Chapter 6 Mega-OATS
Introduction
Large osteochondral defects in the weight-bearing zone of the medial or lateral femoral condyle, especially in young patients, create a challenge for orthopaedic surgeons. Addressing both the cartilaginous and the osseous defect, mosaicplasty represents a modified technique of the conventional osteochondral autologous transplantation system (OATS) technique by transplantation of multiple OATS plugs into the defect area.1,2 However, this technique is limited because of the availability of the plugs at the donor site. Additionally, a primary stability of multiple plugs as well as restoration of the anatomical congruence at the cartilaginous surface level is technically demanding and often infeasible.
In the 1960s and 1970s, the posterior femoral condyle of the knee was already recognized as a potential donor site for osteochondral tissue.3,4 The transfer of the posterior femoral condyle using an anterior approach was started in the 1990s at our department at klinikum Rechts der Isar in Munich, Germany. The autologous Mega-OATS procedure is a technical advancement of the posterior femoral condyle transfer.5,6 Contrarily, the allogenic Mega-OATS technique illustrates an alternative procedure sparing the posterior femoral condyle as the donor site.7 In both autologous and allogenic Mega-OATS techniques, an almost anatomical restoration of the condyle curvature as well as an optimal congruence to the adjacent cartilaginous surface can be achieved. Nevertheless, comorbidities such as malalignment and ligamentous instabilities must be addressed before or ideally simultaneously with the Mega-OATS procedure.
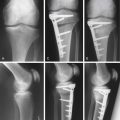
Isolated Mega-OATS procedures as well as Mega-OATS procedures combined with additional procedures (malalignment correction, ligamentous stabilization, meniscus surgery, etc.) were clinically and imaging based (radiological, MRI) reevaluated in the short- and mid-term follow-up. Overall, the reevaluations demonstrated a considerable improvement regarding function, pain reduction, and swelling as well as resumption of sporting activities compared to preoperatively.5,6,8,9
Indications
The indication criteria of the Mega-OATS procedure include the following:
Contraindications
The contraindication criteria for the Mega-OATS technique include the following:
Surgical Technique
Anesthesiology and Positioning
Exposure
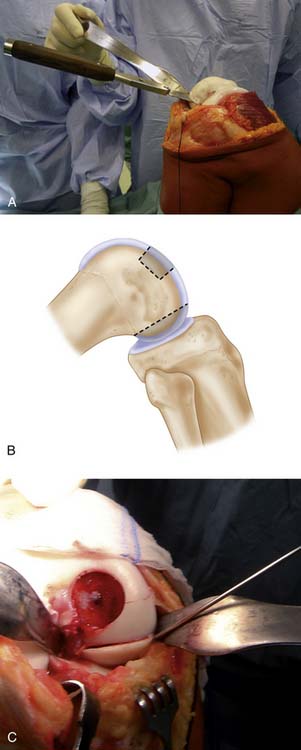
In a maximal flexed knee position, the border of the osteochondral defect at the medial or lateral femoral condyle is marked using a sterile pen (Fig. 6-2).
Mega-OATS Harvest, Preparation, and Implantation
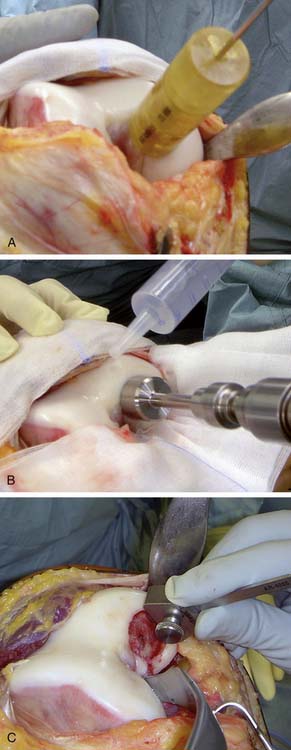
The defect size is measured with a ruler or the Mega-OATS template (Fig. 6-3, A).
A K-wire is perpendicularly positioned in the center of the lesion, serving as a guidance device for the hollow drill (diameter 20 to 35 mm) (Fig. 6-3, B).
The hollow drill creates a stable osteochondral skirt around the defect.
A trephine, equally sized as the hollow drill, is used for preparation of the recipient socket.
Sterile pads may be utilized to avoid dispersion of drilling debris into the joint.
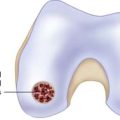
The depth of the socket is defined by the extension of the osseous defect or the necrotic zone. Intraoperatively, the correct drilling depth is accomplished by occurrence of bleeding of the subchondral surfaces within the defect socket. Then, the size of the transplant cavity is measured with the Mega-OATS depth measurement guide (Fig. 6-3, C).
In detail, the direction of the posterior femoral condyle osteotomy is parallel or in elongation to the posterior cortex of the femoral diaphysis (Fig. 6-4, A-B).
To secure the posterior femoral condyle against transplant slippage, the posterior condyle may be temporarily fixed with a K-wire before completion of the osteotomy (Fig. 6-4, C).
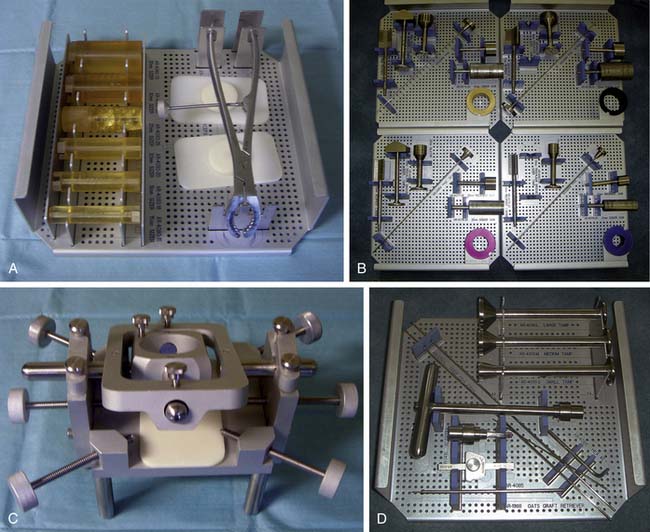
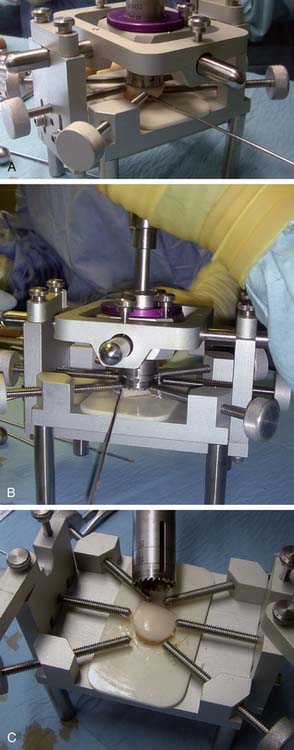
The Mega-OATS cylinder is harvested out of the removed posterior femoral condyle using a specially designed Mega-OATS workstation. The osteotomized posterior femoral condyle is fixed by screws at the workstation (Fig. 6-5, A).
For optimal harvest of the Mega-OATS cylinder, the guiding device of the workstation is adapted perpendicularly to the cartilage surface of the transplant (Fig. 6-5, B).
Then the Mega-OATS cylinder is cut out of the transplant using a core drill (Fig. 6-5, C). Usually, a diameter of the Mega-OATS cylinder between 20 to 35 mm can be achieved depending of the size of the osteochondral defect and the height of the patient.
The prepared Mega-OATS cylinder is finally implanted in the recipient socket following determination of the socket depth. Because the diameter of the Mega-OATS cylinder is 0.4 to 0.5 mm larger than the diameter of the defect socket, a press-fit technique is usually feasible (Fig. 6-6).
Comorbidities
Ligamentous instability should also be addressed at the same time to avoid shear forces at the osteochondral transplant. Separate smaller osteochondral lesions may be treated with additional OATS plugs.
Postoperative Management
Unloading of the operated lower extremity for 6 weeks postoperatively is mandatory.
Continuous passive motion therapy and isometric muscle strengthening are concomitantly recommended.
Postoperative Imaging
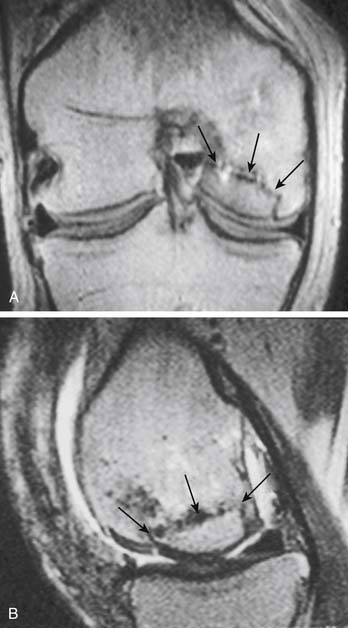
Postoperative standard radiography of the knee joint is performed after removal of the drain. A routine MRI postoperatively is not necessary but may be indicated in prolonged postoperative pain and swelling as well as for evaluation of osseous ingrowth, chondral congruency, and graft viability (Fig. 6-7, A-B). For special evaluation of graft viability, MRI may be enhanced using an intravenous fluid application.
1. Hangody L., Kish G., Karpati Z., Szerb I., Udvarhelyi I. Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A preliminary report. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):262-267.
2. Hangody L., Ráthonyi G.K., Duska Z., Vasarhelyi G., Fules P., Modis L. Autologous osteochondral mosaicplasty. Surgical technique. J Bone Joint Surg Am. 2004 Mar;86-A(Suppl 1):65-72.
3. Müller W. Osteochondrosis dissecans. In: Hastings D.E., editor. Progress in orthopaedic surgery. New York: Springer; 1978:135-142.
4. Wagner H., [Surgical treatment of osteochondritis dissecans, a cause of arthritis deformans of the knee.] Rev Chir Orthop Reparatrice Appar Mot 1964(50):335-352.
5. Agneskirchner J.D., Brucker P., Burkart A., Imhoff A.B. Large osteochondral defects of the femoral condyle: press-fit transplantation of the posterior femoral condyle (MEGA-OATS). Knee Surg Sports Traumatol Arthrosc. 2002 May;10(3):160-168. Epub 2001 Dec 13
6. Brucker P., Agneskirchner J.D., Burkart A., Imhoff A.B. Mega-OATS. Technik und Ergebnisse. Unfallchirurg. 2002 May;105(5):443-449.
7. Karataglis D., Learmonth D.J. Management of big osteochondral defects of the knee using osteochondral allografts with the MEGA-OATS technique. Knee. 2005 Oct;12(5):389-393.
8. Braun S., Minzlaff P., Hollweck R., Wortler K., Imhoff A.B. The 5.5-year results of MegaOATS–autologous transfer of the posterior femoral condyle: a case-series study. Arthritis Res Ther. 2008;10(3):R68.
9. Brucker P.U., Braun S., Imhoff A.B. [Mega-OATS technique–autologous osteochondral transplantation as a salvage procedure for large osteochondral defects of the femoral condyle]. Oper Orthop Traumatol. 2008 Sep;20(3):188-198.
10. König U., Imhoff A.B. Arthroskopie-qualifizierte Stadieneinteilung der osteochondralen Läsion (OCL) am Knie. Arthroskopie. 2003;16:23-28.