CHAPTER 7 Meniscal Repair
In 1885, Thomas Annandale performed the first meniscal repair.1 Because of the lack of understanding regarding the role of the meniscus, this discovery went unheralded for many years. Over time, the major role that the menisci play in load distribution, shock absorption, secondary stabilization of the knee joint, and proprioception was better understood. The menisci transmit at least 50% of a compressive load with the knee in extension.2 This increases to 85% in 90 degrees of flexion. Following a meniscectomy, the contact area is decreased by 50%, which increases the load per unit area and leads to subsequent degenerative changes in the knee. Removal of 15% to 34% of a meniscus can increase contact pressure more than 350%, so even partial meniscectomy can significantly alter joint biomechanics.3
As our knowledge of the essential role that the meniscus plays in proper knee function increased, preserving its function became increasingly important. Arthroscopic inside-out repair techniques gained popularity in the early 1980s.4 Following that, outside-in procedures were developed to decrease the chance of neurovascular injury. Recently, all-inside methods are increasingly being performed because of ease of application, decreased operative times, and even lower risk to the neurovascular structures. These techniques have led to healing rates from 60% to 80% for isolated repairs and up to 90% with concomitant anterior cruciate ligament (ACL) reconstruction.5
ANATOMY
The menisci are semilunar fibrocartilaginous structures that cover 50% of the medial and 70% of the lateral tibial plateaus.6 In cross section, their superior surface is concave and the inferior surface is convex to facilitate congruency with the femoral and tibial articular surfaces. The medial meniscus is shaped like a “C” whereas the lateral meniscus more closely resembles an incomplete “O” that is open medially. The coronary ligaments anchor both menisci to the tibia. Additionally, the medial meniscus has extensive peripheral attachments to the capsule and deep medial collateral ligament (MCL). Because of fewer capsular attachments, the popliteal hiatus, and no link to the neighboring collateral ligament, the lateral meniscus is more mobile and can displace up to 1 cm with knee range of motion.7 Its major connections to the posterior femur are through the ligaments of Humphrey and Wrisberg.
The solid microstructure of the menisci is 75% composed of collagen, with a 90% predominance of type I. The collagen is arranged in various patterns, but most of the fibers are aligned circumferentially.8 The orientation of these fibers permits absorption of the hoop stresses generated during natural movement. Radially oriented fibers provide a link between the circumferential bundles and add strength to the overall construct.9 Longitudinal or bucket handle meniscal tears disrupt these radial links between the circumferential collagen fibers. Repairing these tears may restore the biomechanical function of the native meniscus. Vertical mattress stitch configuration, which mimics the path of the radially oriented fibers, may secure more of the circumferential fibers and lead to greater repair strength more than other suture techniques.10
Thorough understanding of the meniscal microvasculature is necessary when considering repair of a tear because it plays a role in the potential for healing. Vessels from the superior and inferior branches of the medial and lateral genicular arteries perforate the menisci at the capsular attachments.11 In the area of the popliteal hiatus, the lateral meniscus lacks this peripheral supply and is an area of relative avascularity. The entire meniscus has a blood supply at birth but by 9 months, the inner third is avascular.12 By age 10, the menisci resemble those of an adult, with the outer 10% to 30% of the medial rim and 10% to 25% of the lateral rim vascularized. For clinical purposes, the menisci are often considered to have three zones, with the peripheral 3 mm considered vascular (red-red), more than 5 mm from the meniscocapsular junction, avascular (white-white), and between 3 and 5 mm, variable (red-white).13
PATIENT EVALUATION
History and Physical Examination
The diagnosis of a meniscal tear begins with a thorough initial evaluation in the office. Combining the patient’s history, physical examination, and plain radiographs can lead to a sensitivity of 88% to 95%, specificity of 72% to 92%, and positive predictive value of 58% to 85% for meniscal injuries.14 Meniscal tears in younger patients typically occur after an acute traumatic event, which often involves a twisting or hyperflexion mechanism. In the fourth decade and beyond, degenerative changes in the menisci often play a role in tears, so that less dramatic events, or even none at all, can results in a tear. Patients typically report pain, swelling, locking, catching, and giving out.
There are several tests described that focus directly on meniscal injuries. Unfortunately, no single physical examination finding can reliably predict the presence of a tear. A recent meta-analysis found a pooled sensitivity and specificity of 70% and 71% for McMurray’s test, 60% and 70% for Apley’s test, and 63% and 77% for joint line tenderness, respectively.15 Despite these findings, the authors concluded that none of the tests could accurately diagnose a tear based on the heterogeneity of study results. They could not explain the wide variation seen between each individual study’s results. Nevertheless, these tests are valuable to perform and help discern what is going on with the patient’s knee.
Diagnostic Imaging
Magnetic resonance imaging (MRI) has become the gold standard for meniscal imaging, although one must take into account that up to 13% of asymptomatic patients younger than 45 and 39% older than 45 years may have a “positive” scan.16 Benefits of MRI include providing additional information regarding associated injuries inside the knee, as well as tear location and configuration. A retrospective review following surgery for bucket handle meniscal tears has shown that whether a lesion was reparable or not could be accurately predicted 93% (26/28) of the time.17 The criteria created for this study included rim width less than 4 mm, tear length more than 1 cm, and isosignals of the peripheral rim and inner fragment with the normal contralateral meniscus in the same knee, indicating a nondegenerative process. Typically, contrast is not necessary to image the menisci properly, but should be used in cases involving a prior repair or if more than 25% of the meniscus has previously been resected to evaluate for a re-tear.18
TREATMENT
Indications and Contraindications
Once a patient has been diagnosed with a symptomatic tear of the meniscus and surgery is indicated, a number of factors play a role when considering whether the tear in this particular patient can and should be repaired. We typically explain to patients that much like real estate, location is the most important factor in addressing reparability. Adequate vascularity is a requirement for healing, so tears in the peripheral red-red zone have the best chance of healing. Tear configuration is the second most important factor, because longitudinal and vertical tears have a higher rate of healing than radial, horizontal cleavage, or degenerative tears. The third factor is size, or length, of the tear. Usually, a tear must be at least 1 cm long to be considered for repair, because smaller tears may be inherently stable and heal without surgery or be asymptomatic.19 Many of these factors are best judged arthroscopically. Acute tears also have a higher rate of healing than chronic injuries.20
Stability of the knee is another factor to consider when contemplating meniscal repair. Healing rates are less than 30% in an ACL-deficient knee that remains unreconstructed.5 It has been shown in several studies that simultaneous ACL reconstruction enhances the success of meniscal healing.21,22
In general, many surgeons consider patients younger than 40 years for meniscal repair. Although some studies have shown that older patients can heal following repairs,22 one has to weigh the risks and benefits versus a partial meniscectomy. Subjecting older patients to the risk of a possible second surgery if the tear doesn’t heal, as well as the difficulties of rehabilitation, may be unnecessary, considering that they might do just as well with a meniscectomy. In addition, older people are more likely to have articular cartilage changes and tissues with poorer healing qualities, which can jeopardize the success of a repair.
Conservative Management
Nonsurgical treatment may be considered for a select group of tears. Partial or small (less than 5 mm) complete tears located in the peripheral third may heal without operative intervention. This should only be considered for acute traumatic tears. Chronic and degenerative lesions are less likely to improve without surgery. In addition, meniscal tears generally do not heal in ligamentously unstable knees and nonoperative management is typically avoided.
Arthroscopic Technique
Meniscal Preparation
There are multiple techniques to promote a vascular environment. Abrasion of the synovial fringes extending over the peripheral edges of the meniscus with a rasp can stimulate a proliferative response to enhance healing.23 In a rabbit model, this has been shown to improve the mechanical properties of the healed meniscus significantly.24 Another option is trephination of the peripheral meniscal rim. We prefer to do this by creating multiple perforations with an 18- or 20-gauge needle from outside-in. This technique creates conduits for vascular migration to the tear. It is important to minimize channel size to limit disruption of the collagen framework that provides the beneficial biomechanical properties of the meniscus.25 Rotational flaps of vascular synovial pedicles have also been shown to aid meniscal healing in animal models, but are rarely used in humans because of difficulties applying this technique arthroscopically.26
Fixation
Vertical mattress orientation of the sutures is preferred whenever possible. These have been shown to be superior biomechanically to horizontal mattress and mulberry knot techniques.27 The number of fixation points used depends on the length and stability of the tear. Most surgeons tend to space fixators or sutures 5 to 8 mm apart. It is important to range the knee several times after final fixation has been applied. If subsequent gapping or displacement is noted, additional fixation or alternate methods must be added.
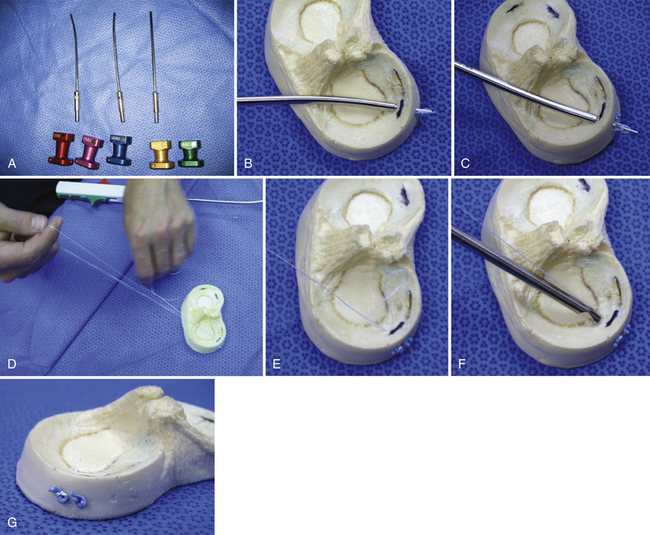
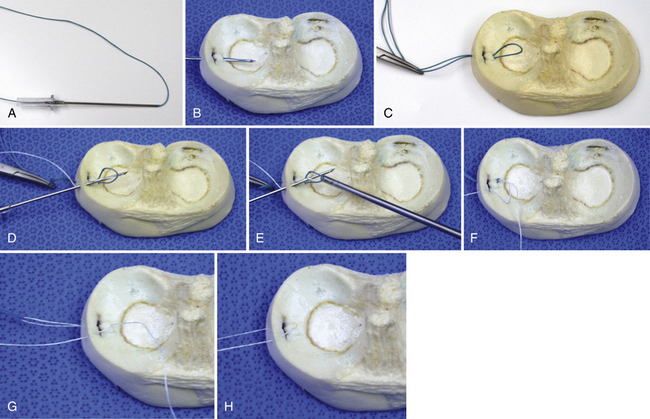
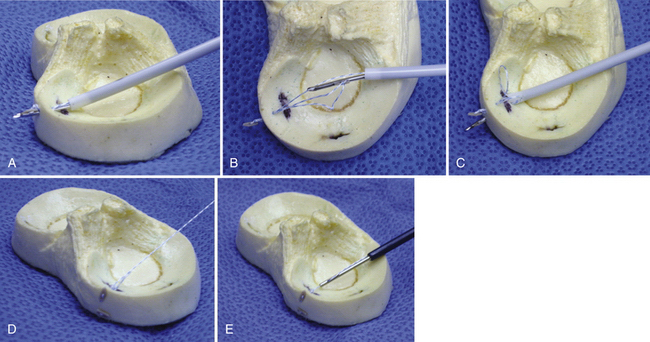
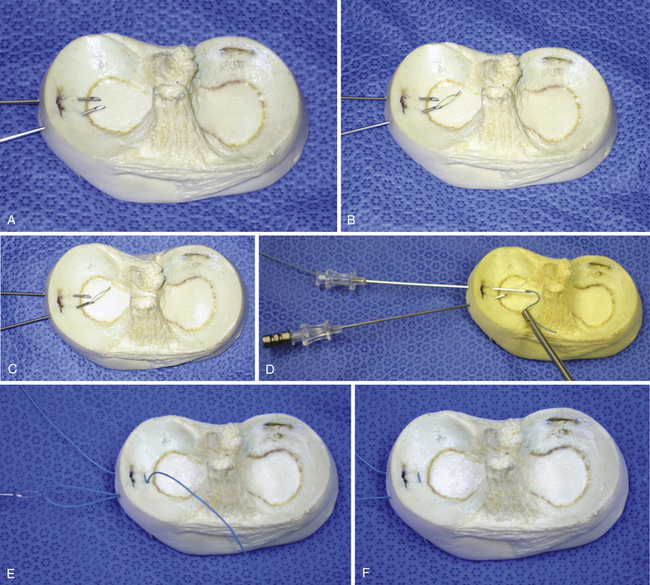
The choice regarding which fixation technique to use varies based on tear size, configuration, and location, as well as surgeon preference (Figs 1 to 6). It is also important to recognize that meniscal fixators cost significantly more than sutures. Typically, for tears located posteriorly, we prefer all-inside meniscal fixators to limit the risk of neurovascular injury. For anterior third tears, we typically use an outside-in technique. Once started, we often continue to use this technique into the middle third of the meniscus. It is not uncommon for us to achieve hybrid fixation with different techniques in the same tear.
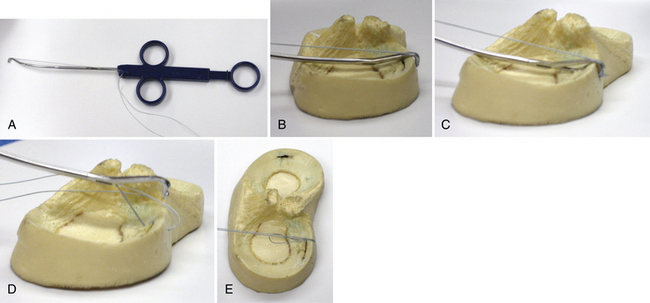
FIGURE 7-3 Arthrex (Naples, Fla) Viper technique. A, Load suture on device. B, Place device over tear site. C, Deploy needle. D, Withdraw device. E, Secure with a racking hitch knot.
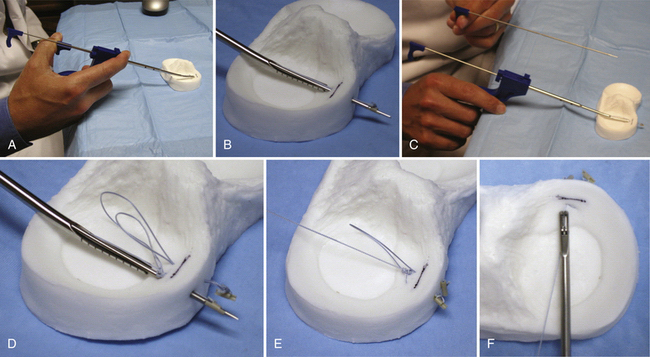
FIGURE 7-5 Arthrex (Naples, Fla) Meniscal Cinch technique. A, Hold device like a syringe. B, Deploy first needle. C, Remove needle. D, Reposition device and fire second needle. E, Pull on single strand. F, Cut suture once tensioned appropriately.
Inside-Out Repair.
Inside-out repairs are best suited for middle or posterior tears. Medially, the saphenous nerve is at risk. With the arthroscope in the anterolateral portal, it is brought up to the medial tear to transilluminate the skin where the planned incision is to be made. One can visualize the saphenous vein in this manner, knowing that the nerve lies immediately posterior and therefore can be avoided. Flex the knee 90 degrees also to let the nerve slide posteriorly, away from the area that is being manipulated. A 4-cm incision is made in line with the posteromedial border of the tibia, just posterior to the MCL. Place one third of the incision proximally and two thirds distally to the joint line. Dissect carefully through the subcutaneous tissues. Incise the fascia anterior to the sartorius muscle. Retract it posteriorly, along with the semitendinosus. Anteriorly, you will see the superficial MCL. Develop the interval between the joint capsule and the medial head of the gastrocnemius bluntly with a finger. Place a retractor or pediatric gynecologic speculum posteriorly to retract the gastrocnemius and semimembranosus.
The common peroneal nerve is at greatest risk laterally. Once again, flex the knee 90 degrees to let it drift posterior to the operative field. Make a 4-cm incision just posterior to the lateral collateral ligament. It should be centered just distally to the joint line, but should not extend beyond the level of the fibular head. This is the soft spot of the lateral knee, where posterolateral portals are made. After dissection through the subcutaneous tissues, identify the iliotibial band and biceps femoris. Retract the biceps posteriorly to protect the peroneal nerve. Elevate the lateral head of the gastrocnemius off the knee capsule and place a retractor or pediatric gynecologic speculum posteriorly.
Outside-In Repair.
One very simple and cost-effective technique was first described in 2004.28 Preload an 18-gauge needle with a suture that is at least 40 cm long. Roughly 10 cm of the stitch should extend beyond the needle tip. Transilluminate the skin to help identify where the needle should be placed. Pierce both the inner and outer portions on the meniscus across the tear. The needle should be directed so that it comes out on the superior surface of the inner meniscal rim. Use an arthroscopic grasper through the ipsilateral portal to hold the loop inside the knee joint while withdrawing the needle. Pull the needle out away from the skin approximately 15 cm without unloading the suture, or the surgeon may choose to reload the needle with a second suture. Tag the two suture limbs coming from the skin. Reinsert the needle through the same track and perforate the superior portion of the peripheral rim only in a vertical mattress fashion. Direct the needle so that it passes through the suture loop held by the grasper. Use the grasper to grab the suture from the needle tip and pull it out the ipsilateral portal. Pull on the two sutures held by the tag clamp to shuttle the suture from the second needle insertion through the path from the first insertion. Remove the needle and repeat the process as necessary.
All-Inside Repair.
The first generation of all-inside meniscal fixators consisted of rigid, bioabsorbable arrows, darts, and screws that could be placed across tears. Each device has a specific technique for insertion, but in general a curved cannula is used to place them in the proper location. After the tear is pierced with a trocar, the device is screwed or tapped into position. These fixators do not allow for the ability to tension the repair. In addition, several studies have demonstrated unacceptable failure rates and serious complications, including chondral scoring from the fixator’s head, implant breakage, insertion difficulties, and postoperative joint line irritation from the devices.29,30
Adjuncts to Repair
As noted, simultaneous ACL reconstruction has been shown to enhance the ability of the meniscus to heal. One theory is that the tear is bathed postoperatively in cytokines and growth factors from the bone marrow released during tunnel drilling and notchplasty.19 This has led to the development of several methods to try and mimic this milieu. Intercondylar microfracture with an awl can simulate the environment created by a notchplasty, but the results have not been studied clinically.31 A fibrin clot can be made with the patient’s whole blood stirred in a container with a sintered glass rod. This should be placed in the tear prior to compressing it with the fixation. Studies have suggested that it may improve meniscal healing for red-white tears.32 Platelet-rich plasma derived from whole-blood centrifugation provides growth factors in higher concentrations than fibrin clot and has shown promise in promoting healing elsewhere in the body, but has not been studied for meniscal repair.19
1. Annandale T. An operation for displaced semilunar cartilage. Br J Med. April 1885;18:779.
2. Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints. Part I: tibial surface of the knee. J Biomech Eng. 1983;105:216-225.
3. Seedholm BB, Hargreaves DJ. Transmission of the load in the knee joint with special reference to the role of the menisci. Eng Med. 1979;8:220.
4. Barber FA, McGarry JE. Meniscal repair techniques. Sports Med Arthrosc Rev. 2007;15:199-207.
5. Turman KA, Diduch DR. Meniscal repair:indications and techniques. J Knee Surg. 2008;21:154-162.
6. Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34:252-257.
7. Scott WN. ed. Surgery of the Knee, 4th ed. Philadelphia: Elsevier, 2006:15-24.
8. Bullough PG, Munuera L, Murphy J, Weinstein AM. The strength of the menisci of the knee as it relates to their fine structure. J Bone Joint Surg Br. 1970;52:564-567.
9. McDevitt CA, Webber RJ. The ultrastructure and biochemistry of the meniscal cartilage. Clin Orthop Relat Res. 1990;(252):8-18.
10. Post MD, Akers MS, Vincent K. Load to failure of common meniscal repair techniques: effects of suture technique and suture material. Arthroscopy. 1997;13:731-736.
11. Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90-95.
12. Greis P, Bardana D, Holstrom M, Burks R. Meniscal injury. I. Basic science and evaluation. J Am Acad Orthop Surg. 2002:168-187.
13. DeHaven KE. Decision-making features in the treatment of meniscal lesions. Clin Orthop Relat Res. 1990;252:49-54.
14. Terry GC, Tagert BE, Young MJ. Reliability of the clinical assessment in predicting the cause of internal derangements of the knee. Arthroscopy. 1995;11:568-576.
15. Hegendus EJ, Cook C, Hasselblad V, et al. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2007;37:541-550.
16. Boden SD, Davis DO, Dina TS, et al. A Prospective and blinded investigation of magnetic resonance imaging of the knee: abnormal findings in asymptomatic subjects. Clin Orthop Relat Res. 1992;282:177-185.
17. Thoreaux P, Rety F, Nourissat G, et al. Bucket handle meniscal lesion: magnetic resonance imaging criteria for reparability. Arthroscopy. 2006;9:954-961.
18. Magee T, Shapiro M, Rodriguez J, et al. MR arthrography of postoperative knee: for which patients is it useful?. Radiology. 2003;229:159-163.
19. Scott WN. ed. Surgery of the Knee, 4th ed. Elsevier; 2006:481-490.
20. Rispoli DM, Miller MD. Options in meniscal repair. Clin Sports Med. 1999;18:77-91.
21. Cannon WD, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament–reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176-181.
22. Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000;16:822-829.
23. Ritchie JR, Miller MD, Bents RT, Smith DK. Meniscal repair in the goat model. The use of healing adjuncts and the role of magnetic resonance arthrography in repair evaluation. Am J Sports Med. 1998;26:278-284.
24. Okuda K, Ochi M, Uchio Y. Meniscal rasping for repair of meniscal tear in the avascular zone. Arthroscopy. 1999;15:281-286.
25. DeHaven KE, Arnoczky SP. Meniscal repair. Part I: basic science, indications for repair, and open repair. J Bone Joint Surg. 1994;76:140-152.
26. Kobuna Y, Shirakura K, Niijima M. Meniscal repair using a flap of synovium. An experimental study in the dog. Am J Knee Surg. 1995;8:52-55.
27. Post WR, Akers SR, Kish V. Load to failure of common meniscal repair techniques: effects of suture technique and material. Arthroscopy. 1997;13:731-736.
28. Laupattarakasem W, Sumanont S, Kesprayura S, Kasemkijwattana C. Arthroscopic outside-in meniscal repair through a needle hole. Arthroscopy. 2004;20:654-657.
29. Kurzweil PR, Tifford CD, Ignacio EM. Unsatisfactory clinical results of meniscal repair using the meniscus arrow. Arthroscopy. 2005;21:905-907.
30. Lee GP, Diduch D. Deteriorating outcomes after meniscal repair using the meniscal arrow in knees undergoing concurrent anterior cruciate ligament reconstruction: increased failure rate with long-term follow-up. Am J Sports Med. 2005;33:1138-1141.
31. Freedman KB, Nho SJ, Cole BJ. Marrow-stimulating technique to augment meniscus repair. Arthroscopy. 2003;19:794-798.
32. McAndrews PT, Arnoczky SP. Meniscal repair enhancement techniques. Clin Sports Med. 1996;15:499-510.