-3). Statistically significant differences were found in the rates of healing for three factors: tibiofemoral compartment of the meniscus repair (higher healing rate in lateral meniscus repairs than in medial meniscus repairs), time from repair to follow-up arthroscopy (higher healing rate in patients evaluated ≤12 mo compared with those evaluated >12 mo postoperatively), and the presence of tibiofemoral symptoms (higher healing rate in asymptomatic patients than in symptomatic patients). A trend (P = .06) was observed for the factor of time from the original knee injury to the meniscus repair (higher healing rate in patients operated on ≤10 wk than in those operated on >10 wk after the injury).
TABLE 28-3 Effect of Various Factors on Healing Rates of Meniscal Repairs that Had Follow-up Arthroscopy
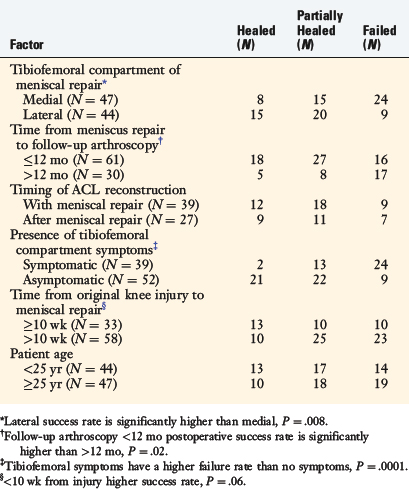
The significantly higher rate of retention of lateral meniscus repairs found in this study agrees with those of other reports.91,120,123 The reasons for the higher failure rate of medial meniscus repairs are unknown at present. The results of this investigation support the repair of meniscus tears that extend into the middle avascular region, especially in patients in their 20s and 30s and highly competitive athletes. The study’s reoperation rate should not be interpreted as the rate of meniscal healing. The long-term function and chondroprotective effects of the repaired menisci need to be determined, and this group of patients is under prospective long-term evaluation.
Outcome of Meniscus Repairs in the Middle Third Region in Patients 40 Years of Age and Older
The clinical outcome of meniscus tears that extended into the avascular region in patients 40 years of age and older was prospectively determined.97 Thirty of 31 consecutive meniscus repairs in 29 patients were followed by either clinical examination or arthroscopy after the initial repair. A clinical evaluation was conducted in 27 patients (28 meniscus repairs) a mean of 34 months (range, 23–71 mo) postoperatively. Six repairs were evaluated with arthroscopy a mean of 24 months (range, 16–36 mo) after the repair.
At follow-up, 26 meniscus repairs (87%) both were asymptomatic for tibiofemoral joint symptoms and had not required further surgery (Table 28-4). There was no significant effect of the tibiofemoral compartment of the meniscus repair, chronicity of injury, concomitant ACL reconstruction, or condition of the articular cartilage on the presence of tibiofemoral pain or meniscus resection (Table 28-5).
TABLE 28-4 Types of Meniscal Tears and Results of Repair According to Follow-up Arthroscopy and Clinical Examination
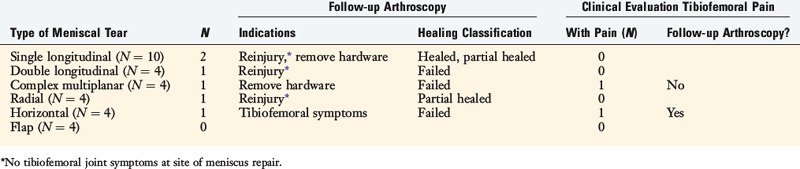
TABLE 28-5 Effect of Four Factors on Presence of Tibiofemoral Symptoms or Arthroscopic Second-Look Failure of Meniscal Repair

There were no infections, knee motion problems, saphenous neuritis, or other major complications.
Outcome of Meniscus Repairs in the Middle Third Region in Patients Younger than 20 Years of Age
A prospective study was conducted on 71 of 74 consecutive meniscus repairs (96% follow-up) that had been done in 58 patients under the age of 20 to determine the clinical outcome.96 Sixty-seven meniscal repairs were examined clinically a mean of 51 months (range, 24–196 mo) after the operation. Thirty-six menisci in 28 knees were evaluated during follow-up arthroscopy a mean of 18 months (range, 3–60 mo) postoperatively. Of these, only 4 menisci were not examined a minimum of 2 years postoperatively.
There was no statistically significant effect of the tibiofemoral compartment of the meniscal repair, chronicity of injury, or concomitant ACL reconstruction on the presence of tibiofemoral joint symptoms or arthroscopic classification of failure. The presence of tibiofemoral pain on the physical examination was found to have a sensitivity rate of 57% and a specificity rate of 93% (Table 28-6) in identifying meniscus repairs classified as failed or that required partial resection at follow-up arthroscopy. The positive predictive value was 92%, and the negative predictive value was 61%.
TABLE 28-6 Diagnostic Test Rates of Tibiofemoral Joint Pain on Clinical Examination in Identifying Failed Meniscal Repairs
| Diagnostic Test | Result (%) |
|---|---|
| Prevalence | 58 |
| Sensitivity | 57 |
| Specificity | 93 |
| False-positive | 7 |
| False-negative | 43 |
| Positive predictive value | 92 |
| Negative predictive value | 61 |
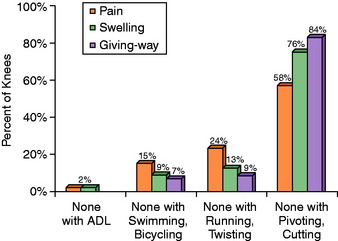
Of the 45 knees that had a concomitant meniscal repair and ACL reconstruction, 26 (58%) had no pain, 34 (76%) had no swelling, and 38 (84%) had no giving-way with sports activities involving jumping, cutting, and pivoting at follow-up (Fig. 28-18). None of these knees had functional limitations with walking, stair-climbing, or squatting. Forty (89%) had no or only slight problems with running, jumping, and twisting.
Before the meniscus repair, 34 patients were participating in various types of athletic activities and 11 had given up sports owing to knee problems (Table 28-7). At follow-up, 33 (73%) had returned to athletics without symptoms or limitations, and 3 (7%) were participating in sports with symptoms against advice. Two (4%) had not returned to sports owing to the knee condition, and 7 (16%) had given up sports activities owing to factors unrelated to the knee condition. At follow-up, 39 (87%) rated the overall knee condition as normal or very good; 2 (4%), as good; 3 (7%), as fair; and 1 (2%), as poor.
TABLE 28-7 Sports Activities of Patients before the Meniscal Repair and at Follow-up*
| Type of Sport | Preoperative | Follow-up |
|---|---|---|
| Jumping, hard pivoting, cutting | 28 | 18 |
| Running, twisting, turning | 3 | 10 |
| Swimming, bicycling | 3 | 8 |
| None | 11 | 9 |
| Change in sports activities | ||
| Increased level, no symptoms | 10 | |
| Same level, no symptoms | 13 | |
| Decreased level, no symptoms | 10 | |
| Playing with symptoms | 3 | |
| No sports, knee-related reasons | 2 | |
| No sports, non–knee-related reasons | 7 |
* In 45 knees that had an anterior cruciate ligament reconstruction and a meniscal repair.
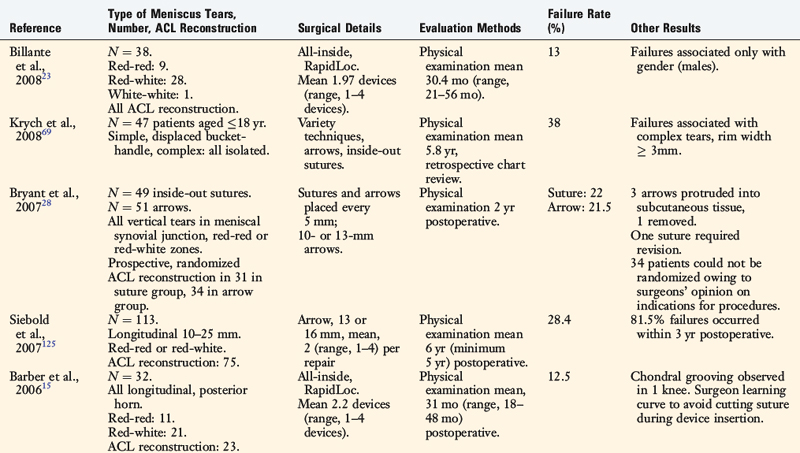
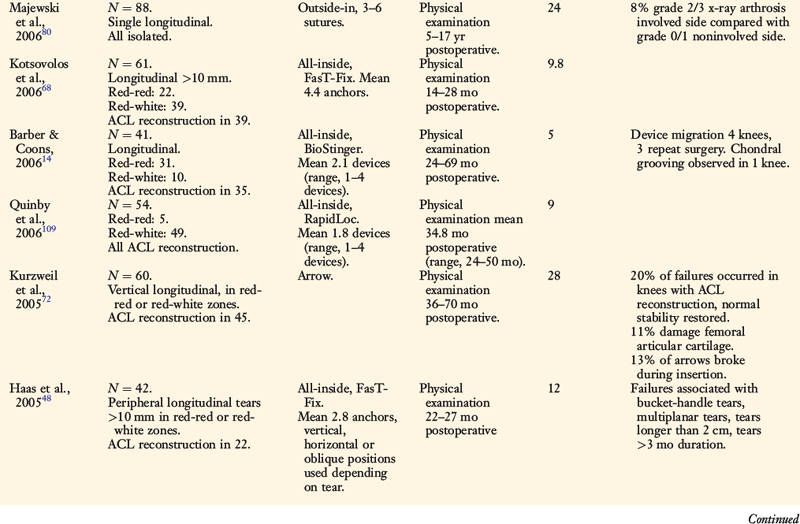
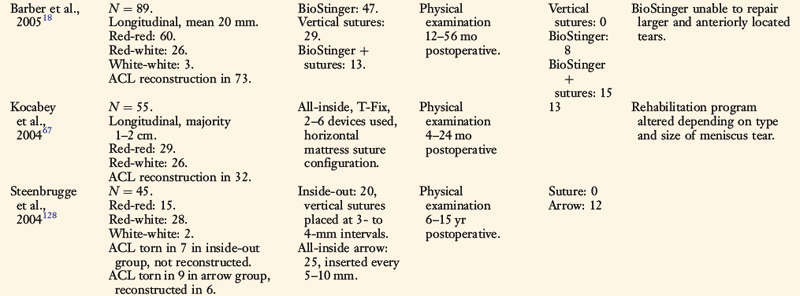
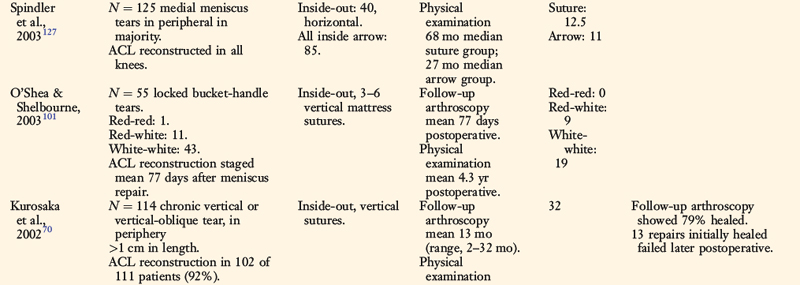
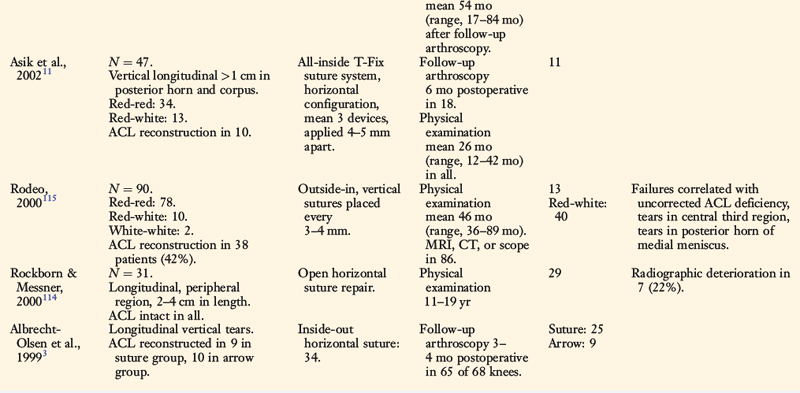
RESULTS FROM OTHER CLINICAL STUDIES
A summary of the clinical outcome of meniscal repair from a variety of investigations published since the mid 1990s is shown in Table 28-8.* The majority of investigations have followed vertical meniscus suture repair techniques; few have reported on the outcome of horizontal suture repair or all-inside fixators. Failure rates of vertical and horizontal suture repairs vary greatly, as do correlations with side of meniscus tear, concurrent ACL reconstruction, location of meniscus tear, age, and gender. For instance, Rodeo et al.115 followed 90 patients who received an outside-in vertical suture meniscal repair and found that failures were associated with uncorrected ACL-deficiency, tears located in the middle third region, and tears located in the posterior horn of the medial meniscus. Asahina et al10 investigated 98 patients who received inside-out vertical suture repair of meniscus tears and found no effect of age, gender, residual instability, or side of meniscus repair with failure.
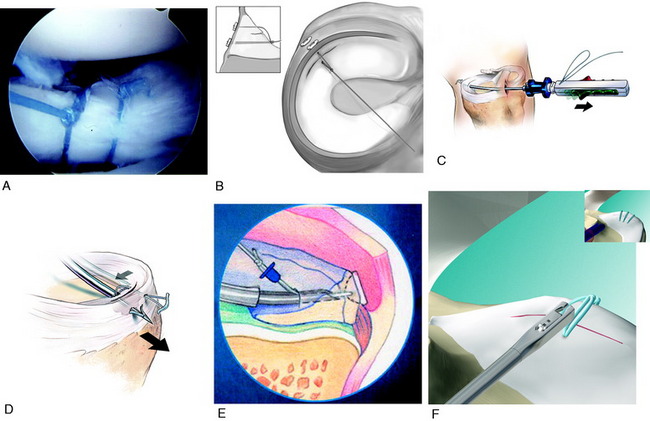
Investigations of newer all-inside suture systems (Fig. 28-19) such as the RapidLoc (DePuy Mitek, Inc., Raynham, MA), MaxFire Meniscal Repair System (Biomet, Warsaw, IN), and FasT-Fix (Acufex, Smith & Nephew, Andover, MA) reported acceptable failure rates between 9% and 13%.11,23,48,64,67,68,109 However, longer-term follow-up is required of this technique to ensure that the rate of failure does not increase with time. Studies with longer-term follow-up of suture repair techniques tend to report higher failure rates, such as 46% in Asahina and associates’ series9 (mean 4 yr; range, 2–9.5 yr follow-up) and 32% in Kurosaka and colleagues’ series70 (mean 4.5 yr; range, 1.4–7 yr follow-up). Kurosaka and colleagues70 found that whereas 79% of 114 meniscal repairs showed arthroscopic demonstration of healing an average of 13 months postoperatively, 13 additional repairs failed later, and cautioned that longer-term studies are required. In addition, most authors use only two to three sutures with the all-inside systems, and studies typically include patients who had concomitant ACL reconstruction. Concern exists regarding the expected inferior fixation strength of these techniques compared with the multiple vertical divergent suturing procedure described in this chapter.
Complications and deteriorating results have been reported following the use of all-inside fixation devices.64,72,74,87,125,136 Kurzweil and coworkers72 followed 60 consecutive meniscus repairs in 57 patients done with an all-inside technique using the Meniscus Arrow (Bionx Implants, Malvern, PA). Forty-five repairs were done concomitantly with ACL reconstructions. At follow-up, 36 to 70 months postoperatively, 17 repairs (28%) had failed and 15 patients (26%) required repeat surgery owing to persistent symptoms. The authors reported several complications, including scoring of the femoral articular cartilage in 6 knees (35% of the failures) and slippage of the cannula during fixator implantation with subsequent arrow breakage in 7 cases. Siebold and associates125 reported a 28% failure rate a mean of 6 years postoperatively in 113 consecutive patients whose meniscus tears were repaired with the Meniscus Arrow. Lee and Diduch74 reported an increasing rate of failure over time in 28 patients who underwent meniscus repair with the Meniscus Arrow and a concomitant ACL reconstruction. The initial success rate of 90.6% reported a mean of 2.3 years postoperatively decreased to 71.4% at 6.6 years. The investigators hypothesized that repair with the arrow resulted in a high rate of partial or incomplete meniscus healing, predisposing the meniscus to subsequent tearing. All failures occurred in knees in which normal or nearly normal stability had been achieved according to KT-2000 data. Complications with this device including chondral damage, cyst formation, chronic effusions, joint irritation, synovitis; device breakage and migration into the extra-articular soft tissues have been reported by several authors.5,32,57,58,72,86,87,102,136
The question of whether meniscal repair is effective in preventing joint deterioration remains unanswered according to published clinical data. The problem of commonly associated ACL tears or other injuries found in these knees precludes scientifically justifiable answers. However, based on the well-documented irreparable joint damage and poor results of long-term clinical studies after partial and total meniscectomy,* preservation of meniscal tissue is paramount for long-term joint function. It is the authors’ opinion that the gold standard for meniscus repair procedures remains a meticulous inside-out repair with multiple vertical divergent sutures and an accessory posteromedial or posterolateral approach to tie the sutures directly posterior to the meniscus attachment. This procedure requires added time and assistants. The less ideal all-inside devices, although more time-efficient, have too high of a failure and complication rate. Revision meniscus repair procedures are often not possible and therefore, the technique with the highest success rate should be performed initially. The authors consider meniscus repair as important, if not more important, as an ACL reconstruction in regard to long-term knee function. The procedures and surgical approaches are not difficult and the anatomical approach is straightforward. There should be an exceedingly low risk of intraoperative complications such as nerve damage and arthrofibrosis if the operative procedure and rehabilitation program discussed in this and other chapters are followed.
In the future, tissue engineering may provide increased success rates of meniscus repair, especially for tears that extend into the avascular region.1,30,34,40,131 Cell-based therapy using either meniscal fibrochondrocytes, articular chondrocytes, or mesenchymal stem cells seeded onto scaffolds offers promise,116,130 as does the introduction of growth factors into repair sites.
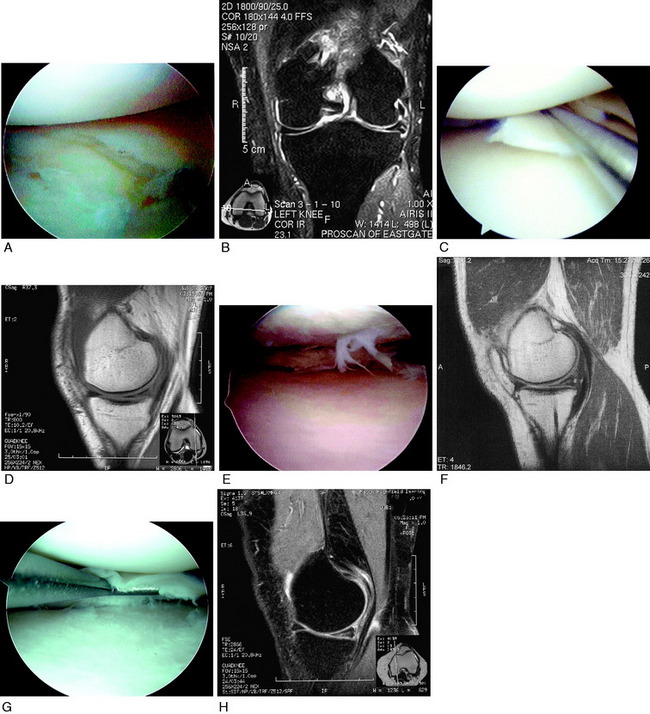
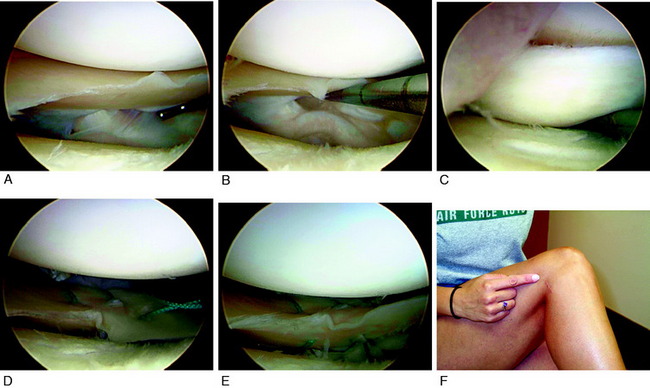
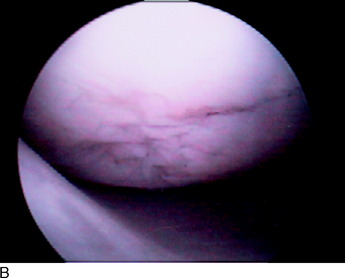
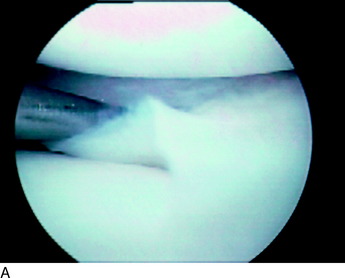
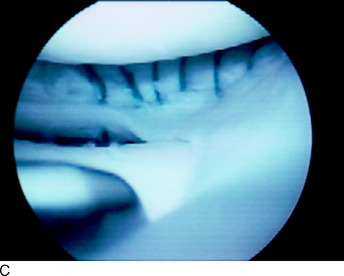
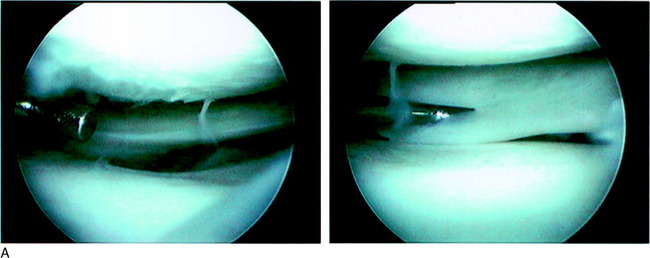
Arthroscopy was performed that initially demonstrated a normal lateral meniscus (Fig. 28-20A). However, further evaluation revealed a large tear of the meniscotibial attachments (see Fig. 28-20B) with an abnormal lift-off and anterior subluxation of the posterior horn from the tibia (see Fig. 28-20C). Maximal varus loading and lateral joint opening was required to separate the tibiofemoral joint, which produced the subluxation of the posterior horn. Multiple vertical divergent sutures were placed superiorly and inferiorly with an outside-in technique, avoiding the popliteal tendon (see Fig. 28-20D and E). The initial sutures were placed superiorly to reduce the meniscus onto the tibia. The patient recovered and returned to athletic activities 6 months postoperatively without pain. The cosmetic appearance of the 2-cm posterolateral approach is shown (see Fig. 28-20F).
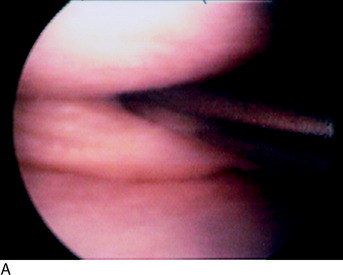
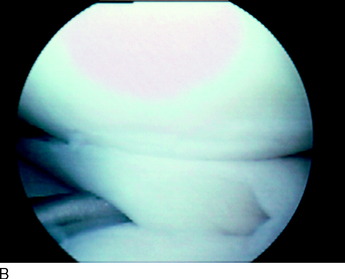
A 16-year-old male athlete presented with a chronic medial meniscus tear that had been treated conservatively. Physical examination demonstrated medial tibiofemoral joint pain, but all other tests and radiographs were normal. At arthroscopy, an unusual complex horizontal meniscal tear was found that extended throughout the entire meniscal body from the periphery to the inner meniscal margin (Fig. 28-21A). Removal of either the superior or the inferior tear component would have substantially compromised the remaining meniscal tissue and function. The body of the meniscus, between the superior and the inferior tear edges, was rasped. Multiple vertical divergent sutures were placed to close the gap between the superior and the inferior tear edges (see Fig. 28-21B).
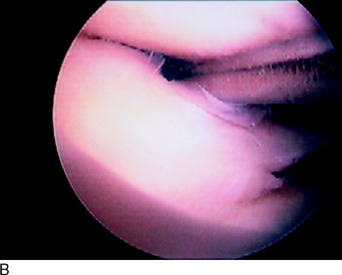
An 18-year-old Division I collegiate hockey player presented 10 months after sustaining a right knee injury in which the lateral aspect of his leg was struck with a helmet. He complained of pain with squatting, twisting, and turning activities. Examination demonstrated lateral joint line tenderness in deep flexion, but no other abnormalities. MRI was negative for a lateral meniscus tear. The patient continued to have pain over the ensuing 5 months and elected to undergo arthroscopy for a potential hypermobile meniscus abnormality. The lateral meniscus hiatus was noted to be increased in size (Fig. 28-22A), and although the meniscus was firmly attached to the capsule, there was increased translation in the central portion of the lateral tibiofemoral compartment. In addition, the anterior rim at the meniscocapsular junction demonstrated fraying (see Fig. 28-22B). An inside-out lateral meniscus repair was performed with eight sutures under arthroscopic control, which successfully resolved the meniscus hypermobility (see Fig. 28-22C).
The patient did well and returned to collegiate hockey without problems. Three years later, he sustained a twisting injury to the same knee and suffered a complete ACL tear and a radial lateral meniscus tear. An ACL autogenous B-PT-B reconstruction was performed. The lateral compartment demonstrated the healed prior meniscus repair in the posterior horn (see Fig. 28-22D). A new radial tear, found at the junction of the anterior and middle thirds, that extended to the capsular margin was repaired with six horizontal mattress sutures (see Fig. 28-22E). The patient recovered without complications.
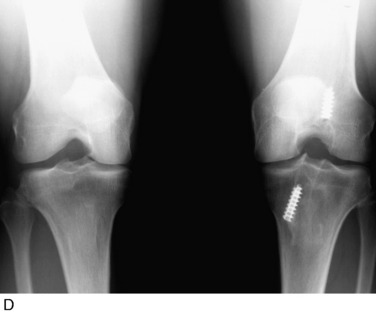
A 33-year-old man presented 1 week after a left knee injury sustained while playing basketball. Physical examination revealed 7 mm of increased anterior tibial translation and severe medial joint line tenderness. The patient had a mild effusion and 90° of knee flexion. He was referred to physical therapy for 4 weeks of rehabilitation to regain normal knee motion and muscle function. A B-PT-B ACL autograft, repair of a complex multiplanar lateral meniscus central third tear, and repair of a 15-mm single longitudinal medial meniscus central third tear were then performed (Fig. 28-23A). The patient had a chronic PCL rupture on the right knee of 12 years’ duration, which had been treated conservatively.
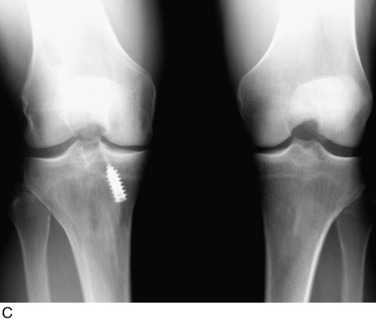
At the latest follow-up evaluation, 15 years postoperatively, the patient had no complaints with his right knee. He had participated in basketball without symptoms and rated the overall condition of his knee as normal. Physical examination demonstrated a grade I pivot shift, a full range of knee motion, and no crepitus, swelling, or joint line pain. All meniscus tests were negative. Standing PA radiographs demonstrated only 1 mm of decrease in the lateral tibiofemoral compartment joint space compared with the opposite knee and no decrease in the medial tibiofemoral compartment joint space (see Fig. 28-23B).
A 35-year-old man presented 19 years after a right ACL rupture (which had been treated conservatively) and 2 days after a left ACL and MCL injury. The left knee injury was treated with a B-PT-B ACL allograft reconstruction, medial collateral ligament primary repair, and a proximal patellar realignment. The patient recovered from this procedure well, but developed increasing instability symptoms with the right knee along with painful crepitus to the lateral tibiofemoral compartment. He underwent a right B-PT-B allograft ACL reconstruction and repair of bilateral peripheral medial (Fig. 28-24A) and lateral (see Fig. 28-24B) meniscus tears. Noteworthy fissuring and fragmentation were noted in the lateral femoral condyle, the medial femoral condyle, and on the undersurface of the patella.
At the most recent evaluation, 11 years postoperatively, the patient reported no knee pain or left knee instability. He participated in low-impact activities weekly without complaints. He had a normal range of knee motion, a grade I pivot shift test, and no joint line tenderness. Radiographs show preservation of the medial tibiofemoral joint space (see Fig. 28-24C).
A 31-year-old man presented 2 months after a twisting injury to the right knee sustained during a soccer game that had been treated elsewhere with a diagnostic arthroscopy. Physical examination revealed 10 mm of increased anterior tibial translation, moderate medial tibiofemoral joint line pain, and a mild effusion. The patient underwent a B-PT-B autogenous ACL reconstruction and a repair of a 20-mm peripheral medial meniscus tear (Fig. 28-25A). Noteworthy fissuring and fragmentation were noted on the medial femoral condyle (see Fig. 28-25B). The patient recovered and was released to full sports activities 9 months later.
At the most recent follow-up evaluation, 16 years postoperative, the patient stated he had participated in competitive soccer without symptoms or functional limitations until a reinjury that had occurred 3 months prior to his examination. He underwent a partial medial meniscectomy elsewhere. Physical examination revealed 2 mm of increased anteroposterior (AP) tibial displacement on KT-2000 testing, no crepitus, a normal range of motion, and no joint line pain. The patient rated the overall condition of his knee as very good. Radiographs demonstrated preservation of the medial tibiofemoral compartment (see Fig. 28-25C). However, the patient was warned that continued high-impact activities might accelerate medial compartment joint arthrosis with the loss of the medial meniscus and preexisting damage noted on the medial femoral condyle.
An 18-year-old male sustained a right knee injury playing basketball and presented 2 weeks later with a mild effusion, 12 mm of increased anterior tibial translation, medial joint line pain, and a nearly normal range of knee motion. He underwent a B-PT-B autogenous ACL reconstruction and bilateral meniscus repairs for double longitudinal posterior horn tears (Fig. 28-26A). There were noteworthy fissuring and fragmentation of the medial femoral condyle (see Fig. 28-26B). He recovered well and returned to basketball for several years. The patient sustained a left knee injury 5 years later and underwent an ACL reconstruction and total medial meniscectomy elsewhere.
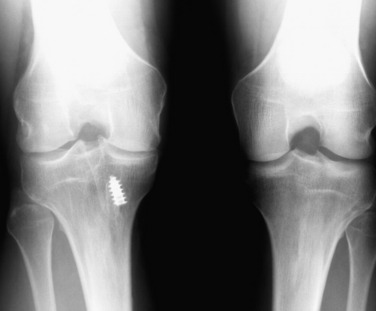
At the most recent follow-up evaluation, 14 years postoperative, the patient rated his right knee as nearly normal without symptoms. Physical examination of the right knee demonstrated a negative Lachman and pivot shift, no meniscus pathology, a full range of knee motion, and no joint effusion. The left knee was symptomatic for medial tibiofemoral compartment symptoms and had drifted into varus malalignment. Radiographs demonstrated preservation of the medial and lateral tibiofemoral compartment joint spaces in the right knee (see Fig. 28-26C), but loss of medial joint space in the left knee (see Fig. 28-26D). An opening wedge high tibial osteotomy was subsequently performed on the left knee.
At the most recent follow-up evaluation, 14 years postoperative, the patient reported no symptoms, locking, or catching and rated the overall condition of his knee as normal. Physical examination demonstrated a negative pivot shift test, 3 mm of increased AP displacement on KT-2000 testing, no tibiofemoral joint line pain or crepitus, and a normal range of knee motion. The patient had a sedentary occupation and weighed 265 pounds. Radiographs detected narrowing to the medial tibiofemoral compartment and 2° of varus alignment (Fig. 28-27). MRI revealed deterioration of the medial meniscus, with only a small remnant remaining. The patient was counseled regarding the potential for a future high tibial osteotomy based on medial tibiofemoral compartment symptoms.
The patient did well for 1 year until he developed lateral joint line pain and catching symptoms. Repeat arthroscopy demonstrated a complex medial meniscus tear extending from the posterior horn to the midbody with horizontal and vertical longitudinal components. A revision meniscus repair was successfully performed with only a small portion of the posterior horn removed. Six years later, the patient reported no problems with light recreational sports and daily activities and rated the overall condition of the knee as good. Physical examination demonstrated a normal range of knee motion, no effusion, no tibiofemoral pain or crepitus, and no meniscus symptoms. Radiographs showed preservation of the medial tibiofemoral joint space (Fig. 28-28A and B).
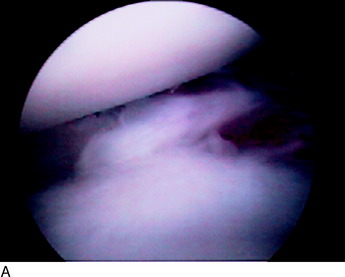
Two years later, the patient had an onset of medial joint line pain and locking. Arthroscopy demonstrated an incomplete tear to the medial meniscus along the inferior border posteriorly (Fig. 28-29A). No repair was deemed necessary. Articular cartilage damage (grade 2A) was noted on the undersurface of the patella, the medial femoral condyle, and the lateral femoral condyle. The patient continued to have a catching sensation and discomfort and underwent arthroscopy 6 months later. The medial meniscus was intact and the lateral meniscus was stable with the exception of a 3-mm radial tear, which was excised.
At the most recent follow-up evaluation, 19 years after the original bilateral meniscus repair procedure, the patient had no symptoms and rated the overall condition of his knee as very good. Physical examination revealed no effusion, a normal range of knee motion, a negative pivot shift test, no increase in AP displacement on KT-2000 testing, and no tibiofemoral joint line pain. Standing PA radiographs demonstrated excellent retention of the lateral and medial compartments of the involved knee (see Fig. 28-29B) compared with the contralateral knee (see Fig. 28-29C).
1 Adams S.B.Jr., Randolph M.A., Gill T.J. Tissue engineering for meniscus repair. J Knee Surg. 2005;18:25-30.
2 Ahmed A.M., Burke D.L. In-vitro measurement of static pressure distribution in synovial joints—part I: tibial surface of the knee. J Biomech Eng. 1983;105:216-225.
3 Albrecht-Olsen P., Kristensen G., Burgaard P., et al. The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7:268-273.
4 Albrecht-Olsen P., Lind T., Kristensen G., Falkenberg B. Failure strength of a new meniscus arrow repair technique: biomechanical comparison with horizontal suture. Arthroscopy. 1997;13:183-187.
5 Albrecht-Olsen P.M., Bak K. Arthroscopic repair of the bucket-handle meniscus. 10 failures in 27 stable knees followed for 3 years. Acta Orthop Scand. 1993;64:446-448.
6 Andersson-Molina H., Karlsson H., Rockborn P. Arthroscopic partial and total meniscectomy: a long-term follow-up study with matched controls. Arthroscopy. 2002;18:183-189.
7 Arnoczky S.P., Warren R.F. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90-95.
8 Arnoczky S.P., Warren R.F. The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med. 1983;11:131-141.
9 Asahina S., Muneta T., Hoshino A., et al. Intermediate-term results of meniscal repair in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 1998;26:688-691.
10 Asahina S., Muneta T., Yamamoto H. Arthroscopic meniscal repair in conjunction with anterior cruciate ligament reconstruction: factors affecting the healing rate. Arthroscopy. 1996;12:541-545.
11 Asik M., Sen C., Erginsu M. Arthroscopic meniscal repair using T-fix. Knee Surg Sports Traumatol Arthrosc. 2002;10:284-288.
12 Asik M., Sener N. Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc. 2002;10:25-29.
13 Asik M., Sener N., Akpinar S., et al. Strength of different meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc. 1997;5:80-83.
14 Barber F.A., Coons D.A. Midterm results of meniscal repair using the BioStinger meniscal repair device. Arthroscopy. 2006;22:400-405.
15 Barber F.A., Coons D.A., Ruiz-Suarez M. Meniscal repair with the RapidLoc meniscal repair device. Arthroscopy. 2006;22:962-966.
16 Barber F.A., Herbert M.A. Meniscal repair devices. Arthroscopy. 2000;16:613-618.
17 Barber F.A., Herbert M.A., Richards D.P. Load to failure testing of new meniscal repair devices. Arthroscopy. 2004;20:45-50.
18 Barber F.A., Johnson D.H., Halbrecht J.L. Arthroscopic meniscal repair using the BioStinger. Arthroscopy. 2005;21:744-750.
19 Barber-Westin S.D., Noyes F.R., McCloskey J.W. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati Knee Rating System in 350 subjects with uninjured, injured, or anterior cruciate ligament–reconstructed knees. Am J Sports Med. 1999;27:402-416.
20 Barrett G.R., Treacy S.H., Ruff C.G. Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population. Arthroscopy. 1997;13:218-223.
21 Becker R., Starke C., Heymann M., Nebelung W. Biomechanical properties under cyclic loading of seven meniscus repair techniques. Clin Orthop Relat Res. 2002;400:236-245.
22 Bhargava M.M., Hidaka C., Hannafin J.A., et al. Effects of hepatocyte growth factor and platelet-derived growth factor on the repair of meniscal defects in vitro. In Vitro Cell Dev Biol Anim. 2005;41:305-310.
23 Billante M.J., Diduch D.R., Lunardini D.J., et al. Meniscal repair using an all-inside, rapidly absorbing, tensionable device. Arthroscopy. 2008;24:779-785.
24 Boenisch U.W., Faber K.J., Ciarelli M., et al. Pull-out strength and stiffness of meniscal repair using absorbable arrows or Ti-Cron vertical and horizontal loop sutures. Am J Sports Med. 1999;27:626-631.
25 Borden P., Nyland J., Caborn D.N., Pienkowski D. Biomechanical comparison of the FasT-Fix meniscal repair suture system with vertical mattress sutures and meniscus arrows. Am J Sports Med. 2003;31:374-378.
26 Bourne R.B., Finlay J.B., Papadopoulos P., Andreae P. The effect of medial meniscectomy on strain distribution in the proximal part of the tibia. J Bone Joint Surg Am. 1984;66:1431-1437.
27 Boytim M.J., Smith J.P., Fischer D.A., Quick D.C. Arthroscopic posteromedial visualization of the knee. Clin Orthop Relat Res. 1995;310:82-86.
28 Bryant D., Dill J., Litchfield R., et al. Effectiveness of bioabsorbable arrows compared with inside-out suturing for vertical, reparable meniscal lesions: a randomized clinical trial. Am J Sports Med. 2007;35:889-896.
29 Bullough P.G., Munuera L., Murphy J., Weinstein A.M. The strength of the menisci of the knee as it relates to their fine structure. J Bone Joint Surg Br. 1970;52:564-570.
30 Buma P., Ramrattan N.N., van Tienen T.G., Veth R.P. Tissue engineering of the meniscus. Biomaterials. 2004;25:1523-1532.
31 Buseck M.S., Noyes F.R. Arthroscopic evaluation of meniscal repairs after anterior cruciate ligament reconstruction and immediate motion. Am J Sports Med. 1991;19:489-494.
32 Calder S.J., Myers P.T. Broken arrow: a complication of meniscal repair. Arthroscopy. 1999;15:651-652.
33 Cannon W.D.Jr., Vittori J.M. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament–reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176-181.
34 Caplan A.I. Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J Cell Physiol. 2007;213:341-347.
35 DeHaven K.E., Arnoczky S.P. Meniscal repair. Part I: basic science, indications for repair, and open repair. J Bone Joint Surg Am. 1994;76:140-152.
36 DeHaven K.E., Lohrer W.A., Lovelock J.E. Long-term results of open meniscal repair. Am J Sports Med. 1995;23:524-530.
37 Dervin G.F., Downing K.J., Keene G.C., McBride D.G. Failure strengths of suture versus biodegradable arrow for meniscal repair: an in vitro study. Arthroscopy. 1997;13:296-300.
38 Dugdale T.W., Noyes F.R., Styer D. Preoperative planning for high tibial osteotomy: The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248-264.
39 Ellermann A., Siebold R., Buelow J.U., Sobau C. Clinical evaluation of meniscus repair with a bioabsorbable arrow: a 2- to 3-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2002;10:289-293.
40 Evans C.H., Ghivizzani S.C., Robbins P.D. The 2003 Nicolas Andry Award. Orthopaedic gene therapy. Clin Orthop Relat Res. 2004;429:316-329.
41 Fairbank F.J. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664-670.
42 Farng E., Sherman O. Meniscal repair devices: a clinical and biomechanical literature review. Arthroscopy. 2004;20:273-286.
43 Fisher S.R., Markel D.C., Koman J.D., Atkinson T.S. Pull-out and shear failure strengths of arthroscopic meniscal repair systems. Knee Surg Sports Traumatol Arthrosc. 2002;10:294-299.
44 Fox M.G. MR imaging of the meniscus: review, current trends, and clinical implications. Radiol Clin North Am. 2007;45:1033-1053. vii
45 Fukubayashi T., Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51:871-879.
46 Gershuni D.H., Skyhar M.J., Danzig L.A., et al. Experimental models to promote healing of tears in the avascular segment of canine knee menisci. J Bone Joint Surg Am. 1989;71:1363-1370.
47 Ghadially F.N., Wedge J.H., LaLonde J.-M. Experimental methods of repairing injured menisci. J Bone Joint Surg Br. 1986;68:106-110.
48 Haas A.L., Schepsis A.A., Hornstein J., Edgar C.M. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005;21:167-175.
49 Hashimoto J., Kurosaka M., Yoshiya S., Hirohata K. Meniscal repair using fibrin sealant and endothelial cell growth factor. An experimental study in dogs. Am J Sports Med. 1992;20:537-541.
50 Heatley F.W. The meniscus-can it be repaired? An experimental investigation in rabbits. J Bone Joint Surg Br. 1980;62:397-402.
51 Henning C.E., Lynch M.A., Clark J.R. Vascularity for healing of meniscus repairs. Arthroscopy. 1987;3:13-18.
52 Henning C.E., Lynch M.A., Yearout K.M., et al. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res. 1990;252:64-72.
53 Hoben G.M., Athanasiou K.A. Creating a spectrum of fibrocartilages through different cell sources and biochemical stimuli. Biotechnol Bioeng. 2008;100:587-598.
54 Hoben G.M., Athanasiou K.A. Meniscal repair with fibrocartilage engineering. Sports Med Arthrosc. 2006;14:129-137.
55 Horibe S., Shino K., Maeda A., et al. Results of isolated meniscal repair evaluated by second-look arthroscopy. Arthroscopy. 1996;12:150-155.
56 Hoshikawa Y., Kuroswa H., Fukubayashi T., et al. The prognosis of meniscectomy in athletes. The simple meniscus lesions without ligamentous instabilities. Am J Sports Med. 1983;11:8-13.
57 Hurel C., Mertens F., Verdonk R. Biofix resorbable meniscus arrow for meniscal ruptures: results of a 1-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8:46-52.
58 Hutchinson M.R., Ash S.A. Failure of a biodegradable meniscal arrow. A case report. Am J Sports Med. 1999;27:101-103.
59 Ishimura M., Ohgushi H., Habata T., et al. Arthroscopic meniscal repair using fibrin glue. Part I: experimental study. Arthroscopy. 1997;13:551-557.
60 Jensen N.C., Riis J., Robertsen K., Holm A.R. Arthroscopic repair of the ruptured meniscus: one to 6.3 years follow-up. Arthroscopy. 1994;10:211-214.
61 Johns D.E., Athanasiou K.A. Growth factor effects on costal chondrocytes for tissue engineering fibrocartilage. Cell Tissue Res. 2008;333:439-447.
62 Johnson R.J., Kettelkamp D.B., Clark W., Leaverton P. Factors affecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56:719-729.
63 Jorgensen U., Sonne-Holm S., Lauridsen F., Rosenklint A. Long-term follow-up of meniscectomy in athletes. A prospective longitudinal study. J Bone Joint Surg Br. 1987;69:80-83.
64 Kalliakmanis A., Zourntos S., Bousgas D., Nikolaou P. Comparison of arthroscopic meniscal repair results using 3 different meniscal repair devices in anterior cruciate ligament reconstruction patients. Arthroscopy. 2008;24:810-816.
65 Kelly B.T., Potter H.G., Deng X.H., et al. Meniscal allograft transplantation in the sheep knee: evaluation of chondroprotective effects. Am J Sports Med. 2006;34:1464-1477.
66 Kettelkamp D.B., Jacobs A.W. Tibiofemoral contact area—determination and implications. J Bone Joint Surg Am. 1972;54:349-356.
67 Kocabey Y., Nyland J., Isbell W.M., Caborn D.N. Patient outcomes following T-Fix meniscal repair and a modifiable, progressive rehabilitation program, a retrospective study. Arch Orthop Trauma Surg. 2004;124:592-596.
68 Kotsovolos E.S., Hantes M.E., Mastrokalos D.S., et al. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy. 2006;22:3-9.
69 Krych A.J., McIntosh A.L., Voll A.E., et al. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36:1283-1289.
70 Kurosaka M., Yoshiya S., Kuroda R., et al. Repeat tears of repaired menisci after arthroscopic confirmation of healing. J Bone Joint Surg Br. 2002;84:34-37.
71 Kurosawa H., Fukubayashi T., Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. 1980;149:283-290.
72 Kurzweil P.R., Tifford C.D., Ignacio E.M. Unsatisfactory clinical results of meniscal repair using the meniscus arrow. Arthroscopy. 2005;21:905.
73 LaPrade R.F., Konowalchuk B.K. Popliteomeniscal fascicle tears causing symptomatic lateral compartment knee pain: diagnosis by the figure-4 test and treatment by open repair. Am J Sports Med. 2005;33:1231-1236.
74 Lee G.P., Diduch D.R. Deteriorating outcomes after meniscal repair using the meniscus arrow in knees undergoing concurrent anterior cruciate ligament reconstruction: increased failure rate with long-term follow-up. Am J Sports Med. 2005;33:1138-1141.
75 Lee S.J., Aadalen K.J., Malaviya P., et al. Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med. 2006;34:1334-1344.
76 Levy A.S., Meier S.W. Approach to cartilage injury in the anterior cruciate ligament–deficient knee. Orthop Clin North Am. 2003;34:149-167.
77 Levy I.M., Torzilli P.A., Warren R.F. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883-888.
78 Lozano J., Ma C.B., Cannon W.D. All-inside meniscus repair: a systematic review. Clin Orthop Relat Res. 2007;455:134-141.
79 Lynch M.A., Henning C.E., Glick K.R.Jr. Knee joint surface changes. Long-term follow-up meniscus tear treatment in stable anterior cruciate ligament reconstructions. Clin Orthop Relat Res. 1983;172:148-153.
80 Majewski M., Stoll R., Widmer H., et al. Midterm and long-term results after arthroscopic suture repair of isolated, longitudinal, vertical meniscal tears in stable knees. Am J Sports Med. 2006;34:1072-1076.
81 Mariani P.P., Santori N., Adriani E., Mastantuono M. Accelerated rehabilitation after arthroscopic meniscal repair: a clinical and magnetic resonance imaging evaluation. Arthroscopy. 1996;12:680-686.
82 Markolf K.L., Bargar W.L., Shoemaker S.C., Amstutz H.C. The role of joint load in knee stability. J Bone Joint Surg Am. 1981;63:570-585.
83 McDermott I.D., Lie D.T., Edwards A., et al. The effects of lateral meniscal allograft transplantation techniques on tibio-femoral contact pressures. Knee Surg Sports Traumatol Arthrosc. 2008;16:553-560.
84 McMurray T.P. The semilunar cartilages. Br J Surg. 1942;29:407.
85 McNicholas M.J., Rowley D.I., McGurty D., et al. Total meniscectomy in adolescence. A thirty-year follow-up. J Bone Joint Surg Br. 2000;82:217-221.
86 Menche D.S., Phillips G.I., Pitman M.I., Steiner G.C. Inflammatory foreign-body reaction to an arthroscopic bioabsorbable meniscal arrow repair. Arthroscopy. 1999;15:770-772.
87 Menetrey J., Seil R., Rupp S., Fritschy D. Chondral damage after meniscal repair with the use of a bioabsorbable implant. Am J Sports Med. 2002;30:896-899.
88 Miller M.D., Kline A.J., Jepsen K.G. All-inside” meniscal repair devices: an experimental study in the goat model. Am J Sports Med. 2004;32:858-862.
89 Miller M.D., Ritchie J.R., Gomez B.A., et al. Meniscal repair. An experimental study in the goat. Am J Sports Med. 1995;23:124-128.
90 Mintzer C.M., Richmond J.C., Taylor J. Meniscal repair in the young athlete. Am J Sports Med. 1998;26:630-633.
91 Morgan C.D., Wojtys E.M., Casscells C.D., Casscells S.W. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991;19:632-637. discussion 637–638
92 Mow V.C., Ratcliffe A., Chern K.Y., Kelly M.A. Structure and function relationships of the menisci of the knee. In: Mow V.C., Arnoczky S.P., Jackson D.W., editors. Knee Meniscus: Basic and Clinical Foundations. New York: Raven; 1992:37-57.
93 Nakhostine M., Gershuni D.H., Danzig L.A. Effects of an insubstance conduit with injection of a blood clot on tears in the avascular region of the meniscus. Acta Orthop Belg. 1991;57:242-246.
94 Newman A.P., Anderson D.R., Daniels A.U., Dales M.C. Mechanics of the healed meniscus in a canine model. Am J Sports Med. 1989;17:164-175.
95 Nourissat G., Beaufils P., Charrois O., et al. Magnetic resonance imaging as a tool to predict reparability of longitudinal full-thickness meniscus lesions. Knee Surg Sports Traumatol Arthrosc. 2008;16:482-486.
96 Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears extending into the avascular zone in patients younger than twenty years of age. Am J Sports Med. 2002;30:589-600.
97 Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16:822-829.
98 Noyes F.R., Bassett R.W., Grood E.S., Butler D.L. Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am. 1980;62:687-695. 757
99 Noyes F.R., Stabler C.L. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med. 1989;17:505-513.
100 Nyland J., Chang H., Kocabey Y., et al. A cyclic testing comparison of FasT-Fix and RapidLoc devices in human cadaveric meniscus. Arch Orthop Trauma Surg. 2008;128:489-494.
101 O’Shea J.J., Shelbourne K.D. Repair of locked bucket-handle meniscal tears in knees with chronic anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:216-220.
102 Oliverson T.J., Lintner D.M. Biofix arrow appearing as a subcutaneous foreign body. Arthroscopy. 2000;16:652-655.
103 Paletta G.A., Manning T., Snell E., et al. The effect of allograft meniscal replacement on intra-articular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med. 1997;25:692-698.
104 Pena E., Calvo B., Martinez M.A., et al. Finite element analysis of the effect of meniscal tears and meniscectomies on human knee biomechanics. Clin Biomech (Bristol, Avon). 2005;20:498-507.
105 Peretti G.M., Gill T.J., Xu J.W., et al. Cell-based therapy for meniscal repair: a large animal study. Am J Sports Med. 2004;32:146-158.
106 Post W.R., Akers S.R., Kish V. Load to failure of common meniscal repair techniques: effects of suture technique and suture material. Arthroscopy. 1997;13:731-736.
107 Potter H.G., Linklater J.M., Allen A.A., et al. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276-1284.
108 Potter H.G., Rodeo S.A., Wickiewicz T.L., Warren R.F. Imaging of meniscal allografts: correlation with clinical and arthroscopic outcomes. Radiology. 1996;198:509-514.
109 Quinby J.S., Golish S.R., Hart J.A., Diduch D.R. All-inside meniscal repair using a new flexible, tensionable device. Am J Sports Med. 2006;34:1281-1286.
110 Rankin C.C., Lintner D.M., Noble P.C., et al. A biomechanical analysis of meniscal repair techniques. Am J Sports Med. 2002;30:492-497.
111 Rimmer M.G., Nawana N.S., Keene G.C.R., Pearcy M.J. Failure strengths of different meniscal suturing techniques. Arthroscopy. 1995;11:146-150.
112 Ritchie J.R., Miller M.D., Bents R.T., Smith D.K. Meniscal repair in the goat model. The use of healing adjuncts on central tears and the role of magnetic resonance arthrography in repair evaluation. Am J Sports Med. 1998;26:278-284.
113 Rockborn P., Gillquist J. Results of open meniscus repair. Long-term follow-up study with a matched uninjured control group. J Bone Joint Surg Br. 2000;82:494-498.
114 Rockborn P., Messner K. Long-term results of meniscus repair and meniscectomy: a 13-year functional and radiographic follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:2-10.
115 Rodeo S.A. Arthroscopic meniscal repair with use of the outside-in technique. J Bone Joint Surg Am. 2000;82:127-141.
116 Rodkey W.G., Steadman J.R., Li S.-T. A clinical study of collagen meniscus implants to restore the injured meniscus. Clin Orthop Relat Res. 1999;367(Suppl):S281-S292.
117 Roeddecker K., Muennich U., Nagelschmidt M. Meniscal healing: A biomechanical study. J Surg Res. 1994;56:20-27.
118 Roos E.M., Ostenberg A., Roos H., et al. Long-term outcome of meniscectomy: symptoms, function, and performance tests in patients with or without radiographic osteoarthritis compared to matched controls. Osteoarthritis Cartilage. 2001;9:316-324.
119 Roos H., Lauren M., Adalberth T., et al. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41:687-693.
120 Rosenberg T.D., Scott S.M., Coward D.B., et al. Arthroscopic meniscal repair evaluated with repeat arthroscopy. Arthroscopy. 1986;2:14-20.
121 Rubman M.H., Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med. 1998;26:87-95.
122 Scheller G., Sobau C., Bulow J.U. Arthroscopic partial lateral meniscectomy in an otherwise normal knee: clinical, functional, and radiographic results of a long-term follow-up study. Arthroscopy. 2001;17:946-952.
123 Scott G.A., Jolly B.L., Henning C.E. Combined posterior incision and arthroscopic intra-articular repair of the meniscus: an examination of factors affecting healing. J Bone Joint Surg Am. 1986;68:847-861.
124 Seedhom B.B., Hargreaves D.J. Transmission of the load in the knee joint with special reference to the role of the menisci. Part II. Experimental results, discussion, and conclusions. Eng Med. 1979;8:220-228.
125 Siebold R., Dehler C., Boes L., Ellermann A. Arthroscopic all-inside repair using the Meniscus Arrow: long-term clinical follow-up of 113 patients. Arthroscopy. 2007;23:394-399.
126 Song E.K., Lee K.B. Biomechanical test comparing the load to failure of the biodegradable meniscus arrow versus meniscal suture. Arthroscopy. 1999;15:726-732.
127 Spindler K.P., McCarty E.C., Warren T.A., et al. Prospective comparison of arthroscopic medial meniscal repair technique: inside-out suture versus entirely arthroscopic arrows. Am J Sports Med. 2003;31:929-934.
128 Steenbrugge F., Verdonk R., Hurel C., Verstraete K. Arthroscopic meniscus repair: inside-out technique vs. Biofix meniscus arrow. Knee Surg Sports Traumatol Arthrosc. 2004;12:43-49.
129 Steinert A.F., Palmer G.D., Capito R., et al. Genetically enhanced engineering of meniscus tissue using ex vivo delivery of transforming growth factor-beta 1 complementary deoxyribonucleic acid. Tissue Eng. 2007;13:2227-2237.
130 Stone K.R., Rodkey W.G., Webber R., et al. Meniscal regeneration with copolymeric collagen scaffolds. In vitro and in vivo studies evaluated clinically, histologically, and biochemically. Am J Sports Med. 1992;20:104-111.
131 Sweigart M.A., Athanasiou K.A. Toward tissue engineering of the knee meniscus. Tissue Eng. 2001;7:111-129.
132 Szomor Z.L., Martin T.E., Bonar F., Murrell G.A. The protective effects of meniscal transplantation on cartilage. An experimental study in sheep. J Bone Joint Surg Am. 2000;82:80-88.
133 Tapper E.M., Hoover N.W. Late results after meniscectomy. J Bone Joint Surg Am. 1969;51:517-526. passim
134 Tenuta J.J., Arciero R.A. Arthroscopic evaluation of meniscal repairs. Factors that affect healing. Am J Sports Med. 1994;22:797-802.
135 Thompson W.O., Thaete F.L., Fu F.H., Dye S.F. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19:210-216.
136 Tingstad E.M., Teitz C.C., Simonian P.T. Complications associated with the use of meniscal arrows. Am J Sports Med. 2001;29:96-98.
137 Tumia N.S., Johnstone A.J. Promoting the proliferative and synthetic activity of knee meniscal fibrochondrocytes using basic fibroblast growth factor in vitro. Am J Sports Med. 2004;32:915-920.
138 Tumia N.S., Johnstone A.J. Regional regenerative potential of meniscal cartilage exposed to recombinant insulin-like growth factor-I in vitro. J Bone Joint Surg Br. 2004;86:1077-1081.
139 Verma N.N., Kolb E., Cole B.J., et al. The effects of medial meniscal transplantation techniques on intra-articular contact pressures. J Knee Surg. 2008;21:20-26.
140 Veth R.P.H. Clinical significance of knee joint changes after meniscectomy. Clin Orthop Relat Res. 1985;198:56-60.
141 Voloshin A.S., Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng. 1983;5:157-161.
142 von Engelhardt L.V., Schmitz A., Pennekamp P.H., et al. Diagnostics of degenerative meniscal tears at 3-Tesla MRI compared to arthroscopy as reference standard. Arch Orthop Trauma Surg. 2008;128:451-456.
143 Walsh S.P., Evans S.L., O’Doherty D.M., Barlow I.W. Failure strengths of suture vs. biodegradable arrow and staple for meniscal repair: an in vitro study. Knee. 2001;8:151-156.
144 Webber R.J., Harris M.G., Hough A.J. Cell culture of rabbit meniscal fibrochondrocytes: proliferative and synthetic response to growth factors and ascorbate. J Orthop Res. 1985;3:36-42.
145 Wilson W., van Rietbergen B., van Donkelaar C.C., Huiskes R. Pathways of load-induced cartilage damage causing cartilage degeneration in the knee after meniscectomy. J Biomech. 2003;36:845-851.
146 Yao J., Lancianese S.L., Hovinga K.R., et al. Magnetic resonance image analysis of meniscal translation and tibio-menisco-femoral contact in deep knee flexion. J Orthop Res. 2008;26:673-684.
147 Zantop T., Eggers A.K., Weimann A., et al. Initial fixation strength of flexible all-inside meniscus suture anchors in comparison to conventional suture technique and rigid anchors: biomechanical evaluation of new meniscus refixation systems. Am J Sports Med. 2004;32:863-869.
148 Zantop T., Ruemmler M., Welbers B., et al. Cyclic loading comparison between biodegradable interference screw fixation and biodegradable double cross-pin fixation of human bone-patellar tendon-bone grafts. Arthroscopy. 2005;21:934-941.
149 Zhang Z., Arnold J.A., Williams T., McCann B. Repairs by trephination and suturing of longitudinal injuries in the avascular area of the meniscus in goats. Am J Sports Med. 1995;23:35-41.
150 Zhang Z.N., Tu K.Y., Xu Y.K., et al. Treatment of longitudinal injuries in avascular area of meniscus in dogs by trephination. Arthroscopy. 1988;4:151-159.
* See references 6, 41, 56, 62, 63, 79, 85, 114, 118, 119, 122, 133, 140.
* See references 4, 16, 17, 24, 25, 37, 43, 88, 126, 143, 147, 148.
* See references 22, 49, 53, 54, 59, 61, 105, 129, 137, 138.
* See references 3, 9–11, 14, 15, 18, 20, 23, 28, 36, 39, 48, 55, 67–70, 72, 74, 80, 81, 90, 101, 109, 113, 115, 125, 127, 128.
* See references 6, 41, 56, 62, 63, 79, 85, 114, 118, 119, 122, 133, 140.