Chapter 11 Median Nerve
Overview
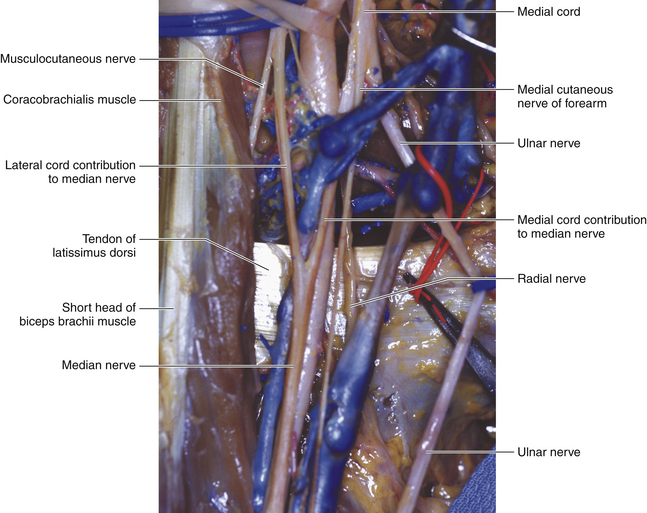
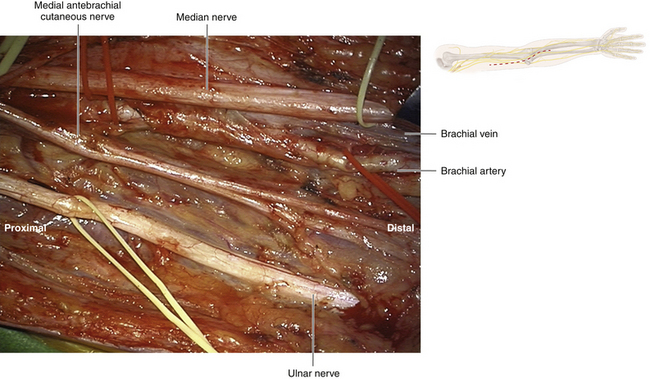
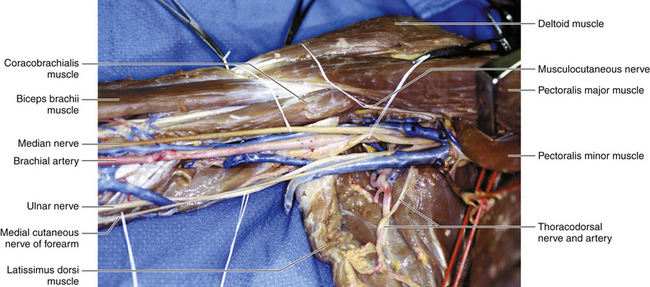
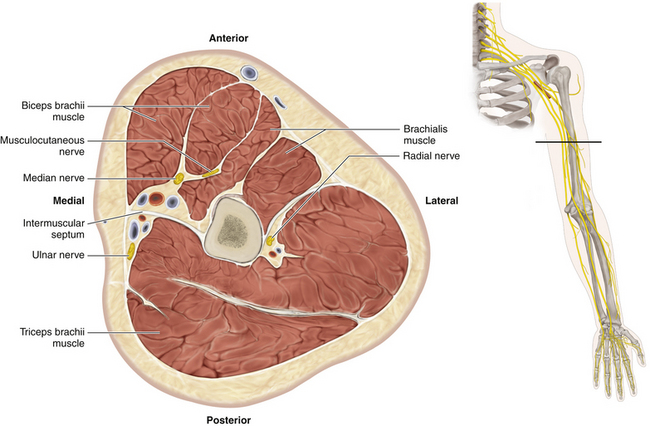
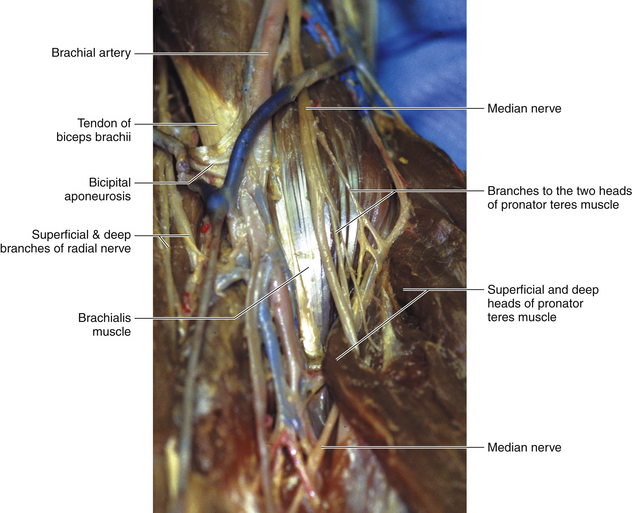
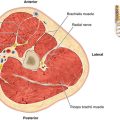
• The median nerve is derived from medial and lateral heads, so named according to their cord of origin. The medial cord contributes primarily motor fibers, and the lateral primarily sensory. The two heads clasp the brachial artery where the medial head runs across the front of the vessel, and the median nerve maintains this close relationship with the artery throughout the arm (Figures 11-1 and 11-2).
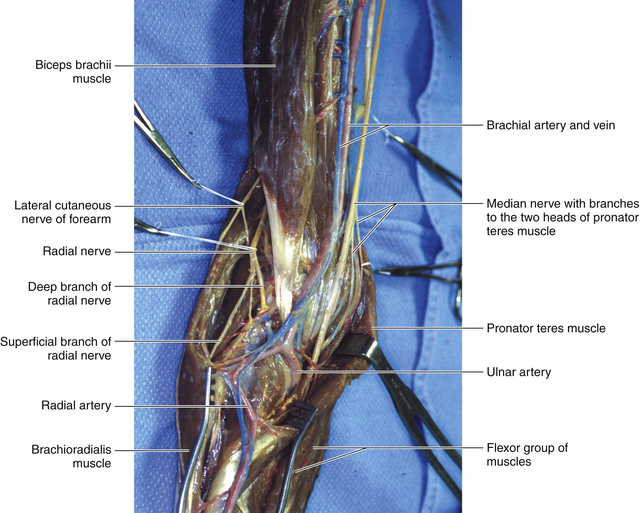
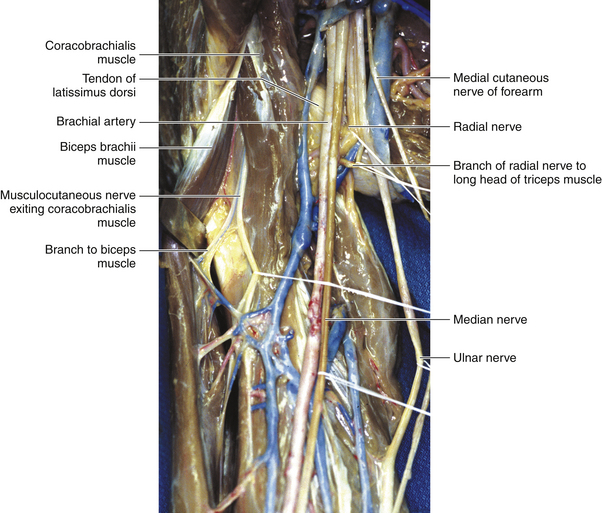
• The nerve runs at first lateral and later medial to the artery. The transition occurs at the level of the insertion of the deltoid. The ulnar artery runs posterior to the median nerve soon after the vessel is formed (Figure 11-3).
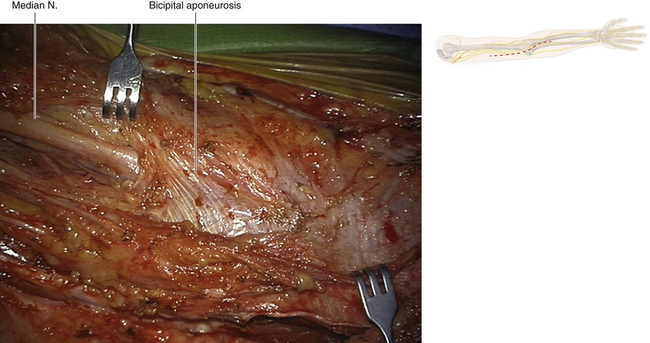
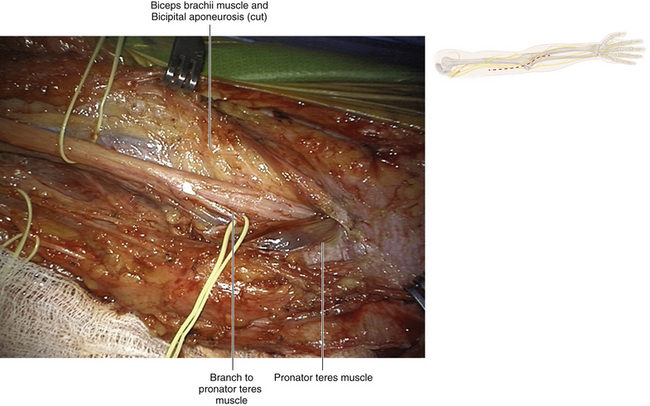
• Throughout its course, the nerve is deep to the investing fascia, which at the elbow is thickened by the bicipital aponeurosis (Figure 11-4).
Surgery
• The skin incision in the arm is placed over the course of the nerve. The pulsating brachial artery is the guide.
• The surgeon must distinguish the median, ulnar, radial, and cutaneous nerves in the proximal arm. The median nerve is lateral to and closely applied to the artery (Figures 11-5 and 11-6).
• Pathology frequently results in close adhesion of the adjacent nerve and artery. In the majority of cases, the nerve can be carefully separated by sharp dissection (Figure 11-7).
• If the surgeon encounters more than minimal adherence of the nerve to the artery, the artery must be dissected out both proximal and distal to the point of nerve injury. Tapes are loosely passed around the vessel at those points and serve as a guide to vascular occlusion, should this be required.
• Vascular clamps must be part of the peripheral nerve instrumentation set and the operating room nurse must know where a full vascular set is available, should this be required.
• In the event of hemorrhage, pressure is applied calmly and accurately, compressing the artery against the humerus. The assistant then applies the vascular clamps in an accurate and unhurried fashion, at the previously prepared sites proximal and distal to the arterial injury. Done in this manner, there is no further injury to the nerve or vessel; both, however, can easily occur if the surgeon has not prepared for brisk hemorrhage ahead of time.
• It is difficult to gain extra length when operating on the median nerve in the arm, so grafts are frequently required.
• The musculocutaneous nerve runs between the two heads of the coracobrachialis. A phylogenetically degenerate third head may persist and may compress the median nerve. A downward and medially pointing bone spur may be present on the anterior aspect of the distal humerus. This will be missed on a routine anteroposterior x-ray film but may be seen in profile on an oblique view. A ligament runs from this spur to the medial epicondyle (ligament of Struthers) and the ligament may compress the median nerve. (This situation is similar to a cervical rib, where the band from the tip of the rib is the culprit, rather than the rib itself.)
• Only on rare occasions is there a median branch communicating with the ulnar nerve (an arm-level Martin-Gruber anastomosis) or a branch from the median nerve to an antebrachial cutaneous nerve.
• This is in contrast to the frequent back-and-forth communications between the lateral and medial cords, and sometimes the posterior cord, as the median nerve is being formed proximally.
The Elbow and Proximal Forearm
• The surgeon must understand the anatomy and function of all forearm muscles so that an accurate clinical examination can be conducted. In addition, some specific points need to be stressed to allow the precise and accurate conduct of surgery.
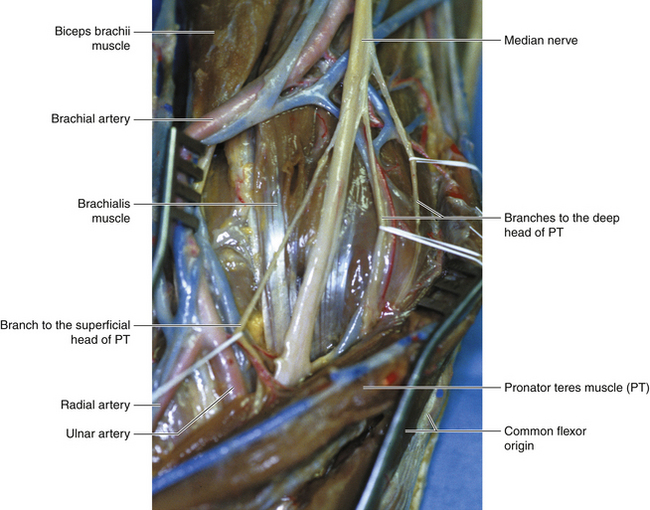
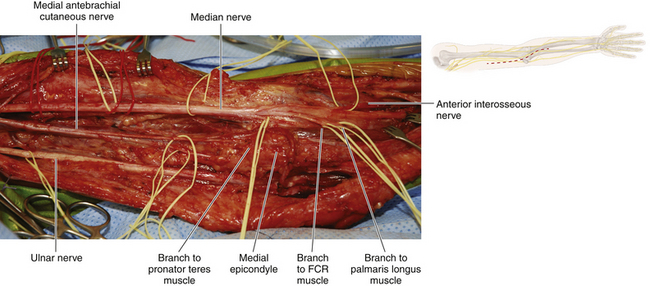
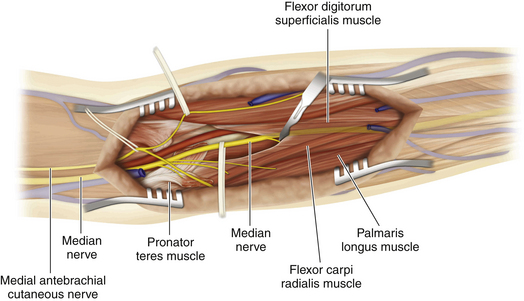
• The two heads of the pronator teres (PT) insert into the radius by a common tendon. The upper lateral border of the superficial head of PT is clearly defined (Figure 11-8). The median nerve in the distal arm and cubital fossa lies medial to the biceps and its tendon and medial to the brachial artery (Figure 11-9). The nerve is resting on the brachialis. The median nerve runs between the two heads of PT; the muscle is supplied by a specific branch of the median nerve, which frequently leaves the main trunk more proximally. The fascia superficial to the muscle is thickened by the bicipital aponeurosis.
• The flexor carpi radialis (FCR) arises from the common flexor head and transforms into its large tendon at the midforearm level. The tendon crosses the median nerve superficially en route to its insertion, lateral to the median nerve at the wrist.
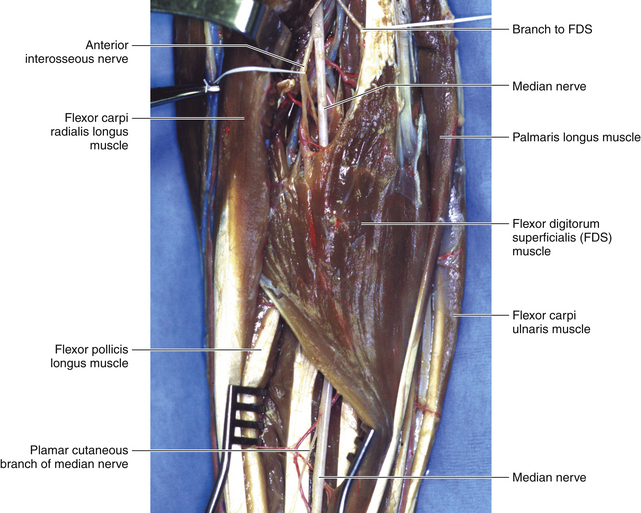
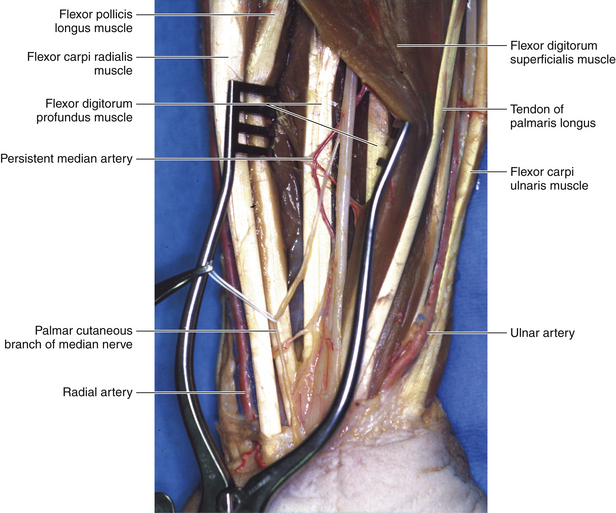
• The palmaris longus (PL) is a small muscle with a long tendon, which inserts into the palmar aponeurosis. The tendon is stuck to the superficial surface of the flexor retinaculum. Proximal to the wrist, the median nerve lies deep to the interval between the FCR and the PL (Figure 11-10).
The Median Nerve Passing Through the Pronator Teres
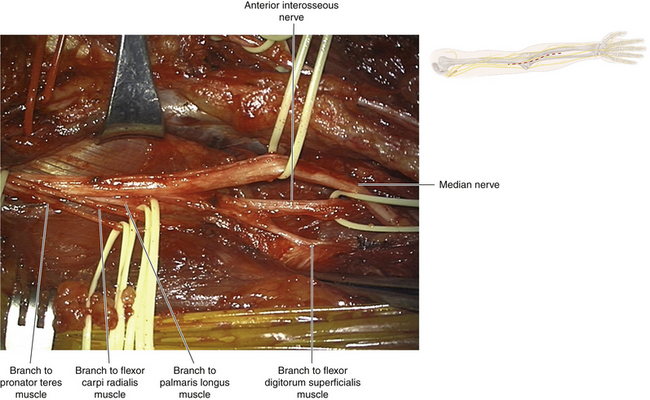
• After giving off a few branches to the pronator teres, the median nerve passes between the two heads of the PT and then crosses the ulnar artery anteriorly (Figure 11-11).
• Emerging from the distal border of the PT, the median nerve passes deep to an arch created by the two heads of the flexor digitorum superficialis (FDS) (Figure 11-12).
• The FDS arises from two heads on the radial and ulnar side of the forearm. The arch formed between the two heads covers the median nerve as it leaves the lower border of the PT. The nerve is stuck to the deep surface of the FDS and escapes lateral to the FDS tendons in the distal forearm. (Figure 11-13)
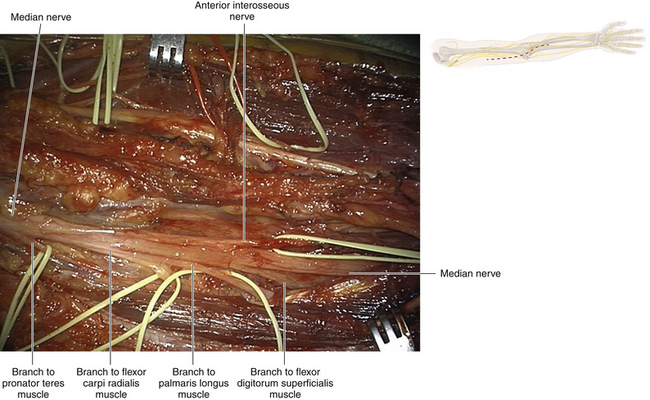
• The anterior interosseous nerve arises laterally from the median nerve.
• Below the PT and FDS, the course of the median nerve in the forearm continues in a straight line into the wrist, on the radial side of the tendon of the PL.
• Proximal to the anterior interosseous branch, the median nerve supplies the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis (Figure 11-14).
Anterior Interosseous Nerve in the Forearm
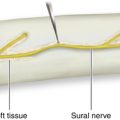
• The anterior interosseous nerve, which arises immediately distal to the FDS arch, is the largest muscular branch of the median nerve.
• It lies at first between the flexor pollicis longus and the flexor digitorum profundus, which are innervated by it.
• Accompanied by the anterior interosseous artery, the anterior interosseous nerve descends in the forearm on the surface of the interosseous membrane.
• The nerve passes deep to and supplies the pronator quadratus muscle.
Surgery at the Elbow and Proximal Forearm
• The median nerve is found at the elbow joint, using the biceps tendon and the brachial artery as landmarks. The overlying fascia is thickened by the bicipital aponeurosis, which is incised to display the nerve.
• This constant point of identification is useful if trouble is encountered in displaying the median nerve in the arm or in displaying the median nerve in the proximal forearm. The nerve is found at the elbow and followed to the point of pathology (Figure 11-15).
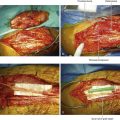
• The surgeon divides the superficial head of the PT in the line of the nerve, being careful of the median nerve branches to that muscle.
• The surgeon next encounters the upper border of the arch between the proximal heads of the FDS. This structure is divided vertically and continued distally, separating muscle fibers (the surgeon is aware that the median nerve is stuck to the undersurface of FDS) (Figure 11-16).
• The median nerve is gently tented forward; this helps identify the anterior interosseous nerve, which is running backward toward the interosseous membrane (Figure 11-17). (Inexperienced surgeons may have trouble finding this nerve, because they usually do not dissect sufficiently distally on the median nerve under the proximal FDS.)
• In the distal forearm, the landmarks are the large tendon of the FCR and the smaller tendon of the PL (see Figure 11-13). The surgeon is constantly reminded of the fact that the tendon of flexor digitorum profundus to the index finger and the tendon of the PL each may mimic the appearance of the median nerve.
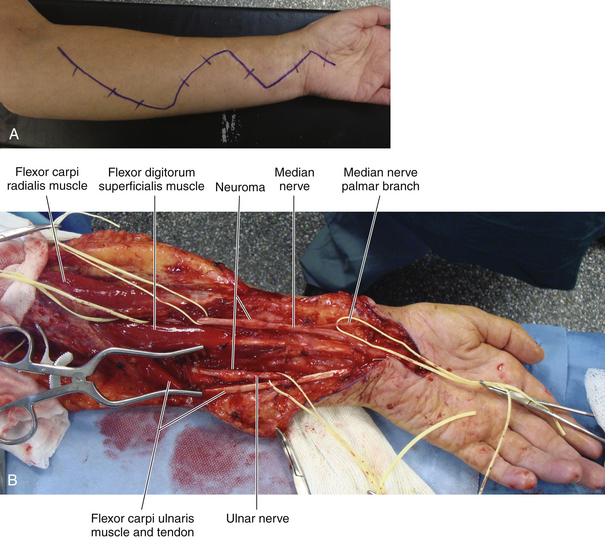
• In midforearm nerve injuries, the median nerve may have to be identified both proximally at the PT and distally at the carpal tunnel so that the operation may proceed from both sides toward the pathology (Figure 11-18).
• A rare median nerve variant is a Martin-Gruber anastomosis, which involves anterior interosseous nerve muscle-destined fibers being carried by the ulnar nerve through the olecranon notch area and from there to the proximal forearm.
• If the median nerve injury is in the distal forearm, the transverse carpal ligament should be divided. This prevents any super added entrapment, and also enables the surgeon to identify the distal stump of the median nerve with certainty (see Figure 11-18).
• The palmar cutaneous branch of the median nerve, a purely sensory nerve, arises approximately 2 or 3 cm proximal to the distal wrist crease.
• It descends along the ulnar side of the flexor carpi radialis, adherent to the undersurface of the fascia.
• At the proximal edge of the transverse carpal ligament, the palmar cutaneous branch deviates laterally and may enter its own tunnel within the ligament.
• Dividing into medial and lateral branches, it becomes subcutaneous to supply the skin of the proximal two fifths of the palm on the radial side and the thenar eminence.
Wrist Level
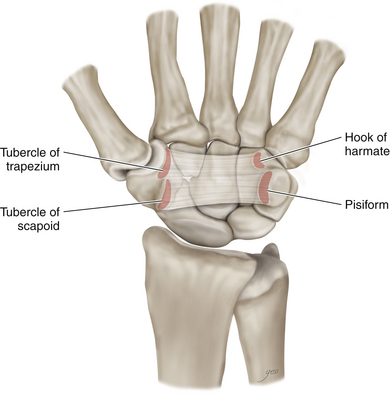
• The flexor retinaculum (FR) has four bony attachments: (1) the tubercle of the scaphoid; (2) the ridge of the trapezium; (3) the pisiform; and (4) the hook of the hamate. The FR has a distinct horizontal distal border (Figure 11-19).
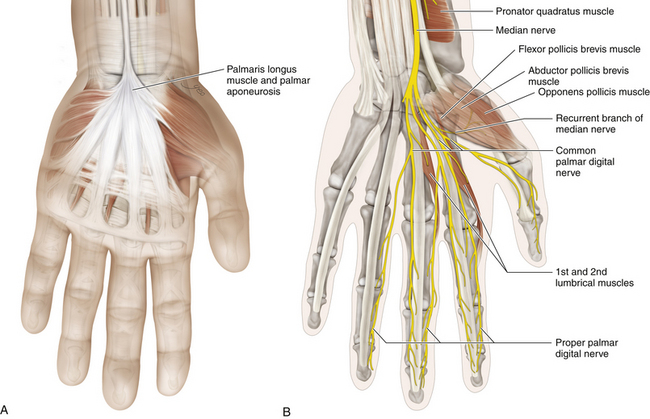
• The tendon of PL is immediately superficial to the FR and expands distally into the palmar aponeurosis.
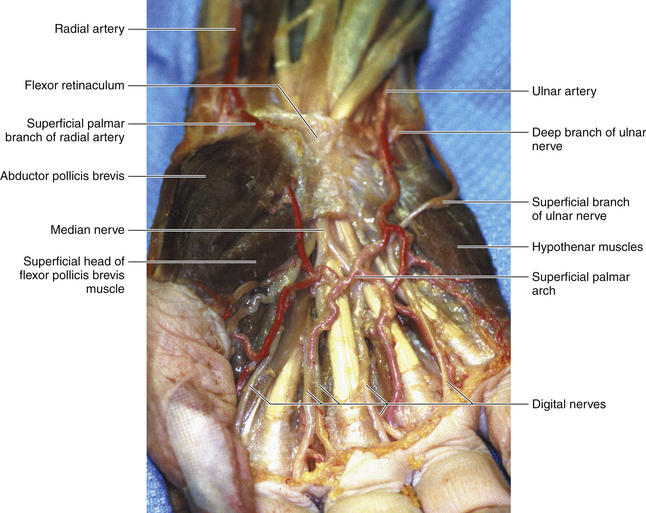
• The superficial palmar arch is surrounded by fat and is positioned just distal to the distal border of the FR (Figure 11-20).
• Proximal to the wrist, the median nerve lies deep to the interval between the FCR and PL tendons (note that the PL may rarely be absent). The median nerve then runs deep to the FR, accompanying the flexor tendons, in the carpal tunnel.
• The median nerve enters the palm of the hand running under the transverse carpal ligament. In the carpal tunnel, the nerve lies lateral to the FDS to the middle finger and medial to the FCR (which is in its own compartment) (Figure 11-21).
• Distal to the FR, the nerve divides into the recurrent motor branch and sensory digital nerves. The recurrent motor branch to the thenar muscles arises from the radial surface of the median nerve. The recurrent branch lies between the fascia and the muscle of the thenar eminence (Figure 11-22).
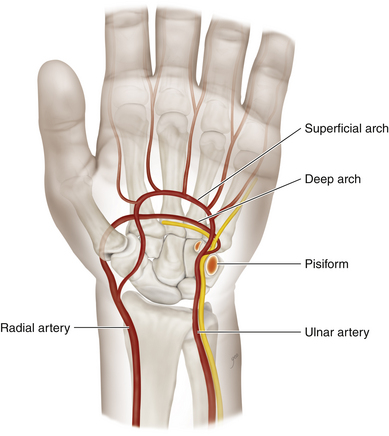
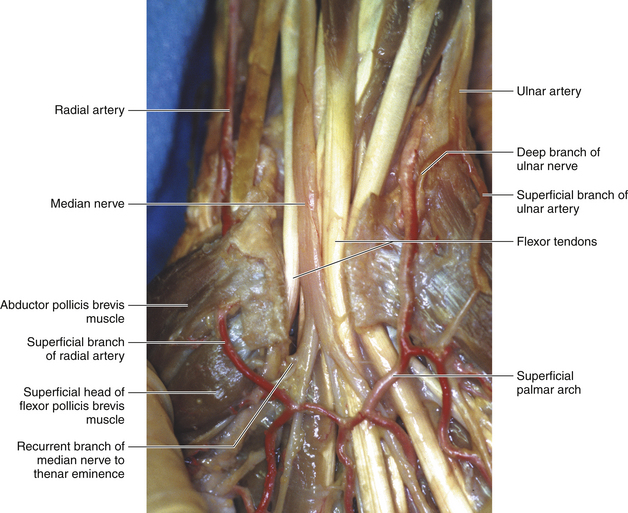
Figure 11-20 The ulnar artery and radial artery contribute to the superficial and deep palmar arches.
Digital Branches of the Median Nerve in the Palm
• In the palm, the nerves are dorsal to the superficial palmar arch and palmar to the flexor tendons. (Figure 11-23)
• The radial division divides into the common digital nerve to the thumb and the proper digital nerve to the radial side of the index finger.
• The ulnar division branches into the common digital nerve to the thumb and the proper digital nerve to the radial side of the index finger.
• The ulnar division branches into the common digital nerves of the second and third web spaces.
• The digital nerves lie dorsal to the superficial palmar arch and palmar to the flexor tendons.
• After division at the level of the metacarpal necks, the digital nerves lie superficial to the digital arteries.
• The nerves enter the fingers between the deep and superficial transverse metacarpal ligaments, maintaining this relationship.
Surgical Technique
• A variety of procedures is available for treatment of carpal tunnel syndrome. Three of these procedures are described.
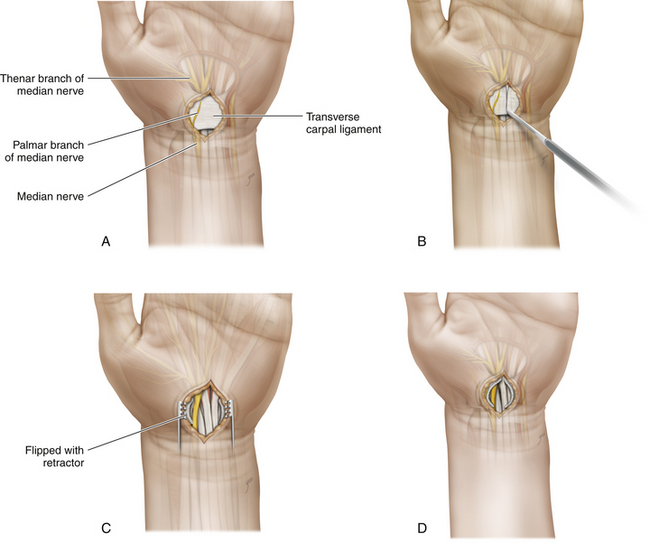
Minimal Access
1. The patient’s arm is positioned in abduction and the incision site is disinfected.
2. A transverse skin incision of approximately 1.5 cm in length is made at the site previously marked at the wrist, ulnar to the palmaris longus tendon.
3. The palmar aponeurosis is split longitudinally, exposing the fascia.
4. To enter the carpal tunnel, a synovial elevator is inserted ulnar to the median nerve, and a dissector is advanced under the transcarpal ligament to prepare the path for the endoscope and mobilize the nerve.
5. The endoscopic device is placed under the transverse carpal ligament in the direction of the fourth finger in order to see the operative field, especially the distal end of the carpal tunnel.
6. The carpal ligament is then released.
7. The endoscope is reinserted to confirm complete division of the ligament.
8. An interrupted 4-0 suture is made.
9. The tourniquet is deflated and external compression is applied for several minutes to minimize the postoperative bleeding risk.
Standard Open Procedure
1. In standard carpal tunnel cases, the objective is to divide the FR, thus opening the carpal tunnel and relieving the entrapment of the median nerve. The four bony points of attachment of the FR can be palpated in one’s own hand, so the extent of the retinaculum is easily appreciated by the surgeon.
2. The incision, placed over the FR, runs from the flexor wrist crease to the level of the lower border of the outstretched thumb. The skin incision is usually drawn with a marking pen and extends along the course of the ulnar side of the lifeline of the palm. If the skin lifeline branches or is eccentric, an up-and-down or vertical incision is directed toward the radial side of the ring finger (fashioned to avoid the palmar sensory branch).
3. Before making the incision, the palm and proximal skin are infiltrated with local anesthetic without epinephrine. An initial wheal is placed on the looser palmar skin with a No. 25 needle, and then a larger No. 23 needle is used to infiltrate the proximal and distal soft tissues through this wheal and then again through the skin that is already anesthetized by the local anesthetic.
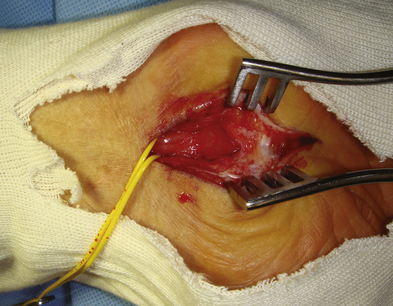
4. The skin cut is retracted by a self-retaining retractor. The incision is deepened through the fat until the very characteristic “gritty” sensation is experienced when the blade cuts into the superficial elements of the FR (Figure 11-24).
5. The surgeon gently cuts the ligament, using the curved edge of the scalpel in repetitive strokes.
6. The cut FR will spring apart under the influence of the self-retaining retractor, and it is essential to check that the distal border of the FR has been totally divided (Figure 11-25).
7. The palmar arterial arch is usually not seen, but the surgeon should be aware that it is a few millimeters away.
8. The thenar recurrent motor branch has a variable origin from the radial side of the nerve and can travel in a forward, oblique, transverse, or, more commonly, truly recurrent (thus the name) fashion to innervate the median nerve-innervated thenar muscles.
9. Neither the main median nerve, the recurrent branch, or the digital branches need be dissected.
10. The FR is not closed, but the skin is carefully closed, usually by interrupted mattress sutures.
11. A dressing is placed over the surgical wound.
12. A “boxing glove” type of dressing is then applied. It is preferable to leave the fingers and thumb relatively free, so that the patient can be encouraged to flex and extend them in the early postoperative hours and days.
13. A sling is fashioned that holds the hand higher than the elbow and is worn for 2 days.
Repeat or Complex Cases
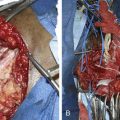
• The procedure should be conducted in the main operating room with appropriate magnification and microsurgical facilities.
• The previously described incision is extended distally. The distal end of the FR is inspected. If this structure had not been completely divided at the previous operation, it is divided now. If the nerve is intact, nothing further need be done and the case is terminated.
• If direct injury to the median nerve is noted, the incision is extended proximally and the investing fascia of the distal forearm is divided over the course of the nerve. The nerve injury is then managed appropriately after visual and electrophysiological assessment of the injury.