10 Masses and Devices
Key Points
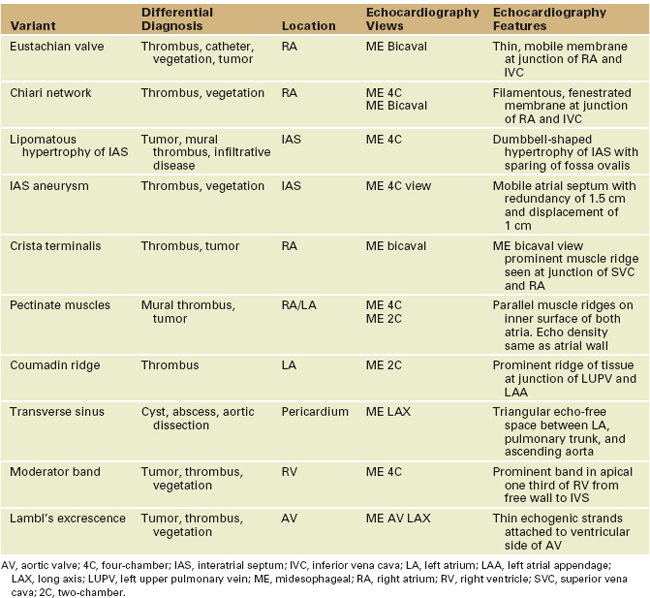
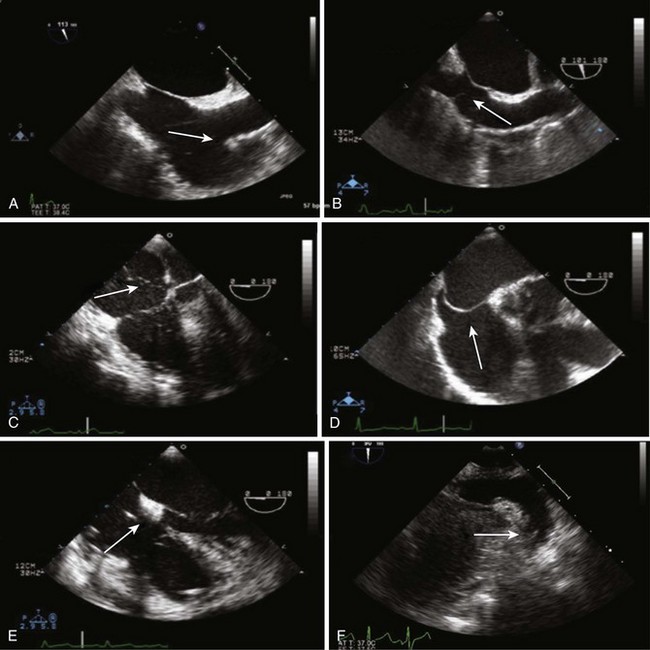
Several normal cardiac structures may mimic abnormal masses. In this section, we describe some of the structures (Table 10-1) that are frequently mistaken for pathologic entities.
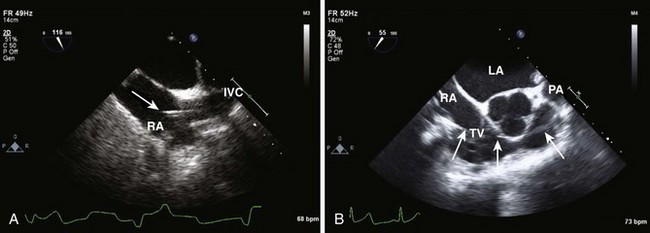
Right Atrium
Crista Terminalis
Eustachian Valve
Left Atrium
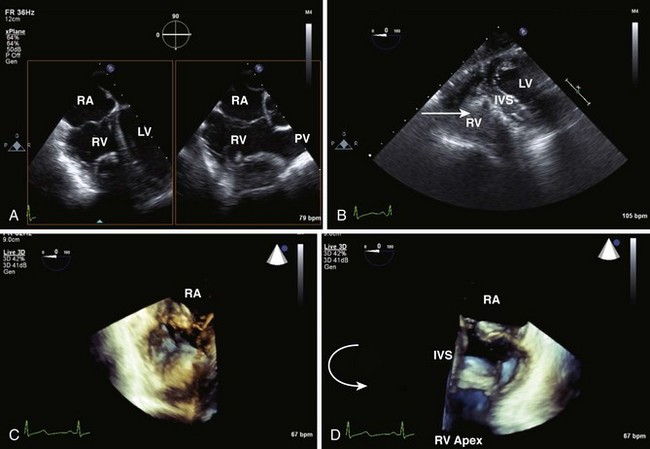
Right Ventricle
Left Ventricle
Aortic Valve
Pericardium
Transverse Sinus, Fat Pad, Cyst
Transverse Sinus
Fat Pad
Transesophageal Echocardiography Assessment of Intracardiac Masses
Systematic Transesophageal Echocardiography Assessment of Intracardiac Masses
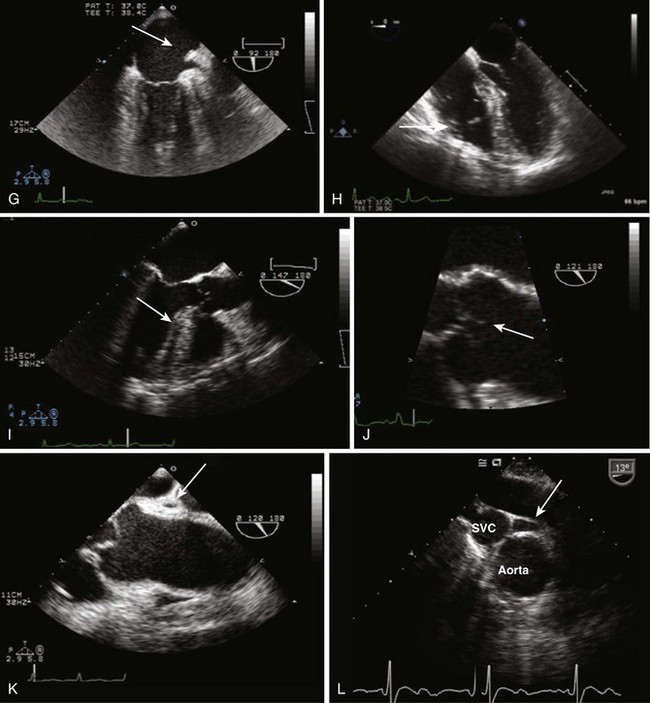
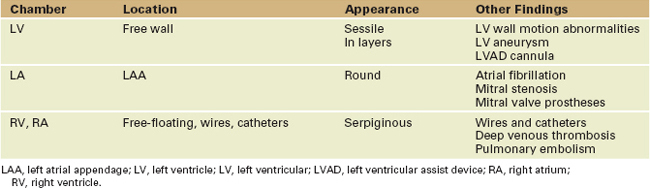
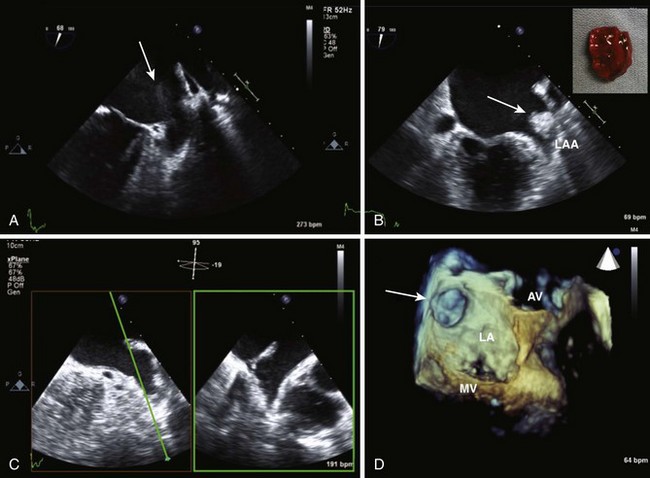
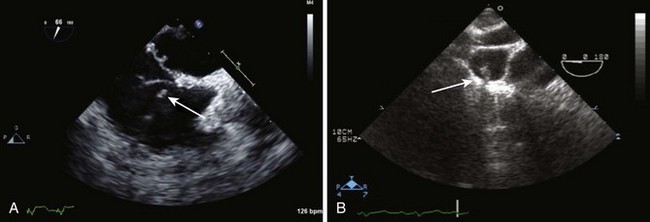
Intracardiac Thrombi
Spontaneous Echocardiographic Contrast
Left Atrium
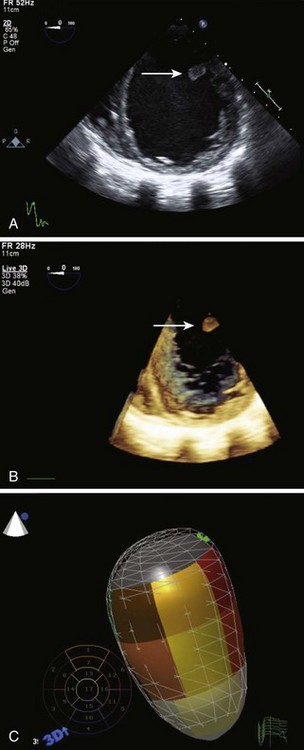
Left Ventricle
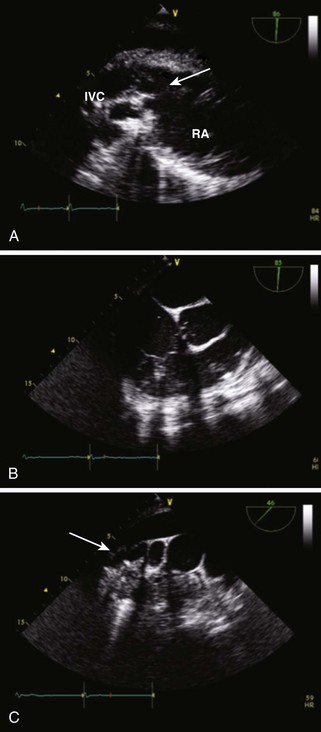
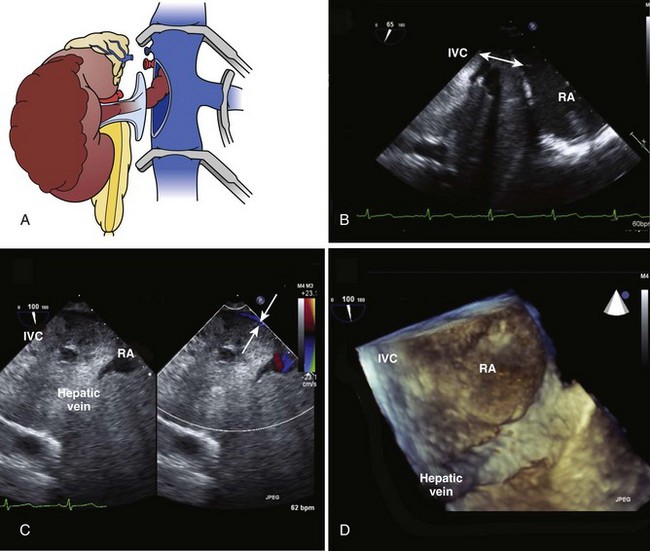
Inferior Vena Cava, Right Atrium, Right Ventricle
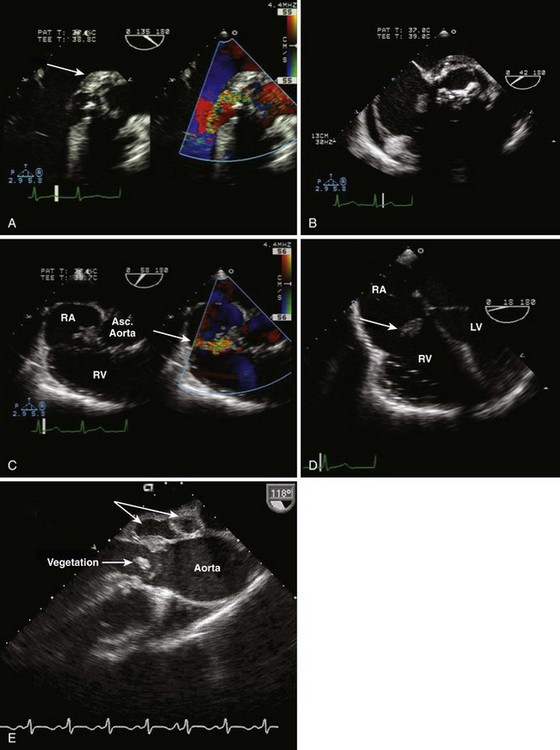
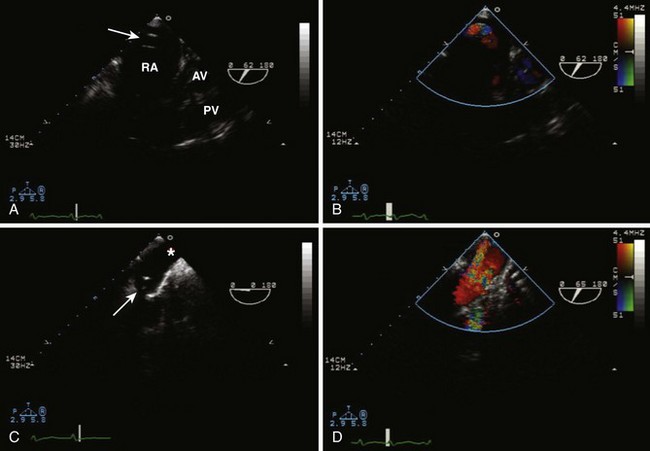
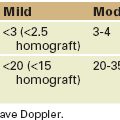
Infective Endocarditis
TABLE 10-3 MODIFIED DUKE CRITERIA
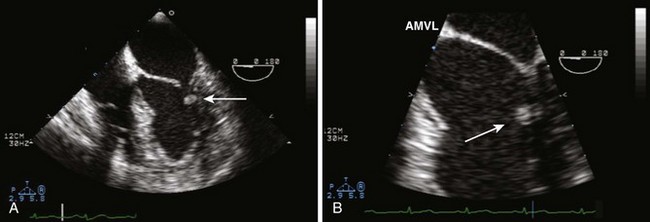
Vegetations
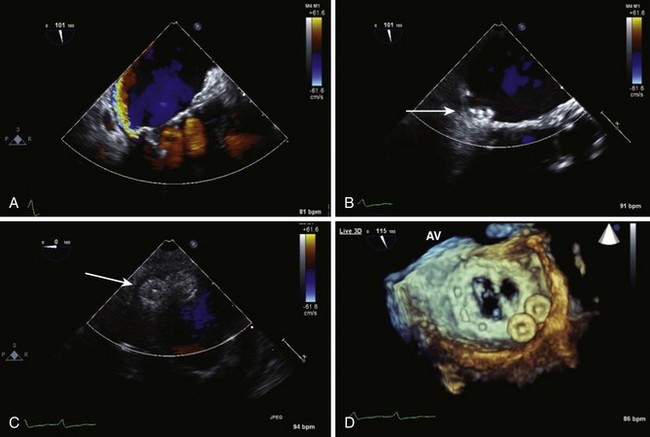
Aortic Valve
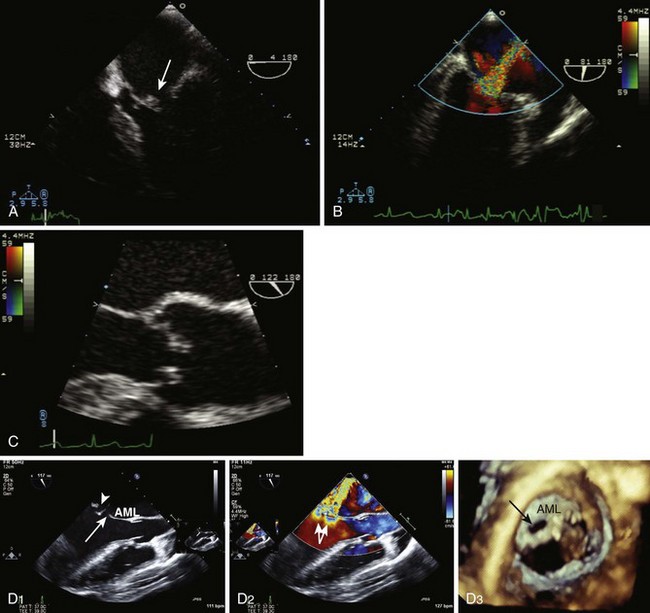
Mitral Valve
Tricuspid Valve
Prosthetic Valves
Abscess
Fistulae
Key Points
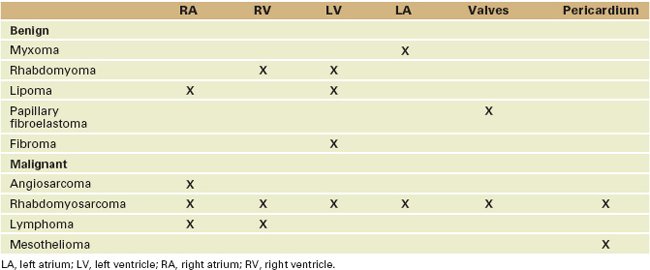
Cardiac Tumors
Benign Primary Cardiac Tumors
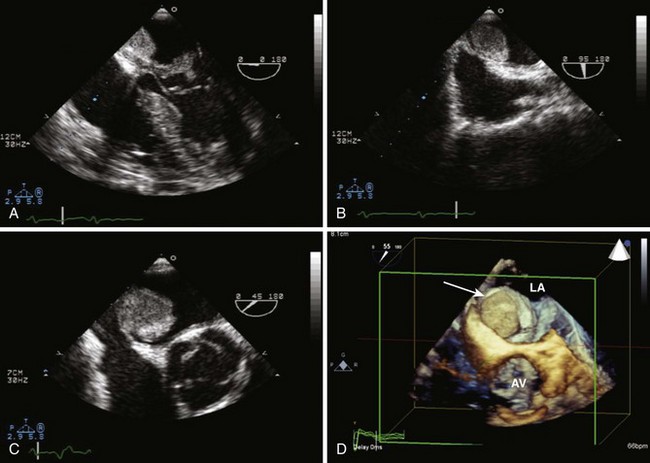
Myxoma
Papillary Fibroelastoma
Malignant Primary Cardiac Tumors
Lymphoma
Intraoperative Echocardiographic Assessment of Cardiac Tumors
Before Cardiopulmonary Bypass
After Cardiopulmonary Bypass
Key Points
Devices for Closure of Intracardiac Shunts
Atrial Septal Defect, Patent Foramen Ovale Device Closure
Before Deployment
Central Venous Catheters
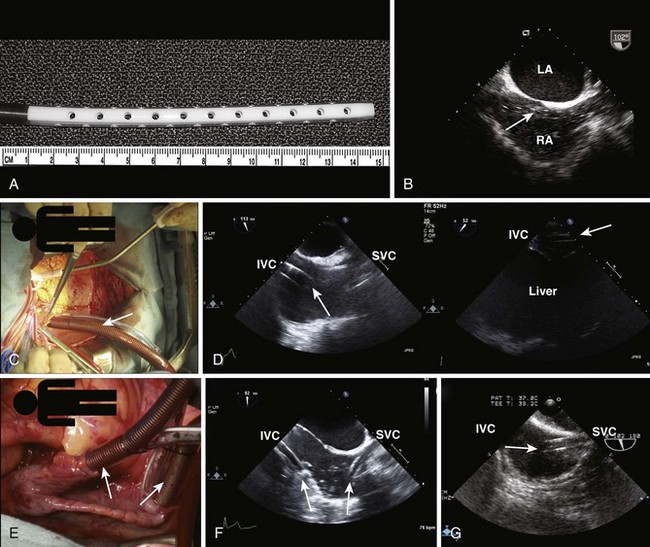
Cardiopulmonary Bypass
Venous Cannulas
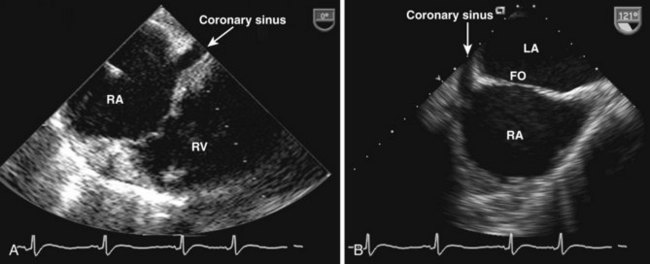
Coronary Sinus Catheter
Arterial Cannulas
Key Points
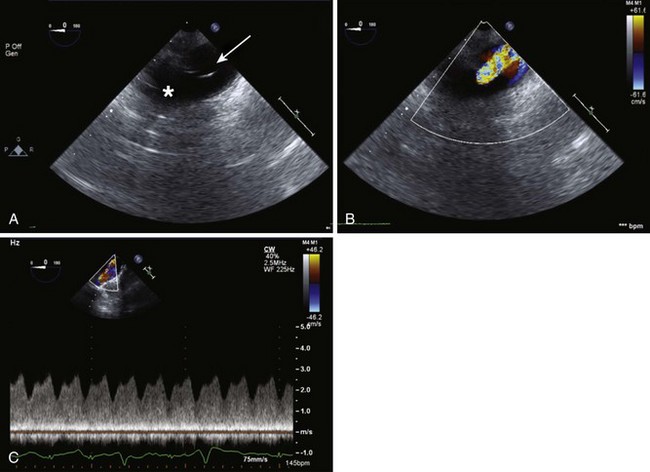
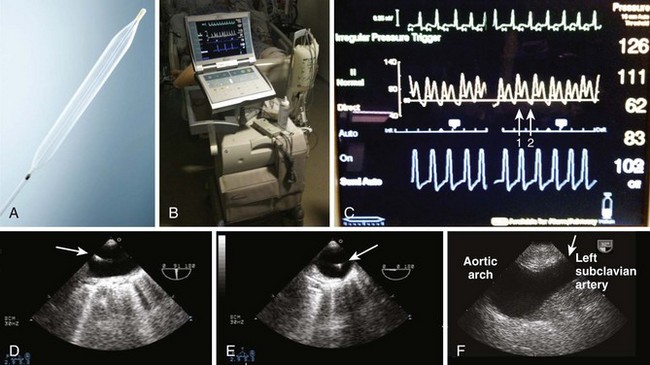
Intra-aortic Balloon Pump
Baseline Assessment
Positioning
Post Positioning
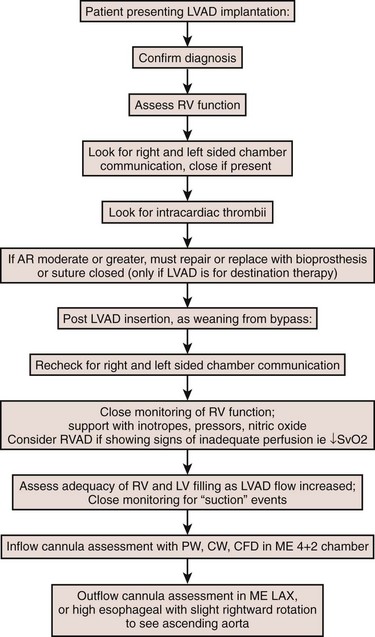
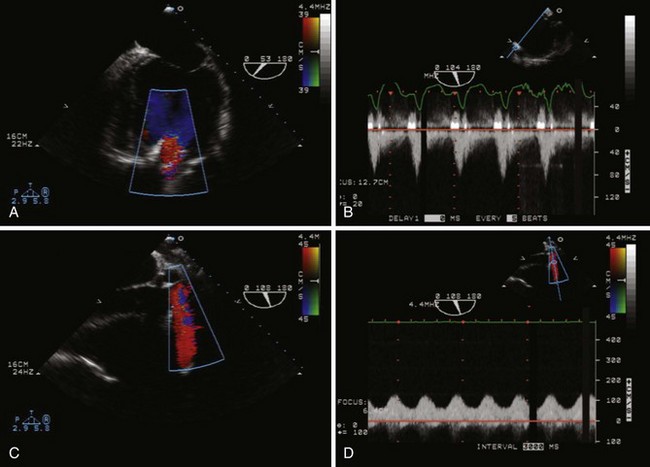
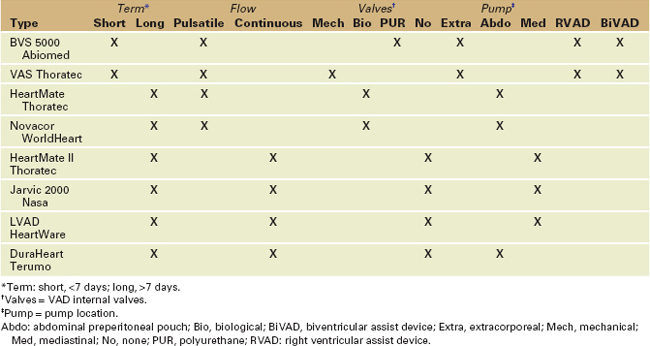
Ventricular Assist Devices
Assessment of Left Ventricular Assist Device Placement (Figures 10-18 and 10-19)
Cannulation
Baseline
Weaning from Cardiopulmonary Bypass
Post Implant
Postoperative Low Device Output and Common Complications
Extracorporeal Membrane Oxygenation
Cannulation
Insertion
Weaning
Key Points
1 Goldman JH, Foster E. Transesophageal echocardiographic (TEE) evaluation of intracardiac and pericardial masses. Cardiol Clin. 2000;18:849-860.
Nice review of TEE imaging of masses.
2 Kerut EK, Norfleet WT, Plotnick GD, Giles TD. Patent foramen ovale: A review of associated conditions and the impact of physiological size. J Am Coll Cardiol. 2001;38:613-623.
Nice clinical and pathologic comparison of the properties and unique characteristics of LV thrombus.
3 Schneider B, Zienkiewicz T, Jansen V, et al. Diagnosis of patent foramen ovale by transesophageal echocardiography and correlation with autopsy findings. Am J Cardiol. 1996;77:1202-1209.
Details the utility of 3D echocardiography in evaluating the LAA for thrombus.
4 Ling LH, Oh JK, Tei C, et al. Pericardial thickness measured with transesophageal echocardiography: Feasibility and potential clinical usefulness. J Am Coll Cardiol. 1997;29:1317-1323.
An excellent clinical and imaging reference for IE.
5 Durand M, Lamarche Y, Denault A. Pericardial tamponade. Can J Anaesth. 2009;56:443-448.
A nice descriptive paper outlining the early experience with percutaneous cardiac interventions.
6 Srichai MB, Junor C, Rodriguez LL, et al. Clinical, imaging, and pathological characteristics of left ventricular thrombus: A comparison of contrast-enhanced magnetic resonance imaging, transthoracic echocardiography, and transesophageal echocardiography with surgical or pathological validation. Am Heart J. 2006;152:75-84.
7 Karakus G, Kodali V, Inamdar V, et al. Comparative assessment of left atrial appendage by transesophageal and combined two- and three-dimensional transthoracic echocardiography. Echocardiography. 2008;25:918-924.
8 Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: Utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96:200-209.
9 Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003;108:1146-1162.
10 Bayer AS, Bolger AF, Taubert KA, et al. Diagnosis and management of infective endocarditis and its complications. Circulation. 1998;98:2936-2948.
11 Shapiro LM. Cardiac tumours: Diagnosis and management. Heart. 2001;85:218-222.
12 Balzer J, Kuhl H, Rassaf T, et al. Real-time transesophageal three-dimensional echocardiography for guidance of percutaneous cardiac interventions: first experience. Clin Res Cardiol. 2008;97:565-574.
13 Biner S, Rafique AM, Kar S, Siegel RJ. Live three-dimensional transesophageal echocardiography-guided transcatheter closure of a mitral paraprosthetic leak by Amplatzer occluder. J Am Soc Echocardiogr. 2008;21:1282e7-1282e9.
14 Dennis C, Spreng DSJr, Nelson GE, et al. Development of a pump-oxygenator to replace the heart and lungs: An apparatus applicable to human patients, and application to one case. Ann Surg. 1951;134:709-721.
15 Applebaum RM, Cutler WM, Bhardwaj N, et al. Utility of transesophageal echocardiography during port-access minimally invasive cardiac surgery. Am J Cardiol. 1998;82:183-188.
16 Kirkeby-Garstad I, Tromsdal A, Sellevold OF, et al. Guiding surgical cannulation of the inferior vena cava with transesophageal echocardiography. Anesth Analg. 2003;96:1288-1293. table of contents
17 Lebon JS, Couture P, Rochon AG, et al. The endovascular coronary sinus catheter in minimally invasive mitral and tricuspid valve surgery: A case series. J Cardiothorac Vasc Anesth. 2010;24:746-751.
18 Varadarajan B, Karski J, Vegas A, Heinrich L. A rare complication of intra-aortic balloon pump placement. J Cardiothorac Vasc Anesth. 2005;19:259-260.
19 Deng MC, Edwards LB, Hertz MI, et al. Mechanical circulatory support device database of the International Society for Heart and Lung Transplantation: Third annual report—2005. J Heart Lung Transplant. 2005;24:1182-1187.
20 Rose EA, Gelijns AC, Moskowitz AJ, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345:1435-1443.
21 Vegas A. Assisting the failing heart. Anesthesiol Clin. 2008;26:539-564.