138
Melanoma mimics
Seborrheic keratosis with an irregular border and a white area that mimics regression in a melanoma. The white surface horn pearls support the diagnosis of seborrheic keratosis.

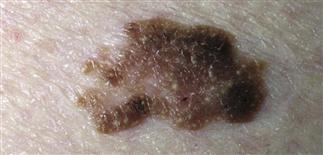
Seborrheic keratosis. A large, multicolored lesion. Magnification showed scale over the entire surface and black horn pearls imbedded in the dark thick areas.

Seborrheic keratosis. The lesion is black with an irregular notched border. The large, black, surface horn pearls support the diagnosis of seborrheic keratosis.

Seborrheic keratosis. A dome-shaped, black lesion that mimics nodular melanoma. Black surface horn pearls support the diagnosis of seborrheic keratosis.
DESCRIPTION
Melanocytic or non-melanocytic skin lesions that may clinically and/or histologically resemble melanoma.
HISTORY
• Benign melanocytic nevi may be clinically suspicious for melanoma. • Roughly 30–50% of melanomas arise in pre-existing melanocytic lesions. • Nevi classified as junctional, compound, intradermal based on location of nevus cells within skin. • Most nevi symmetric, sharply defined, less than 6 mm at greatest diameter, usually one dominant color, usually asymptomatic. Nevi that develop symptoms or change appearance (size, shape, color) are suspicious. • Atypical nevi often larger than 6 mm at greatest diameter, tend to have indistinct borders, variegated pigmentation.
PHYSICAL FINDINGS
• Blue nevi are benign melanocytic nevi with nevus cells located deep within dermis. Blue to black color may suggest melanoma. Blue nevi are defined, uniformly color, stable in appearance. • Combined nevi are blue nevi associated with overlying benign junctional, compound, or intradermal nevus. Combined nevi are solitary, asymmetric with focal pigmentation. • Traumatized nevi often have hemorrhagic crusting suggesting ulceration. Patients are usually aware of trauma. • Nevi previously biopsied can develop recurrent nevus phenomenon, with melanocyte hyperplasia on scar that resembles melanoma clinically and histologically. Review of original biopsy helps exclude melanoma diagnosis. • Pigmented basal cell carcinoma contains melanin pigment. Amount of melanin and its distribution vary. Lesions often pink with focal blue to gray pigment, or jet black. • Seborrheic keratoses often contain varying amounts of melanin. Pigmentation uneven, asymmetric; can grow rapidly. Lesions vary from flat to verrucous; white to pink to jet black. • Spreading pigmented actinic keratosis displays fine reticulated pigmentation, thin scale. Lesions appear on sun-damaged skin, simulate lentigo maligna melanoma. • Vascular lesions, including cherry angiomas, angiokeratomas, hemangiomas, can be red, purple, black. • Friction injury to heel (talon noir) or nail trauma may produce hemorrhage. Hemosiderin may be present, suggesting melanin pigment. • Lesions that mimic melanoma clinically are discriminated from melanoma histologically. • Nevus cells of Spitz nevus may be pleomorphic, indistinguishable from melanoma cells on histologic grounds. Lesion architecture, patient’s age help discern Spitz nevus from melanoma. • Lentigo maligna can be quite subtle, can resemble benign junctional nevi histologically. Junctional nevi are lesions of childhood; junctional nevi from an adult are best considered suspicious.
TREATMENT
• Biopsy suspicious lesions. Histology often discerns melanoma from lesions clinically suspicious for melanoma. • Histologic mimics of melanoma include malignancies derived from non-melanocytic cells. Special stains reveal origin of malignant cells. • Melanocytic lesions that mimic melanoma histologically, such as Spitz nevus, recurrent nevus, require clinicopathologic correlation. • Management and follow-up depend on histologic diagnosis.







