Maxillary Deficiency with Relative Mandibular Excess Growth Patterns
• The Role of Growth Modification in the Preadolescent Patient
• Orthodontic Camouflage Approach
• Surgical Camouflage Approach
• Postsurgical Orthodontic Maintenance and Detailing
• Complications, Informed Consent, and Patient Education
• Malocclusion after Orthodontics and Orthognathic Surgery
• Temporomandibular Disorders: The Effects of Orthodontics and Orthognathic Surgery
Developmental Class III skeletal problems generally result from maxillary deficiency in combination with relative mandibular excess. Through trial and error, it is now recognized that either growth modification in the preadolescent patient or camouflage treatment in the teenager or adult as a method of managing this type of dentofacial deformity is at best relatively ineffective. In addition, even mild degrees of a Class III facial appearance are aesthetically noticeable as unattractive by the general population.76 Therefore, the perceived need for treatment (i.e., de facto orthognathic surgery) for the Class III patient—whether by the public, the evaluating clinicians, the affected individual, or the patient’s family and friends—will be high.13,72,78,125
There is a strong family tendency for a Class III skeletal pattern. The so-called “Habsburg jaw” within the royal European family is well documented.58,104,106,122,124 The frequency of Class III skeletal patterns among white people of European or North American ancestry is reported to have a prevalence in the low single digits. There is a somewhat higher prevalence of Class III skeletal patterns among Africans than among Caucasians.27 Data from Japan, Korea, and China confirm a more frequent Class III pattern among Asians than among any other subgroup (i.e., >4%).28,117 Incidence rates of Class III malocclusion of as high as 13% have been reported in specific regions of Asia.119 Lew and colleagues examined occlusal parameters in 1050 Chinese schoolchildren who were between 12 and 14 years old.48 They found an incidence of 12.6% for Class III malocclusion, 58.8% for Class I occlusion, and 21.5% for Class II malocclusion. Samman and colleagues investigated 300 Chinese individuals residing in Hong Kong who were known to have dentofacial deformities and who had been referred to an “orthognathic surgery clinic.”91 After excluding those individuals with cleft lip and palate, 222 study patients remained. Forty-seven percent of these individuals (n = 104) were found to have a Class III skeletal malocclusion.
Despite hereditary tendencies, the development of a Class III jaw disharmony is believed to be multifactorial and complex.8,33,39,57 Alternatively, it has been documented that environmental factors have a significant effect on vertical facial growth (see Chapter 21). The combination of an individual’s hereditary tendency toward a Class III skeletal pattern and a longstanding, forced mouth breathing, open-jaw posture during growth explains the occasional occurrence of a long face growth pattern (i.e., excess vertical growth) with Class III negative overjet malocclusion.29 An outlier for a Class III skeletal pattern is the impaired midface growth that is seen in many individuals from all backgrounds with repaired cleft palates (see Chapters 32, 33, and 34). Another commonly seen clinical pattern is the individual with maxillary vertical deficiency and a prominent pogonion (i.e., pseudoprognathism) as a result of “over closure” (see Chapter 23).97,99,109
An additional source of data regarding the prevalence of individuals with skeletal Class III is the National Health and Nutrition Examination Survey III, a large-scale epidemiologic survey of the U.S. population that was carried out during the 1990s (see Chapter 3).77 The data from this study confirm that Class III problems increase from early childhood through adolescence.1,18 This can be explained by the expected late growth spurt in the mandible as compared with the maxilla. The study also confirmed that the presence of 2 mm or more of negative overjet is about twice as likely to occur among African Americans than among Caucasian Americans or Mexican Americans. Data from a U.S. public health survey of youths between the ages of 12 and 17 years indicates that about 14% have a mandibular first molar that is mesial in relation to the maxillary first molar.42
With regard to treatment, by the late 1800s, both Edward Angle, an orthodontist, and Vilray Blair, a surgeon, recognized that orthodontic treatment alone could not solve the Class III skeletal problem.15 Angle suggested that the only possible way to correct a true mandibular protrusion was with a combination of orthodontics and surgery.2 By the late 1800s, the initial orthognathic procedures were carried out to “set-back” the prominent mandible (see Chapter 2).
Functional Aspects
• Predictable articulation errors in speech result from a Class III malocclusion (see Chapter 8).
• Chronic obstructed nasal breathing is commonly seen in the presence of maxillary deficiency (see Chapter 10).
• Characteristic difficulties with swallowing and chewing as a result of a Class III malocclusion are expected (see Chapter 8).
• Wide lip separation (often with upper lip hypotonia) and mentalis strain required for lip seal are commonly seen in the presence of a significant negative overjet.
• Detrimental long-term effects on the dentition and the periodontium that result from a Class III malocclusion (secondary occlusal trauma), dental crowding, or previous camouflage orthodontics are often seen (see Chapter 6).
• The incidence of temporomandibular disorder (TMD) may be higher among these patients than among individuals with normal jaw harmony and occlusion (see Chapter 9).
Clinical Characteristics
Profile View
• Long chin–neck length and acute angle with a visually accentuated inferior border of the mandible
• Prominent chin with a reduced labiomental fold
• Protrusive and thick lower lip and vermillion
• Sunken-appearing midface (A negative vector relationship between the ocular globe and the lower eyelid as a result of anterior maxillary deficiency is a frequent finding.)
• Deflated, short, hypotonic appearance of the upper lip, with a thin vermillion
Frontal View
• Sunken-appearing cheeks (i.e., the impression of flat cheek bones)
• Middle one third of the face appears flat and long
• Increased scleral show (i.e., pulling down of the lower lids)
• Narrow alar base with paranasal flattening
• Flat and relatively short upper lip with reduced vermillion exposure
• Normal to deficient maxillary tooth to upper lip relationship frequently seen
Dental Characteristics
• Minimal attached gingiva over the labial aspects of the mandibular anterior teeth is frequently seen (see Chapter 6).
• Mandibular incisors are usually upright or lingually inclined.
• Interdental spacing with flared mandibular incisors may also be seen, especially in the presence of an anterior open bite with lip incompetence.
• Class III malocclusion (molar and canine) with anterior open bite, negative overjet, and posterior crossbites is frequent.
• Narrow maxillary arch width is seen as excess negative space in the buccal corridors.
• Dental crowding with flared maxillary incisors is frequent.
Radiographic Findings
• Maxillary horizontal deficiency
• Concave anterior maxilla consistent with a negative vector relationship of the ocular globe to the lower eyelid
• Flat, counterclockwise-rotated maxillary plane
• Procumbent maxillary incisors
• Flat base of the nose with retrusive pyriform rims
• Altered lower anterior facial height (either short or long)
• B-point is anterior to or in front of A-point in profile (i.e., natural head position)
• Negative overjet to the occlusion
• Prognathic-appearing mandible
• Lingually inclined mandibular incisors frequently found
• Chin morphology varies, but it is generally dysmorphic. Frequent patterns of chin dysmorphology include vertical excess with either a prominent or flat pogonion.
The Role of Growth Modification in the Preadolescent Patient
Most studies have found no difference in the ultimate size of the mandible between children with Class III conditions who were treated with a chin cup and those who were not.105 Wylhelm-Nold and colleagues presented some evidence that the use of the chin cup in preschool-aged children was able to decrease mandibular anterior growth if good compliance was achieved.123 Unfortunately, this did not prevent the mandible from continuing an excess growth pattern later during childhood, after the chin cup treatment was stopped. In fact, a rebound accelerated growth effect was documented. What chin cup therapy may accomplish is a change in the growth vector of the mandible, with more downward and backward (clockwise) rotation.37 These secondary changes have their own negative effects on facial morphology and occlusion (i.e., the law of unintended consequences).
With the realization that the presenting maxillary deficiency should be the primary focus of the correction for most skeletal Class III individuals, growth modification moved toward methods of stimulating the upper jaw. The Delaire face mask has been used extensively to pull the maxilla forward.24 The work of Baccetti and McNamara confirmed that use of the Delaire face mask for the individual with maxillary deficiency is more likely to have effect when it is used before the patient is 8 years old.6,21,92 After this age, tooth movement (dental compensation) and mandibular clockwise rotation will be the likely consequences of this form of treatment rather than the hoped for horizontal maxillary projection. In addition, many children experience recurrence of the deformity after face mask therapy is discontinued. It is unlikely that face mask (for the maxilla) and chin cup (for the mandible) interventions will be effective in the long term for preventing the need for orthognathic surgery in all but mild cases. An accepted guideline is that more than 2 to 4 mm of reverse overjet in the preadolescent child indicates that surgery will eventually be needed if both facial and dental correction are sought.
DeClerck and colleagues used orthopedic traction on the maxilla and compression on the mandible with temporary mini-plate skeletal anchorage and elastics in a limited number (n = 3) of 10- to 11-year-old children presenting with skeletal Class III malocclusions.25 Pure bone-borne orthopedic forces were applied with intermaxillary elastics on the skeletally anchored mini-plates. This approach was shown to either enhance midface growth or to hold back the mandible; in any case, the intent was to produce a corrected overjet. Although the authors were encouraged, many unknowns remained, including the ideal age for this type of orthopedic traction; the effect of the direction of force on the rotation of the palatal and mandibular planes; the long-term effects on the temporomandibular joints; and the need for retention to prevent catch-up growth of the mandible or relapse of the maxilla afterward. DeClerck’s ongoing prospective clinical trial of this promising work on a larger sample of patients (as well as the work of other independent researchers) will help to answer these questions and to determine the true effectiveness of a growth-modification approach that involves temporary skeletal anchorage and elastics.21,92
Orthodontic Camouflage Approach
It is not uncommon for the orthognathic surgeon to see an adult in consultation who is emotionally exhausted after having undergone failed growth modification followed by disappointment after additional years of camouflage orthodontics. The individual may present with 1) significant residual malocclusion (i.e., effects on speech, swallowing, and chewing) 2) deteriorating periodontal health (i.e., crest bone loss and gingival recession associated with lower anterior and upper posterior teeth), 3) often with chronic upper airway obstruction (i.e. deviated septum, hypertrophic inferior turbinates, and tight nasal apertures) and 4) self-esteem and body image issues related to the facial disproportion and disappointment with failed treatment (Figs. 20-1 through Fig. 20-4).
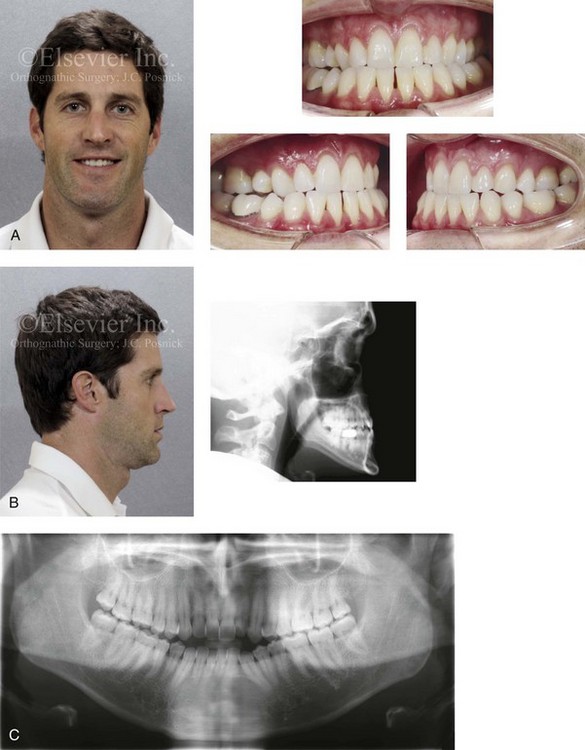
Figure 20-1 A 34-year-old male arrived for the evaluation of a longstanding jaw deformity with malocclusion, chronic obstructive nasal breathing, and periodontal issues. Since his early childhood years, the patient was known to have a maxillary deficiency with a relative mandibular excess growth pattern. The family elected a camouflage orthodontic approach that included four bicuspid extractions and the introduction of dental compensation in an attempt to neutralize the occlusion when the patient was 10 to 15 years old. He is a forced mouth breather as a result of increased nasal airway resistance. The patient underwent septoplasty when he was 20 years old, but significant improvement of the airway did not occur. His general dentist confirmed labial bone loss and gingival recession of the mandibular anterior and maxillary posterior dentition. He was referred to this surgeon, and a comprehensive orthognathic and dental rehabilitation approach was selected. Consultation with a periodontist, an orthodontist, and an ear, nose, and throat specialist was carried out. The patient was confirmed to have residual deviation of the septum and enlarged inferior turbinates, which explained the continual difficulty that he had breathing through his nose. A degree of root resorption of the anterior dentition was confirmed. The need for gingival grafting to attain improved root coverage and to generate a wider band of attachment was recommended for tooth nos. 3, 11, 14, 19, 20, 23 through 26, 29, and 30. This will be followed by the orthodontic removal of dental compensation and then orthognathic and intranasal procedures to improve long-term dental health, to enhance facial aesthetics, and to open the upper airway. A, Frontal facial and occlusal views before retreatment. B, Profile facial and lateral cephalometric radiograph before retreatment. C, Panorex radiograph before retreatment.
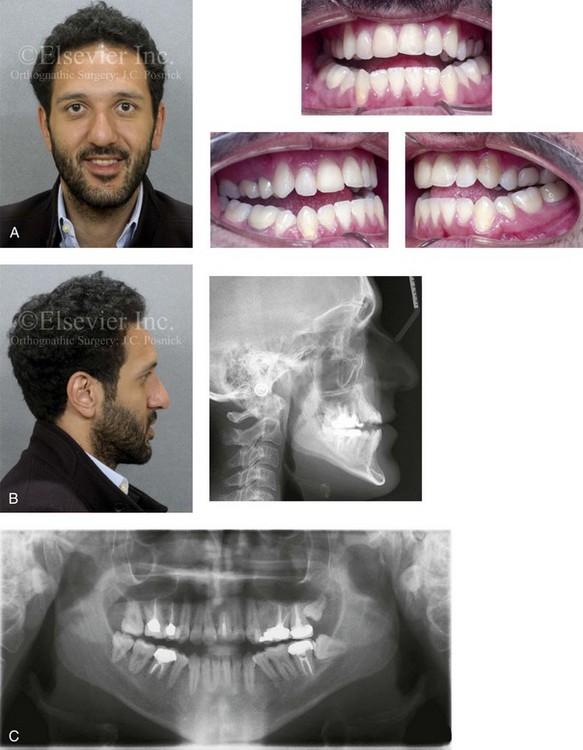
Figure 20-2 A 26-year-old man arrived for surgical evaluation. Since the mixed dentition, he had been recognized as having a developmental jaw deformity characterized by maxillary deficiency in combination with relative mandibular excess. Camouflage orthodontic treatment that included four bicuspid extractions was carried out when the patient was between 12 and 16 years old. A residual Class III negative overjet with an anterior open-bite malocclusion remains. The patient has never been able to breathe well through the nose as a result of septal deviation and inferior turbinate enlargement. Secondary occlusal trauma resulted in the need for root canal therapy and crowns in all four posterior quadrants. There is labial bone loss and gingival recession associated with the anterior mandibular teeth. A comprehensive dental rehabilitative and reconstructive approach will require periodontal evaluation and treatment followed by orthodontic decompensation and then by jaw and intranasal surgery. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment. C, Panorex radiograph before retreatment.
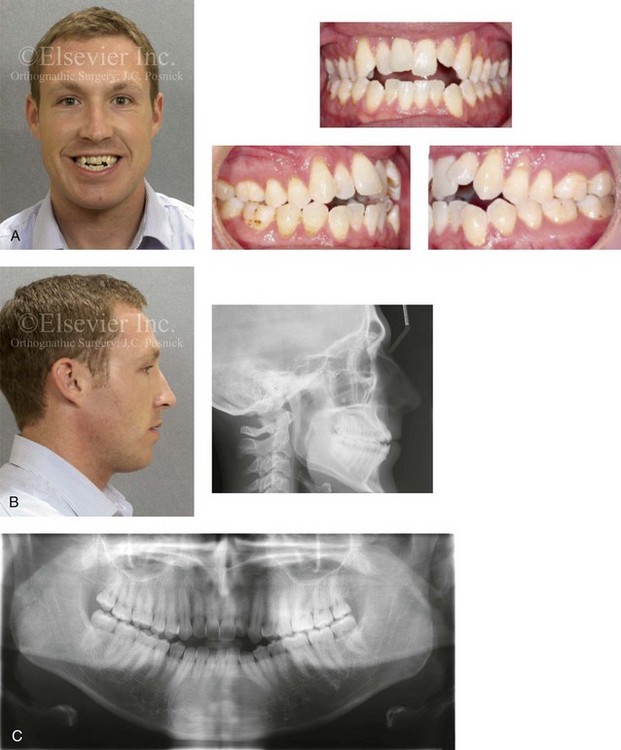
Figure 20-3 A 30-year-old man arrived for the evaluation of a longstanding jaw deformity with malocclusion, chronic obstructive nasal breathing, and an awareness of periodontal issues. Since his early childhood years, he was known to have a jaw deformity with malocclusion, including an anterior open bite. When he was between 8 and 12 years old, he underwent orthodontic camouflage treatment in an attempt to close the open bite; this included full bracketing and the use of heavy anterior elastics. By the time that he graduated from high school, he was conscious of a significant recurrent anterior open bite with dental crowding. Throughout his college years, he was aware of gingival recession on the labial aspect of many of the anterior teeth of the maxilla more so than the mandible. He was sent by his general dentist for an orthodontic evaluation and then to this surgeon for an opinion. The patient was referred for periodontal evaluation with confirmation of significant labial bone loss of the anterior dentition (more so on the maxilla than the mandible) and gingival recession. A comprehensive approach was recommended; this would include gingival grafting and four bicuspid extractions, with orthodontic retraction of the anterior dentition into the solid alveolar bone. This would be followed by jaw reconstruction, finishing orthodontics, and periodontal surveillance. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment. C, Panorex radiograph before retreatment.
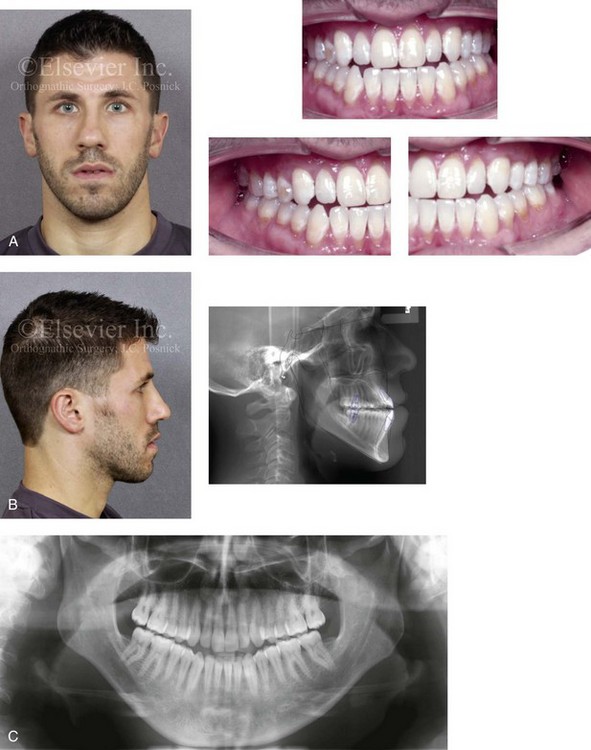
Figure 20-4 A 29-year-old man arrived for the evaluation of a longstanding developmental jaw deformity characterized by maxillary deficiency with relative mandibular excess. There is malocclusion and chronic obstructive nasal breathing. By the time he was 13 years old, he was referred by his pediatric dentist to an orthodontist for the evaluation of a Class III negative overjet malocclusion. He then underwent a 2-year course of compensatory orthodontics in an attempt to neutralize the occlusion. He was left with an Angle Class III negative overjet and early signs of gingival recession. The patient also has a history of stress-induced asthma and chronic obstructed nasal breathing. He uses Flonase, Singulair, and other medications in an effort to open the nasal airway, and he is also being seen by an allergist. For his gingival recession, he was referred to a periodontist, and connective tissue grafting was carried out for the lower anterior dentition on several of the maxillary posterior teeth. An orthodontic consultation confirmed crowding, the proclination of the maxillary anterior dentition, and uprighted mandibular anterior teeth. Evaluation of the upper airway documented a deviated septum and hypertrophic inferior turbinates. An orthodontic and surgical approach was recommended to limit further secondary dental trauma, to stabilize the periodontium, and to correct the occlusion. A, Frontal facial and occlusal views before retreatment. B, Profile facial and lateral cephalometric radiographs before retreatment. C, Panorex radiograph before re-treatment.
• Moderate or severe Class III patterns (i.e., >4 mm of reverse overjet)
• Moderate to severe vertical skeletal discrepancies
• Significant dental crowding in the lower jaw and significant anterior dental protrusion in the upper jaw
• A concern that the planned orthodontic mechanics may cause periodontal deterioration
Definitive Reconstruction
Timing of Orthognathic Surgery
Skeletally immature individuals with true mandibular excess can be expected to outgrow any early orthodontic or surgical corrections and later require further treatment.7,17,83,90 Indirect methods of assessing growth maturity (e.g., a hand–wrist film to determine bone age) are not accurate enough to be used in isolation for planning the timing of surgery. A reasonable method to assess growth maturation is through the analysis of serial lateral cephalometric radiographs. These radiographs can be used in two ways: for a cervical vertebral analysis or to make sequential direct mandibular measurements. Surgery is delayed until the deceleration of growth can be documented. The use of a quantitative condylar head bone scan can also be helpful to evaluate the growth of the mandible in the adolescent, but both false-positives and false-negatives may occur. If the Class III condition is largely the result of maxillary deficiency, gauging the preferred timing of surgery is more straightforward, because the late postsurgical growth of the mandible is less likely (see Chapter 17).
Alexander and colleagues completed a study of craniofacial growth changes in Caucasians with untreated Class III malocclusions by using longitudinal cephalometric records (n = 103).1 In girls, the mandibular growth spurt generally occurred between the ages of 10 and 12 years. In boys, the growth spurt was usually between the ages of 12 and 15 years. In some of the Class III subjects, limited degrees of mandibular growth relative to that of maxillary growth were documented to continue after the adolescent spurt. After the age of 13 years in girls and 15 years in boys and until closer to the age of 17 years, annual increments of mandibular growth were often between 1.5 mm and 2.0 mm, whereas increments of midface length dropped to less than 1 mm. The authors concluded that the differential growth behavior of the two jaws among individuals with Class III conditions may result in recurrent jaw disharmony and malocclusion when orthodontic or surgical treatment is undertaken before or during puberty.
Pre-Orthodontic Periodontal Checklist (see Chapter 6)
• Assess for active gingivitis or periodontitis and the need for treatment.
• Assess the current level of oral hygiene and the need for a home care program.
• Assess for the effects of occlusal trauma and malocclusion on the periodontium.
• Assess the level of attached gingiva and the need for augmentation.
• Confirm the adequacy of the alveolar bone and the need to create space with the use of extractions.
• Assess the need for restorations to remove decay, to replace deficient enamel, and to achieve a healthy gingival interface.
Orthodontic Preparation for Orthognathic Surgery
1. Before orthodontic decompensation, assess the level of attached gingiva, the position of the labial and lingual plates, and the alveolar crest heights. Consider the effects of any planned orthodontic maneuvers on the periodontium.
2. Make decisions about the tooth (root) size to alveolar volume discrepancies in each arch and the need for extractions to establish and preserve periodontal health.
3. Create a plan (i.e., separate surgical and orthodontic objectives) to achieve preferred anteroposterior and vertical incisor positions in the maxilla and the mandible.
4. Understand how the orthodontic objectives become more limited when they are combined with the planned surgical procedures (e.g., maxillary segmentation, bimaxillary osteotomies) to then achieve the final desired arch form, midline positioning, occlusion, and facial symmetry and proportions.
5. Make decisions about orthodontic mechanics and anchorage requirements to achieve the chosen objectives.
6. At the end of the presurgical orthodontic phase (i.e., 4 to 6 weeks before surgery), full-dimensional stabilizing (i.e., passive) arch wires should be in place. The placement of surgical hooks can be done just before surgery.
Leveling the Mandibular Arch
When an accentuated curve of Spee is present in the lower arch of a patient with Class III malocclusion, it is managed through a combination of intrusion of the incisors and extrusion of the premolars or molars.20,49 In preparation for surgery, repositioning the lower incisors forward is generally advantageous for the Class III skeletal pattern. Therefore, lower arch extractions are rarely indicated. If limited labial bone is present, a periodontal evaluation is recommended before the incisors are orthodontically moved forward. If gingival recession has occurred or if the gingiva is genetically inadequate, augmentation grafting procedures are indicated (see Chapter 6).
Leveling of the Maxillary Arch
If the upper arch is narrow, then orthodontic leveling is performed in segments in anticipation of surgical management.8,14,16,22,71,88,95,114 If the curve of Spee is excessive as a result of vertical skeletal dysplasia, then leveling is also done in segments in preparation for surgical correction (see Chapter 17).
In the presence of maxillary deficiency, limited space to uncrowd the upper teeth may leave the roots tipped outside of the solid alveolar housing. In this circumstance, maxillary first bicuspid extractions with space closure before surgery is preferred. With only borderline crowding, extractions are often not carried out. Limited dental space deficiency can often be managed through the judicious use of interproximal reduction. In addition, the aesthetic consequences of mildly proclined incisors (i.e., A-point to B-point discrepancy in profile) can be improved via the clockwise rotation of the maxillomandibular complex at the time of surgery (see Chapters 12 and 13).
Immediate Presurgical Planning
The immediate presurgical planning takes into account collaborative clinical efforts between the orthodontist, the surgeon, the patient, and the patient’s family that will have been ongoing since the initial consultation visits.32,74,75,84,93,98 Depending on the condition of the dentition and the supporting structures, the restorative dentist and the periodontist may also have been intricately involved.
First, broad-stroke clinical decisions are made involving the preferred vector changes for each jaw; only then are the precise millimeter distances and angular changes required for each jaw to achieve the desired results determined (see Chapter 12). Analytic model planning is carried out on the articulated dental casts with use of the Erickson Model Table. Splints are constructed to assist with the achievement of the precise occlusion and the preferred facial aesthetics in the operating room (see Chapter 13).
During surgical planning, consideration should be given to the following eight aspects (see Chapter 12):
1. Assess the degree of horizontal advancement required in the midface as measured at the maxillary incisal edge.
2. Assess the degree of vertical change required in the midface as measured at the maxillary incisal edge.
3. Assess the potential advantages of clockwise rotation of the maxillary plane to achieve preferred A-point to B-point positioning (i.e., pitch orientation).
4. Clarify any maxillary midline to facial midline discrepancies and their planned correction (i.e. yaw orientation).
5. Identify any canting (i.e., roll orientation) of the maxilla and its planned correction.
If more than 4 degrees of cant are present, this will be noticeable to even the untrained eye at conversational distance (see Chapter 12).
6. Identify the advantages of segmentation of the upper jaw to achieve the preferred maxillary arch form and occlusion.
7. Assess the baseline chin morphology.
8. Assess the baseline pyriform rim, floor of nose, and anterior nasal spine morphology.
Basic Surgical Approach
Regardless of the cause of the Class III skeletal pattern, the common aesthetic impression in profile is of a flat or concave midface with a long and forward-projecting chin.89 The classic dentofacial deformity of maxillary deficiency with relative mandibular excess will require at a minimum a Le Fort I osteotomy with horizontal advancement.30,31,38,62,85,86,112 The need for additional vector changes in the maxilla should always be considered (e.g., transverse widening, vertical adjustment, maxillary midline to facial midline correction, cant correction, clockwise maxillary plane rotation).121
The Le Fort I osteotomy (often performed in segments) with three-dimensional repositioning is generally combined with sagittal split ramus osteotomies to place the distal mandible into ideal occlusion at the new maxillary location.9–12,50–52,63–66,70,87,94,110,113 In most cases, the full overjet deficiency is corrected in the maxilla. Clockwise rotation of the maxilla and the mandible will generally leave the mandibular incisor unchanged in the sagittal (i.e., horizontal) plane. However, the pogonion will have moved posteriorly.
An osteotomy of the chin with horizontal or vertical change is also frequently desirable.36 If chronic nasal obstruction is present, then procedures to improve the airway in accordance with the physical examination (i.e., septoplasty, inferior turbinate reduction) may be simultaneously accomplished (Figs. 20-5 through Fig. 20-20).73,75
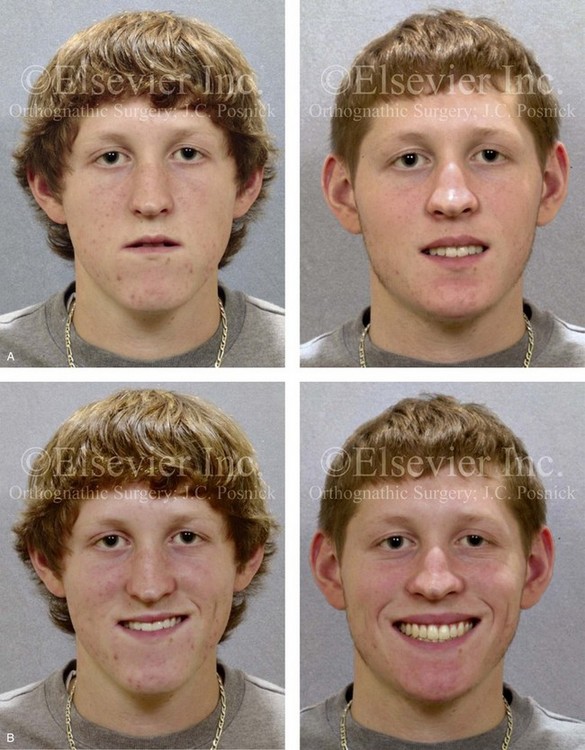
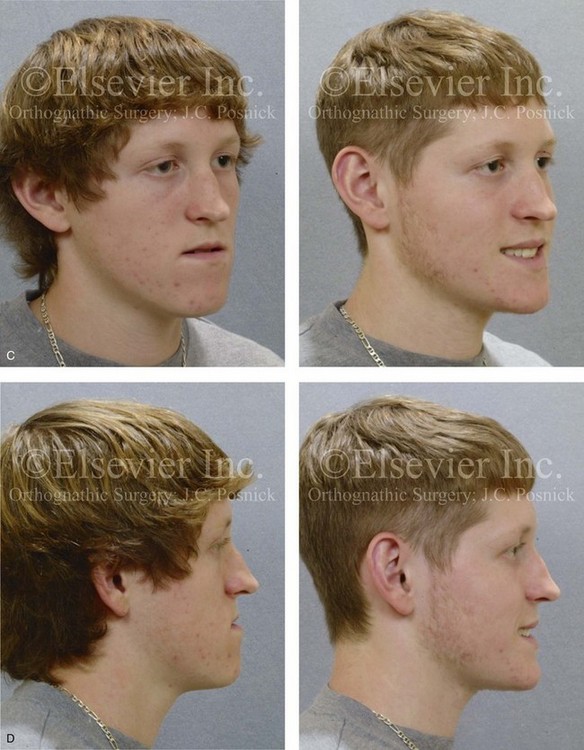

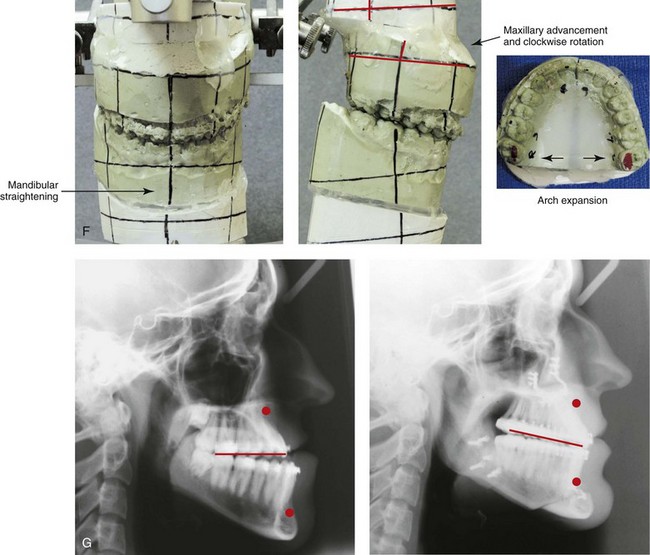
Figure 20-5 A 17-year-old high school student was referred by his orthodontist for surgical evaluation. A non-extraction orthodontic approach had previously been carried out, without success. The Class III negative overjet anterior open-bite malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings (i.e. septal deviation and inferior turbinate hypertrophy), intranasal procedures were also planned. When orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (limited corrections); osseous genioplasty (vertical reduction and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and then after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
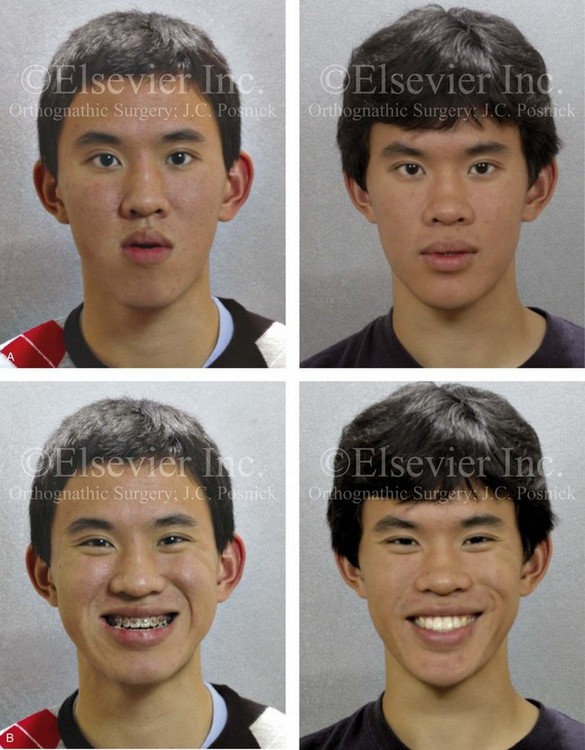

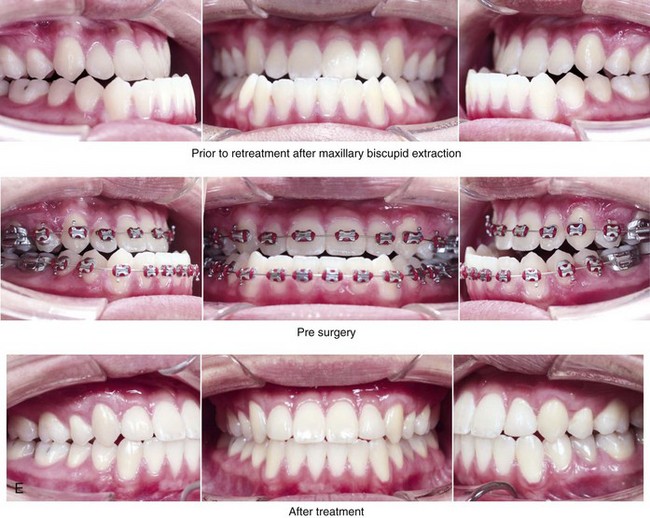
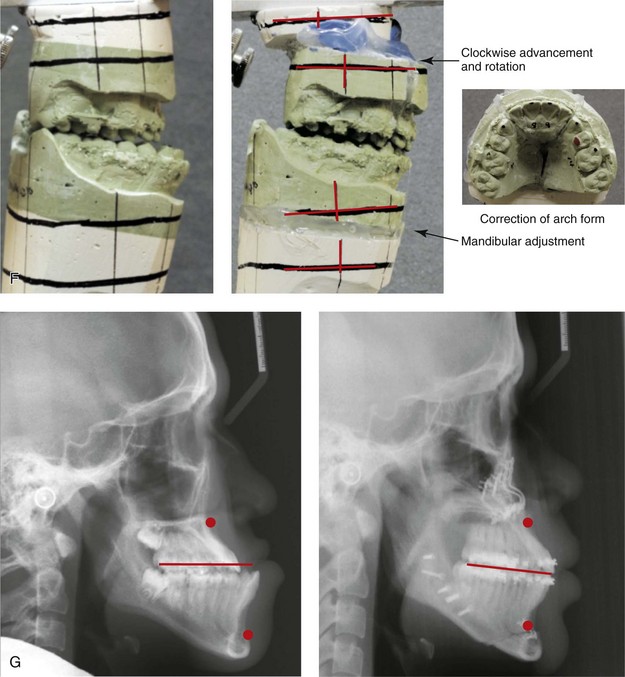
Figure 20-6 A 17-year-old high school student was referred by his orthodontist for surgical evaluation. The patient’s Class III negative overjet anterior open-bite malocclusion required redo orthodontics, including maxillary bicuspid extractions and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also required. When orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, clockwise rotation, horizontal advancement, and vertical lengthening); sagittal split ramus osteotomies (limited corrections); osseous genioplasty (vertical reduction and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and then after the completion of treatment. The patient required gingival grafting on the labial aspect of the right maxillary canine. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
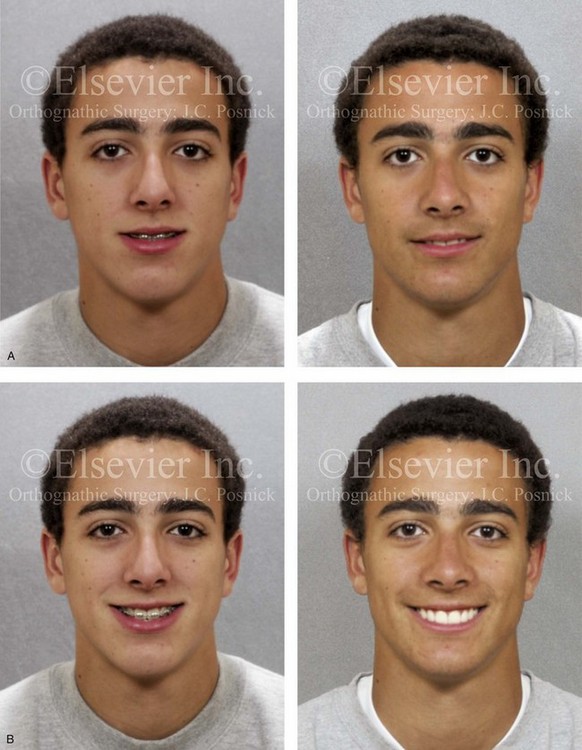
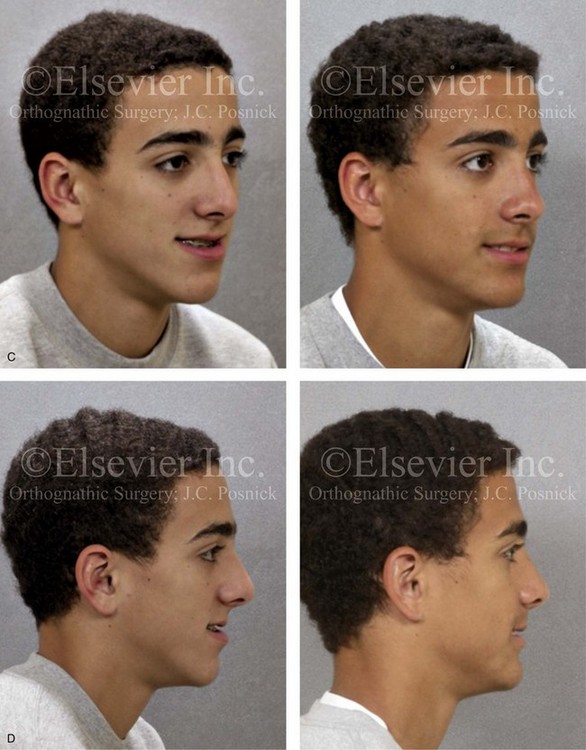
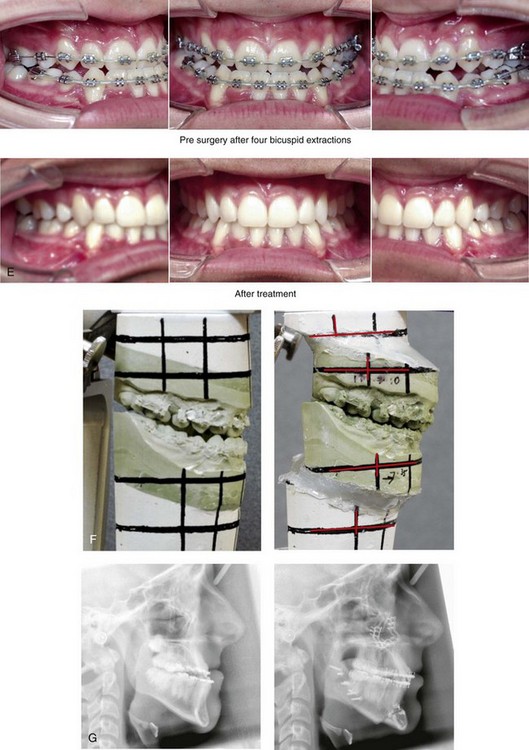
Figure 20-7 A 16-year-old high school student was referred by his orthodontist for surgical evaluation. He had previously undergone orthodontics, including four bicuspid extractions. The residual Class III negative overjet malocclusion required further orthodontics in combination with jaw reconstruction. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also required. When the orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement); sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views with redo orthodontics in progress and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment. Note the gingival recession on the labial aspect of the mandibular canines as a result of the orthodontic mechanics.
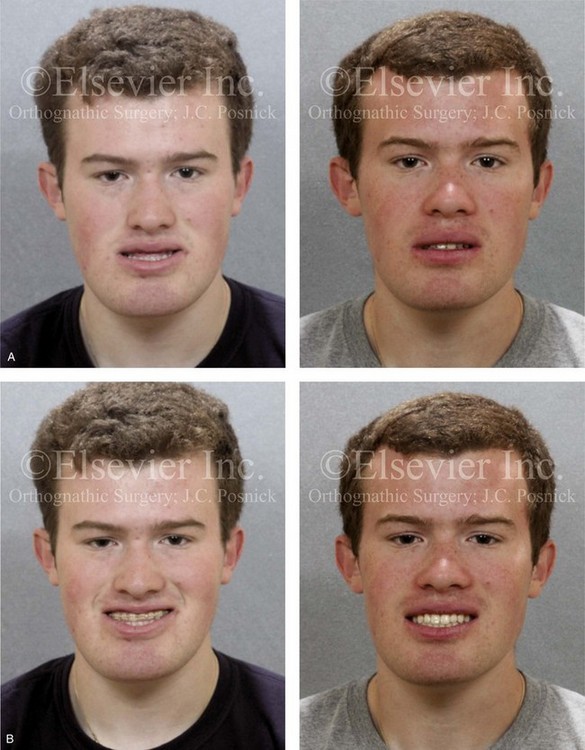

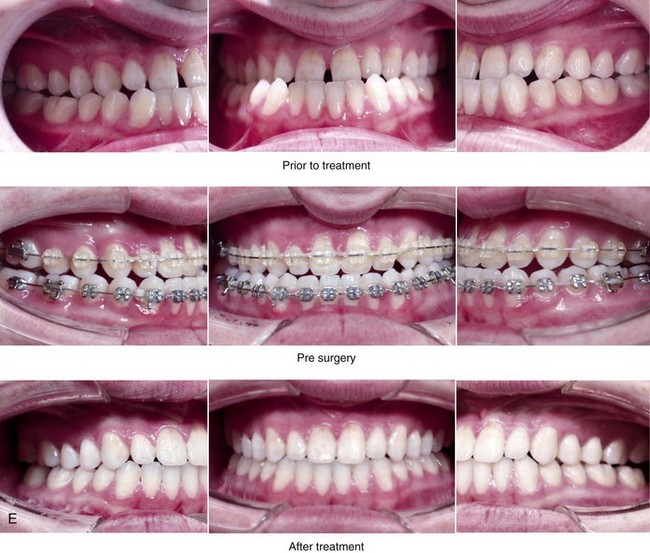
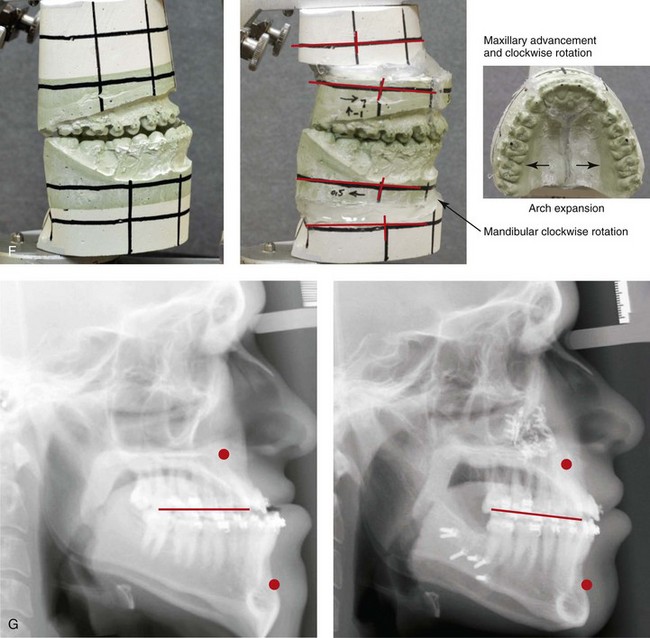
Figure 20-8 A 20-year-old college student was referred by his orthodontist for surgical evaluation. His Class III negative overjet anterior open-bite malocclusion required jaw surgery. Orthodontic decompensation was carried out without maxillary extractions, which left the incisors moderately procumbent. The patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation) and sagittal split ramus osteotomies (clockwise rotation). Note the aesthetic advantage of the maxillomandibular clockwise rotation as part of the correction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before treatment, with orthodontics in progress, and then after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
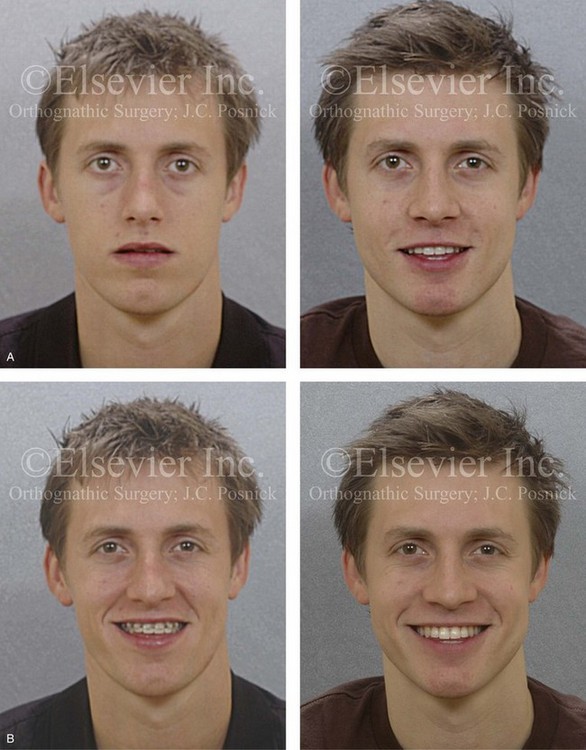

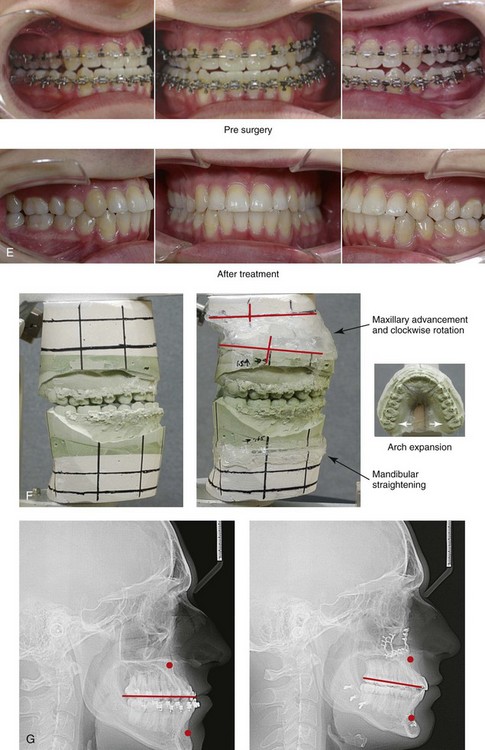
Figure 20-9 A 22-year-old man was referred by his orthodontist for surgical evaluation. A non-extraction orthodontic approach had previously been carried out, without success. The patient’s Class III negative overjet anterior open-bite malocclusion required redo orthodontics and jaw surgery. Because he had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also needed. When preoperative orthodontics were complete, the patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (limited corrections); osseous genioplasty (minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillary clockwise rotation in the presence of baseline incisor procumbancy. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views with orthodontics in progress and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
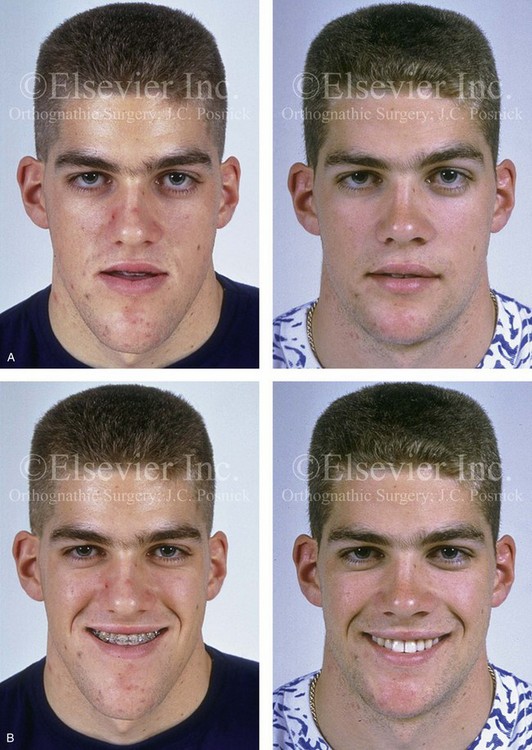
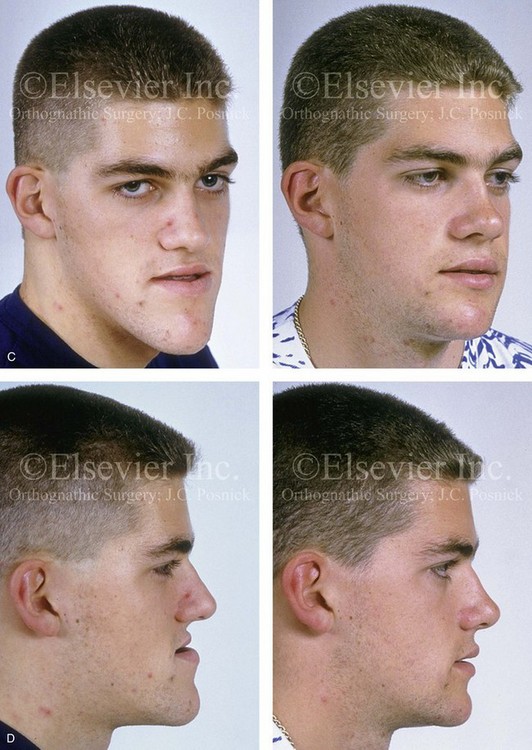
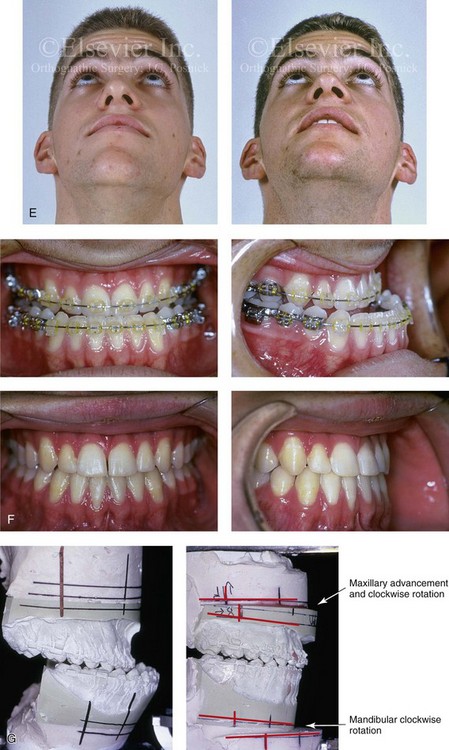
Figure 20-10 A 17-year-old high school student was referred by his orthodontist, who requested surgical evaluation for a Le Fort III advancement. The Class III negative overjet malocclusion with maxillary deficiency gave the impression of flat cheekbones and infraorbital rims. Evaluation confirmed that the patient’s deformity was limited to the maxilla and the mandible. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also required. When preparatory orthodontics were complete, the patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (set-back and clockwise rotation); osseous genioplasty (vertical reduction); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillomandibular clockwise rotation in the presence of baseline incisor procumbancy. This rotation projects the pyriform rims forward and sets back the pogonion. The orthodontic over-retraction of the lower incisors resulted in labial bone loss and gingival recession. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Worm’s-eye views before and after reconstruction. F, Occlusal views with orthodontics in progress and after the completion of treatment. Note the mild gingival recession on the labial aspect of the mandibular anterior teeth as a result of orthodontic mechanics. G, Articulated dental casts that indicate analytic model planning.
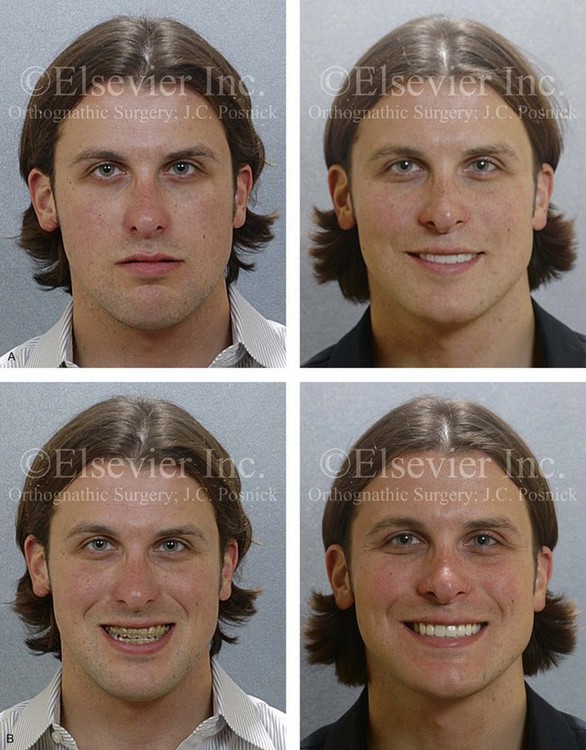
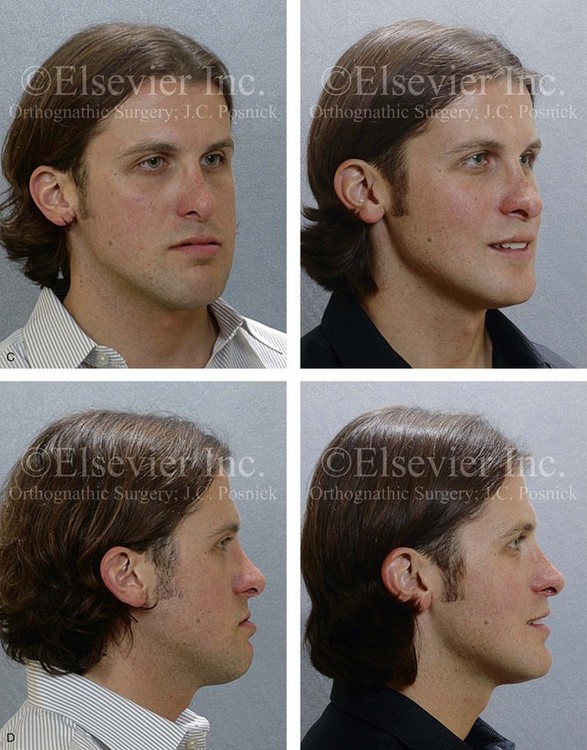

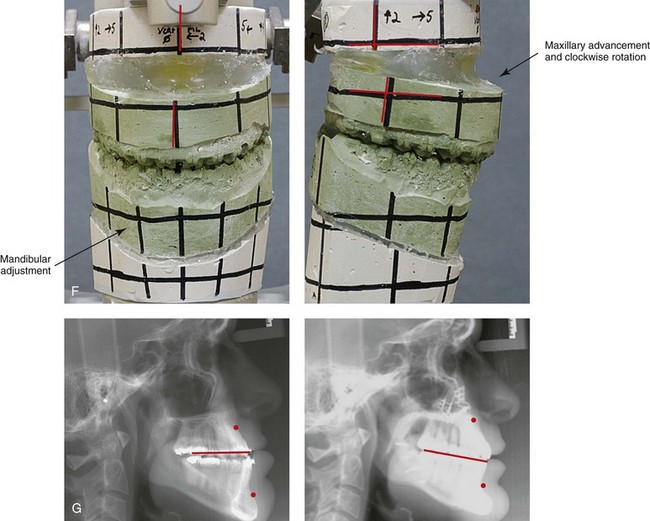
Figure 20-11 A 25-year-old man was referred for surgical evaluation. A non-extraction orthodontic camouflage approach had previously been carried out, without success. He previously underwent a cosmetic rhinoplasty in an attempt to reduce the size of the nose. The Class III negative overjet malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also required. When the presurgical orthodontics were complete, the patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (clockwise rotation); osseous genioplasty (vertical reduction and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillomandibular clockwise rotation in the presence of baseline incisor procumbancy. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. Note the gingival recession on the labial aspect of the mandibular and maxillary anterior dentition as a result of the dental roots being crowded into limited available alveolar bone. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
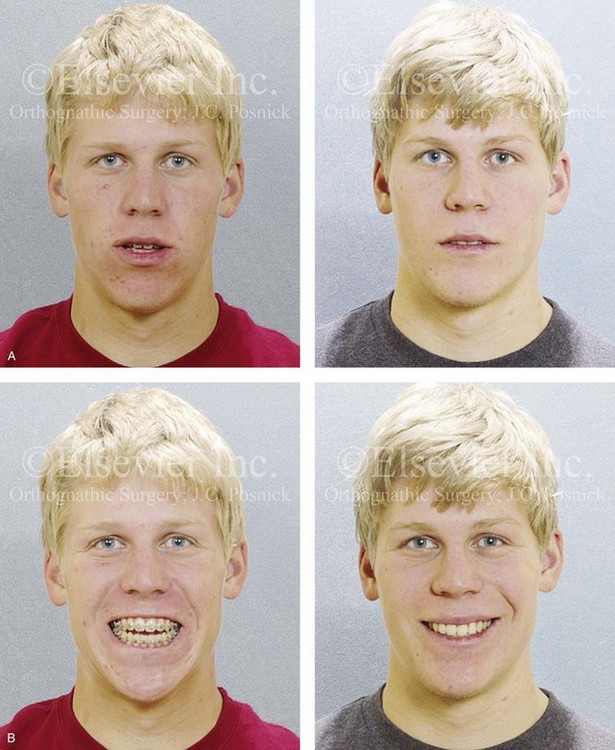
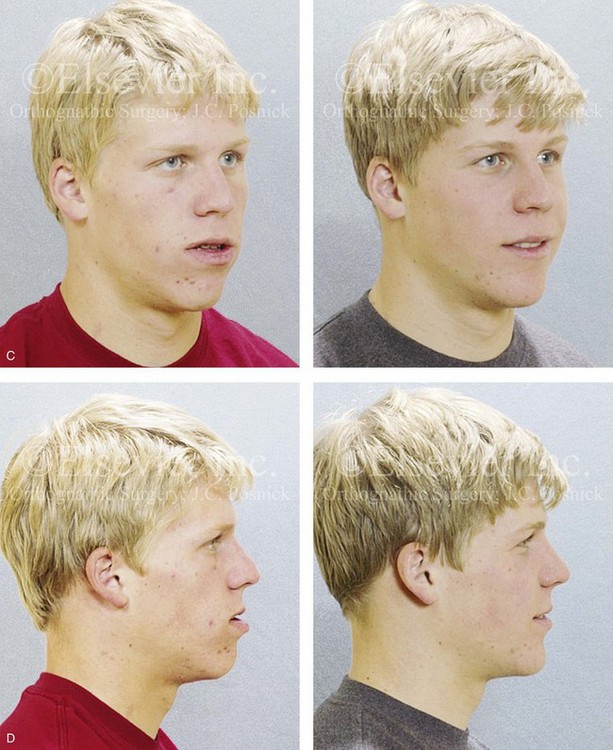
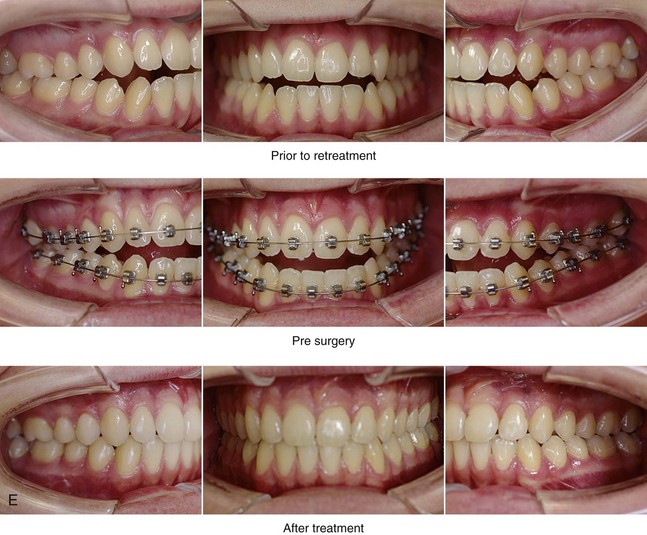
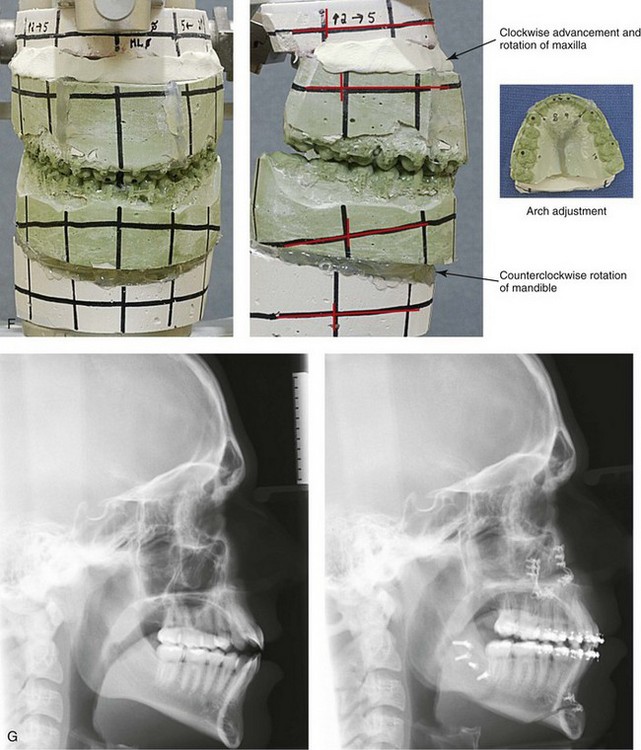
Figure 20-12 An 18-year-old high school student was referred by his orthodontist for surgical evaluation. A non-extraction orthodontic approach had previously been carried out, without success. The Class III negative overjet anterior open-bite malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. When orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, correction of curve of Spee, horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (counterclockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillary clockwise rotation and the mandibular counterclockwise rotation. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.


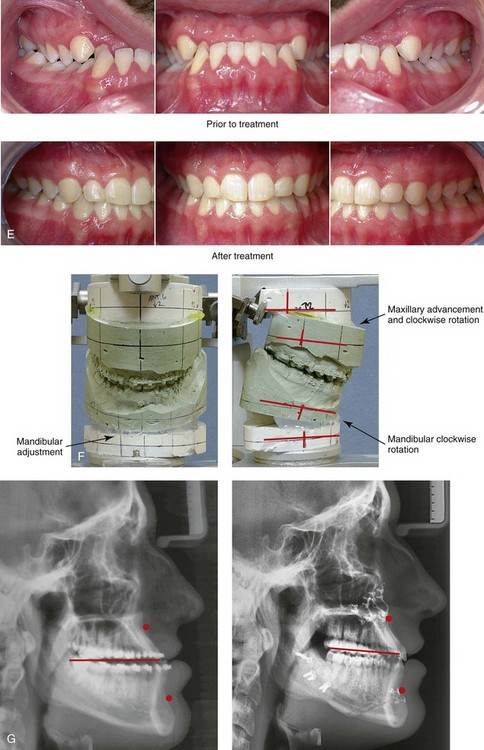
Figure 20-13 A 20-year-old college student was referred for surgical evaluation. The Class III negative overjet deep-bite malocclusion required orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. Orthodontics was carried out without extraction. A degree of maxillary incisor procumbency remained. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (clockwise rotation); osseous genioplasty (vertical reduction and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillomandibular clockwise rotation in the presence of baseline incisor procumbancy. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
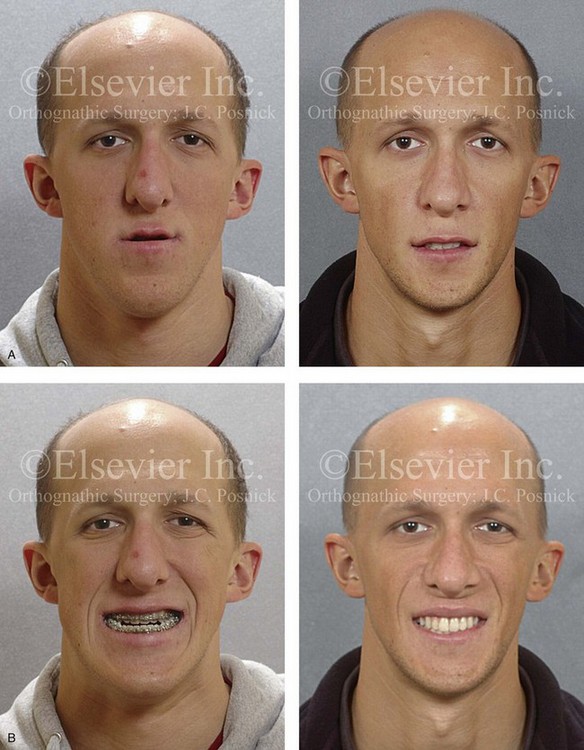
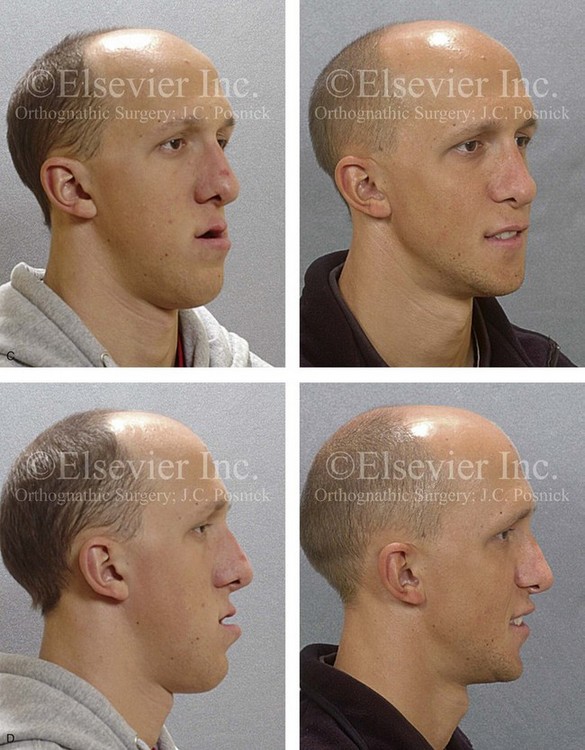
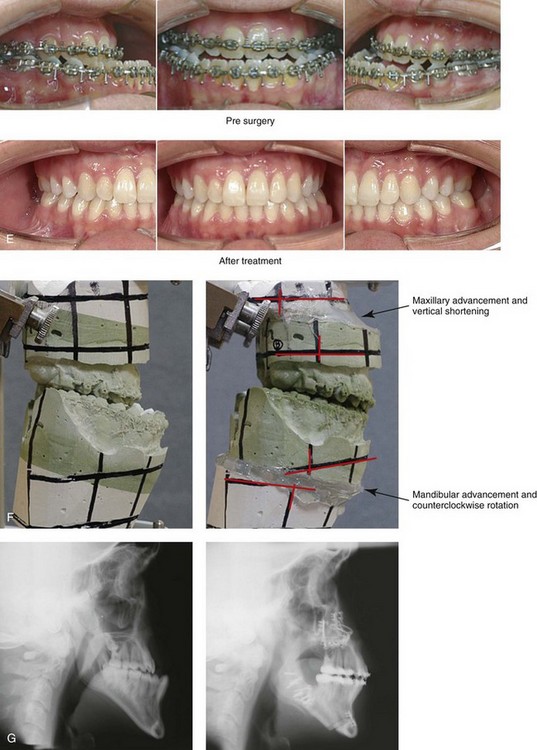
Figure 20-14 A 19-year-old college freshman was referred for evaluation. He had a maxillary deficiency with a relative mandibular excess growth pattern and a Class III negative overjet anterior open-bite malocclusion. During the mixed dentition, the patient was treated with growth-modification techniques and rapid palatal expansion. When he was 18 years old, orthodontic mechanics were reinitiated; in preparation for jaw reconstruction. The maxillary and mandibular second molars were poorly developed and required removal. The patient had a lifelong history of nasal obstruction; physical examination confirmed a deviated septum, enlarged inferior turbinates, and a constricted nasal aperture. When orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy (+12 mm horizontal advancement, +2 mm vertical lengthening, 2.5 mm midline correction) and interpositional iliac bone graft; sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening); and septoplasty, inferior turbinate reduction, and pyriform rim recontouring. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views with orthodontics in progress and then 4 years after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



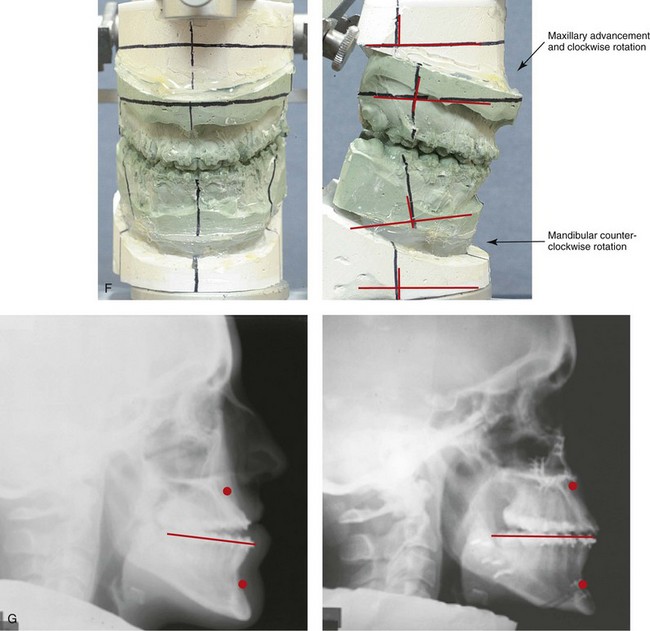
Figure 20-15 A 27-year-old woman was referred by her orthodontist for surgical evaluation. A non-extraction orthodontic approach had been carried out during her high school years, without success. Her Class III negative overjet anterior open-bite malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. After the orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (counterclockwise rotation); osseous genioplasty (vertical reduction); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the mandibular counterclockwise rotation. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



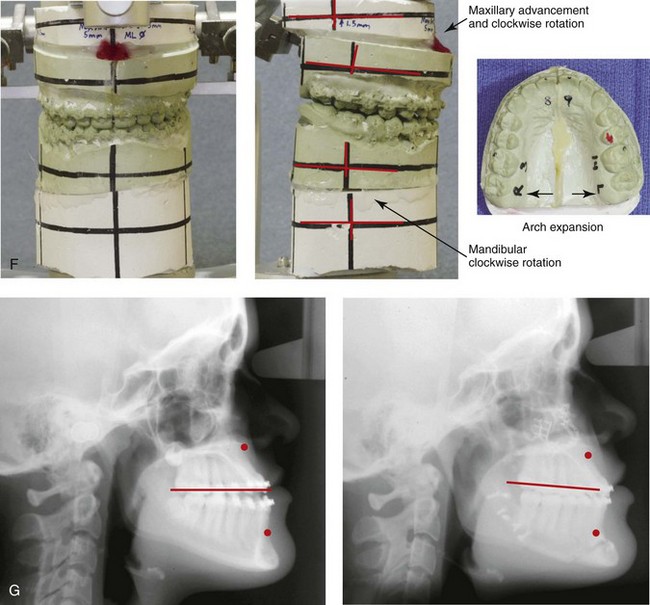
Figure 20-16 A 16-year-old high school student was referred by her orthodontist for surgical evaluation. A non-extraction orthodontic approach had previously been carried out, without success. The Class III negative overjet anterior open-bite malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. Presurgical orthodontics were carried out without extractions, and the maxillary anterior procumbancy remained. The patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (minimal clockwise rotation); osseous genioplasty (vertical reduction and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillary plane clockwise rotation in the presence of baseline incisor procumbency. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
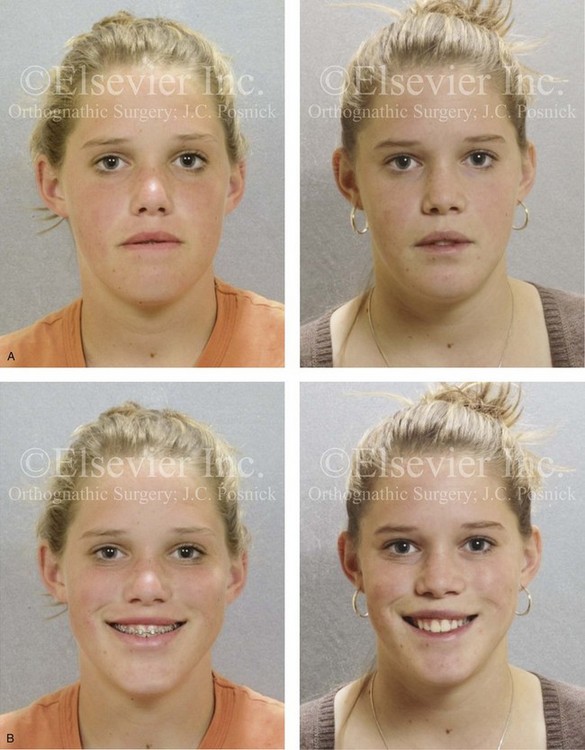


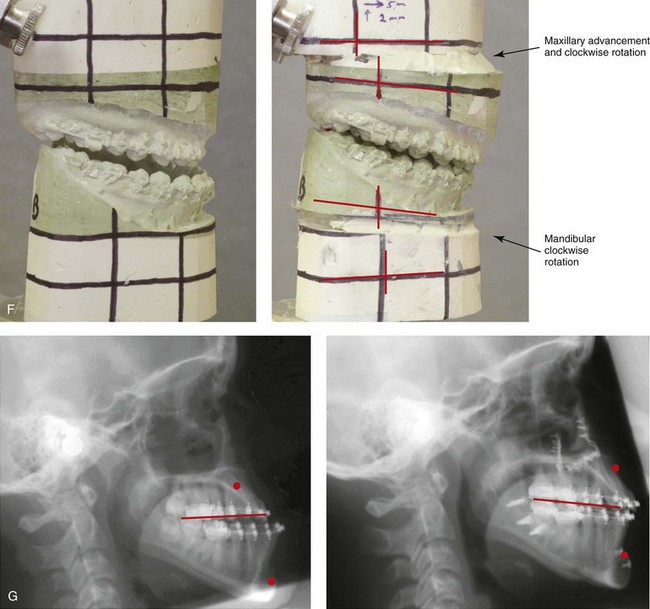
Figure 20-17 A 15-year-old high school student was referred by her orthodontist for surgical evaluation. A non-extraction orthodontic approach had previously been carried out, without success. The Class III negative overjet malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. Presurgical orthodontics were carried out without extractions, and the maxillary incisor procumbency remained. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (clockwise rotation); osseous genioplasty (vertical reduction and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillomandibular clockwise rotation in the presence of baseline incisor procumbency. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
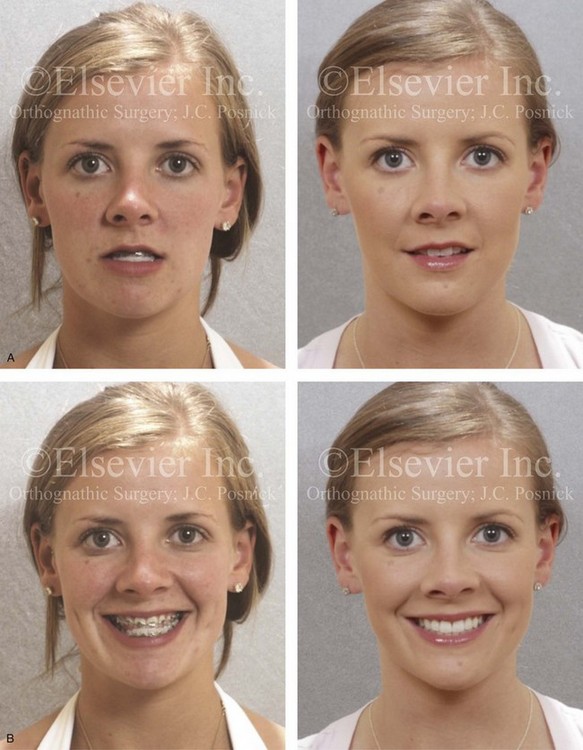

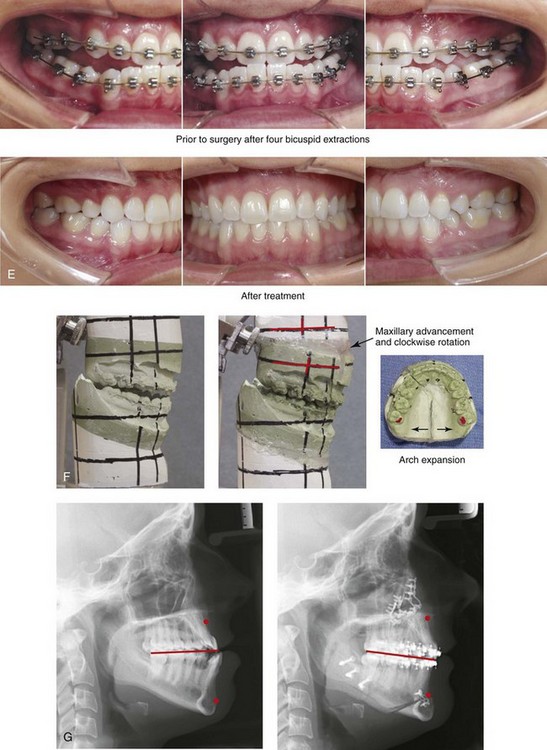
Figure 20-18 A 21-year-old woman was referred for surgical evaluation. An orthodontic approach that involved four bicuspid extractions to neutralize the occlusion had previously been carried out, without success. The Class III negative overjet malocclusion required redo orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. When the orthodontic decompensation was complete, the patient’s surgery included maxillary Le Fort I osteotomy in segments (arch expansion, horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (minimal corrections); osseous genioplasty (minimal horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views with orthodontics in progress and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



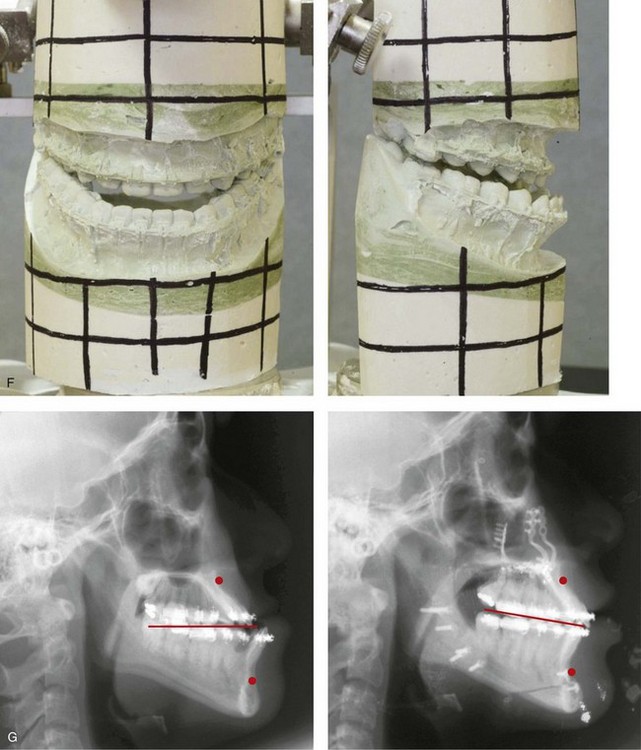
Figure 20-19 A 16-year-old high school student was referred by her orthodontist for surgical evaluation. Her Class III negative overjet malocclusion required orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. Presurgical orthodontics were completed without extractions, and the maxillary dental root crowding in the alveolar bone and the incisor procumbency remained. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical lengthening, and clockwise rotation); sagittal split ramus osteotomies (clockwise rotation); osseous genioplasty (minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillomandibular clockwise rotation. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before treatment, with orthodontics in progress, and after the completion of treatment. Note that the maxillary dental roots are crowded in the alveolus, which resulted in labial gingival recession. F, Articulated dental casts before analytic model planning. G, Lateral cephalometric radiographs before and after treatment.



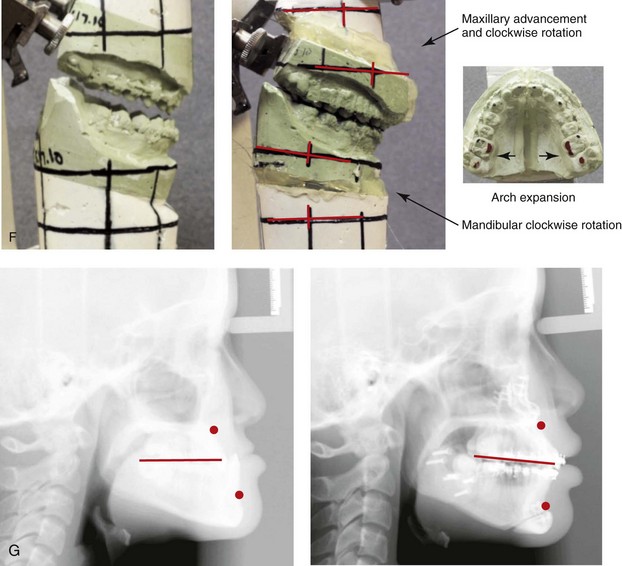
Figure 20-20 A 16-year-old high school student was referred by her orthodontist for surgical evaluation. The Class III negative overjet malocclusion required orthodontics and jaw surgery. Because the patient had a lifelong history of nasal obstruction and consistent physical findings, intranasal procedures were also beneficial. Presurgical orthodontics was completed without extractions, and the maxillary incisor procumbency remained but without dental root crowding in the alveolar process. The patient’s surgery included maxillary Le Fort I osteotomy in segments (horizontal advancement, vertical lengthening, arch expansion, and clockwise rotation); sagittal split ramus osteotomies (clockwise rotation); osseous genioplasty (minimal horizontal advancement); and septoplasty and inferior turbinate reduction. Note the aesthetic advantage of the maxillomandibular clockwise rotation in the presence of baseline excess incisor inclination. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and after the completion of treatment. F, Articulated dental casts before analytic model planning. G, Lateral cephalometric radiographs before and after treatment.
In general, well thought out maxillary surgical maneuvers (i.e., horizontal advancement, clockwise rotation) will also correct the presenting negative vector relationship between the ocular globe and the lower eyelid. In doing so, the overlying cheek and periorbital soft tissues are immediately enhanced. This also limits the unattractive eyelid and midface aging effects that would otherwise occur (i.e., soft-tissue descent, rounding of the palpebral fissure, lengthening of the lower lid, loss of cheek region soft-tissue prominence; see Chapter 25).
When limiting the surgery to one jaw (either through mandibular set-back or Le Fort I advancement), the immediate correction of the occlusion may be possible, but a suboptimal outcome is likely. A one-jaw approach is rarely preferred from the overall perspective of facial aesthetics, occlusal stability, and upper airway management. A Le Fort I osteotomy in combination with mandibular ramus osteotomies that incorporates clockwise rotation of the maxillomandibular complex is generally needed to achieve midface fullness, to improve the projection of the nasal tip and, to enhance the upper lip to tooth aesthetics (see Figs. 20-5 through 20-20).
Demetriades and colleagues confirmed the clinical importance of considering the airway when formulating a treatment plan for the correction of a skeletal Class III pattern.26 They reported on 26 patients who presented with developmental dentofacial deformities that were characterized by maxillary deficiency in combination with relative mandibular excess. The patients were divided into two groups. All patients underwent mandibular ramus osteotomies with a degree of set-back. The Group 1 study patients (n = 13) underwent mandibular set-back of 5 mm or more without simultaneous Le Fort I osteotomy. The Group 2 study patients (n = 13) underwent limited mandibular set-back, but their procedures were performed in combination with Le Fort I advancement. All study patients underwent preoperative and postoperative lateral cephalometric radiographs at standard intervals. Any changes that occurred in the position of the hyoid bone, the distance of the palate to the posterior nasal spine, the retrolingual space, and the hypopharyngeal space were measured from the postoperative radiographs. Preoperative and postoperative portable polysomnography were also carried out. The study confirmed that mandibular retropositioning of 5 mm or more can significantly decrease the posterior airway space and cause mild to moderate obstructive sleep apnea. The study also suggested that, when a limited mandibular set-back is carried out in combination with maxillary Le Fort I advancement, significant negative effects on the posterior airway space are likely prevented.
Postsurgical Orthodontic Maintenance and Detailing
The surgeon’s effective management of the patient’s in-hospital and at-home convalescence during the initial healing period (i.e., 5 weeks) is essential for a successful outcome (see Chapter 11). Cephalometric and Panorex radiographs and facial and occlusal photographs are obtained at standard postoperative intervals to document progress. We prefer to take these records at the 5-week postoperative interval as a matter of routine.
Complications, Informed Consent, and Patient Education
Complications and patient dissatisfaction will always occur in a small percentage of individuals.4,23,44,46,47,53,54,120 The clinician’s ability to communicate the potential risks and complications, the alternative approaches available, and the benefits of the recommended treatment plan to the patient and the family is essential to achieve a favorable result. When the patient, the family, and all treating clinicians are fully informed, shared responsibility for the treatment outcome is more likely (see Chapter 16).
Malocclusion after Orthodontics and Orthognathic Surgery
There are inherent biologic challenges to the orthodontic movement of the teeth in the alveolar process and to the surgical repositioning of the jaws or jaw segments in the individual with maxillary deficiency and relative mandibular excess. These include the technical aspects of the repositioning, the initial healing requirements, and the difficulties associated with the long-term maintenance of the mechanically relocated teeth, jaws, and jaw segments. When following sound biomechanical and aesthetic principles, clinicians carry out orthodontic treatment and surgical procedures and then effectively maintain the results, in most cases. Potential intraoperative technical difficulties associated with sagittal split ramus osteotomies of the mandible and maxillary Le Fort I osteotomies can result in an immediate (i.e., early) malocclusion; however, these difficulties are generally preventable (see Chapter 17).*
Timing the surgery to limit ongoing mandibular growth afterward is usually possible, but it is more problematic for the skeletal Class III patient than the Class II patient (see Chapter 17). Significant condylar resorption after orthognathic surgery is rarely seen in the skeletal Class III patient (see Chapter 36).
Proffit and colleagues make a compelling argument that for the Class III patient, when the orthognathic procedure is a mandibular set-back only versus two-jaw surgery then relapse at the ramus osteotomy site is a common occurrence.79,80 Research confirms better long-term skeletal and occlusal stability when two-jaw surgery (i.e., maxillary advancement with limited mandibular setback) is performed for the management of most Class III skeletal patterns.81
Temporomandibular Disorders: The Effects of Orthodontics and Orthognathic Surgery
It is estimated that an average of 32% of the population reports at least one symptom of TMD, whereas an average of 55% demonstrate at least one clinical sign. TMD includes various signs and symptoms of the temporomandibular joint, the masticatory muscles, and related structures. The signs and symptoms may include a spectrum of referred head and neck pain; joint noise (e.g., popping, clicking, crepitus); reduced or altered mandibular movements as a result of muscle spasm or disc displacement, with or without reduction; condylar head erosion, and pain on direct palpation of either of the temporomandibular joints or the masticatory muscles.3,5
Occlusal factors (i.e., degrees of malocclusion) are often claimed to be associated with TMD. Interestingly, the correction of a skeletal Class III jaw deformity through orthodontics and orthognathic surgery often relieves the signs and symptoms of TMD, but this is not predictable for each individual patient (see Chapter 9).
Suboptimal Facial Aesthetics after Orthognathic Surgery
An accurate pretreatment facial analysis should limit the incidence of suboptimal aesthetics after surgery. Many of the aesthetic treatment planning pitfalls for the correction of skeletal Class III patterns were reviewed earlier in this chapter. Clearly stated and realistic objectives that are discussed and agreed upon by all parties are essential. Comprehensive and meticulous treatment planning, accurate surgical execution, and good patient cooperation further ensure a favorable result. Despite the following of these steps, patient and family dissatisfaction are to be expected in a small percentage of cases.40,41,56,68,103,115 Maintaining open lines of communication, reasonable patient and family flexibility, and clinician responsiveness to ongoing needs and concerns will generally result in the satisfactory resolution of these issues (see Chapter 7).
References
1. Alexander, AEZ, McNamara, JA, Jr., Franchi, L, Baccetti, T. Semilongitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion. Am J Orthod Dentofacial Orthop. 2009; 135:700. e1–700. e14.
2. Angle, EH. Treatment of malocclusion of the teeth: Angle’s system, ed 7. Philadelphia: SS White; 1907.
3. Athanasiou, AE. Number and intensity of occlusal contacts following surgical correction of mandibular prognathism. J Oral Rehabil. 1992; 19:145.
4. Athanasiou, AE. Morphologic and functional implications of the surgical-orthodontic management of mandibular prognathism: A comprehensive review. Am J Orthod Dentofacial Orthop. 1993; 103:439.
5. Athanasiou, AE, Mavreas, D. Tomographic assessment of alterations of the temporomandibular joint after surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1991; 6:105.
6. Baccetti, T, McGill, JS, Franchi, L, et al. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998; 113:333–343.
7. Baccetti, T, Reyes, BC, McNamara, JA, Jr. Craniofacial changes in Class III malocclusion as related to skeletal and dental maturation. Am J Orthod Dentofacial Orthop. 2007; 132:171. e1–171. e12.
8. Bailey, LJ, White, RP, Proffit, WR, et al. Segmental Le Fort I osteotomy for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:728.
9. Becker, R. Results in the treatment of prognathism and open bite with simultaneous tongue reduction. Dtsch Zahnarztl Z. 1960; 17:892.
10. Bell, WH. Le Fort I osteotomy for correction of maxillary deformities. Oral Surg. 1975; 33:412–426.
11. Bell, WH, Creekmore, DC. Surgical orthodontic correction of mandibular prognathism. Am J Orthod. 1973; 63:256.
12. Bell, WH, Jacobs, JD. Surgical orthodontic correction of horizontal maxillary deficiency. J Oral Surg. 1979; 37:897.
13. Bell, WH, White, RP, Hall, HP, et al. Mandibular excess. In: Bell WH, Proffit WP, White R, eds. Surgical correction of dentofacial deformities. Philadelphia: WB Saunders; 1980:234–441.
14. Betts, NJ, Vanarsdale, RL, Barber, HD, et al. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995; 10:75.
15. Blair, VP. Surgery of the mouth and jaws. St Louis: Mosby; 1914.
16. Bloomquist, DS. The stability of segmentalized Le Fort I osteotomies with miniplate fixation in patients with maxillary hypoplasia [discussion]. J Oral Maxillofac Surg. 1995; 53:1412.
17. Broadbent, HB, Broadbent, HB, Jr., Golden, WH. Bolton standards of dentofacial developmental growth. St Louis: CV Mosby; 1975.
18. Brunell, JA, Bhat, M, Lipton, JA. Prevalence and distribution of selected occlusal characteristics in the US population. 1988–1991. J Dent Res. 1996; 75:706.
19. Busby, BR, Bailey, LJ, Proffit, WR, et al. Long-term stability class III treatment: A study of 5-year postsurgical results. Int J Adult Orthodon Orthognath Surg. 2002; 17:159.
20. Capelozza, L, Martins, A, Mazzotini, R, da Silva, HG. Effects of dental decompensation on the surgical treatment of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1996; 11:165–180.
21. Cevidanes, L, Baccetti, T, Franchi, L, et al. Comparison of two protocols for maxillary protraction: Bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010; 80:799–806.
22. Chamberland, S, Proffit, WL. Short-term and long-term stability of surgically assisted rapid palatal expansion revisited. Am J Orthod Dentofacial Orthop. 2011; 139:815–822.
23. Cho, HJ. Effect of rigid fixation on orthodontic finishing after mandibular bilateral sagittal split setback: The case for miniplate monocortical fixation. J Oral Maxillofac Surg. 2012; 70:e310–e321.
24. Chong, Y, Ive, JC, Årtun, J. Changes following the use of protraction headgear for early correction of Class III malocclusion. Angle Orthod. 1996; 66:351–362.
25. De Clerck, H, Cevidanes, L, Baccetti, T. Dentofacial effects of bone-anchored maxillary protraction: A controlled study of consecutively treated Class III patients. J Oral Maxillofac Surg. 2010; 138(5):577–581.
26. Demetriades, N, Chang, DJ, Laskarides, C, Papageorge, M. Effects of mandibular retropositioning, with or without maxillary advancement, on the oro-naso-pharyngeal airway and development of sleep-related breathing disorders. J Oral Maxillofac Surg. 2010; 68:2431–2436.
27. Downs, WB. Variations in facial relationships: Their significance in treatment and prognosis. Am J Orthod Dentofacial Orthop. 1948; 34:812.
28. El-Gheriani, AA, Maher, BS, El-Gheriani, AS, et al. Segregation analysis of mandibular prognathism in Libya. J Dent Res. 2003; 82:523–527.
29. Ellis, E, III., McNamara, JA, Jr. Components of adult Class III open bite malocclusion. Am J Orthod Dentofacial Orthod. 1984; 86:277.
30. Epker, BN, Fish, LC. The surgical-orthodontic correction of class III skeletal open bite. Am J Orthod Dentofacial Orthop. 1978; 73:601.
31. Epker, BN, Fish, LC, Paulus, PJ. The surgical-orthodontic correction of maxillary deficiency. Oral Surg Oral Med Oral Pathol. 1978; 46:171.
32. Epker, BN, Turvey, TA, Fish, LC. Indications for simultaneous mobilization of the maxilla and mandible for the correction of dentofacial deformities. Oral Surg Oral Med Oral Pathol. 1982; 54:369.
33. Farkas, LG, Sohm, P, Kolar, JC, et al. Inclinations of the facial profile: Art versus reality. Plast Reconstr Surg. 1985; 75:509.
34. Gu, G, Gu, G, Nagata, J, et al. Hyoid position, pharyngeal airway and head posture in relation to relapse after the mandibular setback in skeletal Class III. Clin Orthod Res. 2000; 3:67–77.
35. Hirdnaka, D, Kelly, J. Stability of simultaneous orthognathic surgery on the maxilla and mandible: A computer assisted cephalometric study. Int J Adult Orthodon Orthognath Surg. 1987; 2:193.
36. Hohl, TH, Epker, BN. Macrogenia: A study of treatment results with surgical recommendations. J Oral Surg. 1976; 41:545.
37. Ishii, H, Morita, S, Takeuchi, U, Nakamura, S. Treatment effect of combined maxillary protraction and chincap appliance in severe skeletal Class III cases. Am J Orthod Dentofacial Orthop. 1987; 92:304–312.
38. Jabaley, ME, Edgerton, ME. Surgical correction of congenital midface retrusion in the presence of mandibular prognathism. Plast Reconstr Surg. 1969; 44:1.
39. Jacobson, A, Evans, WG, Preston, CB, Sadowsky, PL. Mandibular prognathism. Am J Orthod. 1974; 66:140–171.
40. Joss, CU, Joss-Vassalli, IM, Bergé, SJ, Kuijpers-Jagtman, AM. Soft tissue profile changes after bilateral sagittal split osteotomy for mandibular setback: A systematic review. J Oral Maxillofac Surg. 2010; 68:2792–2801.
41. Kawamoto, HK, Jr. Reduction mentoplasty [discussion]. Plast Reconstr Surg. 1982; 70:151.
42. Kelly, JE, Harvey, C. An assessment of the teeth of youths 12-17 years. Department of Health, Education, and Welfare Publication No (HRA) 77-1644. Washington, DC: National Center for Health Statistics; 1977.
43. Kim, YG, Oh, SH. Effect of mandibular setback surgery on occlusal force. J Oral Maxillofac Surg. 1997; 55:121.
44. Kobayashi, T, Honma, K, Nakajima, T, et al. Masticatory function in patients with mandibular prognathism before and after orthognathic surgery. J Oral Maxillofac Surg. 1993; 51:997.
45. Kobayashi, T, Watanabe, I, Ueda, K, et al. Stability of the mandible after sagittal ramus osteotomy for correction of prognathism. J Oral Maxillofac Surg. 1986; 44:693.
46. Kondo, E. The course of treatment of a class III skeletal open bite case and its analysis. Aust Orthod J. 1993; 12:217.
47. LaBlanc, JP, Turvey, TA, Epker, BN. Results following simultaneous mobilization of the maxilla and mandible for the correction of dentofacial deformities: Analysis of 100 consecutive patients. J Oral Surg. 1982; 54:607.
48. Lew, KK, Foong, WC, Loh, E. Malocclusion prevalence in an ethnic Chinese population. Aust Dent J. 1993; 38:8.
49. Liao, YF, Chiu, YF, Huang, CS, et al. Presurgical orthodontics versus no presurgical orthodontics: Treatment outcomes of surgical-orthodontic correction for skeletal class III open bite. Plast Reconstr Surg. 2010; 126:2074–2083.
50. de Lira Ade, L, de Moura, WL, de Barros Vieira, JM, et al. Surgical predication of skeletal and soft tissue changes in Class III treatment. J Oral Maxillofac Surg. 2012; 70:e290–e297.
51. Luhr, HG. Zur stabilen osteosynthese bei unterkiefer–frakturen. Dtsch Zahnarztl Z. 1968; 23:754.
52. Luhr, HG. Skelettverlagernde operationen zur harmonisierung des gesichtsprofils––probleme der stabilen fixation von osteotomiesegmenten. In: Pfeifer G, ed. Die asthetik von form und funktion in der plastischen und wiederherstellungschirurgie. Berlin: Springer-Verlag; 1985:87.
53. Magnusson, T, Ahlborg, G, Svartz, K. Function of the masticatory system in 20 patients with mandibular hypo- or hyperplasia after correction by a sagittal split osteotomy. Int J Oral Maxillofac Surg. 1990; 19:289.
54. McHugh, M, Van Sickels, JE. Effect of stabilization of a bilateral sagittal split on orthodontic finishing after mandibular setback: A case for bicortical fixation. J Oral Maxillofac Surg. 2012; 70:e301–e309.
55. McNance, AM, Moss, JP, James, DR. Stability of surgical correction of patients with skeletal III and skeletal II anterior open bite, with increased maxillary mandibular plane angle. Eur J Orthod. 1992; 14:198.
56. McNance, AM, Moss, JP, Wright, WR, et al. A three-dimensional soft tissue analysis of 16 skeletal class III patients following bimaxillary surgery. Br J Oral Maxillofac Surg. 1992; 30:221.
57. Milicesco, V. La valeur de la photographie, de la crâniometrie et de la téléradiographie dans le prognathisme mandibulaire anatomique. Rev Stomatol. 1968; 69:474–480.
58. Miotti, A. Rassegna bibliografica sull’eziologia ed epidemiologia del prognatismo mandibolare. Dent Cadmos. 1982; 50:29–32.
59. Moser, K, Freihofer, HP. Long-term experience with simultaneous movement of the upper and lower jaw. J Oral Maxillofac Surg. 1980; 8:271.
60. Nagai, I, Tanaka, N, Noguchi, M, et al. Changes in occlusal state of patients with mandibular prognathism after orthognathic surgery: A pilot study. Br J Oral Maxillofac Surg. 2001; 39:429.
61. Nagamine, T, Kobayasgi, T, Nakajima, T, et al. The effects of surgical-orthodontic correction of skeletal class III malocclusion on mandibular movement. J Oral Maxillofac Surg. 1993; 51:385.
62. Norholt, SE, Sindet-Pedersen, S, Jensen, J. An extended Le Fort I osteotomy for correction of midface hypoplasia: A modified technique and results in 35 patients. J Oral Maxillofac Surg. 1996; 54:1297.
63. Obwegeser, HL. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. Part 1. Oral Surg. 1957; 10:677.
64. Obwegeser, HL. Eingriffe am overkiefer zur korrektur des progenen zustandsbildes. Schweiz Monatschr Zahnheilkd. 1965; 75:365–373.
65. Obwegeser, HL. Surgical correction of small or retrodisplaced maxillae. Plast Reconstr Surg. 1969; 43:352–365.
66. Obwegeser, HL. Die einzeitige vorbewegung des oberkiefers and ruckbewegung des unterkiefers zur korrektur der extremen “progenie. ”. Schweiz Monatschr Zahnheilkd. 1970; 80:547–555.
67. Ohkura, K, Harada, K, Morishima, S, et al. Changes in bite force and occlusal contact area after orthognathic surgery for correction of mandibular prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:141.
68. Papadopoulos, MA, Lazaridou-Terzoudi, T, Oland, J, et al. Comparison of soft and hard tissue profiles of orthognathic surgery patients treated recently and 20 years earlier. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:e8.
69. Pepersack, WJ, Chausse, JM. Long-term follow-up of the sagittal split technique for correction of mandibular prognathism. J Maxillofac Surg. 1978; 6:117–140.
70. Perthes, G. Operative korrektur der progenie. Zentralbl Chir. 1922; 49:1540–1541.
71. Phillips, C, Medland, WH, Fields, HW, Jr. Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg. 1992; 7:139.
72. Posnick, JC, Mandibular excess and maxillary deficiency. Craniofacial and maxillofacial surgery in children and young adults. Posnick, JC, eds. Craniofacial and maxillofacial surgery in children and young adults; Vol 38. WB Saunders Co, Philadelphia, 2000:1004–1024.
73. Posnick, JC, Agnihotri, N. Managing chronic nasal airway obstruction at the time of orthognathic surgery: A twofer. J Oral Maxillofac Surg. 2011; 69(3):695–701.
74. Posnick, JC, Fantuzzo, J, Orchin, J. Deliberate operative rotation of the maxillo-mandibular complex to alter the A-point to B-point relationship for enhanced facial esthetics. J Oral Maxillofac Surg. 2006; 64:1687–1695.
75. Posnick, JC, Fantuzzo, JJ, Troost, T. Simultaneous intranasal procedures to improve chronic obstructive nasal breathing in patients undergoing maxillary (Le Fort I) osteotomy. J Oral Maxillofac Surg. 2007; 65:2273–2281.
76. Proffit, W, Fields, H, Jr. Contemporary orthodontics, ed 3. St Louis: Mosby; 2007.
77. Proffit, WR, Fields, HW, Moray, LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the N-HANES III survey. Int J Adult Orthodon Orthognath Surg. 1998; 13:97–106.
78. Proffit, WR, Phillips, C, Dann, C, IV. Who seeks surgical orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990; 3:153.
79. Proffit, WR, Phillips, C, Dann, C, IV., et al. Stability after surgical-orthodontic correction of skeletal class III malocclusion: 1. Mandibular setback. Int J Adult Orthodon Orthognath Surg. 1991; 6:7.
80. Proffit, WR, Phillips, C, Dann, C, Turvey, TA. Stability after surgical-orthodontic correction of skeletal class III malocclusion: 3. Combined maxillary and mandibular procedures. Int J Adult Orthodon Orthognath Surg. 1991; 6:221.
81. Proffitt, WR, Phillips, C, Turvey, TA. Stability after mandibular setback: Mandible-only versus 2-jaw surgery. J Oral Maxillofac Surg. 2012; 70:e408–e414.
82. Reitzik, M. Skeletal and dental changes after surgical correction of mandibular prognathism. J Oral Surg. 1980; 38:109.
83. Reyes, BC, Baccetti, T, McNamara, JA, Jr. An estimate of craniofacial growth in Class III malocclusion. Angle Orthod. 2006; 76:577–784.
84. Reyneke, JP, Evans, WG. Surgical manipulation of the occlusal plane. Int J Adult Orthodon Orthognath Surg. 1990; 5:99–110.
85. Rosen, H. Facial skeletal expansion: Treatment strategies and rationale. Plast Reconstr Surg. 1992; 89:798.
86. Rosen, H. Aesthetics in facial skeletal surgery. Perspect Plast Surg. 1993; 6:1.
87. Rosen, HM. Porous block hydroxyapatite as an interpositional bone-graft substitute in orthognathic surgery. Plast Reconstr Surg. 1989; 83:985.
88. Rosen, HM. Segmental osteotomies of the maxilla. Clin Plast Surg. 1989; 16:785.
89. Rosen, HM. Maxillary advancement for mandibular prognathism: Indication and rationale. Plast Reconstr Surg. 1991; 87:823.
90. Sakamoto, E, Sugawara, J, Umemori, M, Mitani, H. Craniofacial growth of mandibular prognathism during pubertal growth period in Japanese boys: Longitudinal study from 10–15 years of age. Jpn J Orthod Soc. 1996; 55:372–386.
91. Samman, N, Tong, AC, Cheung, LK, et al. Analysis of 300 dentofacial deformities in Hong Kong. Int J Adult Orthodon Orthognath Surg. 1992; 7:5.
92. Sar, C, Arman-Özçirpici, A, Uçkan, S, Yazici, AC. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 2011; 139:636–649.
93. Sassouni, V, Nanda, S. Analysis of dentofacial vertical proportions. Am J Orthod. 1964; 50:801.
94. Scholssmann, A. Cited by G Perthes: Operative korrektur der progenie. Zentralbl Chir. 1922; 49:1540–1541.
95. Silverstein, K, Quinn, PD. Surgically-assisted rapid palatal expansion for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:725.
96. Simpson, W. The results of surgery for mandibular prognathism. Br J Oral Surg. 1974; 12:166.
97. Singh, GD. Morphologic determinants in the etiology of class III malocclusion: A review. Clin Anat. 1999; 12:382–405.
98. Singh, GD, McNamara, JA, Jr., Lozanoff, S. Procrustes, Euclidean and cephalometric analysis of the morphology of the mandible in human class III malocclusions. Arch Oral Biol. 1998; 43:535–543.
99. Skaloud, F. New surgical method for correction of prognathism of the mandible. Oral Surg Oral Med Oral Pathol. 1951; 4:689–694.
100. Sorokolit, CA, Nanda, RS. Assessment of the stability of mandibular setback procedures with rigid fixation. J Oral Maxillofac Surg. 1990; 48:817.
101. Stea, G. Notre experience dans le transientdu prognatism. Rev Stomatol. 1971; 72:559.
102. Stella, JP, Astrand, P, Epker, BN. Patterns and etiology of relapse after correction of class III open bite via subcondylar ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1986; 1:91.
103. Stella, JP, Streater, MR, Epker, BN, Sinn, DP. Predictability of upper lip soft tissue changes with maxillary advancement. J Oral Maxillofac Surg. 1989; 47:697.
104. Stiles, KA, Luke, JE. The inheritance of malocclusion due to mandibular prognathism. J Hered. 1953; 44:241–245.
105. Sugawara, J, Tsuchikawa, T, Soya, T, Mitani, H. Late adolescent growth of skeletal Class III craniofaces in Japanese girls: Average growth from 14–17 years of age based on longitudinal data [Japanese]. Nihon Kyosei Shika Gakkai Zasshi. 1983; 42:399–408.
106. Thompson, EM, Winter, RM. Another family with the “Habsburg jaw. ”. J Med Genet. 1988; 25:838–842.
107. Throckmorton, GS. Masticatory function in patients with mandibular prognathism before and after orthognathic surgery [discussion]. J Oral Maxillofac Surg. 1993; 51:1002.
108. Throckmorton, GS. Effect of mandibular setback surgery on occlusal force [discussion]. J Oral Maxillofac Surg. 1997; 55:126.
109. Tollaro, I, Baccetti, T, Franchi, L. Class III malocclusion in the deciduous dentition: A morphological and correlation study. Eur J Orthod. 1994; 16:401–408.
110. Tornes, K. Extraoral and intraoral vertical subcondylar ramus osteotomy for correction of mandibular prognathism. Int J Oral Maxillofac Surg. 1987; 16:671.
111. Tornes, K, Wisth, PJ. Stability after vertical subcondylar ramus osteotomy for correction of mandibular prognathism. Int J Oral Maxillofac Surg. 1988; 17:242.
112. Trauner, R, Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. II. Operating methods for microgenia and distoocclusion. Oral Surg Oral Med Oral Pathol. 1957; 10:787–792.
113. Turvey, TA, Hall, DJ, Fish, LC, Epker, BN. Surgical orthodontic treatment planning for simultaneous mobilization of the maxilla and mandible in the correction of dentofacial deformities. Oral Surg Oral Med Oral Pathol. 1982; 54:491.
114. Vanarsdale, R, White, R. Three-dimensional analysis for skeletal problems. Int J Adult Orthodon Orthognath Surg. 1994; 9:159.
115. Van der Dussen, FN, Egyedi, P. Premature aging of the face after orthognathic surgery. J Craniofac Surg. 1990; 18:335.
116. Wardrop, RW, Wolford, LM. Maxillary stability following downgraft and/or advancement procedures with stabilization using rigid fixation and porous block hydroxyapatite implants. J Oral Maxillofac Surg. 1989; 47:336.
117. Watanabe, M, Suda, N, Ohyama, K. Mandibular prognathism in Japanese families ascertained through orthognathically treated patients. Am J Orthod Dentofacial Orthop. 2005; 128:466–470.
118. Westwood, P, McNamara, JA, Jr., Baccetti, T, et al. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003; 123:306–320.
119. Williams, MD, Sarver, DM, Sadowsky, PL, et al. Combined rapid maxillary expansion and protraction facemask in the treatment of class III malocclusion in growing children: A prospective long-term study. Semin Orthod. 1997; 3:10.
120. Wisth, PJ. Mandibular function and dysfunction in patients with mandibular prognathism. Am J Orthod. 1984; 85:193–198.
121. Wolfe, SA, Berkowitz, S. Combined maxillary and mandibular procedures: Sequential or simultaneous. In: Plastic surgery of the facial skeleton. Boston: Little, Brown; 1989:417.
122. Wollf, G, Wienker, TF, Sander, H. On the genetics of mandibular prognathism: Analysis of large European noble families. J Med Genet. 1993; 30:112–116.
123. Wilhelm-Nold, I, Droschl, H. Die frühbehandlung der progenie im milchgebiß im vergleich zur behandlung im wechselgebiß. J Orofacial Orthopedics/Fortschr Kieferorthop. 1990; 51(3):165–179.
124. Yamaguchi, T, Park, SB, Narita Maki, K, Inoue, I. Genomewide linkage analysis of mandibular prognathism in Korean and Japanese patients. J Dent Res. 2005; 84:255–259.
125. Zhou, Y, Hagg, U, Rabie, AB. Severity of dentofacial deformity, the motivations and the outcome of surgery in skeletal Class III patients. Chin Med J (Engl). 2002; 115:1031.



