Chapter 102 Melaleuca alternifolia (Tea Tree)
Melaleuca alternifolia (family: Myrtaceae)
 Chemical Composition
Chemical Composition
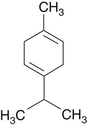
Tea tree leaves contain about 1.8% of oil obtained via steam distillation.1 This oil contains more than 48 compounds, but is chiefly composed of the following2:
The Australian standard (AS 2782-1985) for “Oil of Melaleuca (Terpinen-4-ol type)” sets a minimum content of terpinen-4-ol at 30% and a maximum 1,8-cineol content of 15%.1
 History and Folk Use
History and Folk Use
The medicinal properties of crushed tea tree leaves were known to the Bundjalung Aborigines of northern New South Wales, Australia. The waters of a lagoon where tea tree leaves had fallen and decayed for hundreds of years were viewed as having tremendous healing properties.1
The popular name of tea tree was first reported in 1777, in Captain Cook’s account of his second voyage, entitled A Voyage to the South Pole. The leaves of M. alternifolia were also used by the early settlers of Australia to make tea; hence, the further use of the popular name “tea tree.”1
The first report of tea tree’s medicinal use appeared in the Medical Journal of Australia in 1930.3 A surgeon in Sydney reported impressive results using a solution of tea tree oil to clean surgical wounds. According to this report3:
During World War II, tea tree oil was issued to soldiers to use as a disinfectant. The Australian Army went so far as to commandeer supplies of the oil and exempt leaf cutters from national service to maintain production. The production of tea tree oil during World War II was regarded as an “essential” industry.1
After World War II, the tea tree oil industry stagnated for more than 30 years. There were a number of reasons for this, including the general trend away from natural medicines and toward synthetic medical drugs. However, during the late 1970s and early 1980s, the Australian tea tree oil industry was reborn as successful plantations growing M. alternifolia were established.1
Tea tree oil has been used in the treatment of the following conditions1:
 Pharmacology
Pharmacology
Tea tree oil possesses significant antiseptic properties and is regarded by many as the ideal skin disinfectant. This claim is supported by its efficacy against a wide range of organisms, its good penetration, and its lack of skin irritation.1 The therapeutic uses of tea tree oil are based largely on its antiseptic and antifungal properties. Bacteria and fungal organisms inhibited by tea tree oil are listed in Tables 102-1 and 102-2.1,4–6
TABLE 102-1 Bacteria Inhibited by Melaleuca alternifolia Oil
| BACTERIAL SPECIES | % (vol/vol) | |
|---|---|---|
| MIC | MBC | |
| Acinetobacter baumannii | 1 | 1 |
| Actinomyces viscosus | 0.6 | >0.6 |
| Actinomyces spp. | 1 | 1 |
| Bacillus cereus | 0.3 | |
| Bacteroides spp. | 0.06-0.5 | 0.06-0.12 |
| Corynebacterium spp. | 0.2-2 | 2 |
| Enterococcus faecalis | 0.5->8 | >8 |
| E. faecium (vancomycin resistant) | 0.5-1 | 0.5-1 |
| Escherichia coli | 0.08-2 | 0.25-4 |
| Fusobacterium nucleatum | 0.6->0.6 | 0.25 |
| Klebsiella pneumoniae | 0.25-0.3 | 0.25 |
| Lactobacillus spp. | 1-2 | 2 |
| Micrococcus luteus | 0.06-0.5 | 0.25-6 |
| Peptostreptococcus anaerobius | 0.2-0.25 | 0.03->0.6 |
| Porphyromonas endodontalis | 0.025-0.1 | 0.025-0.1 |
| P. gingivalis | 0.11-0.25 | 0.13->0.6 |
| Prevotella spp. | 0.03-0.25 | 0.03 |
| Prevotella intermedia | 0.003-0.1 | 0.003-0.1 |
| Propionibacterium acnes | 0.05-0.63 | 0.5 |
| Proteus vulgaris | 0.08-2 | 4 |
| Pseudomonas aeruginosa | 1-8 | 2->8 |
| Staphylococcus aureus | 0.5-1.25 | 1-2 |
| S. aureus (methicillin resistant) | 0.04-0.35 | 0.5 |
| S. epidermidis | 0.45-1.25 | 4 |
| S. hominis | 0.5 | 4 |
| Streptococcus pyogenes | 0.12-2 | 0.25-4 |
| Veillonella spp. | 0.016-1 | 0.03-1 |
MBC, minimal bactericidal concentration; MIC, minimum inhibitory concentration.
Data from Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (tea tree) oil: a review of antimicrobial and other medicinal properties. Clin Microbiol Rev. 2006;19:50-62.
TABLE 102-2 Fungi Inhibited by Melaleuca alternifolia Oil
| FUNGAL SPECIES | % (vol/vol) | |
|---|---|---|
| MIC | MFC | |
| Alternaria spp. | 0.016-0.12 | 0.06-2 |
| Aspergillus flavus | 0.31-0.7 | 2-4 |
| A. fumigatus | 0.06->2 | 1-2 |
| A. niger | 0.016-0.4 | 2-8 |
| Blastoschizomyces capitatus | 0.25 | |
| Candida albicans | 0.06-8 | 0.12-1 |
| C. glabrata | 0.03-8 | 0.12-0.5 |
| C. parapsilosis | 0.03-0.5 | 0.12-0.5 |
| C. tropicalis | 0.12-2 | 0.25-0.5 |
| Cladosporium spp. | 0.008-0.12 | 0.12-4 |
| Cryptococcus neoformans | 0.015-0.06 | |
| Epidermophyton flocossum | 0.008-0.7 | 0.12-0.25 |
| Fusarium spp. | 0.008-0.25 | 0.25-2 |
| Malassezia furfur | 0.03-0.12 | 0.5-1.0 |
| M. sympodialis | 0.016-0.12 | 0.06-0.12 |
| Microsporum canis | 0.03-0.5 | 0.25-0.5 |
| M. gypseum | 0.016-0.25 | 0.25-0.5 |
| Penicillium spp. | 0.03-0.06 | 0.5-2 |
| Rhodotorula rubra | 0.06 | 0.5 |
| Saccharomyces cerevisiae | 0.25 | 0.5 |
| Trichophyton mentagrophytes | 0.11-0.44 | 0.25-0.5 |
| T. rubrum | 0.03-0.6 | 0.25-1 |
| T. tonsurans | 0.004-0.016 | 0.12-0.5 |
| Trichosporon spp. | 0.12-0.22 | 0.12 |
MBC, minimal bactericidal concentration; MIC, minimum inhibitory concentration.
Data from Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (tea tree) oil: a review of antimicrobial and other medicinal properties. Clin Microbiol Rev. 2006;19:50-62.
 Clinical Applications
Clinical Applications
Skin Infections
A clinical trial in patients with furuncles demonstrated that tea tree oil encouraged more rapid healing without scarring than was seen in matched control subjects.7 Presumably, the positive clinical effects were due to the oil’s germicidal activity against Staphylococcus aureus. Tea tree oil efficiently kills S. aureus in the stationary growth phase and within biofilms, making it a promising tool for S. aureus eradication.8 In the clinical trial, the method of application consisted of cleaning the site followed by painting the surface of the furuncle freely with tea tree oil two or three times a day.
Lice Infestations
Pediculosis capitis (head lice infestation) treatment typically involves application of topical insecticides such as a pyrethrin or permethrin. An in vitro study showed that tea tree oil exerted the greatest effect of essential oils tested against head lice.9 A clinical study compared the efficacy and safety of three topical pediculicides. A pediculicide containing tea tree and lavender oil was compared with a product containing pyrethrins and piperonyl butoxide; the percentage of subjects who were louse-free one day after the last treatment with the tea tree oil and lavender product was 97.6% (41 of 42 patients) compared with 25% (10 of 40 patients) of those using the product containing pyrethrins and piperonyl butoxide.10 These clinical results, along with in vitro studies, indicate that products containing tea tree oil are effective alternatives to pyrethrin-based products.
Oral Infections
Tea tree oil was shown to exert significant activity against oral pathogens, both bacterial and fungal, and was suggested to be a suitable alternative to chlorhexidine.11 From a clinical perspective, these effects may best be utilized in the treatment of oral candidiasis (thrush). In one open study, 27 patients with acquired immunodeficiency syndrome (AIDS) and oral candidiasis that was clinically refractory to fluconazole were randomly assigned to receive either an alcohol-based or an alcohol-free melaleuca oral solution four times daily for 2 to 4 weeks. Overall, 60% of patients demonstrated a clinical response to the melaleuca oral solution (seven cases were cured and eight cases clinically improved) at 4-week evaluation.12
Tea tree oil appears to be quite useful in oral candidiasis in cancer patients. Often these yeasts are resistant to azole antifungal drugs. In one study, 301 yeasts isolated from the mouths of 199 patients with advanced cancer were shown to be susceptible to tea tree oil, including 41 yeasts that were known to be resistant to both fluconazole and itraconazole.13
Dandruff
There is evidence that dandruff appears to be related to the yeast Pityrosporum ovale. Because tea tree oil has antifungal activity against P. ovale, a 4-week study was designed to investigate the efficacy and tolerability of 5% tea tree oil shampoo versus a placebo in 126 male and female patients, aged 14 years and older, with moderate dandruff. The 5% tea tree oil shampoo group showed a 41% improvement in the quadrant-area-severity score, compared with an 11% improvement in the placebo group. Statistically significant improvements were also observed in the total area of involvement score, the total severity score, and the itchiness and greasiness components of the patients’ self-assessments. The scaliness component of patient self-assessment improved but was not statistically significant. There were no adverse effects.14
Acne
Topical application of tea tree oil is a suitable alternative to benzoyl peroxide preparations. In one study, 124 patients with mild to moderate acne randomly received either a 5% gel of tea tree oil or 5% benzoyl peroxide lotion to be applied topically every day. After 3 months, both treatments produced a significant improvement in the mean number of both noninflamed and inflamed lesions, although with noninflamed lesions, benzoyl peroxide was found to be more effective. An important finding was that there were fewer reports of side effects (dryness, pruritus, stinging, burning, and skin redness) with tea tree oil (44% vs 79%).15
Common Foot Problems
One researcher concluded, after 6 years of using different concentrations and preparations, that tea tree oil eradicated or improved the symptoms of tinea pedis when used daily by patients at home.4 He also reported that even undiluted forms had little effect on onychomycosis (discussed further in “Fungal Nail Infection”). Diluted tea tree oil in solution was found to reduce foot irritation and promote wound healing with surgical incision in cases of corns, calluses, bunions, and hammer toes, and was extremely effective in diminishing bromhidrosis.
In tinea pedis, one double-blind study found that 10% tea tree oil cream compared quite favorably with the antifungal tolnaftate in relieving symptoms, but was less effective in eliminating the fungi from cultures.5 Specifically, both the tea tree group (24 of 37 patients) and the tolnaftate group (19 of 33 patients) showed significant improvement in the four clinical parameters of scaling, inflammation, itching, and burning, but only 30% of the subjects who applied tea tree oil cream tested culture negative, compared with 85% in the tolnaftate group.
In another double-blind trial, 158 patients with tinea pedis were randomly assigned to receive either placebo or 25% or 50% tea tree oil solution.16 Patients applied the solution twice daily to affected areas for 4 weeks and were assessed after 2 and 4 weeks of treatment. A marked clinical response was seen in 68% of the 50% tea tree oil group and in 72% of the 25% tea tree oil group, compared with 39% in the placebo group. Mycologic cure was assessed by culture of skin scrapings taken at baseline and after 4 weeks of treatment. The mycologic cure rate was 64% in the 50% tea tree oil group compared with 31% in the placebo group. Four (3.8%) patients applying tea tree oil experienced moderate to severe dermatitis that improved quickly upon cessation of the study medication.
Fungal Nail Infection
One study compared the efficacy and tolerability of the topical application of 1% clotrimazole (CL) solution with that of 100% tea tree oil for the treatment of toenail onychomycosis.17 The 117 patients received twice daily applications of either 1% CL solution or 100% tea tree oil for 6 months. Débridement and clinical assessment were performed at 0, 1, 3, and 6 months. Culture specimens were obtained at 0 and 6 months. Each patient’s subjective assessment was also obtained 3 months after the conclusion of therapy. After 6 months of therapy, the two treatment groups were comparable on the basis of culture cure (CL = 11%, tea tree = 18%) and clinical assessment documenting partial or full resolution (CL = 61%, tea tree = 60%). Three months later, about half of each group reported continued improvement or resolution (CL = 55%, tea tree = 56%). These results indicate that topical therapy with tea tree oil, in conjunction with débridement, provides excellent improvement in nail appearance and symptomatology.
Vaginal Infections
Tea tree oil demonstrates germicidal activity against a number of common vaginal pathogens and opportunistic organisms, including Trichomonas vaginalis and Candida albicans.18
A 40% solution of tea tree oil emulsified with isopropyl alcohol and water was found in a clinical study to be highly effective for the treatment of cervicitis, chronic endocervicitis, trichomonal vaginitis, and vaginal candidiasis.18 Weekly in-office treatment (usually four to six were necessary) involved thorough washing of the perineum, labia, and vagina with a suitable scrub (the commercial product pHisoHex was used in the study). After drying, the affected areas were washed with a 1% tea tree oil solution. This was followed by insertion of a tampon (three 4 × 4–inch sponges) saturated with the 40% tea tree oil solution. Patients were instructed to remove the tampon after 24 hours.
 Toxicity
Toxicity
Tea tree oil appears to be extremely safe for use as a topical antiseptic.19 However, it may cause allergic contact dermatitis in some individuals. During a 3-year period, seven patients were seen in an outpatient dermatology clinic in Kona, Hawaii, for contact dermatitis due to the use of commercially available product containing 100% tea tree oil.20 The patients were treating preexisting skin conditions, which included foot fungus, dog scratches, insect bites, and rashes. All patients presented with an eczematous dermatitis. Patch tests indicated that all patients were sensitive to a 1% solution of tea tree oil. It is recommended that individuals apply the oil to a small area of skin before using tea tree oil for the first time so as to avoid the bother of experiencing contact dermatitis over a larger area.
 Drug Interactions
Drug Interactions
Tea tree oil may produce a synergistic effect with other topical antimicrobials. In an in vitro study, tea tree oil and tobramycin in combination produced significantly lower minimal inhibitory concentrations against Escherichia coli and Staphylococcus aureus.21 A similar synergism was demonstrated between tea tree oil and the antifungal compound amphotericin in inhibiting Candida species.22
1. Carson C.F., Hammer K.A., Riley T.V. Melaleuca alternifolia (Tea Tree) oil: a review of antimicrobial and other medicinal properties. Clin Microbiol Rev. 2006;19:50–62.
2. Swords G., Hunter G.L.K. Composition of Australian tea tree oil (Melaleuca alternifolia). J Agric Food Chem. 1978;26:734–737.
3. Humphery E.M. A new Australian germicide. Med J Australia. 1930;1:417–418.
4. Walker M. Clinical investigation of Australian Melaleuca alternifolia oil for a variety of common foot problems. Current Podiatry. 1972;18:30–35.
5. Tong M.M., Altman P.M., Barnetson R.S. Tea tree oil in the treatment of tinea pedis. Australas J Dermatol. 1992;33:145–149.
6. Carson C.F., Riley T.V. The antimicrobial activity of tea tree oil. Med J Aust. 1994;160:236.
7. Feinblatt H.M. Cajeput-type oil for the treatment of furunculosis. J Nat Med Assoc. 1960;52:32–34.
8. Kwieciński J., Eick S., Wójcik K. Effects of tea tree (Melaleuca alternifolia) oil on Staphylococcus aureus in biofilms and stationary growth phase. Int J Antimicrob Agents. 2009;33:343–347.
9. Williamson E.M., Priestley C.M., Burgess I.F. An investigation and comparison of the bioactivity of selected essential oils on human lice and house dust mites. Fitoterapia. 2007;78:521–525.
10. Barker S.C., Altman P.M. A randomised, assessor blind, parallel group comparative efficacy trial of three products for the treatment of head lice in children–melaleuca oil and lavender oil, pyrethrins and piperonyl butoxide, and a “suffocation” product. BMC Dermatol, 2010;10:6. http://dx.doi.org/10.1186/1471-5945-10-6.
11. Groppo F.C., Ramacciato J.C., Simoes R.P., et al. Antimicrobial activity of garlic, tea tree oil, and chlorhexidine against oral microorganisms. Int Dent J. 2002;52:433–437.
12. Vazquez J.A., Zawawi A.A. Efficacy of alcohol-based and alcohol-free melaleuca oral solution for the treatment of fluconazole-refractory oropharyngeal candidiasis in patients with AIDS. HIV Clin Trials. 2002;3:379–385.
13. Bagg J., Jackson M.S., Petrina Sweeney M., et al. Susceptibility to Melaleuca alternifolia (tea tree) oil of yeasts isolated from the mouths of patients with advanced cancer. Oral Oncol. 2006;42:487–492.
14. Satchell A.C., Saurajen A., Bell C., et al. Treatment of dandruff with 5% tea tree oil shampoo. J Am Acad Dermatol. 2002;47:852–855.
15. Bassett I.B., Pannowitz D.L., Barnetson R.S. A comparative study of tea-tree oil versus benzoylperoxide in the treatment of acne. Med J Aust. 1990;153:455–458.
16. Satchell A.C., Saurajen A., Bell C., et al. Treatment of interdigital tinea pedis with 25% and 50% tea tree oil solution: a randomized, placebo-controlled, blinded study. Australas J Dermatol. 2002;43:175–178.
17. Buck D.S., Nidorf D.M., Addino J.G. Comparison of two topical preparations for the treatment of onychomycosis. Melaleuca alternifolia (tea tree) oil and clotrimazole. J Fam Pract. 1994;38:601–605.
18. Pena E.F. Melaleuca alternifolia oil: its use for trichomonal vaginitis and other vaginal infections. Obstet Gynecol. 1962;19:793–795.
19. Hammer K.A., Carson C.F., Riley T.V., et al. A review of the toxicity of Melaleuca alternifolia (tea tree) oil. Food Chem Toxicol. 2006;44:616–625.
20. Knight T.E., Hausen B.M. Melaleuca oil (tea tree oil) dermatitis. J Am Acad Dermatol. 1994;30:423–427.
21. D’Arrigo M., Ginestra G., Mandalari G., et al. Synergism and postantibiotic effect of tobramycin and Melaleuca alternifolia (tea tree) oil against Staphylococcus aureus and Escherichia coli. Phytomedicine. 2010;17:317–322.
22. Rosato A., Vitali C., Gallo D., et al. The inhibition of Candida species by selected essential oils and their synergism with amphotericin B. Phytomedicine. 2008;15:635–638.