Chapter 24 Medial and Posteromedial Ligament Injuries
Diagnosis, Operative Techniques, and Clinical Outcomes
INDICATIONS
Medial ligament injuries are among the most frequently treated problems of the knee joint, with the majority not requiring operative intervention. Whereas isolated superficial medial collateral ligament (SMCL) ruptures are common, concomitant damage to the anterior cruciate ligament (ACL) also occurs in many cases, especially in young and active patients.6,11,14,28,33
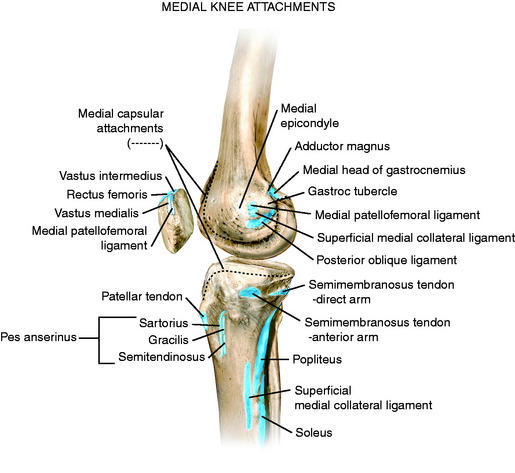
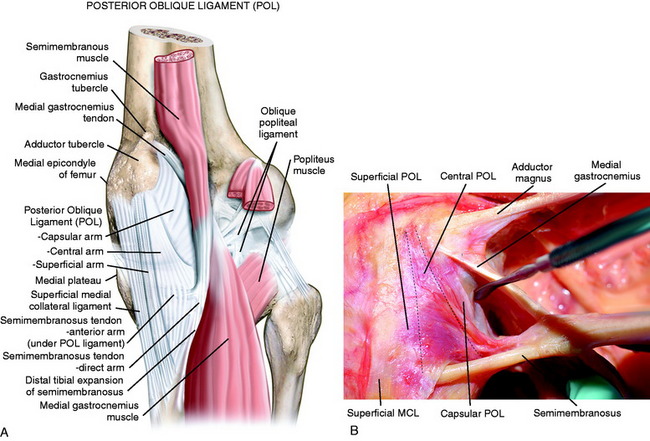
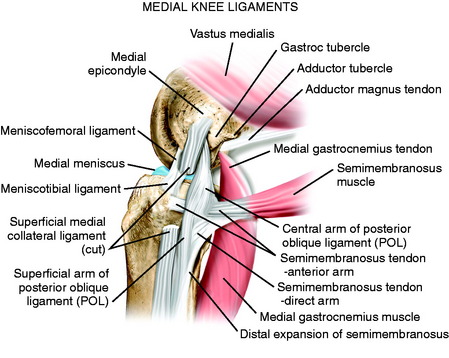
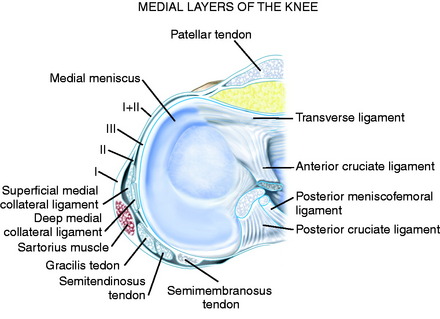
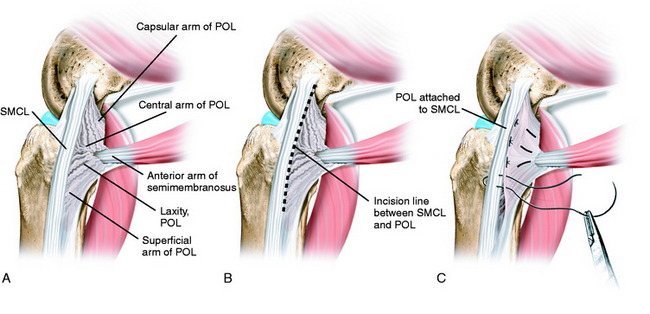
The medial structures identified for purposes of surgical treatment consist of the SMCL, deep medial collateral ligament (DMCL, including meniscus attachments), and the PMC, which includes the structures referred to as the POL and semimembranosus attachments.22,44 The key to the diagnosis and treatment of medial ligament injuries relies on a comprehensive understanding of the intricate anatomy on the medial side of the knee. This is presented in detail in Chapter 1, Medial and Anterior Knee Anatomy. In Figure 24-1, the osseous attachments of the medial structures are shown. Figure 24-2 shows the medial and posteromedial ligament structures, which are discussed in detail. Figure 24-3 shows the relationship of the semimembranosus muscle attachments to the posteromedial structures and POL. These include the bifurcation of the semimembranosus tendon into a direct and anterior area just distal to the joint line and a minor attachment of the direct arm to the medial coronary ligament along the posterior horn of the medial meniscus. The semimembranosus tendon sheath makes up a distal tibial expansion that includes a medial and lateral division. A major attachment of the semimembranosus forms the oblique popliteal ligament, which is a broad fascial band that courses laterally attaching to the fabella, posterolateral capsule, and plantaris (see Chapter 1, Medial and Anterior Knee Anatomy, Figs. 1–4 to 1–10).
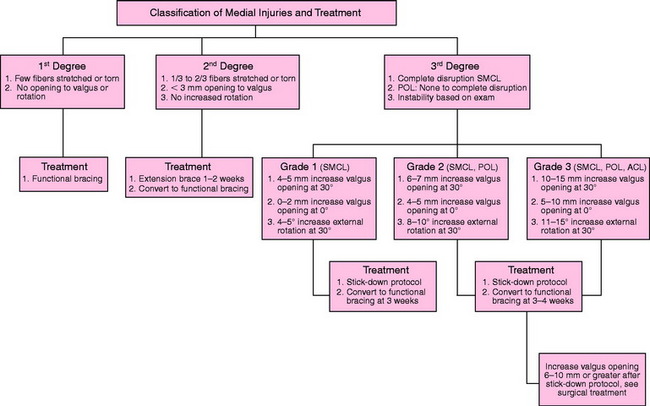
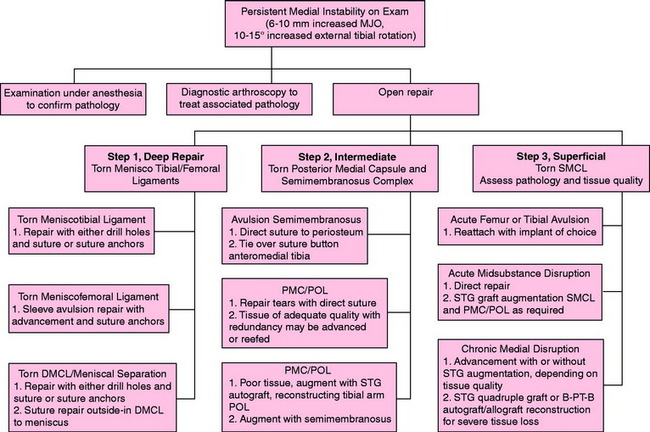
It is important to understand and classify the soft tissue injury of all the medial structures. The majority of acute medial ligament injuries that involve damage to the SMCL alone, or SMCL and PMC, are treated conservatively. The nonoperative treatment algorithm is shown in Figure 24-4 and discussed later in more detail. Gross major disruption of all of the medial structures alone or in addition to the ACL or PCL tears involve a group of select knees. The treatment of these gross ligament disruptions is discussed in a later section of this chapter.
In cases of chronic injury to the medial ligaments, it is important to obtain a complete history and objective and functional rating. The authors’ use the Cincinnati Knee Rating System (CKRS) for this analysis (see Chapter 44, The Cincinnati Knee Rating System) to determine patient complaints of giving-way and the levels of activity at which this symptom occurs as an indication for surgical stabilization procedures. In this chapter, instability refers to an increase in abnormal motion limits as detected on the physical examination, and is not used to indicate giving-way events.
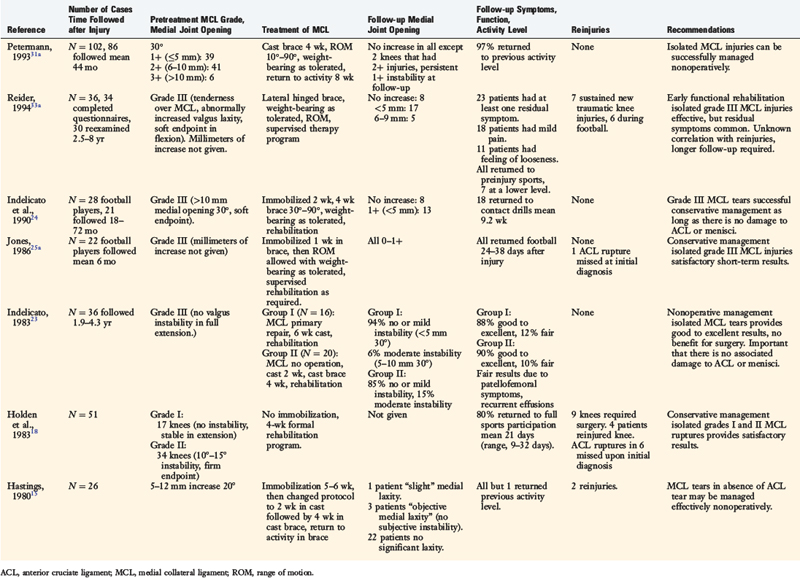
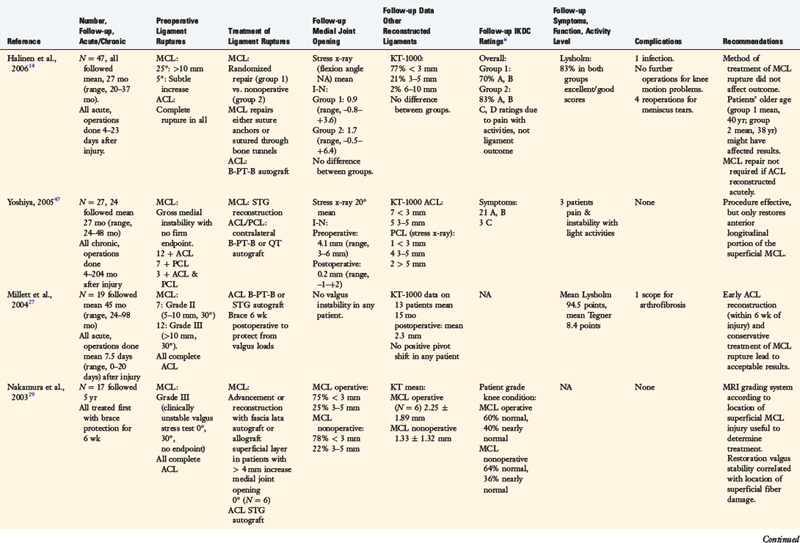
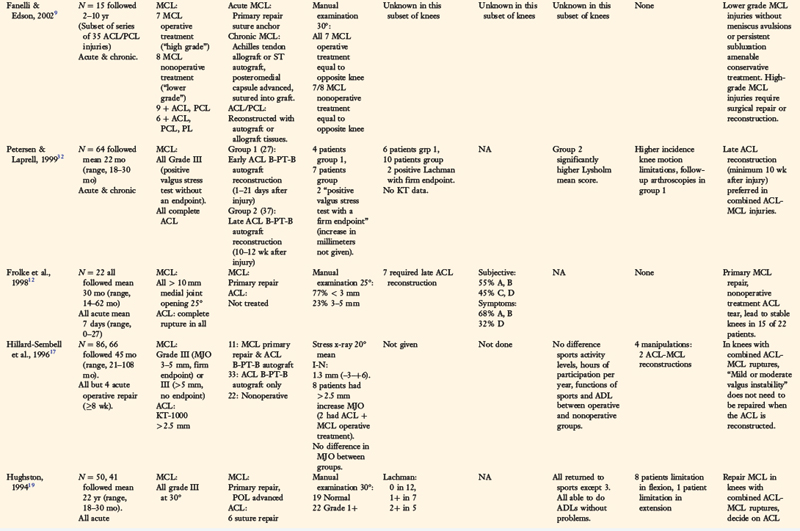
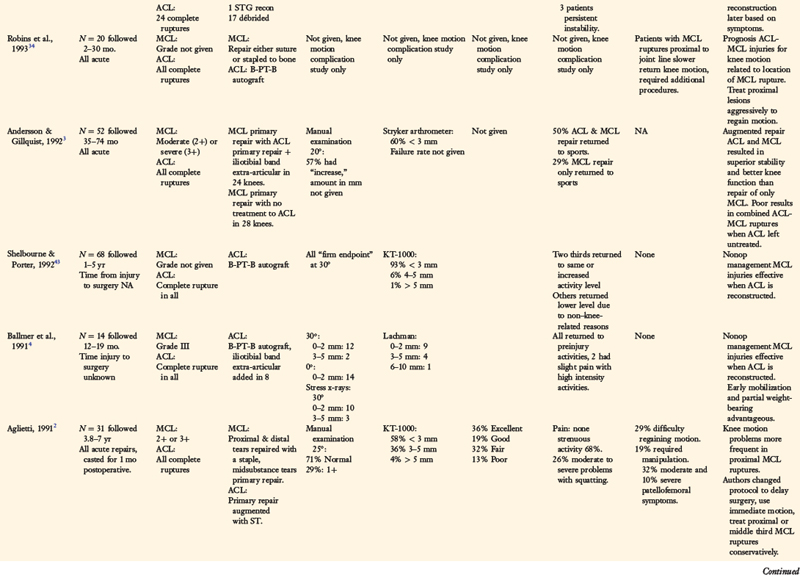
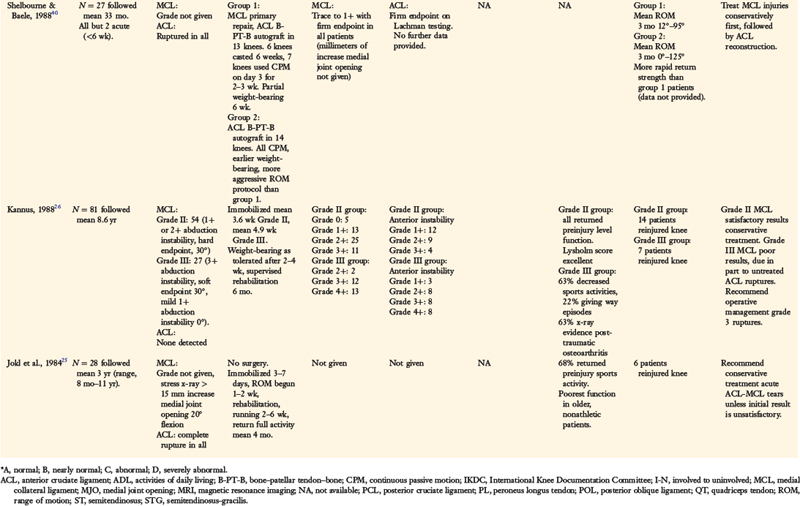
CONTRAINDICATIONS
CLINICAL BIOMECHANICS
A considerable amount of discrepancy exists in the literature regarding the use of terminology to describe and classify the medial ligament injuries from an anatomic standpoint and the abnormal motion limits that exist (see Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries). The authors agree with Hughston and coworkers19 that the clinician must clearly separate and classify medial ligament tears into first degree (tear involving a few fibers), second degree (partial tear, no instability, ≤3 mm of medial joint opening), and third degree (complete rupture) (TABLE 24-1; see also Fig. 24-4).5,10,11,13,20,21,32,42 This is one of the earliest systems devised and is based on a classification proposed by the American Medical Association.1 The problem has arisen, as amply demonstrated in TABLE 24-1, that this classification system has been modified extensively by different authors and it is often not possible to categorize the injury severity of the knees under treatment. For example, some authors in TABLE 24-1 refer to a second-degree or grade 2 instability as one that has a definite laxity or mild to moderate instability, even though the original definition of a second-degree or grade 2 injury represented only a partial ligament tear without any major increase in medial joint opening. Thus, it is necessary in the review of the literature to perform a subset analysis, which has been done in this chapter, to try to obtain the category or type of injury under treatment and the authors’ treatment recommendations.
TABLE 24-1 Published Classification Systems for Ruptures to the Medial Structures of the Knee
| Reference | System |
|---|---|
| Hughston et al., 1976,20 198321 |
MCL, medial collateral ligament.
Critical Points CLINICAL BIOMECHANICS
For purposes of this chapter, the injury classification based on the clinical examination is shown in Figure 24-4. Note that the medial ligament injuries are based on the first-, second-, and third-degree original classification system proposed; the increases in medial joint opening for the third-degree injury are based on the increase in medial joint opening and external tibial rotation. Some classification systems use a system in which each grade represents a further 5-mm increase in joint opening (grades 1, 2, and 3) over the contralateral normal knee, whereas other systems use the grade to represent the absolute amount of joint opening in the injured knee (grades 1+, 2+, and 3+). This chapter uses the increase in millimeters of medial joint opening between the injured and the contralateral normal knee to diagnose the medial ligament injury, because this is the system used in the published biomechanical and kinematic studies to be presented.
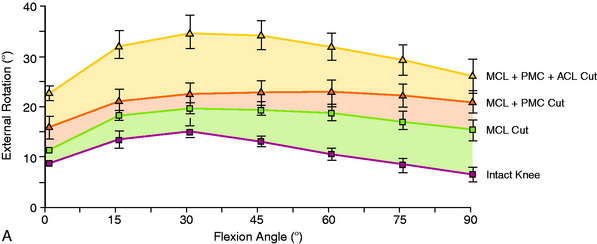
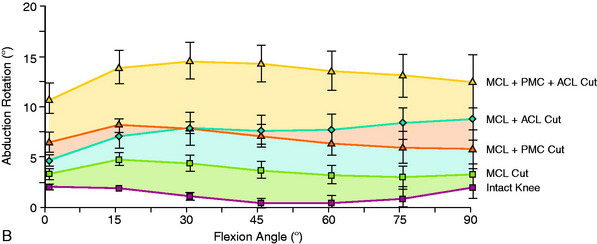
A review of the in vitro cadaveric biomechanical function of the medial ligaments and ACL in resisting medial joint opening, external tibial rotation, and internal tibial rotation is provided in Figure 24-5, summarized in TABLE 24-2, and discussed in more detail in Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries. A finding of increased medial joint space at 30° of flexion (third-degree sprain, parallel fibers of the SMCL), but not at 0° of flexion, indicates that the PMC (including the POL) is still functional. Any further increase in medial joint opening at 0° indicates concurrent damage to the PMC. With complete disruption of the SMCL and PMC, the ACL and PCL become a restraint to further medial joint opening. Knees with rupture to both the medial collateral ligament (MCL) and the POL will demonstrate increases in external tibial rotation (average of 9° at 30° of flexion), increases in internal tibial rotation (average of 12° at 30° of flexion), and increases in abduction testing at 0° and 30° of flexion (averages of 6° and 9°, respectively). The results show the importance of performing the dial tibial rotation test (see Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes) to determine the anterior subluxation of the medial tibial plateau with medial ligament injuries. With a combined MCL/POL injury, there will be a noticeable increase in internal and external tibial rotation. The PMC is an important structure for stabilizing the extended knee under valgus loading.35–37 With knee flexion, the PMC slackens and the MCL becomes the dominant restraint. In the extended knee, with posterior drawer and internal rotation, the PMC tightens based on its attachments at the femur (just posterior to the adductor tubercle) and the posteromedial aspect of the tibia. The increase in abduction for a combined MCL/POL injury and MCL/ACL injury at 15° to 45° of flexion is nearly the same (see Fig. 24-5B). The major difference between these injuries is in increased abduction at full extension in the MCL/POL ruptured knee.
TABLE 24-2 Increases in Motion Limits Relative to the Intact Knee That Occurred When the Indicated Structures Were Sectioned
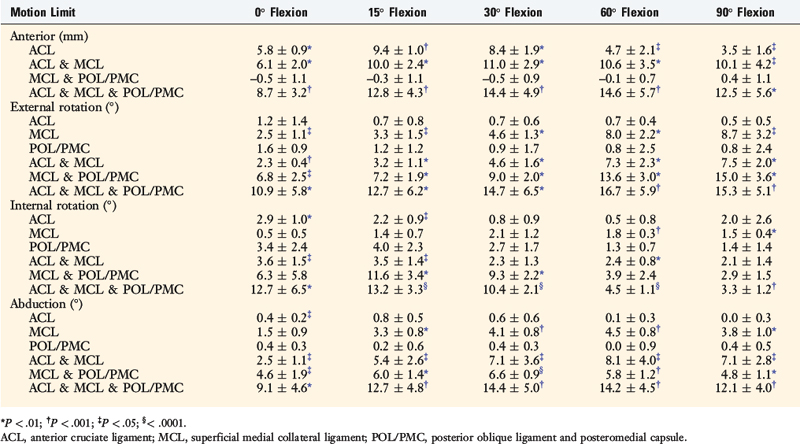
The increase in medial joint opening and external tibial rotation shown in Figure 24-5 provides an indication of an associated ACL tear when these motion limits are distinctly abnormal. In these knees, there is a large increase in anterior tibial translation and the pivot shift test is in the grade III category.
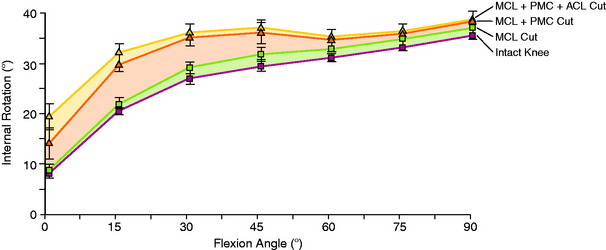
The function of the PMC/POL in resisting internal tibial rotation is shown in Figure 24-6. An increase in the internal rotation limit at low flexion angles is a further diagnostic test for PMC/POL rupture, detected by the dial test.
Sims and Jacobson44 reviewed 93 knees that underwent operative treatment for acute MCL injuries. These authors reported that 93% had associated injury to the POL following the description of Hughston and Eilers.22 The authors emphasized the importance of identification and repair of the POL and tears of the semimembranosus capsular attachment (present in 70% of knees) and associated peripheral detachment of the medial meniscus (present in 30% of knees; Fig. 24-7). The authors postulated that a dynamic function of the semimembranosus attachments exists for knee stability, but this is unproved experimentally. Although some authors describe rupture and surgical repair of the POL alone (anteromedial rotatory instability), the biomechanical data show that the POL is not a primary restraint for medial joint opening or external tibial rotation. Interestingly, an isolated POL injury does produce an increase in internal tibial rotation (see Fig. 24-6), although again, this injury pattern clinically involves a combined PCL/POL disruption.
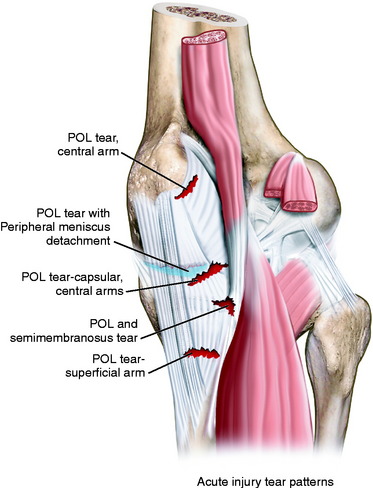
FIGURE 24-7 Three major injury patterns (injury to the POL is common to all): (1) injury to the POL with semimembranosus disruption, (2) injury to the POL with complete peripheral meniscocapsular detachment, and (3) POL injury with semimembranosus injury and peripheral meniscocapsular detachment. Disruption at any level is capable of disabling the dynamic function of the semimembranosus.44
CLINICAL EVALUATION
History and Physical Examination
The comprehensive examination of the knee joint required to detect all abnormalities includes assessment of (1) range of knee flexion and extension, (2) knee joint effusion and swelling, (3) the knee motion limits and subluxations compared with the contralateral knee,31 (4) alignment of the patellofemoral joint, (5) patellofemoral and tibiofemoral crepitus, (6) tenderness along the medial joint line and along the entire course of the SMCL from proximal to distal, (7) overall lower limb alignment, (8) neurovascular status, and (9) gait.
Diagnostic Clinical Tests
The clinical tests for the assessment of ligament injuries are shown in Figure 24-8. SMCL disruption is determined by manual valgus stress testing at 0° and 30° of knee flexion. The surgeon estimates the amount of joint opening (in millimeters) between the initial closed contact position and the open position of each tibiofemoral compartment (avoiding internal or external tibial rotation). The result is recorded according to the increase in the tibiofemoral compartment of the injured knee compared with that of the opposite normal knee.
The tibiofemoral rotation dial test at 30° and 90° with the patient in the supine position is done to determine whether increases in external tibial rotation occur with anterior subluxation of the medial tibial plateau (and not posterior subluxation of the lateral tibial plateau, indicating a posterolateral ligament injury).32 An increase in internal rotation may occur with MCL/POL disruptions (maximum 15°–45° flexion). Associated lateral and posterolateral disruptions are determined by varus stress testing at 0° and 30° of knee flexion.
Radiographs and Imaging Studies
Posterior stress radiographs are obtained in patients with PCL ruptures, especially those in whom the distinction of a partial versus complete PCL tear is difficult to determine on clinical examination (see Chapter 21, Posterior Cruciate Ligament: Diagnosis, Operative Techniques, and Clinical Outcomes).16 Lateral stress radiographs may be required in knees with lateral ligament injury (see Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes). Full standing radiographs of both lower extremities, from the femoral heads to the ankle joints, are done in knees with varus or valgus lower extremity malalignment (see Chapter 31, Primary, Double, and Triple Varus Knee Syndrome: Diagnosis, Operative Techniques, and Clinical Outcomes). The mechanical axis and weight-bearing line are measured.7 Of concern is to exclude a knee with lower extremity valgus alignment and increased medial soft tissue tensile forces with a valgus thrust, indicating the need for a corrective osteotomy in chronic medial injuries.
MRI is helpful to reveal the location of ligament anatomic disruptions, bone contusions, other ligament ruptures, and meniscus tears (Fig. 24-9). A high rate of concurrent lateral meniscus tears has been reported with MCL ruptures, making MRI an important adjunct for an accurate diagnosis.30,41 Ligament avulsion or osteochondral injuries requiring treatment within the initial 7- to 10-day period after injury may exist.
CONSERVATIVE VERSUS OPERATIVE TREATMENT RULES AND PLANNING
Acute Medial and Posteromedial Ligament Ruptures
The treatment rationale for patients with acute medial ligament ruptures is shown in Figure 24-4. The algorithm is divided into three major sections based on the extent of injury to the SMCL and PMC/POL. The first- and second-degree injuries are treated initially with a functional brace, weight-bearing as tolerated, and rehabilitation as detailed in Chapter 25, Rehabilitation of Medial Ligament Injuries. Some second-degree injuries may have considerable medial pain and swelling; in these cases, an extension brace is used for the initial 1 to 2 weeks after the injury.
Critical Points CONSERVATIVE VERSUS OPERATIVE TREATMENT RULES AND PLANNING
Acute Injuries
OPERATIVE TREATMENT
At 7 days, the cylinder cast is split into an anterior and a posterior shell (Fig. 24-10) and the therapist assists the patient with ROM from 0° to 90° in a figure-of-four position (Fig. 24-11) with the hip joint externally rotated to protect the healing medial tissues, described in detail in Chapter 41, Prevention and Treatment of Knee Arthrosis. This protected ROM program is taught to the patient and performed three to four times a day. The split-cylinder cast protection in extension is maintained for 3 weeks, followed by a soft hinged brace. The rehabilitation and crutch-weaning program is detailed in Chapter 25, Rehabilitation of Medial Ligament Injuries. It must be stressed that the senior author has commonly encountered knees referred for treatment in which a complete SMCL injury (and partial-to-complete POL injury) was treated with a soft functional brace in which the golden period of the first few weeks after the injury was lost. A residual symptomatic increased medial joint opening and external tibial rotation required a chronic medial and posteromedial reconstruction.
It is possible to treat almost all medial ligament injuries (with or without concomitant ACL ruptures) using this conservative stick-down program. Operative treatment is recommended for select cases, as discussed next. A displaced meniscus tear on MRI would indicate the necessity to perform a meniscus repair. When there is an associated ACL tear, an ACL reconstruction is performed at an elective time, or under ideal conditions (minimal swelling, early motion), an ACL procedure is performed along with the meniscus repair. In high-performance athletes with gross disruption of the SMCL and POL (with or without ACL tear), the senior author prefers to perform an anatomic repair to restore anatomic continuity and function. In addition, in these gross medial disruptions, the repair of the medial meniscus attachments is always required. In select knees with acute SMCL, POL, and ACL injuries, the medial meniscus may be partially dislodged from the joint, and the distal SMCL so extensively displaced or coiled, that there is a reduced chance that protected immobilization would result in functional medial ligament structures (see Fig. 24-9). An example is the illustrative case described later in this chapter. In the authors’ experience, these knees do better with operative repair. A four-strand semitendinosus-gracilis (STG) autograft may be selected if there is an indication to decrease the morbidity of a bone-patellar tendon-bone (B-PT-B) autograft. The authors prefer an autograft over allografts for reasons discussed in detail in Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes.
In knees considered for operative intervention, the knee is rehabilitated for 7 days, motion to 90° is obtained, and early quadriceps muscle function is restored. The joint and extremity soft tissue swelling must not be excessive. A routine venous ultrasound is conducted before surgery. In acute medial injuries, it is usually not necessary to perform an augmentation of the repair (described later for chronic reconstructions), because the suture fixation methods restore ligament continuity and healing after surgery is prompt. These knees are treated with an immediate ROM program as detailed in Chapter 25, Rehabilitation of Medial Ligament Injuries. Proximal medial ligament disruptions with extensive edema and soft tissue swelling are at risk for ectopic calcification and limitation of joint motion in the first 2 to 3 weeks after surgery. Indomethacin (Indocin) treatment is not routinely administered; however, observation is warranted because indomethacin is only effective if given within the early postoperative course.
Acute Medial Ligament Ruptures with Knee Dislocation
A traumatic knee dislocation with involvement of the medial ligament structures along with the ACL and PCL represents a difficult treatment entity. Too often, these knees have a high incidence of arthrofibrosis after surgery. In the authors’ opinion, it is prudent to treat these knees with the stick-down conservative program and manage the associated injuries at a later time. A posterior calf pad is added to the cylinder cast to maintain a gentle posterior loading and prevent posterior tibial subluxation. Again, a lateral radiograph is obtained to verify tibiofemoral reduction. It is possible for the physical therapist to begin a careful ROM program with the bivalved cylinder cast at the 2nd week as detailed in Chapter 41, Prevention and Treatment of Knee Arthrofibrosis. In select athletes, under ideal circumstances, operative intervention may be considered; these knee injuries are evaluated and treated on a case-by-case basis. Issues related to evaluation of the vascular system are discussed in Chapter 27, Management of Acute Knee Dislocations before Surgical Intervention. The surgery is delayed for 7 days and the initial rehabilitation program begun, as previously discussed. Consultation is always obtained with exclusion of a vascular injury by repeated evaluation and appropriate diagnostic tests including ankle-brachial indices, MRI, and arteriography as indicated. A venous ultrasound is obtained. At surgery, the foot and ankle are positioned to allow vascular checks including Doppler, and tourniquet use is limited to only the initial open exploration to define the injury pattern, then deflated for the repair procedure.
Chronic Medial and Posteromedial Ruptures
Patients with chronic knee injuries that present with severe muscle atrophy require preoperative rehabilitation and patient education before consideration of surgical reconstruction. Frequently, patients who undergo MCL reconstruction (Fig. 24-12) require a concomitant ACL or PCL reconstruction. The appropriate grafts for the cruciate procedures should be determined, as detailed in separate chapters, and autogenous tissues are preferred. However, the surgeon should ensure that B-PT-B and Achilles tendon–bone allografts are available in multiligament reconstructions if needed and advise the patient of this possible choice.
INTRAOPERATIVE EVALUATION
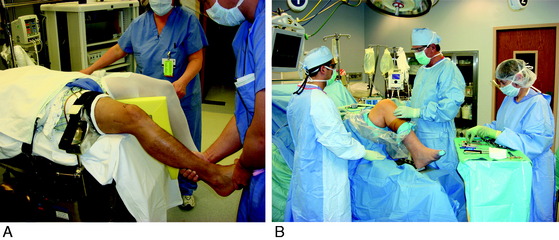
All knee ligament subluxation tests are performed after the induction of anesthesia in both the injured and the contralateral limbs. The amount of increased anterior tibial translation, posterior tibial translation, lateral joint opening, medial joint opening, and external-internal tibial rotation is documented. With ACL and/or SMCL/POL disruptions, the lower portion of the bed is flexed and flexion of the knee is performed as required for the arthroscopic and open approaches (Fig. 24-13A). A leg holder is used for the initial arthroscopic and meniscus procedures and then removed. An alternative approach used in multiligament and PCL disruptions is to position the lower extremity with the foot in an Alvardo holder or thigh post and foot rest to allow the desired amount of knee flexion during surgery (see Fig. 24-13B). The arthroscopic pressure is maintained at a low setting with adequate outflow at all times to prevent fluid extravasation and popliteal and calf swelling, which is documented throughout the case. A thorough arthroscopic examination is conducted, documenting articular cartilage surface abnormalities and the condition of the menisci. It is rare to have the complication of fluid extravascation if these precautions are taken; however, if extravascation occurs, an open approach is used throughout the remainder of the procedure.
Operative Treatment
Acute Medial and Posteromedial Ligament Repairs
The key to the operative procedure is a thorough understanding of the medial anatomy (see Figs. 24-1 to 24-224-3), because the integrity and injury to the SMCL, POL, semimembranosus attachments, and meniscus attachments (DMCL) need to be identified. The goal is to restore normal anatomy and function of all of these structures. The surgical dissection uses a layered approach45 following the description provided in Chapter 1, Medial and Anterior Knee Anatomy (Fig. 24-14).
Critical Points OPERATIVE TREATMENT
Acute Medial and Posteromedial Ligament Repairs
TABLE 24-3 Operative Steps for Acute Medial Ligamentous Ruptures
MCL, medial collateral ligament; MRI, magnetic resonance imaging; PMC, posteromedial capsule; POL, posterior oblique ligament; SMCL, superficial medial collateral ligament.
Chronic Medial and Posteromedial Ligament Repairs
TABLE 24-4 Operative Steps for Chronic Medial Ligamentous Ruptures
B-PT-B, bone–patellar tendon–bone; MCL, medial collateral ligament; PMC, posteromedial capsule; POL, posterior oblique ligament; SMCL, superficial medial collateral ligament; STG, semitendinosus-gracilis; VMO, vastus medialis obliquus.
The operative steps are outlined in TABLE 24-3. It is important to perform a careful limited dissection to avoid further disruption of the neurovascular supply of tissues (Fig. 24-15). Based on preoperative MRI and limited medial dissection, it is possible to identify the tear site of most of the soft tissue structures for the operative repair. A tourniquet is used for the initial exploration and then deflated during the repair portion of the procedure. A limited cosmetic incision along the anteromedial aspect of the tibia provides good exposure for both ACL and medial repairs and is favored over a two-incision approach (Fig. 24-16).
During the initial dissection, an incision is made into the sartorius fascia just anterior to the SMCL and the fascia and pes tendons are reflected posteriorly to allow identification of the medial structures. The tear site of the SMCL is usually easily identified. However, it may be more difficult to recognize the tear site for the PMC capsular arms referred to as the POL divisions (see Fig. 24-2). There may be interstitial tearing of capsular tissues without a definite tear, or the POL may be torn off its femoral or tibial attachment, requiring reattachment. The first goal is to restore normal anatomy. The SMCL, POL, and meniscus sutures are placed to restore anatomic attachment sites. The POL is closed at 10° to 15° of flexion, and the knee is taken to full extension to ensure the sutures are not overtensioned to constrain knee extension and produce a flexion contracture.
The second goal is to perform a meticulous anatomic repair of sufficient strength to allow immediate knee motion following the protocol provided in Chapter 25, Rehabilitation of Medial Ligament Injuries. Numerous ligament fixation devices are available, and a low-profile screw and soft tissue washer or four-prong staple and screw are favored, along with suture anchors. Standard baseball locking sutures of two to three throws are sufficient to tension soft tissues using a combination of nonabsorbable and absorbable sutures. On occasion, the medial ligament disruption is so extensive that it is necessary to perform an augmentation graft for the SMCL and PMC (POL division B; see Fig. 24-2) following the techniques outlined in a chronic medial reconstruction with either an STG autograft or allograft approach, as discussed next.
Chronic Medial and Posteromedial Ligament Repairs
The operative steps are the same as outlined for acute medial repairs in terms of the initial surgical approach and dissection. The specific additional steps are provided in Table 24-4.
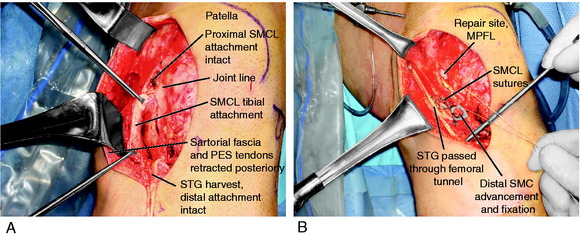
In Figure 24-16, the cosmetic medial skin incision is shown for a patient who had a combined ACL and MCL reconstruction. The standard ACL skin incision is extended proximally to provide adequate exposure for the medial ligament procedure. One of the principles followed is to use the remaining SMCL as a part of the reconstruction by femoral or tibial advancement based on the site of the prior tears. The meniscus attachments medially may require appropriate suture fixation to restore the meniscotibial attachment, with distal SMCL advancement. The second principle is to augment the SMCL reconstruction with STG tendons, which is usually required. The STG tendons are tensioned based on isometric length-tension behavior with knee flexion-extension at surgery.
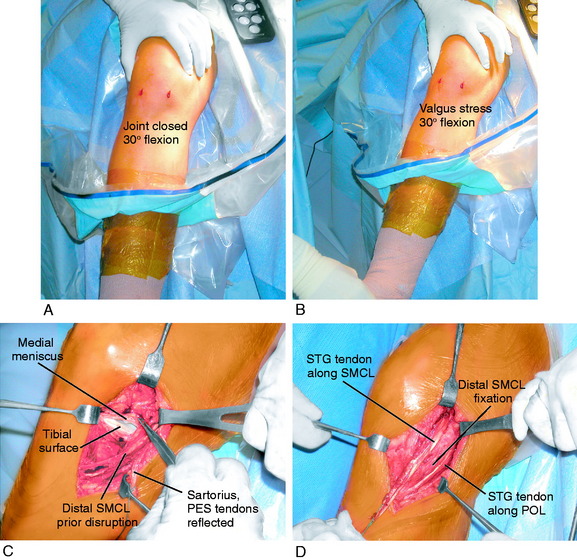
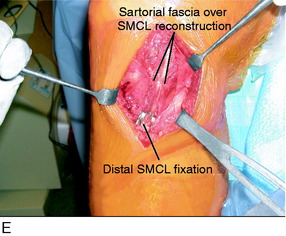
Following the operative principles outlined in Table 24-4, an example of a distal SMCL advancement supplemented with an STG reconstruction for chronic MCL deficiency is shown in Figure 24-17. In Figure 24-18, a more complex medial reconstructive procedure is shown that involved extensive repair of the meniscus attachments and STG tendon reconstruction of both the SMCL and the PMC (POL). The operative procedure provides sufficient strength to allow immediate knee motion postoperatively to lessen the risk of a joint contracture. These procedures involve extensive postoperative rehabilitation, which is described in Chapter 25, Rehabilitation of Medial Ligament Injuries. In Figure 24-19, a proximal advancement of the SMCL and PMC capsular plication are shown; this knee did not require augmentation with an STG graft. In Figure 24-20, the use of a B-PT-B allograft is shown for severe cases of chronic medial ligament disruption. This operative technique is reserved for cases in which no remaining medial ligamentous tissues are present. In most chronic medial ligament injuries, it is possible to use the remaining SMCL and PMC in the reconstructive procedure, and this graft is not required. The Achilles tendon is an alternative allograft, with the bone portion placed at the native SMCL femoral attachment and the full-thickness tendon fixed by a screw and soft tissue washer with additional baseball sutures at the native tibial attachment. The correct attachment points for the SMCL graft are at the native femoral and tibial attachments. If there is any question, the graft attachment is verified by placing a K-wire at the femoral site, attaching suture to the tibial site, and taking the knee through a full ROM. The POL is reattached to its native femoral or tibial site when disruption has occurred. For capsular redundancy, a plication procedure is performed to the posterior edge of the SMCL graft, which provides the stable medial column for the capsular reconstruction.
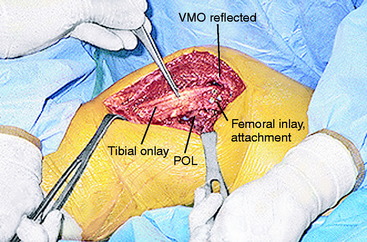
FIGURE 24-20 Demonstration of the use of a long B-PT-B allograft for a severe medial ligament disruption in which no remaining SMCL was present. The bone portions of the graft are placed as an inlay on the femur and as an onlay on the tibia and fixated with cancellous and small fragment screws, respectively. A POL plication was performed (see Table 24-4 for operative steps).
COMPLICATIONS
The most frequent complication of medial and posteromedial ligament surgery relates to the approximately 25% of operated knees that will have initial limitations in regaining normal flexion and extension. It is necessary at surgery not to overtighten the POL plication or repair. The repair is performed at 10° to 15° of flexion, and the knee is taken to full extension at the end of the procedure. The SMCL augmentation or replacement is fixated at native femoral and tibial attachments and not overtensioned in order not to constrain the knee joint. The treatment of knee motion limitations, principles of patellofemoral mobilization, and muscle rehabilitation exercises are covered in detail in Chapter 25, Rehabilitation of Medial Ligament Injuries.
The complication of infection is rare with the use of preoperative intravenous antibiotics at appropriate doses, careful handling of tissues, and other precautions as detailed in Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes.
AUTHORS’ CLINICAL STUDY
A prospective study was conducted to determine the outcome of 46 knees with acute ACL-MCL ruptures in which all patients received an ACL reconstruction and either conservative or operative management of the medial ligament injury, based on the extent of the injury.30 The inclusionary criteria were a complete rupture of the ACL, rupture to a portion or all of the medial ligamentous structures, no rupture to the other knee ligaments, and reconstruction performed within 10 weeks of the original knee injury.
Critical Points AUTHORS’ CLINICAL STUDY
46 knees with acute ACL-MCL ruptures:
Meniscus repairs done in 23 (68%) of group I and in 11 (92%) of group II.
Treatment program of knee motion limitations required in 26% of group I, 17% of group II.
Meniscus tears were common in both groups of patients, occurring in 23 patients (68%) in group I and in 11 patients (92%) in group II. The lateral meniscus was torn in 61% of the knees and the medial meniscus was torn in 33%. In group I, the medial meniscus was repaired in 12 knees and the lateral meniscus was repaired in 7 knees using techniques described in Chapter 28, Meniscus Tears, Diagnosis, Operative Techniques, and Clinical Outcomes.38,39 Thirteen other lateral meniscus tears required partial resection. In group II, the medial meniscus was repaired in 3 knees and the lateral meniscus was repaired in 6 knees. Four other lateral meniscus tears required partial resection.
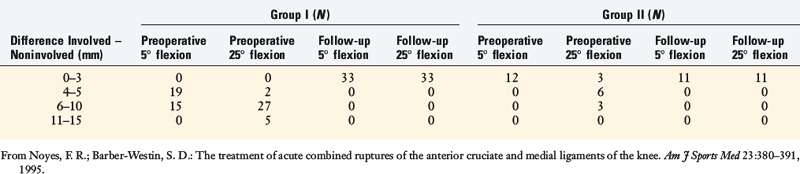
At follow-up, no patient in either group had more than 2 to 3 mm of increase in medial joint space opening (TABLE 24-5). Moderate patellofemoral crepitus was detected in 7 patients in group I and severe crepitus was found in 1 patient. One patient in group II had moderate patellofemoral crepitus. The crepitus was symptomatic with sports activities in 2 of these 9 patients. The ACL reconstructions were rated (based on knee arthrometer and pivot shift testing) as normal in 61% in group I and in 82% in group II; nearly normal in 21% in group I and in 18% in group II; and failed in 18% of group I.
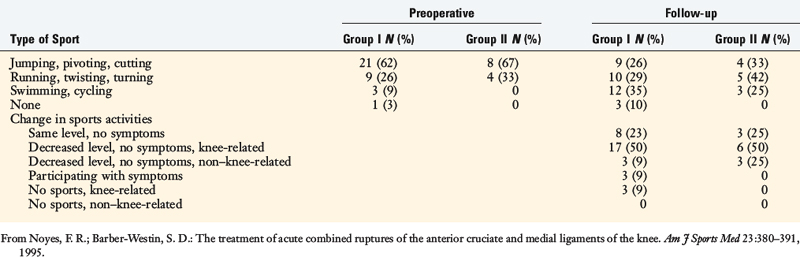
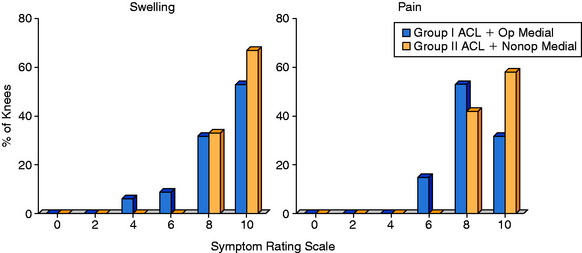
Before the injury, all patients except 1 were participating in sports activities (TABLE 24-6). At follow-up, all except 3 patients in group I had returned to athletics, although over half had returned to a lower level of participation. No patient in either group had problems with walking or stair climbing. However, 7 patients in group I had significant difficulty squatting or kneeling. More patients in group I had swelling and pain with sports activities than those in group II (Fig. 24-21).
The rehabilitation program and early treatment of knee motion limitations successfully restored at least 0° to 135° of knee motion in 96% of the patients. The treatment program of knee motion limitations, described in Chapter 41, Prevention and Treatment of Knee Arthrofibrosis, was instituted in 24% of the knees (26% of group I and 17% of group II). This program is most successful if begun early postoperatively, as early as 3 to 4 weeks if the initial motion goals have not been obtained. Patients with ruptures at or proximal to the medial joint line had a higher incidence of motion complications (7 of 15 patients, 47%) than those with ruptures located distal to the joint line (2 of 18 patients, 11%). Similar findings were reported by Robins and associates.34
The strict overall rating system used in this investigation resulted in 14 patients receiving a fair or poor score. Seven of these 14 patients received this rating, in part, owing to failure of the ACL allograft and the authors advocate autogenous B-PT-B grafts for ACL reconstruction. At the time of the study, the authors used irradiated allografts, and as discussed in Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes, the irradiation process appeared to increase the rate of failure compared with other studies in which fresh-frozen allografts were selected. Patellofemoral joint symptoms accounted for the low ratings in 4 knees, and postoperative motion complications accounted for the ratings in 3 knees. This study was also conducted at a time in which complete disruptions of ACL and medial ligaments were more often treated by operative intervention.
The results of this study, along with other investigations,4,27,29,32,43 promoted a worthwhile reevaluation of the operative recommendation for combined ACL and medial ligament injuries, resulting in the conservative recommendations in this chapter, which have now been used for many years.
RESULTS FROM OTHER CLINICAL STUDIES
Since the early 1990s, several studies have been published that presented various treatment options and outcomes for isolated MCL injuries and combined ACL-MCL ruptures. As shown in Tables 24-7 and 24-8, the severity of the medial ligamentous injuries varies and, in many instances, is difficult to interpret owing to both the ambiguous terminology used to describe the degree or grade of the injury and the lack of data on the estimated (or measured) millimeters of medial joint opening at both 30° and 0° of knee flexion before and after treatment. Even fewer investigators use stress radiography to objectively measure medial joint opening before and after treatment. Therefore, the exact structures that are ruptured (and those that remain intact) in most studies are unknown. Future investigations should provide these data to enable clinicians to understand the exact anatomic structures involved and form rationale treatment decisions regarding which structures require operative restoration and the appropriate timing of those procedures.
TABLE 24-8 Results of Treatment of Combined Medial Collateral Ligament–Anterior Collateral Ligament Injuries
Critical Points RESULTS FROM OTHER CLINICAL STUDIES
The majority of clinical studies that have described the outcome of operative management of SMCL ruptures used primary suture repair procedures, some of which were combined with advancement of the PMC, for acute knee injuries.2,3,12,14,17,19,34,40 Only two series to date described the use of a graft to reconstruct chronic SMCL ruptures; both involved knees with multiligament injuries. Yoshiya and colleagues46 followed 24 patients who underwent an STG SMCL reconstruction. The SMCL ruptures were classified as having gross medial instability with no firm endpoint. It is noted in this study that preoperative valgus stress radiographs measured only a mean of 4.1 mm (range, 3–6 mm) of increased medial joint opening and, therefore, it would appear that these knees would be in the category in which conservative treatment is usually recommended. Twelve patients had a concomitant ACL reconstruction, 7 had a concomitant PCL reconstruction, and 3 had a concomitant bicruciate reconstruction. At an average of 27 months postoperatively, stress radiographs revealed a mean of 0.2 mm (range, –1–+2 mm) increase in medial joint opening. The authors cautioned that, although the procedure was effective, it restored only the anterior longitudinal portion of the SMCL.
Fanelli and Edson9 described a procedure to reconstruct the SMCL in patients with “high-grade” SMCL ruptures using either an Achilles tendon allograft or a semitendinosus tendon autograft. The millimeters of increased medial joint opening at 0° and 30° of flexion that were present before surgery were not provided. The PMC was advanced and sutured into the graft. In a small series of 7 patients followed 2 to 10 years postoperatively, no increase was noted on manual valgus testing at 30° of knee flexion.
Halinen and coworkers14 published to date the only study of acute grade III medial ruptures (defined by the authors as > 10 mm increase in medial joint opening at 25° of flexion and a “subtle” increase at 5° of flexion) that were randomized to either a primary repair or a conservative management group. All 47 patients in the study also had complete ACL ruptures, which were reconstructed with a B-PT-B autograft. The reconstructions were performed between 4 and 23 days after the injury. At follow-up, a mean of 27 months postoperatively, stress radiographs (25° flexion) revealed a mean increase in medial joint opening of 0.9 mm (range, –0.8–+3.6 mm) in the SMCL operatively treated group, and 1.7 mm (range, –0.5–+6.4 mm) in the SMCL conservatively treated group. The authors concluded the SMCL ruptures do not require operative treatment when a concomitant ACL rupture is reconstructed early after injury.
Conservative management of SMCL ruptures has been recommended by many authors following the early investigations of Ellsasser and associates8 and Fetto and Marshall.11 Ellsasser and associates8 reported successful management of isolated MCL injuries in athletes with nonoperative treatment as long as there were no other ligament or meniscus injuries and the knees were stable to valgus stress testing in full extension after the injury. Fetto and Marshall’s series11 included patients with medial joint opening in full extension (termed grade III), and the authors noted that 80% of grade III medial ruptures had concomitant cruciate ligament damage. An excellent or good result in these knees was related to the recovery of ACL stability and not to residual medial joint opening. Many subsequently published studies verified the importance of an intact or reconstructed ACL in the successful nonoperative management of SMCL ruptures.4,15,18,23,24,26,27,32,43
The question of the appropriate timing of ACL reconstruction in knees with concomitant SMCL tears has been addressed by a few investigations. Millett and colleagues27 followed 18 patients who had an ACL reconstruction (B-PT-B or STG autograft) performed a mean of 7.5 days (range, 0–20 days) after an acute ACL-MCL injury. Seven patients had a grade II SMCL injury (5–10 mm medial joint opening at 30° flexion) and 12 had a grade III injury (>10 mm at 30° flexion). Postoperatively, the patients were kept in a brace to protect from excessive valgus loads. At follow-up, a mean of 45 months postoperatively, no valgus instability (at 30° flexion) or positive pivot shift test was detected in any patient. One patient required an arthroscopic procedure for arthrofibrosis. The authors did not provide data regarding the number of patients who returned to preinjury levels of activity or symptoms and functional limitations. They concluded that early ACL reconstruction did not increase the risk of complications, but acknowledged that it is unknown whether this treatment strategy provides superior results over those from a delayed ACL reconstruction approach.
Peterson and Laprell32 found a higher incidence of knee motion complications and poorer subjective scores in knees that underwent early ACL reconstruction (1–21 days after injury) compared with those in whom the ACL reconstruction was delayed (10–12 wk after injury). All patients in their series received a B-PT-B autograft and all had a grade III medial ligament rupture (defined as a positive valgus stress test without an endpoint). Postoperative rehabilitation included no brace in the ACL delayed group, a brace in the early ACL group with limits set from 0° to 100°, full weight-bearing within 1 week for all patients, and intensive therapy training for 2 to 3 months. The authors did not provide preoperative data on muscle strength or range of knee motion for either group. Speculation was made that the motion limitations were due to the postoperative brace worn in the early ACL group, although the amount of time the brace was worn was not provided.
Shelbourne and Patel42 reported that patients with acute combined ACL-SMCL ruptures treated with only ACL reconstruction had more rapid return of knee motion and muscle strength than those treated with ACL reconstruction and SMCL repair. However, 6 of the 13 knees in the combined ACL-SMCL repair group underwent 6 weeks of casting postoperatively whereas the remainder of the knees in the series initiated continuous passive motion on the 3rd postoperative day. The authors did not assess the effect of casting on the study’s outcome. In addition, the severity of the SMCL ruptures was unknown, as no data were provided on the millimeters of medial joint opening at either 30° or 0° of knee flexion before or after surgery. The authors later recommended that all MCL injuries be treated conservatively, regardless of the severity of the injury.42
ILLUSTRATIVE CASE
Case 1
Acute Combined ACL, SMCL, POL Ligament Disruption with Dislodged Bucket-Handle Lateral Meniscus Tear in the Femoral Notch
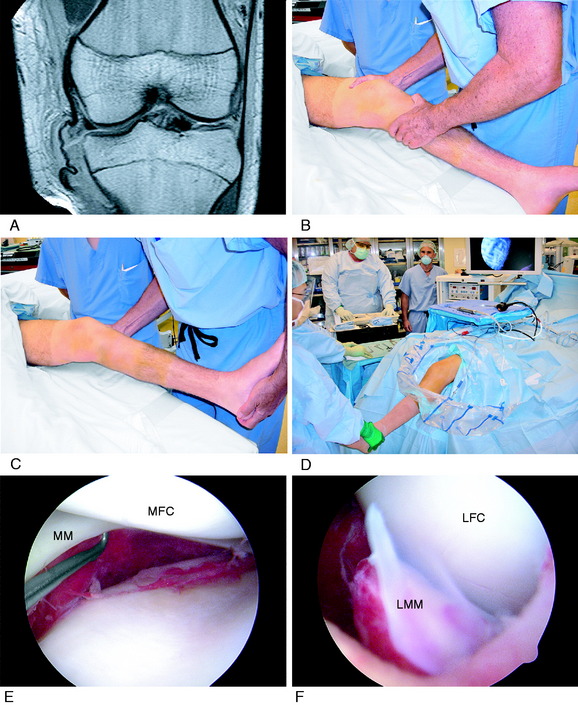
A 16-year-old male sustained a twisting injury to his left knee while water skiing. He was evaluated 5 days after the injury. MRI showed a coiled, disrupted distal MCL rupture, meniscotibial attachment tears, a displaced lateral meniscus within the femoral notch, and an ACL midsubstance rupture (Fig. 24-22A). The physical examination showed 10 mm of increased medial joint opening at 30° of flexion and 5 mm increase at 0°, a positive Lachman test, and a grade III pivot shift test. Surgery was indicated to reduce and repair the lateral meniscus bucket-handle tear. Because the patient had minimal swelling, restoration of motion, and early return of quadriceps function, the decision was made to proceed with a combined ACL-MCL reconstruction.
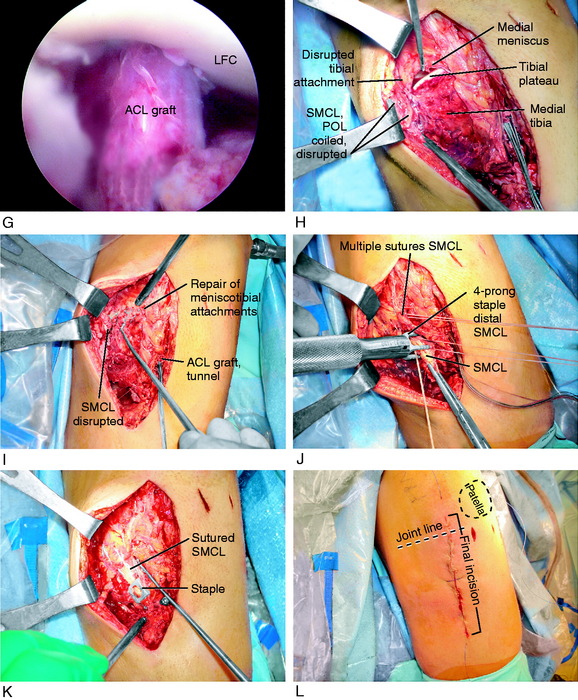
Under anesthesia, the increases in medial joint opening and external tibial rotation were noted (see Fig. 24-22B), along with a positive Lachman test (see Fig. 24-22C). The operative setup allowed for full flexion and extension, with a leg holder used initially for the lateral meniscus repair (see Fig. 24-22D). At arthroscopy, the tearing of the meniscotibial attachments and a 12-mm increase in the medial gap test were noted. The meniscus had a normal relationship with the femoral condyle, indicating a distal attachment tear (see Fig. 24-22E). The lateral meniscus was displaced into the notch, which was reduced and repaired with multiple vertical divergent sutures placed with an inside-out technique through an accessory posterolateral incision (see Fig. 24-22F). An ACL four-strand STG reconstruction was performed using a two-incision technique to achieve anatomic central tibial and femoral attachment locations (see Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes). The distal ACL attachment was fixed after the MCL repair (see Fig. 24-22G).
The medial exploration through the medial incision showed a meniscotibial attachment tear, increased medial joint opening, and disrupted distal SMCL and POL at the tibial attachment (see Fig. 24-22H). The procedure was begun deep with the medial meniscotibial attachment repair using multiple sutures (see Fig. 24-22I). In this case, suture anchors were not required. The entire SMCL and POL tibial attachment sleeve was reattached with three No. 2 baseball sutures placed in the posterior, middle, and anterior portions. A four-prong low-profile staple was used for distal SMCL fixation and as a suture post (see Fig. 24-22J). The combined suture and staple fixation provided secure fixation to allow immediate knee motion (see Fig. 24-22K). The final appearance of the incision is shown in Figure 24-22L, which extended from the midpoint of the patella 10 cm to the point adjacent to the tibial tubercle.
1 Standard Nomenclature of Athletic Injuries. Chicago: American Medical Association:1966.
2 Aglietti P., Buzzi R., Zaccherotti G., D’Andria S. Operative treatment of acute complete lesions of the anterior cruciate and medial collateral ligaments. A 4- to 7-year follow-up study. Am J Knee Surg. 1991;4:186-194.
3 Andersson C., Gillquist J. Treatment of acute isolated and combined ruptures of the anterior cruciate ligament. A long-term follow-up study. Am J Sports Med. 1992;20:7-12.
4 Ballmer P.M., Ballmer F.T., Jakob R.P. Reconstruction of the anterior cruciate ligament alone in the treatment of a combined instability with complete rupture of the medial collateral ligament. A prospective study. Arch Orthop Trauma Surg. 1991;110:139-141.
5 Bergfeld J. First-, second-, and third-degree sprains. Am Sports Med. 1979;7:207-209.
6 Deibert M.C., Aronsson D.D., Johnson R.J., et al. Skiing injuries in children, adolescents, and adults. J Bone Joint Surg Am. 1998;80:25-32.
7 Dugdale T.W., Noyes F.R., Styer D. Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;274:248-264.
8 Ellsasser J.C., Reynolds F.C., Omohundro J.R. The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am. 1974;56:1185-1190.
9 Fanelli G.C., Edson C.J. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703-714.
10 Fanelli G.C., Harris J.D. Late medial collateral ligament reconstruction. Tech Knee Surg. 2007;6:99-105.
11 Fetto J.F., Marshall J.L. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;132:206-218.
12 Frolke J.P., Oskam J., Vierhout P.A. Primary reconstruction of the medial collateral ligament in combined injury of the medial collateral and anterior cruciate ligaments. Short-term results. Knee Surg Sports Traumatol Arthrosc. 1998;6:103-106.
13 Garrick J.G., editor. Orthopaedic Knowledge Update: Sports Medicine 3. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2004:466.
14 Halinen J., Lindahl J., Hirvensalo E., Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34:1134-1140.
15 Hastings D.E. The non-operative management of collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1980;147:22-28.
16 Hewett T.E., Noyes F.R., Lee M.D. Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med. 1997;25:648-655.
17 Hillard-Sembell D., Daniel D.M., Stone M.L., et al. Combined injuries of the anterior cruciate and medial collateral ligaments of the knee. Effect of treatment on stability and function of the joint. J Bone Joint Surg Am. 1996;78:169-176.
18 Holden D.L., Eggert A.W., Butler J.E. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11:340-344.
19 Hughston J.C. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am. 1994;76:1328-1344.
20 Hughston J.C., Andrews J.R., Cross M.J., Moschi A. Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58:159-172.
21 Hughston J.C., Barrett G.R. Acute anteromedial rotatory instability. Long-term results of surgical repair. J Bone Joint Surg Am. 1983;65:145-153.
22 Hughston J.C., Eilers A.F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55:923-940.
23 Indelicato P.A. Non-operative treatment of complete tears of the medial collateral ligament of the knee. J Bone Joint Surg Am. 1983;65:323-329.
24 Indelicato P.A., Hermansdorfer J., Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990;256:174-177.
25 Jokl P., Kaplan N., Stovell P., Keggi K. Non-operative treatment of severe injuries to the medial and anterior cruciate ligaments of the knee. J Bone Joint Surg Am. 1984;66:741-744.
25a Jones R.E., Henley M.B., Francis P. Nonoperative management of isolated grade III collateral ligament injury in high school football players. Clin Orthop Rel Res. 1986;213:137-140.
26 Kannus P. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res. 1988;226:103-112.
27 Millett P.J., Pennock A.T., Sterett W.I., Steadman J.R. Early ACL reconstruction in combined ACL-MCL injuries. J Knee Surg. 2004;17:94-98.
28 Najibi S., Albright J.P. The use of knee braces, part 1: prophylactic knee braces in contact sports. Am J Sports Med. 2005;33:602-611.
29 Nakamura N., Horibe S., Toritsuka Y., et al. Acute grade III medial collateral ligament injury of the knee associated with anterior cruciate ligament tear. The usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med. 2003;31:261-267.
30 Noyes F.R., Barber-Westin S.D. The treatment of acute combined ruptures of the anterior cruciate and medial ligaments of the knee. Am J Sports Med. 1995;23:380-389.
31 Noyes F.R., Grood E.S., Torzilli P.A. Current concepts review. The definitions of terms for motion and position of the knee and injuries of the ligaments. J Bone Joint Surg Am. 1989;71:465-472.
31a Petermann J., von Garrel T., Gotzen L. Non-operative treatment of acute medial collateral ligament lesions of the knee joint. Knee Surg Sports Traumatol Arthosc. 1993;1:93-96.
32 Petersen W., Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament. Early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg. 1999;119:258-262.
33 Peterson L., Junge A., Chomiak J., et al. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28(5 suppl):S51-S57.
33a Reider B., Sathy M.R., Talkington J., et al. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. A five-year follow-up study. Am J Sports Med. 1994;22:470-477.
34 Robins A.J., Newman A.P., Burks R.T. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med. 1993;21:20-25.
35 Robinson J.R., Bull A.M., Amis A.A. Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38:1067-1074.
36 Robinson J.R., Bull A.M., Thomas R.R., Amis A.A. The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med. 2006;34:1815-1823.
37 Robinson J.R., Sanchez-Ballester J., Bull A.M., et al. The posteromedial corner revisited. An anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg Br. 2004;86:674-681.
38 Rubman M.H., Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med. 1998;26:87-95.
39 Rubman M.H., Noyes F.R., Barber-Westin S.D. Technical considerations in the management of complex meniscus tears. Clin Sports Med. 1996;15:511-530.
40 Shelbourne K.D., Baele J.R. Treatment of combined anterior cruciate ligament and medial collateral ligament injuries. Am J Knee Surg. 1988;1:56-58.
41 Shelbourne K.D., Nitz P.A. The O’Donoghue triad revisited. Combined knee injuries involving anterior cruciate and medial collateral ligament tears. Am J Sports Med. 1991;19:474-477.
42 Shelbourne K.D., Patel D.V. Management of combined injuries of the anterior cruciate and medial collateral ligaments. J Bone Joint Surg Am. 1995;77:800-806.
43 Shelbourne K.D., Porter D.A. Anterior cruciate ligament–medial collateral ligament injury: nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med. 1992;20:283-286.
44 Sims W.F., Jacobson K.E. The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med. 2004;32:337-345.
45 Warren L.F., Marshall J.L. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61:56-62.
46 Yoshiya S., Kuroda R., Mizuno K., et al. Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med. 2005;33:1380-1385.
47 Yoshiya S., Kuroda R., Mizuno K., et al. Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med. 2005;33:1380-1385.