CHAPTER 6 Meniscal Resection
ANATOMY
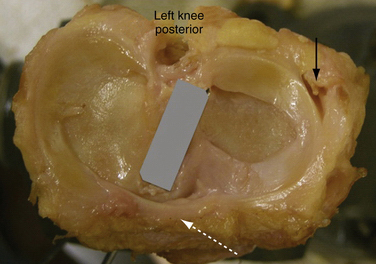
Menisci are discs of fibrocartilage interposed between the femoral condyles and tibial plateau. The articular surface of the medial condyle of the tibia is oval, with the longer axis being in the anteroposterior plane (Fig. 6-1). The central portion of the articular surface is not covered by meniscus and represents the articular area. The lateral meniscus plateau is almost circular and less concave. The menisci cover the peripheral two thirds of the tibia, and serve to deepen its articular surface and stabilize the joint. The upper borders of the menisci are concave and the undersurfaces are flat. Peripherally, the menisci thicken and are attached to the synovium and capsule. Centrally, the border is thin and exists as a free edge.
The medial meniscus is oval, 3.5cm in length, and wider posteriorly from its peripheral to its central aspects in the knee. Its anterior horn attaches to the tibial plateau just anterior to the attachment of the ACL. Some posterior fibers originating from the anterior horn cross the knee joint anteriorly, attaching to the lateral meniscus and forming the transverse ligament (see Fig. 6-1). Posteriorly, the meniscus is anchored to the intercondylar fossa of the tibia between the posterior cruciate ligament (PCL) and lateral meniscal attachment. Along its periphery, the medial meniscus is attached to the joint capsule and the deep medial collateral ligament (MCL). The medial meniscus has less mobility than the lateral meniscus, and moves almost 10 mm from extension to flexion.
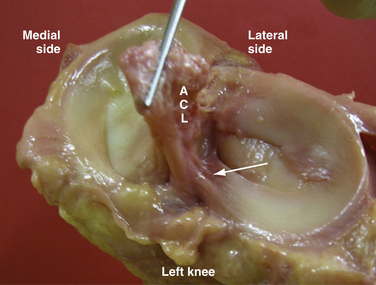
The lateral meniscus is circular, covering a larger portion of the articular surface than its medial counterpart. It is the same width anteriorly and posteriorly. The anterior horn attaches near the intercondylar spine posterior to the attachment of the ACL, with which it partially blends (Fig. 6-2). The posterior horn attaches just posteriorly to the intercondylar spines, anterior to the attachment of the medial meniscus. The lateral meniscus does not attach to the lateral collateral ligament but is attached loosely to synovium along much of its length. The anterior (ligament of Humphrey) and posterior (ligament of Wrisberg) meniscofemoral ligaments run from the posterior horn of the lateral meniscus to anterior and posterior, respectively, to the PCL attachment on the medial femoral condyle. Moreover, the tendon of the popliteus muscle, on its way to insert into the lateral condyle, crosses the joint through a hole on the lateral meniscus called the hiatus popliteus (see Fig. 6-1). This area along the popliteal hiatus is described as the avascular region.
Biomechanics and Meniscal Function
A complete meniscectomy has been shown to decrease the contact area by approximately 50%.1 A partial or total meniscectomy has been clinically demonstrated to result in degenerative changes in the knee.2 This has been postulated to result from the increase in contact pressures in the knee. Even a minor meniscectomy, removing 15% to 34% of the meniscus, increases contact pressures in the knee by up to 350% and can result in degenerative changes. In meniscectomized knees, a significant reduction in contact area of about 55% is observed, and peak contact pressures increase an average of 260.4% compared with those of nonmeniscectomized knees.3
Knee joint stability is enhanced by the menisci in a similar manner to the glenoid or acetabular labrum. The intact meniscus serves as a secondary restraint to anteroposterior knee motion.4 The ACL-deficient knee can place abnormal stress on an intact medial meniscus, resulting in a meniscal tear. The increased anteroposterior motion created by meniscectomy in the ACL-deficient knee can lead to increased instability.
Regenerative Capacity of the Meniscus
King’s 1936 experiment on a canine model represents the historical origin of the interest in meniscal healing.5 Later experimentation demonstrated the necessity of a peripheral blood supply to support the inflammatory cascade required for meniscal healing.6
Studies have shown that when a radial tear extends into the synovium, it can heal spontaneously by 10 weeks.7 The strength of this tissue is 33% normal at 8 weeks, 52% at 4 months, and 62% at 6 months. It is this inherent healing ability of the meniscus that clinical initiatives exploit in efforts to preserve as much meniscal tissue as possible.
CLASSIFICATION
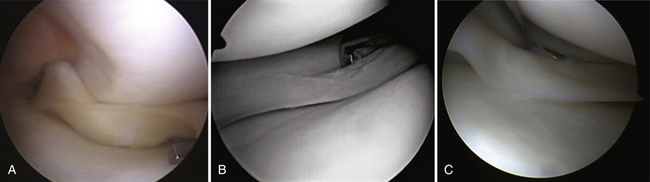
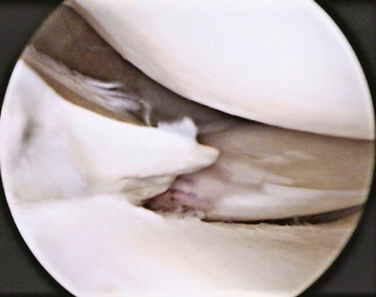
In addition, meniscal tears can be classified depending on their stability (Box 6-1). A tear is considered unstable when it is more than half the length of the meniscus and subluxes under the femoral condyle when probed with a hook (Fig. 6-3A). This concept is especially important to help decide the treatment options—left alone, trephinated, resected, or repaired.
Stable tears, which occur particularly in the posterior aspect of the meniscus and do not subluxate into the joint may be left alone (see Fig. 6-3B and C). Fitzgibbons and Shelbourne8 have found that of 189 patients whose stable meniscal tears of the posterior horn of the medial meniscus were left alone, no patient was symptomatic at 2.6 years following surgery. Also, a stable longitudinal tear of the lateral meniscus, posterior to the popliteus, may be left alone, even in association with a torn ACL.
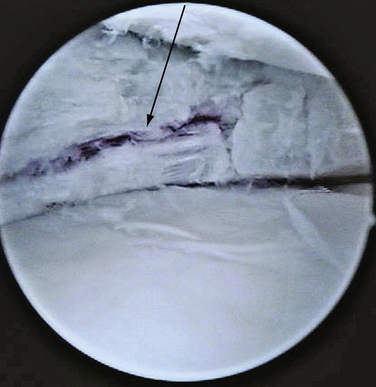
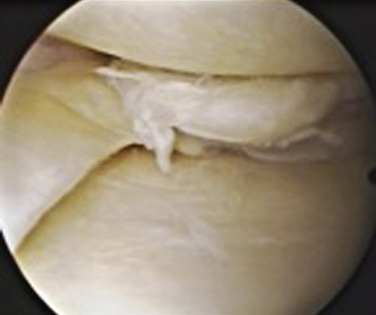
Tears can be described depending on their morphology and based on their configuration. Under these criteria, tears could be vertical or horizontal, according to whether the line of the lesion goes from superior to inferior (vertical) or from inside to outside (horizontal), commonly called open book or fishmouth tear (Fig. 6-4). Moreover, tears can be described as longitudinal if the pattern is from anterior to posterior (Fig. 6-5; also see Fig. 6-3), or transverse, also called a radial or parrot beak tear (Fig. 6-6). Combinations of these four basic patterns make up the others types of tears; the oblique tear is vertical and radial, and the so-called bucket handle tear is a vertical longitudinal tear that is unstable and subluxes completely under the condyle (Fig. 6-7; also see Fig. 6-3A). Finally, the complex tear is a combination of all of these, usually in a degenerative setting, located in the posterior horn of the medial meniscus (Fig. 6-8).
Horizontal-shaped tears usually begin as intrasubstance degeneration in the middle of the meniscus, and migrate toward the free surface. Often, they also extend to the capsular junction and can cause the formation of a cyst. Because of the increasing size of the cyst over time, the patient may experience pain and tenderness. They usually appear more frequently in the lateral meniscus and are filled with a gel-like substance chemically similar to synovial fluid. These cysts have been reported to be 1% to 10% of meniscal pathology.9
Complex tears appear mainly in older patients and are usually associated with cartilage degeneration. They are considered to be part of the process of arthrosis and degenerative arthropathy. Because of their complex pattern, the fragments can be unstable and cause mechanical symptoms. The pain associated with these tears is an added element to the generalized inflammation involved in the osteoarthritic knee. The associated histologic pathology is myxoid degeneration, hyaline acellular degeneration, and dystrophic calcification.10
Finally, tears can be classified depending on the side—that is, the medial or lateral meniscus. Metcalf and colleagues11 have observed that 69% of tears affected the medial meniscus, whereas the lateral was affected 24% of the time. In their review, both menisci were torn at the same time in 7% of patients. Moreover, 80% of the tears were vertical or oblique and affected the posterior medial part of the meniscus.
PATIENT EVALUATION
Physical Examination
The patient is examined for signs of an effusion, loss of quadriceps bulk, and decreased range of motion. Tenderness to palpation along the medial or lateral joint line is among the most sensitive signs of a meniscal tear (Fig. 6-9A). Studies have shown it to be as sensitive as 74%, with a positive predictive value of 50%.12 The collateral and cruciate ligaments need to be assessed to determine whether additional injury is present. In the setting of an ACL-deficient knee the sensitivity of joint line tenderness has been shown to decrease to approximately 50%.
The McMurray test is preferred because it is easy, fast, and reliable. In addition, complementary knee tests may be done in the same position. This provocative test is performed with the patient supine, the hip flexed to 90 degrees, and the knee in forced maximal flexion. The foot is grasped by the heel, the knee is steadied, and the joint line is palpated with the other hand. As the knee is slowly brought into extension, an external rotation stress will test the medial meniscus and an internal rotation stress will test the lateral meniscus (see Fig. 6-9B). As a mnemonic rule, the heel of the foot points toward the injured meniscus. The test is considered positive when the patient feels pain in the appropriate joint line, accompanied by a thud or click. When the clunk is present, the test has a sensitivity of 98% but, because it is not always possible to evoke the clunk, its specificity is only 15%.13
In conclusion, the hallmarks of a meniscal tear are presence of an effusion, joint line tenderness, and a positive McMurray test. When the history and physical examination are considered together, the overall sensitivity to diagnose a meniscal tear, confirmed with arthroscopy, is approximately 95% and specificity is 88%.14
Diagnostic Imaging
Evaluation of the patient with a meniscal tear should include routine anteroposterior (AP) and lateral x-rays of the knee. If degenerative changes are expected, standing views, including a 45-degree flexion AP view, should be obtained to assess the degree of joint space narrowing. Assessing osteoarthritis is important to counsel the patient about expectations of success. It has been proven that the degree of arthrosis before surgery correlates with worse postoperative results in the short- and long-term periods.15,16
Although not clinically indicated for all patients, magnetic resonance imaging (MRI) plays a valuable role in the evaluation of the full range of meniscal pathology, including the primary diagnosis of a meniscal tear, detection of a recurrent tear after resection or repair, and demonstration of associated injuries. MRI shows the relative locations of the tears, and is able to determine the presence of a meniscal tear with an accuracy of over 90%.17 These results indicate that MRI is an accurate noninvasive technique for evaluating meniscal tears.
Image results should be combined with pertinent history and physical examination. It has been proven that meniscal tears in young adults can be completely asymptomatic.18 In these cases, MRI may modify the therapeutic plan. For example, if an athlete suffers an ACL during the season and the MRI demonstrates no tear, one may be inclined to let the athlete finish the season with a brace. If there is a meniscal tear associated with the ACL tear, the preference would be for early reconstruction.
TREATMENT
Indications and Contraindications
Meniscectomy is indicated when the type of tear has no chance to heal spontaneously or repair is not possible. Although technology is improving and the indications for repair are increasing, arthroscopic partial meniscectomy is currently still indicated in 80% of tears (Table 6-1).
TABLE 6-1 Indications for Meniscectomy: Situations in Which Meniscectomy Is Preferred Over Repair
| Factor | Features |
|---|---|
| Meniscal Tear Factors | |
| Location | White-white |
| Morphology | |
In terms of location, according to Arnoczky and Warren,6 tears in the white-white zone have a low degree of vascularity and their chances of healing are very low. These are usually resected. If the tear is in the white-red zone, other factors should be considered to make a decision.
Several patient factors can modify the decision. In terms of age, there may be less vascularity and cellularity in the older meniscus, and thus less healing potential. The older patient often has this type of degenerative tear that is nonreparable. There is no age limit to a meniscus repair, but most surgeons would favor meniscectomy over repair in patients older than 40 years.
Arthroscopic Technique
If the patient continues to have pain, swelling, and locking or catching symptoms, and is willing to undergo surgical treatment, operative intervention is indicated. There are several surgical principles that should be followed to achieve a good outcome (Box 6-2). First, and following the Hippocratic principle of primum non nocere (“First, do no harm”), do not make the situation worse. If there is a stable, partial or total, vertical tear in a young patient, it should be left alone, and no resection is needed. Second, portal placement should be accurate enough to allow good visualization of the entire meniscus and tear configuration. In addition, portals should allow instruments of desired shapes to be introduced without scuffing the articular surface. Third, when resection is performed, the main objective is to achieve a stable peripheral rim and remove any unstable fragments that could cause mechanical symptoms or pain. During meniscectomy, it is important to contour the edges to have a smooth border and avoid progression to a second tear. The probe should be used continuously to assess stability of the rim. With bucket handle tears, 25% have a secondary tear of the rim that could be overlooked. If a complete meniscectomy is performed, care should be taken to prevent excessive bleeding from the meniscocapsular junction. After meniscectomy, or when the tear is left alone, stimulation of healing would help improve the results. This could be done by rasping the synovium, trephinating the meniscus to allow vascularization, and perforating the notch to cause bleeding. The penetration of the subchondral bone in the notch allows bone marrow mesenchymal cells in the field. Finally, adding autologous plasma rich in growth factors and cytokines may optimize the healing environment.
Preparation and Portal Placement
Patient positioning must allow circumferential access to the affected knee. The leg should be prepped and draped to allow posteromedial and posterolateral incisions if they are required in the case of a repair (Fig. 6-10). This can be done with the patient supine so that the break in the table is at the level of the tourniquet and the knee can be flexed to 90 degrees. Alternatively, a leg holder can be used that allows the surgeon to abduct the leg away from the operating table, allowing the knee to flex as needed for access.
Diagnostic arthroscopy is performed using a 30-degree arthroscope. This includes an evaluation of the suprapatellar pouch, both menisci, articular cartilage, and cruciate ligaments. After diagnosis, and based on the type of tear, the medial portal is established. With the help of the finger, the medial soft spot is located. A spinal needle is placed to confirm the position of the new portal. The tip of the needle should be able to reach the area of the meniscal tear. The arthroscope is rotated to view the needle. It is essential to avoid cutting the meniscus or damaging the articular surface of the medial condyle. The medial portal is made with a no. 11 blade in an oblique direction to allow increasing the size of the portal, if needed. Making the incision oblique also reduces the potential to cut the articular surface with the blade. After the portals are established, the menisci are probed on the inferior and superior surfaces to identify any tears. In assessing meniscal stability, it is important to realize that the lateral meniscus is normally more mobile, up to 10 mm, than the medial meniscus,. The definition of an unstable meniscal tear is one that is half the length of the meniscus and subluxes under the condyle when probed with a hook (see Table 6-1). Although a tourniquet may be used to improve visualization during the procedure, some surgeons prefer to leave it deflated for the diagnostic arthroscopy to assess the vascularity of the meniscal tear after rasping. Meniscectomy in the medial meniscus is usually done close to extension and with valgus stress. In ACL-deficient patients, is important to take into account that the lateral compartment is usually subluxed anteriorly in internal rotation. The medial spine will obscure the visualization of the posterior horn of the medial meniscus. To get to the posterior horn of the medial meniscus, the assistant should perform external rotation of the tibia by holding the patient’s ankle or the foot. On occasion, in a very tight knee, an 18-gauge needle may be used to “pie crust” the medial ligament over the tibia. When valgus stress is placed on the MCL, a large enough opening will allow access to the posterior horn.
Resection Techniques
Resecting a Displaced Bucket Handle Tear.
In these cases, the anteriorly displaced fragment (see Fig. 6-7) obscures visualization of the medial compartment and the posterior region of the tear. The rim may be assessed before the tear is reduced to ascertain whether a repair is possible.
Next, use the arthroscopic scissors to cut the posterior horn attachment. Cutting this first avoids the problem of the fragment displacing into the posterior compartment after cutting the anterior horn. The arthroscope may have to be placed into the intercondylar notch and the depth of the cut assessed from there. The anterior attachment is cut as close to the axilla of the tear as possible, leaving a minuscule attachment to prevent the fragment from moving away.
Special Considerations: Anterior Cruciate Ligament Reconstruction and Meniscectomy
Facing a meniscal tear during ACL surgery is not an uncommon situation. In some series, the incidence can be as high as 57%,19 whereas some others have reported an incidence of approximately 30%.20 A predominance of lateral meniscal tears has been demonstrated with acute ACL rupture, whereas the incidence of medial meniscal tears increases significantly with chronic ACL insufficiency. This suggests that lateral meniscal tears occur at the time of injury to the ACL or very soon after injury, whereas medial meniscal tears are acquired after the knee has been ACL-deficient.
A treatment decision is especially important in this scenario. Deciding to leave certain types of tears alone can result in saving time in these long procedures, with good outcomes. Definition of stability during arthroscopy, a tear that does not sublux under the condyles, or one less than 10 mm long, would be helpful in clarifying which tears could be saved. The bleeding environment along with the stable knee facilitates healing after surgery. Taking that into account, some surgeons consider that the radial tear of the lateral meniscus can also be saved in the setting of ACL reconstruction. Shelbourne19 has advocated leaving alone the vertical tear located posterior to the popliteus tendon and the posterior horn avulsion, and has shown in a long-term follow-up that they are asymptomatic. In their series of stable peripheral vertical tears of the medial meniscus treated with trephination and abrasion, Shelbourne and Rask21 have reported a 94% success rate.
Recently, Pujol and Beaufils22 have proposed to leave alone those stable tears placed on the lateral side, based on a systematic review of the literature. On the other hand, they advised that tears in the medial meniscus, including the stable ones, should be repaired or resected because of the undesirable outcomes in the published series. This advice is based on literature results on medial meniscus tears left alone, which have been shown to fail in about 50% of cases. Failure is considered to be pain, locking, or any other clinical meniscal symptoms, along with proof of nonhealing in any image test, such as arthroscopic MRI, normal MRI, or arthroscopy.
In the setting of ACL reconstruction with a tear in the lateral meniscus that could not be left alone, more emphasis should be put on repairing it over resection because of its important role in stability. A repaired lateral meniscus has a potential role in reducing anterior translation and thus protecting the graft from undesirable stresses that could lead to failure.
In terms of timing of ACL surgery with a concomitant meniscal tear, it is advisable to perform the procedure before the third month postinjury, considering the findings of Papastergiou and associates.20 They showed that the prevalence of a meniscal tear needing treatment increases significantly after this period. In their study, the prevalence of meniscal tear in the first 3 months after the traumatic injury was approximately 45%, increasing up to 69% after the sixth month. Considering that the prevalence of medial meniscal tears increases with time, they concluded that ACL reconstruction in the early period would reduce the risk of secondary meniscal tears.
Postoperative Rehabilitation
The goals of rehabilitation after meniscectomy are to diminish the swelling, regain full range of motion (ROM), and obtain similar thigh strength compared with that of the other knee. Some studies have supported physical therapy after partial meniscectomy over no treatment. These studies, which measured isokinetic knee extensor strength, have shown that the speed of strength recovery is significantly faster with physiotherapy (3 weeks) compared with no treatment (7 to 12 weeks).23 Moreover, strength differences between groups were as large as 26% and the residual deficits of the untreated patients were two to three times greater than those of the treated patients.
In another study, a statistically significant improvement in return to sports activity (P = .04) and vertical and horizontal hop tests (P = .04 and P = .02, respectively) was reported for those who received physical therapy 4 weeks after surgery compared who the group who did not receive treatment.24
Controlled physiotherapy is advisable after surgery, especially in noncompliant patients. However, it has been shown in a systematic literature review that a supervised physiotherapy program, plus written and verbal advice after arthroscopic partial meniscectomy surgery, is no more effective than written and verbal advice alone.25 In this same study, the authors concluded that for those patients who have undergone an uncomplicated arthroscopic partial meniscectomy, physical therapy is not necessary, because it will have little or no effect on their return to activities of daily living.
Rehabilitation after meniscectomy can be as aggressive as tolerated by the patient. Pain management during surgery and in the early postoperative period is crucial. The use of intra-articular and portal injections with long-lasting anesthetics (bupivacaine or ropivacaine), in combination with oral analgesics and anti-inflammatories, facilitates the beginning of ROM exercises as early as possible without pain. The use of local anesthetics is also beneficial to diminish the use of opioids, decreasing their side effects.
It has been shown that in the early postoperative period after partial meniscectomy, under a physiotherapist’s supervision, the use of a bicycle ergometer equipped with an adjustable pedal arm improved gait performance at weeks 1, 2, and 4 after surgery compared with nonsupervised rehabilitation.26 However, the most common protocol is to instruct the patient on how to perform the ROM and strengthening exercises by herself or himself.
OUTCOMES
The menisci were once considered a vestigial tissue, without any role in the knee.27 At that time, total open meniscectomy was considered the definitive treatment for its pathology. The short-term results of total meniscectomy are good because it eliminates the mechanical symptoms of locking immediately and achieves fast pain relief. On the other hand, the clinical results worsen with time, and osteoarthritis of the involved compartment appears sooner than age-matched controls without total meniscectomy.28 In addition, total meniscectomy is associated with more radiographic osteoarthritis over time than partial meniscectomy.16
Because of the increasing information about meniscal function, surgical procedures have evolved with the objective of preserving as much tissue as possible. Thus, partial meniscectomy has become the elected treatment when repair is not possible. The American Academy of Orthopaedic Surgeons estimates that 636,000 arthroscopic procedures of the knee are performed each year in the United States.29
With the help of optical magnification and minimally invasive instruments, arthroscopic partial meniscectomy has become the gold standard over open surgery.30 Numerous reports have commented on the beneficial effect of the use of arthroscopy over open surgery.
When analyzing partial meniscectomy results, various methods of determining surgical outcome have been used, ranging from clinical examination to patient satisfaction and radiographic measurements. In general, in the literature, uniformly good to excellent results have been documented in 80% to 95% of patients within the first 5 years after partial meniscectomy. Rockborn and coworkers31 have reported a mean Lysholm score of more than 84 in the first year after meniscectomy. It has been shown that allowing the patient to watch the arthroscopic procedure increases his or her overall understanding and satisfaction in the early postoperative period. In addition, it decreases the anxiety and worries about the surgery and the postoperative period significantly.32
Clinical outcomes in the long term are also satisfactory. Burks and colleagues33 have published overall Lysholm scores of 94 and average satisfaction index of 8.8. Moreover, the Tegner change of desired versus actual activity level was 0.3. This means that the subjective results were satisfactory 15 years after meniscectomy.
Higuchi and associates,34 based on the criteria of Tapper and Hoover and the International Knee Documented Committee’s evaluation form (IKDC), rated their results after 12.2 years postmeniscectomy as being excellent and good in 71% of their series.
Because of the variety of measuring tools used in the different studies, it is difficult to compare their results. Addressing that issue, the University of Western Ontario has developed, and validated the WOMET.35 This is a simple, disease-specific tool designed to evaluate health-related quality of life in patients with meniscal pathology to be used in research or in clinical practice uniformly.
Meniscectomy is a well-known risk factor for secondary osteoarthritis (OA) of the knee. Traditionally considered as a result of joint injury and increased cartilage contact stress caused by the loss of meniscal tissue, wear and tear is a straightforward explanation for secondary knee OA. In addition, there is proof of an interaction between primary heritable OA and exogenous secondary OA caused by meniscectomy.36 Moreover, there is a sixfold increased relative risk for the development of radiographic osteoarthritis after total meniscectomy compared with nonoperated controls.2 However, as expected, partial meniscectomy induces less radiographic OA over time than does total meniscectomy.16
Is important to note that radiographic changes do not clearly correlate with clinical symptoms.37 Thus, radiographic outcome appears to be a poor determinant of overall outcome from surgery.
Degenerative tears of the menisci have been associated with osteoarthritis. Whether degenerative tear is a cause or consequence of osteoarthritis is still unknown. Some studies have suggested that a degenerative tear could be the first sign of arthritis in the knee. Patients suffering a degenerative tear experience worse clinical outcomes than those with a traumatic lesion.38 Partial meniscectomy of degenerative tears is associated with a high risk of radiographic and symptomatic tibiofemoral arthritis at 16-year follow-up.2 Evaluating for pain after exercise at 8.5 years follow-up, patients with flap or horizontal tears had worse clinical outcomes after meniscectomy than those with bucket handle tears.39
Data regarding medial versus lateral partial meniscectomy are controversial. Although in vivo studies have not clearly shown significant differences between sides, laboratory studies have proven that lateral partial meniscectomy is more dangerous than the same procedure performed in the medial compartment. Englund and Lohmander16 published worse radiographic outcomes in association with lateral meniscectomy 22 years after surgery than medial meniscectomy. The lateral meniscus carries a higher load in the knee compared with the medial meniscus. Consequently, its loss may result in increased cartilage contact stress.
However, only some factors have proven to affect the outcome significantly. In the short term, only female gender and previous OA are associated with a slower rate of recovery from arthroscopic partial meniscectomy, whereas age, body mass index, depth of meniscal excision, involvement of one or both menisci, and extent of meniscal tear show no association.15 In the long term, contributing risk factors for arthritis development after meniscal resection are similar to risk factors for common knee osteoarthritis. Systemic and local biomechanical factors interact. Younger patient age predicts a better long-term prognosis after meniscectomy, whereas, obesity, female gender, and preexisting early-stage OA are features associated with poor self-reported and radiographic outcomes.16
COMPLICATIONS
The overall complication rate of knee arthroscopy is relatively low.40 It has been estimated in retrospective large series of 118,590 and 395,566 arthroscopies to be 0.8%41 and 0.5%,42 respectively. In those series, complications were more likely to occur with more complex procedures, such as meniscal repair, synovectomy, and intra-articular reconstruction of both the ACL and PCL. In a prospective study reviewing 10,262 procedures, Small43 has found an overall complication rate of 1.68%. The most common complications in this study were hemarthrosis (60.1%), infection (12.1%), thromboembolic disease (6.9%), anesthetic complications (6.4%), instrument failure (2.9%), complex regional pain syndrome 1 (CRPS 1; 2.3%), ligament injury (1.2%), and fracture or neurologic injury (0.6% each).
Medial collateral injury during arthroscopic maneuvers may occur. Leg holders or posts are commonly used to aid exposure, particularly of the posterior horn of the medial meniscus. To achieve better exposure, valgus force is applied. If force is not used judiciously, a medial collateral ligament injury may result. This is especially possible in a tight medial compartment in a middle-aged or older patient in whom the soft tissues are likely to be less flexible. Small42 has reported a 0.003% incidence of medial collateral injury; ninety % of them were attributed to the use of the leg holder. Treatment is normally conservative by functional bracing, with initial restriction of extension.
On the medial side, the infragenicular branches of the saphenous nerve (IGBSN) can be affected more commonly. Sherman and colleagues44 have reported an incidence of 22.2% of sensory changes in the distribution of the IGBSN after standard portals had been used. Although safe zones have been advocated, the wide variability in the course of the nerve precludes the absolute avoidance of damage. Mochida and associates45 have recommended that arthroscopic portals should be positioned close to both the patella and patellar tendon if injury to the IGBSN is to be avoided. On the lateral side, there has been a report of injury to the common peroneal nerve during lateral meniscectomy,46 but this complication usually occurs during meniscal suture.
A temporary paresis may occur after prolonged inflation of the tourniquet. In the series of Sherman and coworkers,44 the incidence of complications was directly related to age and tourniquet time. However, the higher risk for major complications was in the group in which the tourniquet time was longer than 60 minutes regardless of age, with a predicted complication rate of 14.3%. To avoid this type of complication, it is important that regular checks be made on the accuracy of tourniquet pressure, which should be deflated after a maximum of 2 hours.
Infection rates of arthroscopic meniscectomy are similar to those of other basic arthroscopic procedures. Kirchhoff46a has reported an incidence of infection in elected arthroscopy of 0.42%. In knee arthroscopy, Sherman and colleagues44 have reported an incidence of 0.1%, DeLee41 of 0.08%, D’Angelo and Ogilvie-Harris47 of 0.23%, and Armstrong and associates48 of 0.42%. This severe complication may be avoided with the use of antibiotic prophylaxis. Bert47a has shown that routine antibiotic administration does not reduce the rate of postoperative septic arthritis. Although some institutions do not routinely use antibiotic prophylaxis in arthroscopic meniscectomy procedures, D’Angelo and Ogilvie-Harris47 have recommended its use based on their cost-effective analysis. On the other hand, the appearance of septic arthritis of the knee postmeniscectomy is a devastating complication that should be treated aggressively. The most common infecting organism is Staphylococcus aureus. In the treatment protocol, arthroscopic débridement, along with intravenous antibiotics, should be included. Continuous passive motion is recommended as soon as the patient tolerates it.
Some exceptional complications have been reported. Berndt and coworkers49 have reported the appearance of heterotopic ossification of the medial portal after partial meniscectomy. Furthermore, MacDessi and colleagues50 have reported a series of eight cases of osteonecrosis after meniscectomy. They attributed the cause to subchondral fractures and suggested that this complication should be treated successfully with arthroplasty.
CONCLUSIONS
Although meniscectomy is still the most frequent current procedure, there is an increasing interest in preserving techniques because of more information about the role of the menisci. Moreover, new biologic enhancing techniques, along with tissue engineering, may be the future of the treatment of meniscal pathology.
1. Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints. Part I: tibial surface of the knee. J Biomech Eng. 1983;105:216-225.
2. Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178-2187.
3. von Lewinski G, Stukenborg-Colsman C, Ostermeier S, Hurschler C. Experimental measurement of tibiofemoral contact area in a meniscectomized ovine model using a resistive pressure-measuring sensor. Ann Biomed Eng. 2006;34:1607-1614.
4. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883-888.
5. King D. The healing of semilunar cartilages. 1936. Clin Orthop Relat Res. 1990;(252):4-7.
6. Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90-95.
7. Arnoczky SP, Warren RF. The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med. 1983;11:131-141.
8. Fitzgibbons RE, Shelbourne KD. “Aggressive” nontreatment of lateral meniscal tears seen during anterior cruciate ligament reconstruction. Am J Sports Med. 1995;23:156-159.
9. Lantz B, Singer KM. Meniscal cysts. Clin Sports Med. 1990;9:707-725.
10. Ferrer-Roca O, Vilalta C. Lesions of the meniscus. Part I: macroscopic and histologic findings. Clin Orthop Relat Res. 1980;(146):289-300.
11. Metcalf R, Burks R, Metcalf M. Arrhroscopic meniscectomy. In: McGinty J, Caspari R, Jackson R, editors. Operative Arthroscopy. Philadelphia: Lippincott-Raven; 1996:263-297.
12. Shelbourne KD, Martini DJ, McCarroll JR, VanMeter CD. Correlation of joint line tenderness and meniscal lesions in patients with acute anterior cruciate ligament tears. Am J Sports Med. 1995;23:166-169.
13. Evans PJ, Bell GD, Frank C. Prospective evaluation of the McMurray test. Am J Sports Med. 1993;21:604-608.
14. Terry GC, Tagert BE, Young MJ. Reliability of the clinical assessment in predicting the cause of internal derangements of the knee. Arthroscopy. 1995;11:568-576.
15. Fabricant PD, Rosenberger PH, Jokl P, Ickovics JR. Predictors of short-term recovery differ from those of long-term outcome after arthroscopic partial meniscectomy. Arthroscopy. 2008;24:769-778.
16. Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50:2811-2819.
17. Konan S, Rayan F, Haddad FS. Do physical diagnostic tests accurately detect meniscal tears. Knee Surg Sports Traumatol Arthrosc. 2009;17:806-811.
18. Boden SD, Davis DO, Dina TS, et al. A prospective and blinded investigation of magnetic resonance imaging of the knee. Abnormal findings in asymptomatic subjects. Clin Orthop Relat Res. 1992;(282):177-185.
19. Shelbourne K. “Aggressive” nontreatment of lateral menical tears seen during anterior cruciate ligament reconstruction. Knee. 1996;3:201-237.
20. Papastergiou SG, Koukoulias NE, Mikalef P, et al. Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:1438-1444.
21. Shelbourne KD, Rask BP. The sequelae of salvaged nondegenerative peripheral vertical medial meniscus tears with anterior cruciate ligament reconstruction. Arthroscopy. 2001;17:270-274.
22. Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17:396-401.
23. Moffet H, Richards CL, Malouin F, et al. Early and intensive physiotherapy accelerates recovery postarthroscopic meniscectomy: results of a randomised controlled study. Arch Phys Med Rehabil. 1994;75:415-426.
24. Vervest AM, Maurer CA, Schambergen TG, et al. Effectiveness of physiotherapy after meniscectomy. Knee Surg Sports Traumatol Arthrosc. 1999;7:360-364.
25. Goodwin P, Morrisey M. Physical therapy after arthroscopic partial meniscectomy: is it effective. Exerc Sports Sci Rev. 2003;2:85-90.
26. Kelln BM, Ingersoll CD, Saliba S, et al. Effect of early active range of motion rehabilitation on outcome measures after partial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2009;17:607-616.
27. Bland-Sutton J. Ligaments: Their Nature and Morphology, 2nd ed. London: J Lewis, 1897.
28. Roos H, Laurén M, Adalberth T, et al. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41:687-693.
29. Praemer A, Furner S, Rice D. Musculoskeletal Conditions in the United States, 2nd ed. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 1999.
30. Simpson DA, Thomas NP, Aichroth PM. Open and closed meniscectomy. A comparative analysis. J Bone Joint Surg Br. 1986;68:301-304.
31. Rockborn P, Hamberg P, Gillquist J. Arthroscopic meniscectomy: treatment costs and postoperative function in a historical perspective. Acta Orthop Scand. 2000;71:455-460.
32. Bayar A, Tuncay I, Atasoy N, et al. The effect of watching live arthroscopic views on postoperative anxiety of patients. Knee Surg Sports Traumatol Arthrosc. 2008;16:982-987.
33. Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13:673-679.
34. Higuchi H, Kimura M, Shirakura K, et al. Factors affecting long-term results after arthroscopic partial meniscectomy. Clin Orthop Relat Res. 2000;(377):161-168.
35. Kirkley A, Griffin S, Whelan D. The development and validation of a quality of life-measurement tool for patients with meniscal pathology: the Western Ontario Meniscal Evaluation Tool (WOMET). Clin J Sports Med. 2007;17:349-356.
36. Englund M. The role of the meniscus in osteoarthritis genesis. Med Clin North Am. 2009;93:37-43.
37. Fabricant PD, Jokl P. Surgical outcomes after arthroscopic partial meniscectomy. J Am Acad Orthop Surg. 2007;15:647-653.
38. Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford). 2001;40:631-639.
39. Fauno P, Nielsen AB. Arthroscopic partial meniscectomy: a long-term follow-up. Arthroscopy. 1992;8:345-349.
40. Allum R. Complications of arthroscopy of the knee. J Bone Joint Surg Br. 2002;84:937-945.
41. DeLee J. Complications of arthroscopy and arthroscopic surgery: results of a national survey. J Arthrosc Rel Surg. 1985;1:214-220.
42. Small NC. Complications in arthroscopy: the knee and other joints, Committee on Complications of the Arthroscopy Association of North America. Arthroscopy. 1986;2:253-258.
43. Small NC. Complications in arthroscopic surgery performed by experienced arthroscopists. Arthroscopy. 1988;4:215-221.
44. Sherman OH, Fox JM, Snyder SJ, et al. Arthroscopy—”no-problem surgery.” An analysis of complications in two thousand six hundred and forty cases. J Bone Joint Surg Am. 1986;68:256-265.
45. Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop Relat Res. 1995;(320):88-94.
46. Rodeo SA, Sobel M, Weiland AJ. Deep peroneal-nerve injury as a result of arthroscopic meniscectomy. A case report and review of the literature. J Bone Joint Surg Am. 1993;75:1221-1224.
46a. Paul J, Kirchhoff C, Imhoff AB, Hinterwinner S. Infection after arthroscopy orthopade. 1050-2 PMID 1878. 2008. Nov;37(11):915.
47. D’Angelo GL, Ogilvie-Harris DJ. Septic arthritis following arthroscopy, with cost/benefit analysis of antibiotic prophylaxis. Arthroscopy. 1988;4:10-14.
47a. Bert JM, Giannini D, Nace L. Antibiotic prophylaxis for arthroscopy of the knee:: is it necessary?. Arthroscopy. 2007;23:4-60.
48. Armstrong RW, Bolding F, Joseph R. Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy. 1992;8:213-223.
49. Berndt C, Ganko A, Whitehouse SL. Crawford RW. Heterotopic ossification within an arthroscopic portal after uneventful partial meniscectomy. Knee. 2008;15:416-418.
50. MacDessi SJ, Brophy RH, Bullough PG, et al. Subchondral fracture following arthroscopic knee surgery. A series of eight cases. J Bone Joint Surg Am. 2008;90:1007-1012.