CHAPTER 90 Mechanisms of Normal and Abnormal Swallowing
Stages of Normal Deglutition
Swallowing is a complex neuromuscular function involving structures in the oral cavity, pharynx, larynx, and esophagus. Various researchers have divided normal swallowing into four stages: the oral preparatory stage, the oral stage, the pharyngeal stage, and the esophageal stage.1–5 The first two stages, the oral preparatory and the oral, are under voluntary control, whereas the second two stages, the pharyngeal and esophageal, are involuntary, being under reflexive control.6,7 The oral stage of swallow is under voluntary control, whereas the pharyngeal swallow is no longer considered a reflex but rather a programmed activity; the motor program varies with the characteristics of the food being swallowed (i.e., the bolus), voluntary control, and other as yet undefined parameters.
Voluntary Stages of the Swallow
Oral Preparatory Stage
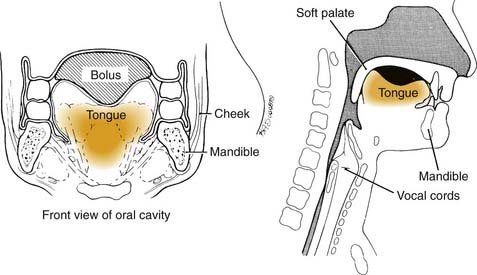
The oral preparatory aspect of deglutition, which prepares food for the swallow, involves the coordination of (1) lip closure to hold food in the mouth anteriorly, (2) tension in the labial and buccal musculature to close the anterior and lateral sulci, (3) rotary motion of the jaw for chewing, (4) lateral rolling motion of the tongue to position food on the teeth during mastication, and (5) bulging forward of the soft palate to seal the oral cavity posteriorly and widen the nasal airway.4 The forward position of the soft palate is not present during active chewing, and premature spillage while chewing is common and normal in people of all ages. Much of this coordination requires cerebellar input.8 The oral phase of deglutition is mechanical in that it involves the reduction of solid food to a pulverized consistency that may be easily swallowed. The most important neuromuscular function involved in the oral preparatory phase is the lateral rolling motion of the tongue.9 Without normal range-of-tongue motion, the manipulation and mastication of food during the oral preparatory phase would be impossible. At the termination of the oral preparatory phase, the tongue pulls the food together into a ball or bolus and holds it in a cohesive fashion on the floor of the mouth or against the hard palate (Fig. 90-1) in preparation for the beginning of the oral phase of the swallow.4,7,10–13
Oral Stage
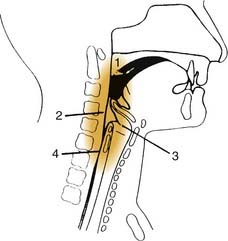
The oral stage of the swallow is also a mechanical, voluntary stage and is designed to move food from the front of the oral cavity to the pharynx, wherein the pharyngeal stage of swallow is initiated. Again, tongue motion is the most critical element in this phase of the swallow because the tongue shapes, lifts, and squeezes the bolus upward and backward along the hard palate until the food reaches the pharynx.14–17 During this posterior propulsion by the midline of the tongue, the lateral margins of the tongue are sealed against the alveolar ridge, providing resistance against which the midline of the tongue propels the bolus.15 Tension in the buccal musculature is also thought to contribute to propelling the bolus backward, but to a much lesser degree than tongue movements.18 When the head or leading edge of the mandible crosses the tongue base, the pharyngeal swallow should be triggered in healthy people of all ages (Fig. 90-2). The pharyngeal swallow is usually triggered by the glossopharyngeal nerve (C9). In healthy people, the oral stage lasts no more than 1 to 1.5 seconds and is slightly prolonged with increasing age and with increasing viscosity of the bolus swallowed.5,19
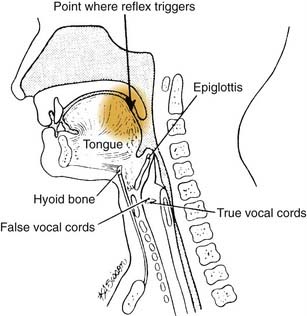
Figure 90-2. The lateral view of the head and neck illustrating the normal point at which swallowing reflex triggers.
In animal studies and in healthy humans, the pharyngeal swallow has been found to be triggered not only from C9 but also from the superior laryngeal nerve at the inlet of the larynx.20–25 Normal swallowing does not use this secondary mechanism for triggering the pharyngeal swallow because food would have almost entered the airway by the time the pharyngeal swallow was triggered. Thus when videofluoroscopic examination of a patient shows that the pharyngeal swallow triggers late, as food is about to enter the airway or after the bolus has come to rest in the valleculae or pyriform sinuses, the patient is said to have a disorder of swallowing called a delayed triggering of the pharyngeal swallow.
Programmed Stages of the Swallow
Pharyngeal Stage
The pharyngeal swallow is mediated in the lower brainstem (the medulla) in the reticular formation immediately adjacent to the respiratory center. Coordination exists between these two centers because respiration ceases for a fraction of a second when the airway closes during the pharyngeal swallow. There is also cortical input to the triggering of the pharyngeal swallow through the tongue movement patterns in the oral phase of the swallow.20 The exact neurologic substrate for this cortical input is not clearly understood.26
Neuromuscular Activities Characteristic of the Pharyngeal Swallow
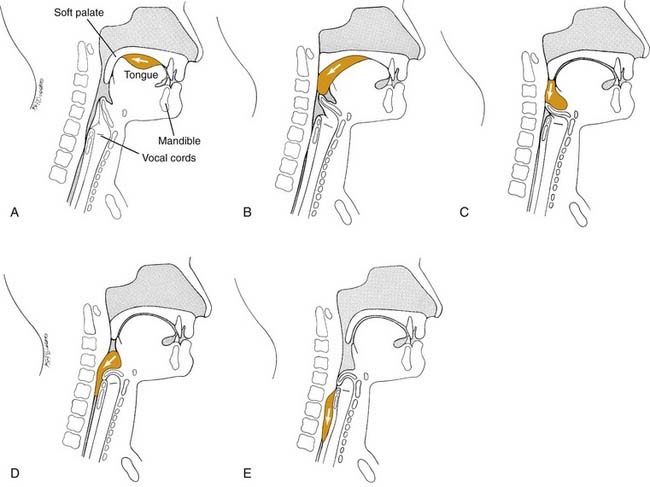
When the swallowing reflex is triggered, the brainstem swallowing center programs five neuromuscular activities to occur (Fig. 90-3). If triggering of the pharyngeal swallow is delayed, none of these neuromuscular activities occurs until pharyngeal swallow triggers (1) velopharyngeal closure to prevent backflow of material up the nose; (2) tongue base retraction to propel the bolus through the pharynx; (3) pharyngeal contraction to clear residue through the pharynx; (4) airway protection, which involves both elevation and closure of the larynx; and (5) cricopharyngeal or upper esophageal sphincter (UES) opening to allow the bolus to pass into the esophagus.1,2,27–33
Velopharyngeal closure and hyoid and laryngeal elevation occur as the first response to triggering the pharyngeal swallow. Then laryngeal closure occurs, followed closely by opening of the cricopharyngeal sphincter. These neuromuscular functions also overlap but do not all last for the entire pharyngeal stage of the swallow. Instead, each lasts only as long as the bolus is passing that part of the pharynx. When the bolus has reached the middle to lower pharynx, the soft palate lowers. At that time, the larynx is closed and elevated and the upper esophageal sphincter is open, preventing the passing bolus from entering the airway and allowing it to enter the esophagus. The duration of the pharyngeal stage of the swallow normally lasts a maximum of 1 second and does not vary dramatically with the consistency of food or age or gender of the patient.5,19
Airway Protection
Airway protection, as noted previously, involves two dimensions: elevation and closure. Elevation is created by contraction of strap musculature, which positions the larynx upward and forward under the tongue base as it is retracted at the end of the oral phase of the swallow. The larynx is pulled up and out of the way of the passage of the food bolus over the base of the tongue. Closure of the larynx involves three sphincters: the epiglottis and aryepiglottic folds, the false vocal folds and airway entrance, and the true vocal folds.27,28,34–36 The relative importance of each of the three sphincters has been debated in the literature.35,37,38 Most authors agree that the epiglottis and aryepiglottic folds play a relatively minor role in protecting the airway; their purpose is to divert food around the airway. The most important level of closure, airway entrance closure, is maintained only for the fraction of a second that the bolus is passing the airway.
Cricopharyngeal (Upper Esophageal Sphincter) Opening
The cricopharyngeus muscle acts in opposition to the function of the constrictor mechanism of the pharynx. At rest the constrictors are relaxed, and the cricopharyngeus muscle or upper esophageal sphincter is in tonic contraction to prevent air intake into the esophagus concurrent with inhalation into the lungs. Also, the contracted cricopharyngeus muscle prevents backflow from the esophagus into the pharynx.1 During the swallow, as the constrictor mechanism is contracting, the cricopharyngeus muscle relaxes at the appropriate moment. The anterior superior movement of the larynx opens the UES, and the bolus passes into the esophagus. The duration of UES opening and airway closure increases as bolus volume increases.39
Pharyngeal Pressure Generation: Tongue Base Retraction and Pharyngeal Contraction
When the tail of the bolus reaches the tongue base, the tongue base moves rapidly backward like a piston, increasing pressure in the pharynx. As the tongue base moves backward, the lateral and posterior pharyngeal walls at the tongue base level move inward. The tongue base and pharyngeal walls should make complete contact. Electromyographic and radiographic studies have shown that pharyngeal contraction, or the squeezing action of the constrictor mechanism to move the bolus through the pharynx, occurs sequentially, beginning in the superior constrictor muscle and moving through the medial to the inferior constrictor muscle.29,40
Pharyngeal contraction is responsible for clearing material from the pharyngeal walls and pyriform sinuses. When residue or material remains in the valleculae after the swallow, it is interpreted as a symptom of reduced tongue base movement.41 Tongue base movement occurs later as bolus volume increases.
Esophageal Stage
When the bolus has passed through the UES, the esophageal phase of swallow begins. The esophageal stage has greater variability in duration than the other stages of the swallow. Normal esophageal transit may vary from 8 to 20 seconds.4 The upper third of the esophagus is composed of mixed voluntary and involuntary muscle, and the lower two thirds is composed entirely of involuntary muscle. The lower esophageal sphincter acts as a valve to the stomach, which must open in time to allow the bolus to pass from the esophagus into the stomach.
Figure 90-4 illustrates the progression of the bolus through the pharynx. If an anatomic or neuromuscular disorder affects the pharyngeal stage of the swallow, aspiration may result.
Signs and Symptoms of Abnormal Swallow
Aspiration (Coughing, Choking)
Aspiration is the entry of material into the airway below the true vocal folds. The effect of chronic aspiration in adults is not well understood, but in the long term it may result in pneumonia or pulmonary changes. Patients who are observed to aspirate on a radiographic study of swallowing are at significantly greater risk of pneumonia developing than patients who do not show aspiration on such a study. Many patients with head and neck cancer who have chronic aspiration do not survive long enough to experience the long-term effects of their aspiration. Aspiration may occur before, during, or after the pharyngeal swallow.4 Aspiration that occurs before the pharyngeal swallow may result from one of two disorders: reduced tongue control or a delayed or absent pharyngeal swallow. When tongue control is reduced during the oral preparatory or oral stages of the swallow, bits and pieces of food may fall into the pharynx and the open airway as the patient chews. Importantly, the airway is normally open during the oral preparatory and oral stages of the swallow. The airway is closed only for a fraction of a second during the pharyngeal swallow. Aspiration before the swallow can also occur because of a delayed or absent pharyngeal swallow. In these patients, the food is propelled out of the oral cavity by the tongue and falls into the pharynx, wherein it may come to rest in the valleculae, the pyriform sinus, or the airway before the pharyngeal swallow is triggered. The entry of food into the airway does not always trigger a cough, particularly in neurologically impaired patients and some patients with head and neck cancer in whom sensory input is damaged.41,42
Evaluation of Swallowing
Videofluoroscopy
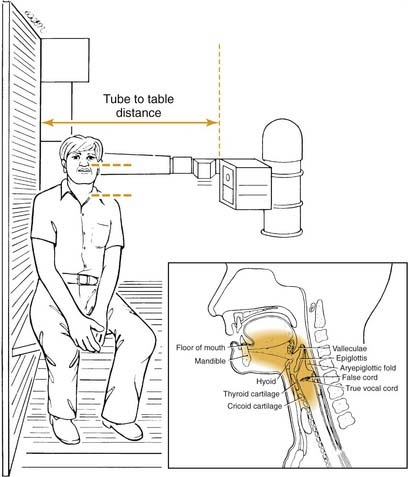
During the MBS, the patient is seated upright in a normal eating position. In dysphagic patients, the physiology of the oral cavity and pharynx in the normal eating position must be established first. Then, if desired, the patient’s position can be changed to note the postural effects on food flow during swallowing. In the modified barium swallow procedure, the patient is initially viewed in the lateral plane with the fluoroscopy tube focused on the lips anteriorly and the seventh cervical vertebra inferiorly as shown in Figure 90-5. This allows complete assessment of oral and pharyngeal motility and of aspiration during the pharyngeal aspect of the swallow. In the anteroposterior view, the trachea overlies the esophagus, making assessment of aspiration difficult.
The major purposes of the modified barium swallow are to (1) define the immediate oral and pharyngeal motility disorders during the swallow; (2) identify the presence of aspiration during swallow of any food consistency; (3) assess the speed of the swallow (compared with normal); and (4) assess the effects of therapy strategies such as postural changes, heightened sensory input, and therapy procedures including swallowing maneuvers.16,36,41,43–50 If the patient aspirates or has a highly inefficient swallow, treatment procedures are introduced during the videofluoroscopic study to improve the swallow and allow the patient to continue to eat orally or return to oral intake as quickly as possible. The purpose of the test is to restore oral intake—not to stop the patient from eating.
Endoscopy
Endoscopy by way of transnasal placement of a flexible fiberoptic scope has been used to evaluate some selected aspects of the swallow.50–53 The oral stages cannot be viewed, and during the swallow the image disappears as the pharynx contracts and closes against the scope. Any residual food in the pharynx after the swallow may be identified, as may any aspiration of the residue after the swallow.
Manometry
Manometry is usually used to examine esophageal peristalsis and the adequacy of functioning of the upper and lower esophageal sphincters.3,54,55 The patient swallows a soft tube containing pressure sensors. These sensors are positioned so that one registers the pressure in the UES, the second registers pressure changes in the body of the esophagus, and the third registers pressure in the lower esophageal sphincter. The gauges also may be positioned to register pressure in the pharynx, cricopharyngeal sphincter, and the body of the esophagus, thus permitting observation of the temporal relationship between pharyngeal contraction and opening of the cricopharyngeal sphincter.
Swallowing Disorders Resulting from Treatment for Head and Neck Cancer
Radiotherapy
Radiotherapy for the oral cavity and pharynx, in addition to reducing salivary flow and causing short-term oral or pharyngeal edema, may lead to difficulties with triggering of the pharyngeal swallow, laryngeal elevation, and pharyngeal contraction that may begin immediately or months after the therapy is completed.4,56 Presumably, the problem with laryngeal elevation and pharyngeal contraction relates to increased fibrosis after radiation. The symptoms vary in duration and severity and may appear 6 months or more after completion of a full course of radiotherapy. The long-term effects of radiotherapy on swallowing deserve greater attention and more thorough study.
Surgical Treatment
The effects of surgical treatment for patients with head and neck cancer on swallowing depend on the site and extent of the resection and the nature of reconstruction.4,57,58 Some data indicate that the reconstruction determines the swallowing pattern of the patient postoperatively, particularly when smaller amounts of tissue are resected.
Tongue
Within the oral cavity, the tongue is the most important organ for maintaining normal food intake. The tongue is responsible for oral manipulation and chewing to prepare food for the swallow and is responsible for the oral initiation of the swallow. Every effort should be made to permit as much range and coordination of tongue motion as possible. Use of the tongue in surgical closure may dramatically reduce the patient’s ability to handle a normal diet.16
Posterior Oral Cavity
When a tumor invades the posterior oral cavity, a number of swallowing actions may be affected59 including tongue mobility during oral preparation and the oral initiation of the swallow, triggering of the pharyngeal swallow, velopharyngeal closure, tongue base retraction, and pharyngeal contraction. Surgery at the tonsil and base of the tongue directly invades the sensory area where the pharyngeal swallow is usually triggered and also damages the attachments of the pharyngeal constrictors into the base of the tongue, thus reducing tongue base retraction and pharyngeal contraction. Reconstruction of this area with a thick and bulky flap interferes with functioning of the pharynx, tongue, and remaining healthy tissues.60
Pharynx
Surgical involvement of the pharyngeal wall itself may dramatically impair pharyngeal contraction. If the surgical resection involves only one side of the pharynx, the patient may turn his or her head to the operated side to assist swallowing on the unoperated and less damaged side, thus directing food down the more normal side.43 Alternately, the patient may tilt his or her head toward the more normal side to assist gravitational drainage of food down the stronger side. As in the oral cavity, the nature of the reconstruction may interfere with function on the unoperated side so that even with a change in head position the patient is permanently unable to handle food thicker than liquid and may even have difficulty with liquid. Greater pharyngeal peristalsis is required to move heavier and thicker food than is required for liquid.
Larynx
After hemilaryngectomy, laryngeal closure is the greatest problem.4 Depending again on the nature of the reconstruction and on the nature and amount of tissue positioned on the resected side, many patients regain normal swallowing in a relatively short time (1 month) after hemilaryngectomy with swallowing retraining, which usually involves laryngeal adduction exercises.61
Patients who have undergone supraglottic laryngectomy often have multiple problems with swallowing, which may include reduction in laryngeal elevation, laryngeal entrance closure, and tongue base retraction.62 During the supraglottic laryngectomy procedure, portions or all of the hyoid bone are removed, and thus laryngeal suspension from the hyoid is disturbed.63,64 Resultant residue at the top of the larynx may be aspirated after the swallow when the patients open the larynx and inhale. Airway protection in these patients is achieved by retraction of the tongue base to contact the anteriorly tilting arytenoid cartilages.65 Any damage to the tongue base or the arytenoid cartilages or their function in adduction and anterior tilting results in inability to protect the airway and aspiration after the swallow.
Summary
Studies have shown that the bedside evaluation of aspiration may be as much as 40% in error in identifying patients who are aspirating50 and cannot identify the underlying causes so that effective management may be planned. Optimum treatment of a patient with a swallowing disorder involves videofluoroscopic evaluation of swallowing at the time oral feeding is to be reinitiated so that appropriate swallowing therapy may be planned, the patient may be quickly advanced to as normal a diet as possible, and potential complications from chronic aspiration, malnutrition, or dehydration may be avoided.
Ardran J, Kemp F. Closure and opening of the larynx during swallowing. Br J Radiol. 1956;29:205.
Bastian RN. Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg. 1991;104:339.
Jacob P, Kahrilas P, Logemann J, et al. Upper esophageal sphincter opening and modulation during swallowing. Gastroenterology. 1989;97:1469.
Kahrilas PJ, Lin S, Logemann JA, et al. Deglutitive tongue action: volume accommodation and bolus propulsion. Gastroenterology. 1993;104:152.
Kahrilas PJ, Logemann JA. Volume accommodations during swallowing. Dysphagia. 1993;8:259.
Kahrilas PJ, Logemann JA, Krugler C, et al. Volitional augmentation of upper esophageal sphincter opening during swallowing. Am J Physiol. 1991;260:G450.
Kahrilas PJ, Logemann JA, Lin S, et al. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992;103:128.
Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216.
Lazarus C, Logemann JA, Gibbons P. Effects of maneuvers on swallowing function in a dysphagic oral cancer patient. Head Neck. 1993;15:419.
Lazarus CL, Logemann JA, Pauloski BR, et al. Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy. Laryngoscope. 1996;106:1157.
Logemann J. Evaluation and Treatment of Swallowing Disorders, 2nd ed. Austin, TX: Pro-Ed; 1998.
Logemann JA. A Manual for Videofluoroscopic Evaluation of Swallowing, 2nd ed. Austin, Texas: Pro-Ed; 1993.
Logemann J, Bytell D. Swallowing disorders in three types of head and neck surgical patients. Cancer. 1979;44:1075.
Logemann JA, Kahrilas PJ, Cheng J, et al. Closure mechanisms of the laryngeal vestibule during swallow. Am J Physiol. 1992;262:G338.
Logemann J, Kahrilas P, Kobara M, Vakil NB. The benefit of head rotation on pharyngo-esophageal dysphagia. Arch Phys Med Rehabil. 1989;70:767.
Logemann JA, Pauloski BR, Rademaker AW, et al. Speech and swallow function after tonsil/base of tongue resection w/primary closure. J Speech Hear Res. 1993;36:918.
Logemann JA, Rademaker AW, Pauloski BR, et al. Effects of postural change on aspiration in head and neck surgical patients. Otolaryngol Head Neck Surg. 1994;110:222.
Logemann JA, Gibbons P, Rademaker AW, et al. Mechanisms of recovery of swallow after supraglottic laryngectomy. J Speech Hear Res. 1994;37:965.
Martin-Harris B, Logemann JA, McMahon S, et al. Clinical utility of the modified barium swallow. Dysphagia. 2000;15:136.
Martin BJW, Logemann JA, Shaker R, et al. Normal laryngeal valving patterns during three breath-hold maneuvers: a pilot investigation. Dysphagia. 1993;8:11.
Rademaker AW, Logemann JA, Pauloski BR, et al. Recovery of postoperative swallowing in patients undergoing partial laryngectomy. Head Neck. 1993;15:325.
Rasley A, Logemann JA, Kahrilas PJ, et al. Prevention of barium aspiration during videofluoroscopic swallowing studies: value of change in posture. Am J Roentgenol. 1993;160:1005.
Robbins J, Hamilton JW, Lof GL, et al. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103:823.
Veis S, Logemann J. The nature of swallowing disorders in CVA patients. Arch Phys Med Rehabil. 1985;66:372.
1. Ardran J, Kemp F. The mechanism of swallowing. Proc R Soc Med. 1951;44:1038.
2. Bosma J. Deglutition: pharyngeal stage. Physiol Rev. 1957;37:275.
3. Fyke F, Code C. Resting and deglutition pressures in the pharyngo esophageal region. Gastroenterology. 1955;29:24.
4. Logemann J. Evaluation and treatment of swallowing disorders, 2nd ed. Austin, TX: Pro-Ed; 1998.
5. Mandelstam P, Lieber A. Cineradiographic evaluation of the esophagus in normal adults. Gastroenterology. 1970;58:32.
6. Miller A. Characteristics of the swallowing reflex induced by peripheral nerve and brain stem stimulation. Exp Neurol. 1972;34:210.
7. Sessle B, Hannan A. Mastication and swallowing. Toronto: University of Toronto Press; 1976.
8. Larson C, Sutton D. Effects of cerebellar lesions on monkey jaw-force control: implications for understanding ataxic dysarthria. J Speech Hear Res. 1978;21:295.
9. Ingervall B. Activity of temporal and lip muscles during swallowing and chewing. J Oral Rehabil. 1978;5:329.
10. Dodds WJ, Taylor AJ, Stewart ET, et al. Tipper and dipper types of oral swallows. Am J Roentgenol. 1989;153:1197.
11. Shawker T, Sonies B, Stone B. Soft tissue anatomy of the tongue and floor of the mouth; an ultrasound demonstration. Brain Lang. 1984;21:335.
12. Shawker T, Sonies JS, Stone M. Real-time ultrasound visualization of tongue movement during swallowing. J Clin Ultrasound. 1983;11:485.
13. Shedd D, Kirschner J, Scatliff J. Oral and pharyngeal components of deglutition. Arch Surg. 1961;82:371.
14. Hryeyshyn A, Basmajian J. Electromyography of the oral stage of swallowing in man. Am J Anat. 1972;133:333.
15. Kahrilas PJ, Lin S, Logemann JA, et al. Deglutitive tongue action: volume accommodation and bolus propulsion. Gastroenterology. 1993;104:152.
16. Kahrilas PJ, Logemann JA, Krugler C, et al. Volitional augmentation of upper esophageal sphincter opening during swallowing. Am J Physiol. 1991;260:G450.
17. Lowe A. The neural regulation of tongue movement. Prog Neurobiol. 1981;15:295.
18. Shedd D, Scatliff J, Kirscher J. The buccopharyngeal propulsive mechanism in human deglutition. Surgery. 1960;48:846.
19. Blonsky E, Logemann JA, Boshes B, et al. Comparison of speech and swallowing function in patients with tremor disorders and in normal geriatric patients: a cinefluorographic study. J Gerontol. 1975;30:299.
20. Jean A, Car A. Inputs to the swallowing medullary neurons from the peripheral afferent fibers and the swallowing cortical area. Brain Res. 1979;178:567.
21. Hollshwandner J, Brenman HS, Friedman MH. Role of afferent sensors in the initiation of swallowing in man. J Dent Res. 1975;54:83.
22. Jean A, Car A, Roman C. Comparison of activity upon time versus medullary neurones during swallowing. Exp Brain Res. 1975;22:211.
23. Mansson I, Sandberg N. Oropharyngeal sensitivity and elicitation of swallowing in man. Acta Otolaryngol. 1975;79:140.
24. Miller A, Loizzi R. Anatomical and functional differentiation of superior laryngeal nerve fibers affecting swallowing and respiration. Exp Neurol. 1974;42:369.
25. Pommerenke W. A study of the sensory areas eliciting the swallowing reflex. Am J Physiol. 1928;84:36.
26. Veis S, Logemann J. The nature of swallowing disorders in CVA patients. Arch Phys Med Rehabil. 1985;66:372.
27. Ardran J, Kemp F. The protection of the laryngeal airway during swallowing. Br J Radiol. 1952;25:406.
28. Logemann JA, Kahrilas PJ, Cheng J, et al. Closure mechanisms of the laryngeal vestibule during swallow. Am J Physiol. 1992;262:G338.
29. Kahrilas PJ, Logemann JA, Lin S, et al. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992;103:128.
30. Jacob P, Kahrilas P, Logemann J, et al. Upper esophageal sphincter opening and modulation during swallowing. Gastroenterology. 1989;97:1469.
31. Kirchner J. The motor activity of the cricopharyngeus muscle. Laryngoscope. 1958;68:1119.
32. Negus V. The second stage of swallowing. Acta Otolaryngol. 1949;78(Suppl):75.
33. Ohmae Y, Logemann JA, Kaiser P, et al. Timing of glottic closure during normal swallow. Head Neck. 1995;17:394.
34. Ardran J, Kemp F. Closure and opening of the larynx during swallowing. Br J Radiol. 1956;29:205.
35. Ardran J, Kemp F. The mechanism of the larynx. II. The epiglottis and closure of the larynx. Br J Radiol. 1967;40:372.
36. Rasley A, Logemann JA, Kahrilas PJ, et al. Prevention of barium aspiration during videofluoroscopic swallowing studies: value of change in posture. Am J Roentgenol. 1993;160:1005.
37. Fink R. The Human Larynx: A Functional Study. New York: Raven Press; 1975.
38. Fink R, Demarest R. Laryngeal Biomechanics. Cambridge, Massachusetts: Harvard University Press; 1978.
39. Kahrilas PJ, Logemann JA. Volume accommodations during swallowing. Dysphagia. 1993;8:259.
40. Doty R, Bosma J. An electro myographic analysis of reflex deglutition. J Neurophysiol. 1956;19:44.
41. Logemann JA. A Manual for Videofluoroscopic Evaluation of Swallowing, ed 2. Austin, Texas: Pro-Ed; 1993.
42. Linden P, Siebens A. Dysphagia: predicting laryngeal penetration. Arch Phys Med Rehabil. 1983;64:281.
43. Logemann J, Kahrilas P, Kobara M, Vakil NB. The benefit of head rotation on pharyngo-esophageal dysphagia. Arch Phys Med Rehabil. 1989;70:767.
44. Logemann JA. Preswallow sensory input: its potential importance to dysphagic patients and normal individuals [editorial]. Dysphagia. 1996;11:9.
45. Lazarus C, Logemann JA, Gibbons P. Effects of maneuvers on swallowing function in a dysphagic oral cancer patient. Head Neck. 1993;15:419.
46. Logemann JA, Kahrilas PJ. Relearning to swallow post CVA: application of maneuvers and indirect biofeedback: a case study. Neurology. 1990;40:1136.
47. Logemann JA, Rademaker AW, Pauloski BR, et al. Effects of postural change on aspiration in head and neck surgical patients. Otolaryngol Head Neck Surg. 1994;110:222.
48. Martin-Harris B, Logemann JA, McMahon S, et al. Clinical utility of the modified barium swallow. Dysphagia. 2000;15:136.
49. Martin BJW, Logemann JA, Shaker R, et al. Normal laryngeal valving patterns during three breath-hold maneuvers: a pilot investigation. Dysphagia. 1993;8:11.
50. Robbins J, Hamilton JW, Lof GL, et al. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103:823.
51. Bastian RN. Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg. 1991;104:339.
52. Kidder TM, Langmore SE, Martin BW. Indications and techniques of endoscopy in evaluation of cervical dysphagia: comparison with radiographic techniques. Dysphagia. 1994;9:256.
53. Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2:216.
54. Kelley M. Evaluation of the patient with dysphagia. Mod Treat. 1970;27:1087.
55. Van Trappen G, Hellemans J. Studies on the normal deglutition complex. Am J Dig Dis. 1978;12:255.
56. Lazarus CL, Logemann JA, Pauloski BR, et al. Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy. Laryngoscope. 1996;106:1157.
57. Logemann J, Bytell D. Swallowing disorders in three types of head and neck surgical patients. Cancer. 1979;44:1075.
58. McConnel FMS, Logemann JA, Rademaker AW, et al. Surgical variables affecting postoperative swallowing efficiency in oral cancer patients: a pilot study. Laryngoscope. 1994;104:87.
59. Logemann JA, Pauloski BR, Rademaker AW, et al. Speech and swallow function after tonsil/base of tongue resection w/primary closure. J Speech Hear Res. 1993;36:918.
60. McConnel F, Teechgraeber R. Comparison of three methods of oral reconstruction, their effects on speech and tongue motion, paper presented at the American Academy of Facial Plastic and Reconstructive Surgery. Palm Beach, May 1982.
61. Jenkins P, Logemann J, Lazarus C. Functional changes after hemilaryngectomy, paper presented at the American Speech Language Hearing Association annual meeting. Los Angeles, 1981.
62. Rademaker AW, Logemann JA, Pauloski BR, et al. Recovery of postoperative swallowing in patients undergoing partial laryngectomy. Head Neck. 1993;15:325.
63. Ogura JH, Biller HF, Calcateura TC. Surgical treatment of carcinoma of the larynx, pharynx, base of tongue and cervical esophagus. Intern Surg. 1969;52:29.
64. Shumrick D, Keith R. Conservation surgery of the larynx, scientific exhibit at the ASHA Annual Meeting. Denver, 1968.
65. Logemann JA, Gibbons P, Rademaker AW, et al. Mechanisms of recovery of swallow after supraglottic laryngectomy. J Speech Hear Res. 1994;37:965.