CHAPTER 12 Medial Unicompartmental Knee Replacement
Cementless Options
 Cementless fixation in unicompartmental knee replacement has the theoretical potential of very long-term biologic fixation.
Cementless fixation in unicompartmental knee replacement has the theoretical potential of very long-term biologic fixation.Rationale
The development of cementless UKR has mirrored that of total knee replacement (TKR), with the use of porous coatings, with and without hydroxyapatite, and, in some designs, the addition of cancellous screw augmentation. All designs have utilized a keel on the tibial component, although the shape, size, and direction have shown considerable variation (Figs. 12–1 and 12–2). The femoral component has usually mirrored the cemented equivalent for each design, although those femoral designs with a single peg had a second peg added for rotational stability.
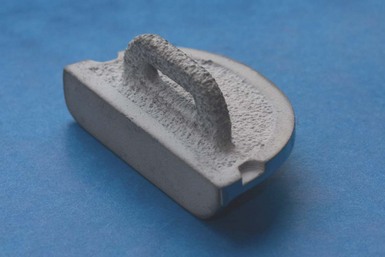
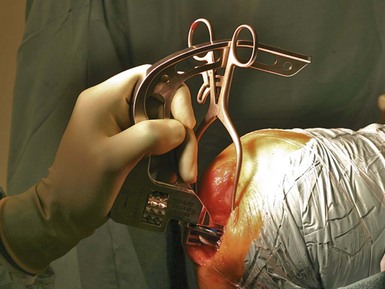
Figure 12–1 A cementless Oxford tibial component demonstrating a porous titanium layer with a hydroxyapatite coating.

(Photograph courtesy of Jean-Alain Epinette.)
One of the first advocates of cementless UKR was Jean-Alain Epinette,1 who designed and developed a hydroxyapatite-coated tibial component. This component differed from most designs by employing a horizontal keel that slotted beneath the tibial spines, thus maintaining bone stock beneath the tibial tray. In addition, there were cancellous screws to augment the initial fixation. Kaiser and Whiteside further highlighted the importance of initial stability in 1990, with a cadaveric in vitro study demonstrating the additional stability provided by cancellous screws in a unicompartmental tibial component, compared with a posteriorly angled peg.2
Cementless fixation in UKR has mainly been used in the few centers that are strong advocates of unicompartmental surgery. The latest reports from the Australian and New Zealand joint registries show that cementless UKR accounts for 11% and 6% of all UKR procedures, respectively.3,4 The Swedish register reported that all the UKRs performed in 2009 had both components cemented.5 Neither the National Joint Registry of England and Wales nor the Canadian registry gives information regarding fixation method for UKR.6,7
Although the presence of thin, nonprogressive, radiolucent lines (Fig. 12–3) has long been recognized in knee arthroplasty, with no associated increase in failure rate, the exact cause and effect of these lines is still unknown. There is, however, a perception that a radiolucent line is indicative of suboptimal fixation. The incidence of radiolucency differs beneath different implants, suggesting that the mechanical environment is important in their development. Forsythe et al.8 reported an incidence of over 50% with the cementless Whiteside Ortholoc II UKR, whereas Pandit et al.9 reported just 7% of cementless Oxford tibial components had a partial radiolucency, with none with a full radiolucency. There is also a reported increase in incidence of radiolucent lines with cemented Oxford components compared to the cementless version.9 There is no clear consensus on the role or importance of thin (≤1 mm), stable, so-called physiologic radiolucent lines, although there is evidence that they are not associated with either loosening or a decrease in clinical outcome scores. However, the greatly reduced incidence in cementless UKR is encouraging and suggests good bony fixation (Fig. 12–4). The Oxford UKR is particularly suited to cementless fixation because of the fully mobile bearing. The bearing movement causes a marked reduction in shear forces being transmitted through the tibial tray, and therefore the tray is mostly subjected to compression. This is an almost ideal mechanical environment for cementless fixation. Radiostereometric analysis studies of cementless fixation in TKR have shown a consistent pattern of migration, which differs from cemented fixation. Cemented components usually demonstrate continuous early migration, but the magnitude is small and stability is achieved by 2 years. In contrast, cementless components usually migrate a larger amount in the first few months before stabilizing. Onsten and Carlsson have demonstrated a reduction in the movement between 1 and 2 years postoperatively with the addition of a layer of hydroxyapatite to a porous-coated PFC tibial component.10,11 Likewise, Regner et al. demonstrated the reduction in maximum total point movement at 5 years in the Freeman-Samuelson TKR tibial component with the addition of hydroxyapatite to the undersurface.12
Indications
The indications for UKR are controversial and vary according to the surgeon’s philosophy. At Oxford, our view is that there should be full-thickness cartilage loss on both the medial tibial plateau and femoral condyle (bone-on-bone osteoarthritis), any intra-articular varus deformity should be correctable, and the anterior cruciate ligament (ACL) should be intact. Patello-femoral joint damage is ignored unless there is severe damage laterally. Cartilage damage on the lateral femoral condyle is permissible provided there is full-thickness cartilage present on a valgus stress radiograph and there is no full-thickness loss centrally. Full-thickness damage on the medial side of the lateral femoral condyle is not a contraindication.13 We do not consider age, gender, activity level, or Body Mass Index to be contraindications. These indications are our routine for both cemented and cementless UKR. Bontemps also noted that the indications for cemented and cementless UKR are the same; however, due to cost saving, he favors cemented fixation in the elderly.14 The suitability of cementless UKR in cases of osteonecrosis or areas of bone loss is less easily described. The consensus in our group is that, if the knee is suitable for cemented UKR once the bony surfaces are prepared, then cementless UKR is also indicated. Our rationale for this is based on evidence that one does not require total bony ingrowth to maintain implant stability and therefore, if the bony surface can support the implant, then either fixation method is acceptable. Epinette’s group demonstrated implant stability in cementless UKR when the amount of bony contact between tibia and component was between 38% and 52%1 (Fig. 12–5).
Setup And Equipment
As with all arthroplasty surgery, the patient setup is of paramount importance. The patient should be set up as for routine medial unicompartmental knee arthroplasty. We recommend the use of a secure leg support, placed at midthigh, to allow the leg to hang and flex fully during surgery and to avoid pressure on the popliteal structures when fully flexed (Fig. 12–6). The Oxford cementless UKR uses the standard equipment trays in addition to the cementless tray. The specialist cementless tray includes instruments and trials specific for the cementless procedure. It contains cementless femoral trials, tibial templates with narrower keel slots, a narrower keel slot pick, and a cementless tibial component introducer. It is essential to use a narrower keel slot saw blade (Synvasive, Reno, NV). The keel slot width is of paramount importance, and therefore particular care needs to be taken when cutting the slot. The narrow keel slot pick also allows clearance of the keel slot without widening it unnecessarily. While the femoral component does not require any special equipment, implantation of the tibial component requires a specific introducer (Fig. 12–7). The introducer for implanting the Oxford tibial tray allows accurate placement of the tray, ensuring it is placed far enough back on the plateau before release and subsequent final seating. This facilitates firm seating on the posterior cortex and prevents anterior overhang.
Approach
Initially the Oxford UKR was implanted through a long midline incision as used for TKR. The Phase 3 instrumentation was introduced to allow the use of a short medial incision. Clinical studies have demonstrated that patients make a quicker recovery postoperatively and have equal outcome scores.15–18 Therefore, the Oxford cementless UKR utilizes a short medial incision, from the medial pole of the patella to the tibial tubercle, as per the standard approach for cemented arthroplasty. Although there are advantages to a shorter incision, adequate exposure is important and the incision must be long enough to allow adequate inspection of the other compartments, retraction of the patella, and excision of osteophytes. The anteromedial corner of the tibia should be exposed to allow seating of the tibial cutting jig and exposure, and subsequent removal, of any osteophytes. Ligaments are never released, and care is taken to protect the medial collateral ligament (MCL). A specific retractor has been designed to help protect the MCL. The patella should not be inverted but can be retracted laterally. Introduction of a femoral intramedullary rod is helpful for alignment of the femoral component, as well as acting as an effective patellar retractor. Once the decision to proceed with UKR has been made, all osteophytes around the medial femoral condyle, intracondylar notch, and anterior aspect of the medial tibial plateau should be removed. There is often an osteophyte anterior to the insertion of the ACL.
Postsurgical Follow-Up
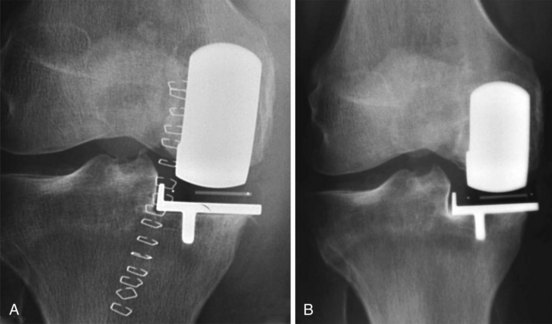
Before discharge, patients have routine radiographs with the anteroposterior view taken parallel to the tibial tray, allowing assessment of the component-bone interface. The lateral view is perpendicular to the femoral component, allowing assessment of bony contact around each peg. Using carefully screened radiographs enables proper evaluation of the interfaces and allows comparison with subsequent radiographs. The accuracy of detecting radiolucent lines, and hence assessment of whether they are progressive, is dependent on the reproducible acquisition of radiographs. The incidence of radiolucent lines beneath the cemented tibial component in Oxford UKR is approximately 62%.19 However, the incidence in cementless Oxford UKR is markedly reduced at 1 year, with only 7% having a partial radiolucency and none having a complete radiolucency.9 Radiographs taken in the first few days after surgery sometimes demonstrate a thin radiolucent line beneath the tibial tray (Fig. 12–8A). This is indicative of the tray not being fully seated at the time of surgery. However, with normal postoperative rehabilitation the radiolucent line disappears and the tray becomes securely seated on the tibial plateau (Fig. 12–8B).
Clinical Results
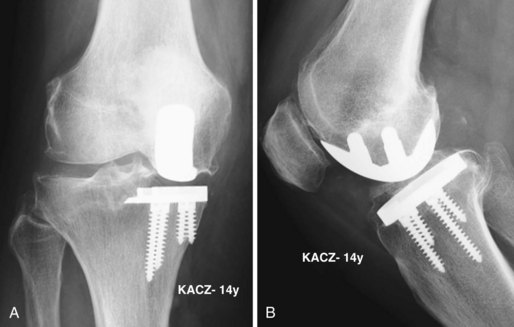
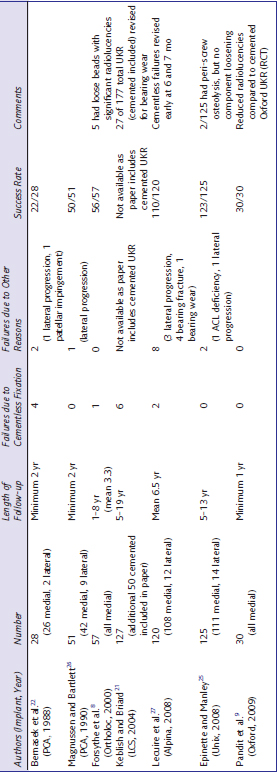
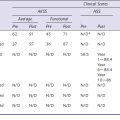
Clinical results of cementless UKR are not commonly reported, and those reports evident in the literature are usually short series. A single randomized, controlled trial of cemented versus cementless UKR at Oxford has shown no difference in clinical outcome, and a reduced incidence of radiolucency with cementless fixation, at 2 years.20 There have also been reports that contribute to the base of knowledge in UKR fixation, with lessons being learned and improvements made. A report from Keblish and Briard in 2004 regarding the LCS mobile-bearing UKR highlights the reasonable clinical results obtainable, but again shows that there are concerns regarding cementless fixation as all the failures of fixation in the study were in the cementless group.21 The Porous Coated Anatomic UKR had initial success, using both cemented and cementless fixation methods. However, Bernasek et al. described an increased number of failures due to fixation in the early postoperative period, with fibrous tissue forming at the implant-bone interface22 in the cementless components. Lindstrand and Stenstrom reported good results initially with the same implant, but then showed a deterioration between 4 and 8 years postoperatively.23,24 Although the failures described in the midterm were mostly related to extreme polyethylene wear, this demonstrates the difficulty in obtaining long-term follow-up on UKR fixed without cement. Epinette and Manley have provided perhaps the best mid- to long-term follow-up of a cementless UKR.25 At a minimum follow-up of 5 years, with a maximum of 13 years, there were no failures of fixation from 125 hydroxyapatite-coated Unix knee replacements. Radiographs obtained 14 years after surgery show that excellent fixation without the development of radiolucencies can be achieved (Fig. 12–9). The results of the available published reports are summarized in Table 12–1. The data presented demonstrate the need for further studies with longer follow-up in addition to focus on particular patient groups, such as the young with high demand.
1 Bauer TW, Jiang M, Epinette JA. Hydroxyapatite-coated unicompartmental knee arthroplasty: histologic analysis of retrieved implants. In: Cartier P, Epinette JA, Deschamps G, Hernigou P, editors. Unicompartmental Knee Arthroplasty. Paris: Expansion Scientifique Francaise; 1996:43-50.
2 Kaiser AD, Whiteside LA. The effect of screws and pegs on the initial fixation stability of an uncemented unicondylar knee replacement. Clin Orthop Relat Res. 1990;259:169-178.
3 Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: Australian Orthopaedic Association; 2009.
4 New Zealand Orthopaedic Association. The New Zealand Joint Registry: Annual Report. Wellington: New Zealand Orthopaedic Association; 2009.
5 Swedish Knee Arthroplasty Register. Annual Report. Lund: Swedish Knee Arthroplasty Register; 2009.
6 Canadian Institute for Health Information. Hip and Knee Replacements in Canada—Canadian Joint Replacement Registry. 2008–2009 Annual Report. Ottawa, Ontario: Canadian Institute for Health Information; 2009.
7 National Joint Registry of England and Wales. 6th Annual Report. Hemel Hempstead, UK: National Joint Registry of England and Wales, 2009.
8 Forsythe ME, Englund RE, Leighton RK. Unicondylar knee arthroplasty: a cementless perspective. Can J Surg. 2000;43:417-424.
9 Pandit H, Jenkins C, Beard DJ, et al. Cementless Oxford unicompartmental knee replacement shows reduced radiolucency at one year. J Bone Joint Surg [Br]. 2009;91:185-189.
10 Carlsson A, Bjorkman A, Besjakov J, Onsten I. Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop. 2005;76:362-369.
11 Onsten I, Nordqvist A, Carlsson AS, et al. Hydroxyapatite augmentation of the porous coating improves fixation of tibial components: a randomised RSA study in 116 patients. J Bone Joint Surg [Br]. 1998;80:417-425.
12 Regner L, Carlsson L, Karrholm J, Herberts P. Tibial component fixation in porous- and hydroxyapatite-coated total knee arthroplasty: a radiostereometric evaluation of migration and inducible displacement after 5 years. J Arthroplasty. 2000;15:681-689.
13 Kendrick BJ, Rout R, Bottomley NJ, et al. The implications of damage to the lateral femoral condyle on medial unicompartmental knee replacement. J Bone Joint Surg [Br]. 2010;92:374-379.
14 Bontemps G, Brust K. Medial compartment knee replacement: cemented vs. uncemented. Combined Bristol and Oxford Unicompartmental Arthritis Symposium, Nuffield Orthopaedic Centre, November 18th 2009.
15 Price AJ, Webb J, Topf H, et al. Rapid recovery after Oxford unicompartmental arthroplasty through a short incision. J Arthroplasty. 2001;16:970-976.
16 Rees JL, Price AJ, Beard DJ, et al. Minimally invasive Oxford unicompartmental knee arthroplasty: functional results at 1 year and the effect of surgical inexperience. Knee. 2004;11:363-367.
17 Carlsson LV, Albrektsson BE, Regner LR. Minimally invasive surgery vs conventional exposure using the Miller-Galante unicompartmental knee arthroplasty: a randomized radiostereometric study. J Arthroplasty. 2006;21:151-156.
18 Romanowski MR, Repicci JA. Minimally invasive unicondylar arthroplasty: eight-year follow-up. J Knee Surg. 2002;15:17-22.
19 Gulati A, Chau R, Pandit HG, et al. The incidence of physiological radiolucency following Oxford unicompartmental knee replacement and its relationship to outcome. J Bone Joint Surg [Br]. 2009;91:896-902.
20 Kendrick BJL, Pandit H, Jenkins C, et al. Cementless fixation of unicompartmental knee replacement decreases radiolucency at two years. Paper presented at the Annual Meeting of the British Association for Surgery of the Knee, Oxford, 2010.
21 Keblish PA, Briard JL. Mobile-bearing unicompartmental knee arthroplasty: a 2-center study with an 11-year (mean) follow-up. J Arthroplasty. 2004;19(7 Suppl 2):87-94.
22 Bernasek TL, Rand JA, Bryan RS. Unicompartmental porous coated anatomic total knee arthroplasty. Clin Orthop Relat Res. 1988;236:52-59.
23 Lindstrand A, Stenstrom A. Polyethylene wear of the PCA unicompartmental knee: prospective 5 (4–8) year study of 120 arthrosis knees. Acta Orthop Scand. 1992;63:260-262.
24 Lindstrand A, Stenstrom A, Egund N. The PCA unicompartmental knee: a 1–4-year comparison of fixation with or without cement. Acta Orthop Scand. 1988;59:695-700.
25 Epinette JA, Manley MT. Is hydroxyapatite a reliable fixation option in unicompartmental knee arthroplasty? A 5- to 13-year experience with the hydroxyapatite-coated unix prosthesis. J Knee Surg. 2008;21:299-306.
26 Magnussen PA, Bartlett RJ. Cementless PCA unicompartmental joint arthroplasty for osteoarthritis of the knee: a prospective study of 51 cases. J Arthroplasty. 1990;5:151-158.
27 Lecuire F, Fayard JP, Simottel JC, et al. Mid-term results of a new cementless hydroxyapatite coated anatomic unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol. 2008;18:279-285.