226 Mass Critical Care
The devastating events of September 11, 2001, in the United States, subsequent acts of bioterrorism, and emerging infectious disease pandemics have brought new challenges to the field of disaster management and multidisciplinary hazard mitigation. Even though war- and terrorism-related disasters have gathered much attention recently, natural disasters have occurred with increasing frequency over the past decades. This has been attributed to the growth of human populations in geographically disaster-prone areas, rapid industrialization, and increasing exposure to toxic and hazardous materials.1–3
Analyses of the response of different healthcare systems to major disasters in the past have demonstrated the need for a more clearly identified planning process to attend to the response to multihazard events.4 This provides a basic understanding of common disaster scenarios and highlights the role of the intensivist in the medical response to disasters. It is important for the practicing critical care clinician to keep in mind that their role is first and foremost as a first receiver, rather than first responder; a well-trained intensivist may be of much greater value remaining in the hospital setting rather than quickly mobilizing to the field, where their lack of situational preparedness may make them more of a hindrance than an asset.5
 Background
Background
Major disasters occur regularly and cause widespread human death and suffering. Over the past 2 decades, more than 3 million lives have been lost worldwide to major disasters. A total of 39,073 persons were reported killed by disasters alone in 2001, with the decade’s annual average of around 62,000. Even though the numbers of geophysical disasters such as earthquakes and volcanic eruptions have remained fairly constant over the past decade, the past 2 years have seen the highest number of weather-related disasters reported over the decade.6 As populations grow and occupy spaces that are vulnerable to different hazards, disasters will increase in severity and impact. Recent events since the September 2001 terrorism attacks have brought attention to the effects of manmade disasters on the healthcare system and the need to anticipate and plan for such low-probability yet catastrophic events. Even though there is basic similarity in the response to various hazardous events, each type of disaster presents responders with unique demands. After any disaster, healthcare systems are tasked with preventing excessive deaths, mitigating suffering, and dealing with often overwhelming inadequacy of resources. Over the past few years, disaster medicine has thus grown into a unique specialty to deal with planning and preparing for such cataclysmic events. It shares a common ideal with public health: “greatest good for the greatest number.”3
 Terminology
Terminology
Physicians and healthcare personnel should be familiar with basic nomenclature and terminology in disaster medicine. Clear, common, and concise definitions are important to effective communication and evoking appropriate responses to disaster situations. Uniform use of terminology across healthcare systems provides a basis for analysis and construction of an effective disaster plan and response by all responders.7 Controversies surrounding the definitions of disasters, hazards, and causalities are included in the discussions that follow.
The word disaster connotes a subjective assessment that has various meanings to different people and has an inherent bias, depending on the person using it. For example, a local, state, or federal “disaster declaration” implies commitment of financial and other resources. Similarly, a disaster in one community is not necessarily the same to another. Currently there is no uniformly accepted definition for the word disaster.7 De Boer recognizes the lack of a meaningful definition for the word and proposes instead the term medical severity index (MSI).8 This term, however, has not gained sufficient acceptance for routine use. Different modifiers can lead to different definitions of the term disaster. They include the type of disaster, geographic area involved, timing, onset of the event, size of the community affected, baseline resources available to the community, and finally, the physical, psychosocial, and economic injury caused by the event. However, from a healthcare standpoint, the most important variable that defines a disaster is its functional impact on the healthcare facility.7 Despite various attempts to clear the confusion surrounding the terminology, the issue remains unresolved.7,9–10 What follows are the commonly used definitions in disaster medicine from a healthcare perspective:
 Classification of Disasters
Classification of Disasters
Natural disasters arise from forces of nature and include earthquakes, volcanic eruptions, hurricanes, floods, fire, and tornadoes. In addition, infectious disasters can be classified as epidemic or pandemic and are discussed elsewhere. Manmade disasters are due to identifiable human causes and may be further classified as complex emergencies (e.g., wars, terrorist attacks) and technological disasters (e.g., industrial accidents, explosions from hazardous material).15 Other classifications include those based on onset (acute versus insidious disasters), predictability, duration, and frequency. From a public health perspective, disasters have to be defined by their effect on people and the healthcare system. The concept of functional impact to the healthcare system is thus paramount.15–16
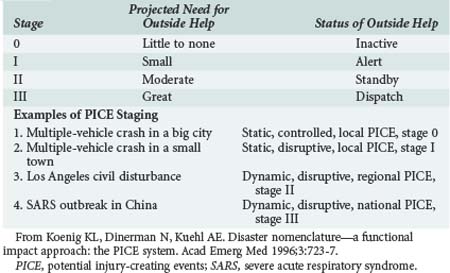
The PICE system attempts to create uniformity to address the wide spectrum of situations.7 The two major aims of this system are to effectively communicate both the operational consequences to a hospital or community and the type and amount of outside assistance needed. Four modifiers for an event are chosen from a standardized group of prefixes, and a stage is assigned (Table 226-1). Column A (first prefix) describes the potential for additional casualties. For example a finite number of persons injured in an airplane crash is a “static event,” whereas an ongoing fire is a “dynamic” event. Column B (second prefix) describes whether local resources are sufficient (“controlled”) or overwhelmed. If they are overwhelmed, the two modifiers “disruptive” and “paralytic” indicate whether they must be simply augmented or totally reconstituted. Paralytic PICE are the most daunting of all situations, and they can be either destructive or nondestructive (Table 226-2). Column C describes the extent of geographic involvement. PICE stage refers to the likelihood that outside medical help is required (Table 226-3). This PICE model provides important concepts for disaster planners, researchers, and responders. Using this system, disasters can be described both prospectively and retrospectively. PICE is a valuable tool for use in planning and disaster mitigation, but the system warrants validation on a wider scale. It may also require further refinement to delineate the type of aid needed by an affected community.7
| A | B | C |
|---|---|---|
| Static | Controlled | Local |
| Dynamic | Disruptive | Regional |
| Paralytic | National | |
| International |
PICE, potential injury-creating events.
Data from Koenig KL, Dinerman N, Kuehl AE. Disaster nomenclature—a functional impact approach: the PICE system. Acad Emerg Med 1996;3:723-7.
| Destructive | Nondestructive |
|---|---|
| Bomb explosion | Snowstorm |
| Earthquake | Employee strike |
| Tornado | Power failure |
| Civil unrest | Water supply cutoff |
| HazMat spill | |
| Fire | |
| Building collapse |
HazMat, hazardous materials; PICE, potential injury-creating events.
Data from Koenig KL, Dinerman N, Kuehl AE. Disaster nomenclature—a functional impact approach: the PICE system. Acad Emerg Med 1996;3:723-7.
 Natural Disasters
Natural Disasters
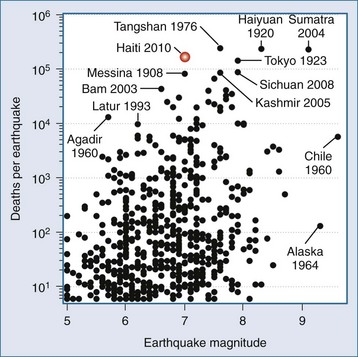
Earthquakes
Earthquakes are a well-known and publicized model of a disaster that results in significant mortality,17 as can be seen in Figure 226-1 describing deaths from earthquakes since 1990. A homogenous population well trained in basic trauma and life support and the architectural design of the stricken area’s housing and public facilities are two major determinants of outcomes for earthquake victims. The massive earthquakes of the past 10 years in Turkey, Taiwan, Sumatra, Kashmir, Sichuan, and Haiti have shown us that sound engineering design for earthquake resistance in civil structures such as schools, hospitals, fire stations, and correctional facilities have a major impact on outcomes. In addition, urban earthquakes generate massive fiscal impact on the world in terms of reconstruction grants provided by wealthier countries for devastated urban areas. Moderately destructive earthquakes in the developing world usually cost up to $10 billion in reconstruction; the needs of developing countries with urban earthquakes may cost an order of magnitude more.
Responders from the very experienced Israel Defense Forces (IDF) air-deployed within 48 hours of the Haiti earthquake. This team had extensive experience over the years with international response and consists of 230 people. The team unpacked and built their portable hospital within 8 hours, and during 10 days of operation treated more than 1100 patients in a facility designed to provide 60 inpatient beds, including 4 intensive care beds and 1 operating room.18 Most of the first wave of casualties presented with crushed limbs with open infected wounds, with the later arrivals presenting with sepsis and poor chance of outcome. Despite the repeated experience from prior earthquakes showing that victims of crush syndrome and acute renal failure require emergency dialysis to prevent death, this facility relied on other international teams for dialysis. Their major dilemmas were practical implementation of the triage algorithm by military personnel to a civilian population. The simple priorities were urgency, resources available, and probability of saving life. Patients with brain injury, paraplegia due to spine injuries, or a low Glasgow Coma Scale score were immediately transferred to other facilities, since no neurosurgical capabilities were available. A triage panel of three senior physicians relieved individual physicians of personal accountability. Half of the intensive care capability was always dedicated to postoperative care, with the remaining 2 beds used for prolonged intensive care; only patients who were expected to stabilize within 24 hours were placed in these beds. The very early discharge policy permitted this military facility to treat more than 100 patients per day.
Second, let us consider the response of the U.S. military, which at this point had a considerable portfolio on providing international disaster relief in catastrophic events such as the Indonesian tsunami that devastated Sumatra. The United States Naval Ship (USNS) Comfort, one of Military Sealift Command’s two hospital ships, was deployed as part of the mission termed “Operation Unified Response.” It started accepting casualties within 7 days of the earthquake. The ship is a 1000-bed facility which includes 75 intensive care unit beds, blood bank, hemodialysis, pathology, physical therapy, morgue, and radiology with computed tomography and ultrasonography capability. It is staffed with 1000 active-duty U.S. medical personnel, including three physician intensivists, and it was allocated to stay up to 6 months.19–20
Third, let us consider the relearning of the lessons of civil-military collaboration in disaster response.21 A volunteer medical team with civilian personnel under the auspices of the international medical corps flew to the Dominican Republic and reached Hopital de l’Universite d’Etat d’Haiti in Port-au-Prince after a long bus ride on January 17. There were more than 800 injured in the partially destroyed facility, with the primary diagnoses being crush injuries, compartment syndrome, infected fractures, and hemorrhagic shock. One physician and one nurse were covering up to 80 critically ill patients in the wards. An aftershock of 5.9 magnitude resulted in an exodus of casualties and higher rates of heat stroke in dehydrated hypovolemic patients exposed to tropical temperatures. Destruction of the prison system released some 4000 criminals into the community, and no security was available until arrival of a U.S. airborne infantry regiment. With arrival of the USNS Comfort on January 20, evacuation of the most critically ill patients started, but a triage list developed rapidly, with ship facilities accepting preferentially complicated injuries, obstetric patients, and maxillofacial injuries. Patients with pelvic fractures, closed head injuries, complete spinal cord lesions, and mechanical ventilation cases were of too-high acuity for the USNS Comfort. Family structures became fragmented as separation of children from parents occurred. Yet the collaboration of civilian and military medical personnel was considered a success.
Next, let us consider the experiences of academic centers delivering care to victims of the Haitian earthquake on-site.22 The Miller School of Medicine of the University of Miami and Project Medishare had the advantage of long experience of collaboration with Haiti as well as close geographic proximity, and they were able to provide emergency relief within 20 hours. Within 8 days, they were able to establish a field hospital at the city airport, and by January 21, 140 patients were transferred into the upgrade facility. The well-organized command center with satellite links for telephone and Internet access were available. A joint adult-pediatric triage team accompanied by Creole-speaking medical staff of Haitian origin was used. Multiple surgeries were performed under local peripheral nerve blocks, with guillotine amputations being frequent. Highest-acuity patients were transferred to the IDF field hospital or the USNS Comfort. The command center eventually provided psychiatrists to manage the posttraumatic stress syndrome and a buddy system for follow-up support.
Finally, one must consider the critical care response from New York City. While many small teams and a large volume of supplies were dispatched, an organized response was delivered under the leadership of Dr. Ernest Benjamin, division chief of critical care in surgery at Mt. Sinai Hospital. Dr. Benjamin, with close family ties to Haiti, arrived in Port-au-Prince 3 days after the initial event and after rapid assessment of needs and resources available, organized the deployment of the 27-member critical care team to his home country, which arrived on January 20. The team remained on-site for 2 weeks and was responsible for postanesthesia and postoperative care delivery, with Dr. Benjamin being deputized as the director of critical care and recovery at the national hospital. The home institution effectively secured anonymous donations of private jets able to transport the team personnel and some 3000 pounds of medical supplies per flight. The team delivered intensive care with minimal technology but with kindness and dignity towards the suffering population. This certainly was not a medical tourism venture but a true integrated response with both language and cultural sensitivities and capabilities, so important in catastrophic situations that will take decades for the local population to recover from.23
Experience in managing catastrophic international disasters continues to accumulate with unfortunate regularity. The preceding discussion suggests that combinations of dialysis, orthopedic surgery, pediatric trauma, security, transportation, posttraumatic stress treatment, and cultural and language sensitivities are crucial in earthquakes. Disasters produce well-defined syndromes with well-defined mortalities. It is the recovery phase that continues to require persistence and improvement. One of the most experienced managers and thought leaders in disaster management, Dr. Eric Noji, enumerated the most important factors in public health after disasters: environmental health, epidemic management, immunization, controlling the spread of HIV/AIDS, management of dead bodies, nutrition, maternal and child health, medical services, and thorough public health surveillance. It is a common error to deliver a few weeks of heroic quality care then abandon the population to the ravages of destroyed infrastructure, including public health organization.24
Volcanic Eruptions
A volcano is a hill or a mountain built around a vent that connects with reservoirs of molten rock below the earth’s surface.25 Different types of eruptive events occur, including pyroclastic explosions, hot ash releases, lava flows, gas emissions, and glowing avalanches (gas and ash releases). Lava flows tend not to result in high casualties, because they are easily avoidable. The “composite” type of volcano is associated with a more violent eruption from within the chimney. These eruptions are associated with air shock waves, rock projectiles (some with high thermal energy), release of noxious gases, pyroclastic flows, and mud flows (lahars). Pyroclastic flows and lahars are often fast moving and are the main cause of damage and deaths from volcanoes, as evidenced by the small eruption of the Nevado del Ruiz in Columbia that killed more than 23,000 people.26 The release of ash and its subsequent rapid buildup on building structures can be substantial, causing them to collapse within a matter of hours. Ash is also responsible for the clogging of filters and machinery, causing electrical storms and fires, and interfering with communications. Ash is a main cause for respiratory-related syndromes and conjunctival and corneal injury. A variety of toxic gases (e.g., carbon dioxide, hydrogen sulfide, sulfur dioxide, hydrogen chloride, hydrogen fluoride, and carbon monoxide [CO]) are released during eruptions, causing bronchospasm, pulmonary edema, hypoxemia, cellular asphyxiation, topical irritation of skin and other mucosal surfaces, and death.27 Damage to health infrastructures and water systems can be severe. Problems related to communication (ashes cause serious interference) and transportation (poor visibility and slippery roads) are likely. Depending on the initial assessment, various needs can be anticipated. Reducing the risk for vulnerable groups of being exposed to ash, raising awareness of the risk associated with ash (health and mechanical risk), and maintaining food security conditions over the long term (lava, ash, and acid rain cause damage to crops and livestock) can help minimize suffering.28
Hurricanes, Cyclones, and Typhoons
The large rotating weather systems that form seasonally over tropical oceans are variously named, depending on the geographic region where they form.29–31 They consist of a calm inner portion called the eye, surrounded by a wall of rain and high-velocity winds. Based on central pressure, wind speed, storm surge, and potential destruction, their severity is graded on a scale of 1 to 5 (Saffir Simpson scale).30 They are among the most destructive natural phenomena. Cyclones during 1970 and 1991 in Bangladesh claimed 300,000 and 100,000 lives, respectively, due to flooding.32 The most devastating hurricane ever to hit the United States was in 1900 at Galveston, Texas. It claimed an estimated 8000 to 12,000 lives.33 The greatest damage to life and property is not from the wind but from secondary events such as storm surges, flooding, landslides, and tornadoes. Ninety percent of all hurricane-related deaths occur from storm surge–related drowning.1 The most common injury patterns include lacerations (during the cleanup phase), followed by blunt trauma and puncture wounds. Late morbidity can be due to post-disaster cleanup accidents (e.g., electrocution), dehydration, wound infection, and outbreaks of communicable disease.31,34 Data from hurricane Katrina confirmed data from previous meteorological events: the leading mechanisms of injuries are fall, lacerations, and piercing injuries, with cleanup being the primary activity at the time of injury.35 Recent experiences in the aftermath of hurricane Katrina in 2005 indicate that resources may have to be provided for an extended period after the initial inciting event, and that significant resources may have to be provided for patients with chronic medical illnesses.34,36
Floods
There are three major types of floods: flash floods (caused by heavy rain and dam failures), coastal floods, and river floods. Together, they are the most common type of disasters and account for at least half of all disaster-related deaths.37,38 The primary cause of death is drowning, followed by hypothermia and injury due to floating debris.39,40 The impact on the health infrastructures and lifeline systems can be massive and may result in food shortages. Interruption of basic public services (e.g., sanitation, drinking water, electricity) may result in outbreaks of communicable disease.38,40 Another concern is the increase in both vectorborne diseases (e.g., malaria, St. Louis encephalitis) and displacement of wildlife (e.g., poisonous snakes and rodents).39,40
Landslides
Landslides are more widespread than any other geologic event. They are defined as downslope transport of soil and rock resulting from natural phenomena or manmade actions. Landslides can also occur secondary to heavy storms, volcanic eruptions, and earthquakes. Landslides cause high mortality and few injuries. Trauma and suffocation by entrapment are common. Pending an assessment, needs can be anticipated, such as search and rescue, mass casualty management, and emergency shelter for the homeless.41,42
Pandemic 2009 H1N1 Influenza a Virus
Within weeks, the virus quickly spread worldwide through human-to-human transmission. On April 26, 2009, the CDC’s Strategic National Stockpile began releasing 25% of the supplies in the stockpile for the treatment and protection from influenza.43 On June 11, 2009, the World Health Organization (WHO) declared the 2009 H1N1 influenza a global pandemic, generating the first influenza pandemic of the 21st century, with more than 70 countries reporting cases of H1N1 infection. By June 19, 2009, all 50 states in the United States, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands had reported cases of 2009 H1N1 infection. More strikingly, the Centers for Disease Control and Prevention (CDC) Emerging Infections Program (EIP) estimated the number of hospitalizations and deaths in people 64 years and younger. The virus was most likely to strike children, young adults, and those with underlying pulmonary and cardiac disease. Pregnant women in their second and third trimester were also at high risk. Patients requiring intensive care had a remarkable prevalence of obesity.43
Influenza vaccines are most effective not only to prevent but also to mitigate the severity of illness. The pandemic H1N1 influenza vaccine was promptly developed by the WHO and national authorities. A national influenza vaccination campaign was launched in the United States in October 2009, and the first H1N1 vaccine was made available at that time. Despite the rapid response of the authorities, developing countries in the Southern Hemisphere experienced delays and shortages of the vaccines. Thus, recent research and developmental work have been encouraging for developing a “universal” influenza vaccine that could provide efficacious cross-reactive immunity and induce broad protection against different variants and subtypes of the influenza virus.44
To date, the preliminary data show that about 8% of H1N1 patients were hospitalized (23 per 100,000 population); 6.5% to 25% of these required being in the ICU (28.7 per million inhabitants) for a median of 7 to 12 days, with a peak bed occupancy of 6.3 to 10.6 per million inhabitants; 65% to 97% of ICU patients required mechanical ventilation, with median ventilator duration in survivors of 7 to 15 days; 5% to 22% required renal replacement therapy; and 28-day ICU mortality was 14% to 40%.45–51
Critical care capacity is a key element of hospital surge capacity planning.10 The proportion of ICU beds occupied by patients with H1N1 varied. In Australia and New Zealand, it peaked at 19%7 while in Mexico, many patients required mechanical ventilation outside the ICUs.6 To match the surge capacity with increasing ICU demands during a pandemic is a difficult task, since uncertainty exists for many of these parameters. The disease brought a surge of not only critically ill patients but patients who required prolonged mechanical ventilation and ICU management. Hospitals should maximize the number of ICU beds by expanding ICUs and other areas with appropriate beds and monitors. Elective procedures should be minimized when resources are limited, and critical care capacity should be augmented.
Safe practices and safe respiratory equipment are needed to minimize aerosol generation when caring for patients with influenza. These measures include handwashing and wearing gloves and gowns. The use of N95 respirators reduces the transmission of epidemic respiratory viruses. Staff training in personal protective equipment use is essential. Use of bag-mask ventilation and disconnection of the ventilator circuit should be minimized. Moreover, the use of heated humidifiers on ventilators, Venturi masks, and nebulized medications should be avoided.52
When the number of critically ill patients far exceeds a hospital’s traditional critical care capacity, modified standards of critical care to provide limited but high-yield critical care interventions should be the goal in order to accommodate far more patients. Triage criteria should be objective, transparent, and ethical and be applied justifiably and publicly disclosed. The ICU triage protocols for pandemics should only be triggered when ICU resources across a broad geographic area are or will be overwhelmed despite all reasonable efforts to extend resources or obtain additional resources.53 The Sequential Organ Failure Assessment (SOFA) score, though not validated, has been proposed to determine qualification for ICU admission during mass critical care.
The major characteristics of 2009 H1N1 influenza A infection were the rapidly progressive lower respiratory tract disease leading to acute respiratory distress syndrome (ARDS) with refractory hypoxemia. A substantial number of H1N1 ICU patients required advanced ventilatory support (ranging from 1.7% to 11.9%) and rescue therapies including high levels of inspired oxygen and positive end-expiratory pressure (PEEP), inverse ratio ventilation, airway pressure release ventilation (APRV), neuromuscular blockade, inhaled nitric oxide, high-frequency oscillatory ventilation (HFOV), extracorporeal membrane oxygenation (ECMO), volumetric diffusive respiration, and prone-positioning ventilation.46,49,51,54 Of particular interest was the successful use of ECMO in the management of refractory hypoxemia in these patients in two studies. The median durations of therapy and survival rates to ICU discharge were 10 days and 15 days—71% and 67%, respectively.55,56
As of March 13, 2010, the CDC estimates of 2009 H1N1 influenza cases, hospitalizations, and deaths in the United States since April 2009 were 60 million cases, 270,000 hospitalizations, and 12,270 H1N1-related deaths, respectively.57 The virus did not mutate during the pandemic to a more lethal form. Widespread resistance to oseltamivir did not develop. The WHO declared an end to the H1N1 pandemic on Aug 10, 2010. According to Margaret Chan, the Director-General of the WHO, the H1N1 virus is no longer the dominant circulating virus worldwide. Based on the available evidence and experience from past pandemics, “it is likely that the virus will continue to cause serious disease in the younger age group, at least in the immediate post-pandemic period. The H1N1 virus is expected to take on the behavior of a seasonal influenza virus and to circulate for some years.”
Other Natural Disasters
Tornadoes occur most commonly in the North American Midwest. Over 4115 deaths and 70,000 injuries have been ascribed to them during the years 1950 to 1994. They cause widespread destruction of community infrastructure. Injuries most commonly seen are complex contaminated soft-tissue injury (50%), fractures (30%), head injury (10%), and blunt trauma to the chest and abdomen (10%).58,59 Firestorms, wildfires, tsunamis, winter storms, and heat waves are other natural phenomena capable of creating mass injuries from thermal burns, airway injury, smoke inhalation, heat-related disorders, and hypothermia.60–63
 Manmade Disasters
Manmade Disasters
Transportation Disasters
Transportation accidents can produce injuries and death similar to those seen in major natural disasters. Some of the largest civilian disasters in North America have been related to transportation of hazardous materials.64 Motor vehicle accidents, railway accidents, airplane crashes, and shipwrecks are some of the common transportation accidents. They cause a wide range of injuries including multiple trauma, fractures, burns, chemical injuries, hypothermia, dehydration, asphyxiation, and CO inhalation. The hazard risk to a healthcare facility increases with its proximity to a chemical plant or highway, and such factors should be considered in the emergency preparedness plan of the hospital.65
Weapons of Mass Destruction
Weapons of mass destruction (WMD) are those nuclear, biological, chemical, incendiary, or conventional explosive agents that pose a potential threat to health, safety, food supply, property, or the environment. Since the devastating terrorist attacks in September 2001 and subsequent intentional release of anthrax spores in the United States, there is growing concern around the world about the possible threat of chemical, biological, or nuclear weapons used against a civilian population. Compared with the frequency of natural and technology-related disasters, the incidence of use of WMD to cause death and injury is relatively rare. However, biological and chemical weapons are relatively accessible, and WMD are thought to be available to most foreign states and terrorist groups. In response to a WMD incident, healthcare personnel will be called on to manage unprecedented numbers of casualties in an environment of panic, fear, and paranoia that accompanies terrorism. Because most attacks occur without warning, the local healthcare system will be the first and most critical interface for detection, notification, rapid diagnosis, and treatment. The best defense in reducing casualties will therefore rest on the ability of medical and public health personnel to recognize symptoms and provide rapid clinical and epidemiologic diagnosis of an event. This requires that healthcare providers be well informed of potential biological, chemical, and nuclear agents. They must have a heightened index of suspicion and be able to identify unusual disease patterns to determine whether WMD are the etiologic agents of illness. Physicians will need to practice appropriate surveillance and reporting and develop knowledge of mass decontamination, use of proper personal protection equipment, and safety protocols related to a biological, chemical, or radiologic event.66–68 Salient characteristics and brief management strategies of the different WMD are discussed here. Detailed description of individual biological and chemical agents, diagnosis, postexposure management, vaccination, infection control measures, and use of personal protection equipment is beyond the scope of this chapter.
Biological Weapons
Biological weapons can be either pathogens (disease-causing organisms such as viruses or bacteria) or toxins (poisons of biological origin). Compared with other WMD, biological weapons are characterized by ease of accessibility and dissemination, difficulty in detection because of their slow onset of action, and their ability to cause widespread panic through the fear of contagion. They can be spread through various means, including aerial bombs, aerosol sprays, explosives, and food or water contamination. Multiple factors including particle size of the agent, stability of the agent, wind speed, wind direction, and atmospheric conditions can alter the effectiveness of a delivery system. Based on the ease of dissemination, ability to cause high mortality, public panic and social disruption, and requirement for special action for public health preparedness, the Centers for Disease Control and Prevention (CDC) has classified biological weapons into three categories (Table 226-4).69 Category A agents are of particular concern because they can cause widespread disease through their ease of transmission, result in high mortality rates, cause panic and social disruption, and require special attention during public health preparedness. General features that should alert healthcare providers to the possibility of a bioterrorism-related outbreak include70:
The main steps involved in management of a bioterrorist attack are containment, notification, confirmation, and directed antibiotic treatment and prophylaxis. In the event of a suspected bioterrorist attack, the CDC has issued protocols for early notification of local and state public health department agencies.71 The Association for Professionals in Infection Control and Epidemiology in cooperation with the CDC devised the “Bioterrorism Readiness Plan,” with a template for healthcare facilities to serve as a reference document to facilitate preparation of bioterrorism readiness plans for healthcare facilities. This tool guides infection-control professionals and healthcare epidemiologists in the development of practical and realistic response plans for their institutions in the event of a bioterrorism attack.72 Discussion of individual biological agents is beyond the scope of this chapter. The reader is referred to our review of bioterrorism and critical care,73,74 as well as the numerous resources and websites available on the Internet (Box 226-1).
Box 226-1
Additional Disaster Information Resources
General Disaster Resources and Websites
Chemical Weapons
Chemical incidents are accidental or intentional events that threaten or do expose responders and members of the public to a chemical hazard. Agents that have been commonly used as chemical weapons are also used in industrial processes. Most industrial incidents occur at an interface between transport, storage, processing, use, or disposal of hazardous chemicals, where these systems are more vulnerable to failure, error, or manipulation. The catastrophic effect of these agents has been utilized several times in the past for military purposes, and with the proliferation of these weapons, civilian populations are now faced with a significant threat.75 Typically, chemical warfare agents are classified into the following categories76:
Nuclear Weapons and Radiation Accidents
Approximately 50% of the energy released from a nuclear bomb is due to the blast and shock waves, giving a majority of the survivors blast-related injuries as well as creating extensive infrastructure damage. About 35% of the energy released is thermal radiation (in orders of tens of millions of degrees), giving rise to high-degree skin burns. Depending on the size of the device and the altitude of detonation, an electromagnetic pulse is generated with the explosion. This is capable of disrupting all electrical equipment within 20 to several hundreds of kilometers.78 The radiation-related energy released from a nuclear detonation is around 15% (5% from the initial nuclear radiation and 10% from the residual nuclear radiation), giving rise to external contamination, systemic irradiation, and internal contamination-related illness. Immediate ionizing radiation consists of gamma, beta, neutron, and a small amount of alpha radiation. Residual radiation occurs in the forms of induced radiation and fallout. Induced radiation occurs because of neutron-induced gamma activity of the immediate soil, silicon, manganese, aluminum, zinc, copper, and sodium. The half-lives of the various substances are a few minutes to 15 hours. “Fallout” is the fusion of the various radionuclides generated in the fission reaction with condensation, producing a snowflake-like debris that falls to earth. Fallout is a potential form of delayed radiation exposure and can cause internal contamination.78
Surviving hospitals and staff near an impact area should serve as a triage center and transport victims to unaffected centers elsewhere through notification of the National Disaster Medical System Hospital Activation System.79 Other agencies that have to be notified include the Federal Bureau of Investigation, Nuclear Regulatory Commission, Department of Energy, and the Department of Defense. Large-scale decontamination should be managed outside the hospital area as far as is possible, but plans for indoor decontamination should also be in place. A radiation emergency area (both in and out of the hospital) should to be designated, with checkpoints nearing the cold zone. Management plans for the safe disposal of human waste and bodies should be in place so as not to increase the exposure risk. Triage of patients should be done on the basis of doing the greatest good for the greatest number. Based on predictive models, isolated irradiation, burns, and blast-related injuries would constitute 40% of injuries. Combined injuries would account for the rest. Attending to trauma victims should take precedence over all other medical issues, because a given patient is not likely to succumb immediately from radiation injury.
Patient care should begin with the use of universal precautions and personal protective equipment.78 Dosimetry readings of the area may help during triage, defining those with systemic irradiation injury (possibly received greater than 450 rad exposure). In determining patient viability, three parameters are of the most use: time of onset of vomiting, the decrease in the absolute lymphocyte count over a 24-hour period, and presence of conventional trauma burns.80 Victims who are not viable or who have lethal doses of radiation exposure are likely to benefit from supportive/palliative care.
Hazardous Materials Disasters
A hazardous material (HazMat) is a substance potentially toxic to the environment or living organisms. Full-scale disasters from HazMat are relatively rare, but isolated incidents are among the most common in the community and are not limited to chemicals but can include various biological and radiologic materials as well. Knowledge of the types of industries present in the community would be helpful in developing a potential plan to deal with likely HazMat situations. Management of a HazMat situation requires attention to several key points: identification of the offending agent, appropriate personal protection equipment of responders, prompt containment of the agent, demarcating areas for decontamination (including removal and disposal of clothes and waste from the decontamination), and resuscitation of victims. Injuries secondary to release of hazardous materials can present as chemical burns, inhalational injury, and a variety of systemic injuries.81–82
 Medical Disaster Syndromes
Medical Disaster Syndromes
Blast Injuries
Bombs contain an array of compounds such as nitroglycerin, trinitrotoluene, and others that are encased in a metal or plastic case. Decomposition of the solid or liquid compound into gas leads to massive dissipation of energy and pressure creating a blast wave (shock wave). This destructive effect can be increased by the presence of nuts, nails, and bolts in the casing. Water transmits blast waves more efficiently than air, with the greatest impact being on structures that are the deepest.83 There are four types of blast injuries:
The most common injuries associated with fatality in blast incidents include subarachnoid hemorrhage (66%), fracture of the skull (51%), lung contusion (47%), tympanic membrane rupture (45%), and liver laceration (34%). Unfortunately, the extent of the blast injury cannot be assessed during the course of rapid triage examinations. In the absence of overt trauma, a focused physical examination should include examination for ruptured tympanic membrane, hypopharyngeal contusions, hemoptysis, and auscultation for wheezing. The presence of a ruptured tympanic membrane is almost always an indicator that the patient has been exposed to a blast wave powerful enough to cause serious damage. The thorax is frequently involved in a blast injury, manifesting with wheezing, hemoptysis, pneumothorax, hemothorax, and air embolism. Patients may have myocardial contusion as well. The presentation of serious pulmonary injury may be delayed. Pulmonary barotrauma is the most common fatal primary blast injury. Patients with nonpenetrating lung injury will likely have hypoxia requiring support ranging from oxygen therapy to mechanical ventilation. This may result from pulmonary contusion, systemic air embolism, and disseminated intravascular coagulation. Acute gas embolism, a form of pulmonary barotrauma, is also associated with blast injuries. Air emboli most commonly occlude blood vessels in the brain or spinal cord, resulting in neurologic symptoms that must be differentiated from the direct effect of trauma. Patients thought to have gas embolism require decompression treatment. Administration of 100% oxygen by tight-fitting facemask and left lateral recumbent position may help. Definitive treatment is with the use of hyperbaric oxygen. Patients with blast injury of the lung are likely to present with abdominal injuries that are usually more delayed. These include delayed bowel perforation and liver lacerations. The former may warrant exploratory laparotomy.84–87
All patients with significant burns, suspected air embolism, radiation or white phosphorus contamination, abdominal signs of contusion/hematoma, or clinical evidence of pulmonary contusion or pneumothorax should be admitted to the hospital. Patients with tympanic membrane rupture and suspected pneumothorax should get some form of chest imaging, and a significant observation period may be warranted. Other investigations must be judiciously ordered, keeping in mind the limited availability of resources in a mass-casualty incident. Screening urinalysis for presence of hematuria, tests for CO poisoning (explosion in a closed space or associated with fire) and cyanide toxicity (due to combustion of plastics), and assessment of acid-base status may be indicated. Use of abdominal computed tomography to rule out intestinal hematomas is not routinely warranted and should be dictated by clinical signs and symptoms. Pregnant patients with blast injuries warrant special consideration, and appropriate consultation is necessary to rule out blast injury to the fetus.85 Supplemental oxygen therapy, maintaining spontaneous respiration, and low PEEP (if mechanical ventilation is required) are some of the guiding principles in managing pulmonary blast injuries. Routine corticosteroids and antibiotics are not warranted. Exposure to white phosphorus explosives (e.g., in hand grenades) deserves special mention. Use of a Wood’s light in a darkened resuscitation suite or operating room may help identify white phosphorus light particles in the wound. White phosphorus injury can cause lung injury through irritation, as well as severe hypokalemia and hyperphosphatemia with cardiac arrhythmias and death. External burns should be lavaged with 1% copper sulfate solution. This forms a blue-black cupric phosphide coating and prevents combustion so that the particles can safely be removed.88
Crush Injury Syndrome
Crush injury syndrome refers to systemic manifestations of extensive muscle damage caused by entrapment of victims under collapsed buildings or debris. Reported incidence depends on the type of disaster, ranging from 2% to 40%. Metabolic alterations from the release of muscle constituents into the circulation include myoglobinemia leading to acute renal failure, hyperkalemia, hyperphosphatemia, and disseminated intravascular coagulation. Increased intracellular calcium concentrations appear to be the final common pathway. Muscle damage that occurs is due not only to direct crush injury but also to vascular injury and insufficiency leading to altered compartment pressures and reperfusion injury. Inelastic fascial sheaths encase skeletal muscles in the forearm and lower leg and are particularly vulnerable to dramatic increases in compartment pressures, resulting in compartment syndrome. An intracompartmental pressure in excess of 40 mm Hg lasting longer than 8 hours defines this syndrome. Pressures as high as 240 mm Hg can be seen with crush injuries. Compartment syndromes are seen with limb fractures, use of military antishock trousers, pneumatic splints, vascular injuries, and crush injuries. The affected limb may present with severe pain associated with passive stretch or extension, flaccid paralysis, and sensory loss. Capillary refill and peripheral pulses are usually present unless the compartmental pressure equals the diastolic pressure. Diagnosis requires a high degree of clinical suspicion and entails prompt bedside measurement of compartmental pressures. A simple and easy method that can be performed in the hospital or field hospital is using an 18-gauge needle attached to a mercury manometer. In an ICU, pressure transducers used to measure central venous pressures can be attached to the 18-gauge needle to obtain the same information.89
Resuscitation of patients with crush injury (any victim crushed or immobilized for more than 4 hours) should begin in the field. After adequate intravenous access is achieved, isotonic fluid replacement with normal saline (rate of 1-1.5 L/h) should begin even before extrication of the crushed limb. If fluid therapy is delayed, the incidence of renal failure increases to 50%; delays of 12 hours are associated with a 100% incidence. Occurrence of renal failure is associated with a 20% to 40% mortality rate. Urinary alkalinization with sodium bicarbonate and mannitol or acetazolamide administration are used to maintain urine pH greater than 7.5. Although this intervention is widely used, there are no prospective randomized controlled trials to support it. Dialysis may be indicated if aggressive fluid resuscitation fails, and this may create a huge demand for dialysis machines in disaster situations. Peritoneal dialysis if the abdomen is intact and continuous arteriovenous hemofiltration may be other useful options. The latter option, however, is complicated by hemorrhagic problems related to the use of heparin and immobilization. Life-threatening infections are common after crush injuries and may be increased in the presence of a fasciotomy. In unsalvageable limbs, it may be advisable to perform on-field amputations to avoid the systemic effects of a crush injury syndrome. For this purpose, ketamine is the anesthetic and analgesic of choice because of its safety profile in the field.89
Particulate Health Problems
Many disasters result in release of copious particulate matter, causing a wide spectrum of respiratory illnesses including cough, wheezing, smoke inhalation injury, reactive airways disease, and ARDS. Volcanic eruptions with associated pyroclastic flows and ash fall are some of the most devastating producers of particulate matter. Mortality in these situations arises from suffocation by ash in the upper airways, ARDS, and inhalation burns. The massive building collapse and fires associated with the 2001 World Trade Center terrorist attack caused significant pulmonary complaints among rescue personnel.90
Smoke inhalation injury resulting from exposure to noxious products of combustion in fires may account for as many as 75% of fire-related deaths in the United States. The three primary mechanisms that lead to injury in smoke inhalation are thermal damage, asphyxiation, and pulmonary irritation. Combustion utilizes oxygen in the airways and causes a decrease in fraction of inspired oxygen, leading to hypoxemia. Increased CO levels decrease the oxygen-carrying capacity of the blood and cause myocardial depression. Combustion of plastics, polyurethane, wool, silk, nylon, rubber, and paper products can lead to the production of cyanide gas, resulting in anaerobic metabolism and decreased oxygen consumption. Rarely, we may also find methemoglobinemia, which reduces oxygen-carrying capacity.91
Serial bronchoscopy is indicated in the first 18 to 24 hours to assess airway edema and sloughing. Early bronchoscopy can be of diagnostic and therapeutic value, particularly when lobar atelectasis is present. High-flow humidified oxygen is critical to reverse or prevent hypoxemia. About 50% of patients with an inhalation injury require tracheal intubation, and this number increases in patients who have burn injuries. The need for tracheal intubation is determined by the need to maintain airway patency and pulmonary toilet and to provide positive-pressure ventilation. Positive-pressure ventilation with PEEP increases short-term survival and is associated with decreased tracheobronchial cast formation. Cyanide toxicity (levels > 0.1 mg/L) should be promptly treated using a USA cyanide kit. Recommendations for the use of hyperbaric oxygen in the setting of CO poisoning include CO levels greater than 25% to 30%, neurologic compromise, metabolic acidosis, or electrocardiographic evidence of myocardial ischemia, infarction, or dysrhythmias. Hyperbaric oxygen has been used in cyanide toxicity but has not been proven effective. The role of corticosteroids is controversial, and they can be detrimental if given in the presence of cutaneous burns. Empirically administered antibiotics are another issue in dispute. Common pitfalls in the initial management of smoke inhalation are using initial PaO2 to predict adequacy of oxygenation, placing small-diameter nasotracheal tubes, intubating without applying PEEP, and restricting fluids for concomitant inhalation and burn injury.91,92 General measures that could be employed in a field setting include simple airway protection by clearing any particulate matter in the airway, supplemental oxygen, and nebulizer treatment if available. Patients with preexisting asthma and emphysema should be observed for exacerbations.
Acute Radiation Syndrome
Ionizing radiation can be either charged or uncharged particles (photons). Beta particles are capable of penetrating a few centimeters of tissue. Gamma rays and x-rays are capable of penetrating through tissue and concrete. Gamma, x-ray, and beta radiations are considered low linear energy transfer radiation. Alpha particles have no penetrating power past the keratinized layer of skin, but they take on clinical significance if they are internalized by ingestion or inhalation. Neutron emission (e.g., from nuclear reactors, nuclear devices, and industrial moisture detectors) is highly potent radiation that penetrates deep and creates denser ionization trails. Alpha and neutron emissions are considered high linear energy transfer radiation and have significantly more biological effects than low linear energy transfer radiation by a factor of up to 20. When the process of ionization occurs within living tissue it causes breakage in the chemical bonds, and the most susceptible target is the cellular DNA. This leads to impaired mitosis and subsequent organ failure. Large doses of radiation are generally considered to cause more biological destruction than fractionated doses. Systemic radiation illness and lethality from it can result from as little as 450 rad. Precise measurements of the amount of radiation following a nuclear accident will be delayed. Hospital gamma cameras are an invaluable resource for helping determine the exposure in an individual. Higher systemic doses are suggested by shorter onset of prodromal symptoms such as nausea, vomiting, and diarrhea. Serial absolute lymphocyte counts will screen those patients who have psychogenic vomiting. Acute radiation syndrome has four distinct phases67,78,80:
Psychological Trauma
The psychological component in a traumatic event is often overlooked, with the major focus usually being on physical health issues. Studies evaluating the emotional impact from disasters indicate that a majority of victims, first responders, and mortuary volunteers will suffer some form of psychological trauma. Intensivists should be aware that behavioral changes may not be only due to the catastrophic insult but also due to organic causes such as head injury, inability to take predisaster psychiatric medications, and toxin or chemical exposure. Groups at risk, such as children, adolescents, and victims who have been exposed to traumatic stressors of bereavement, witnessing death, and situations evoking guilt, fear, or anger, should receive prompt psychiatric and posttraumatic counseling. Interventions such as debriefing, eye movement desensitization and reprocessing, and critical incident stress management may help minimize emotional suffering and morbidity.93
Other Syndromes
Burns, blunt trauma, intraabdominal injury, head injuries, penetrating trauma, and hypothermia are some of the other disaster syndromes encountered in the field. Specific discussion of these entities is beyond the scope of this chapter, and the reader is referred to other chapters for management details.5
 Disaster Preparedness
Disaster Preparedness
For intensivists to be able to deal with a disaster, it is paramount that they be a part of the disaster-planning effort. Disaster planning includes development of action programs to minimize loss of life and damage during a disaster, provide the greatest good for the greatest number of people, train healthcare personnel and civilians, coordinate response efforts, maintain adequate supplies of equipment and personnel, and rehabilitate the community after the disaster. Knowledge of potential disasters to which the community is prone should be an integral part of the planning process. Having an understanding of what the resources and capabilities are of the community, hospital, and its ICU on a continual basis and provision for modular expandability are vital for any successful emergency response. The mere existence of a disaster plan does not ensure that the hospital system is actually prepared.94 The following paragraphs elucidate some of the common issues and misconceptions related to disasters and common principles useful in designing a disaster plan. Subsequently, a pragmatic view is presented of the role of the ICU physician in a disaster situation.
Common Issues and Misconceptions in Disaster Planning
Typically, the hospital nearest to the disaster site will receive the bulk of the casualties. It is thus important to conduct a careful survey of a disaster plan’s jurisdiction to identify potential sites (i.e., industries, nuclear reactors, highways) and likely types of hazardous events that could occur in the area. Hospitals in the nearby area receive few disaster victims, and an average have at least 20% of their beds vacant. Disaster plans would thus need to include transfer agreements between hospitals and nearby ICUs to meet bed shortages by activating the National Disaster Medical System Hospital Activation System.79,94,95
Very few casualties actually require hospital admission. A study of 29 mass-casualty incidents found that less than 10% of casualties required overnight admission under usual criteria (even though more were admitted because they were involved in the disaster rather than because of severity of their condition). Large numbers of casualties with minor conditions will appear at the nearest hospitals, often on foot or in private vehicles, police cars, buses, taxis, and other non-ambulance forms of transport. Field triage stations are often bypassed, and this in turn causes enormous strain on the emergency department services.96
Most of the logistical problems faced in disaster situations are not caused by shortages of medical resources but rather from failure to coordinate their distribution.94 Inexperienced volunteers may not be familiar with the triage system or principles of personal safety, and massive numbers of volunteers can present serious administrative challenges. This results in disorganization and inefficiency.81 Technical hazard sheets designed by the WHO for most disasters also suggest that medical personnel, blood donors, and blood products should not be sent empirically to a disaster site.97
Principles in Disaster Planning
Existing Preparedness Requirements
In developing disaster plans, hospitals must take into account the broad national and local requirements imposed by various governmental agencies. Common agencies involved in this process include the Centers for Medicare and Medicaid Services (CMS) as well as The Joint Commission (TJC). The CMS’s conditions for emergency preparedness and services establish minimum requirements for hospitals that participate in Medicare or Medicaid programs. Similarly, TJC standards apply to a full range of hospitals from small rural to large urban academic centers and are focused on four main areas: (1) emergency preparedness management plan (Standard EC 4.1), (2) security management plan (Standard EC 2.1), (3) hazardous materials and waste management plan (Standard EC 3.1), and (4) emergency preparedness drills (Standard EC 4.2). Readers are referred to the TJC website for the most up-to-date standards for management of environment of care.98
Hazard Vulnerability Analysis
This is the first step of any disaster plan, with the main aim of identifying potential hazardous events and situations that can occur in or around the healthcare facility. This process of evaluating and predicting hazard risk is not restricted to geographic events but extends to institution-specific variables such as utility failures, local threats of gang-related activity, and presence of a local high-risk industry such as a chemical or nuclear power plant. TJC requires a formal documented hazard vulnerability analysis that is integrated with the emergency management plan, setting priorities among potential emergencies and also defining the hospital’s role in the local community-wide emergency plan.98
Incident Command System
The Incident Command System (ICS) is designed to provide the basic architecture of an emergency management response. Major barriers to medical response arise from the lack of coordination among various public and healthcare agencies and from the lack of operational integration of various medical specialties. The ICS incorporates all these agencies and ensures a cooperative and effective response to a crisis. The concept of ICS resulted from the analysis of the devastating wildfires in Southern California in 1970 and has since been modified and successfully adapted to different disaster situations related to healthcare facilities.84–86 The ICS specifies a common terminology and a command structure with five functional sections:
There is a designated person who will have the authority to declare an emergency. All personnel involved in the command system should be aware of the exact predetermined location of the command center. The plan should also provide protocols that will guide notification and the sequence of mobilization of these personnel in a disaster situation. The command system must also have independent telephone lines to ensure uninterrupted communication with the external world in a disaster situation. Once initiated, the ICS has a built-in chain of command that would be responsible for triage of patients and allocation of personnel and resources.99
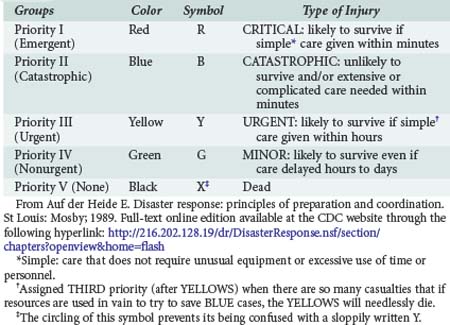
Triage
Appropriate triage is a vital function during an emergency management response. This is a dynamic process that is not necessarily confined to the disaster site or the emergency department but rather is carried through several levels of the medical response pathway of a disaster response. Modern triage is based on the likelihood of survival in relation to the resources available at the time of the decision.100 Problems commonly encountered in the triage process include101:
Major Utilities, Supplies, and Equipment
Disaster plans and drills should factor in the possibility of internal and external power outages and related disruptions (ventilator and monitoring device failures, communication failures including breakdown of cellular phones, and elevator failures) and water supply and gas supply shortages. The plan should have an up-to-date inventory of all supplies and capabilities of the facility. Number of ventilators in use and its absolute capacity, inventory of various ICU supplies, and vendor lists should be readily available if there is sudden demand for supplies. The disaster plan should allow for at least 2 days’ worth of supplies. Regular drills will help identify various bottlenecks and will also provide knowledge of the absolute capacity of devices, equipment, and services in a disaster situation. Plans to evacuate critically ill patients to nearby hospitals in the event of failure of backup systems should also be addressed in the process. Since the anthrax attacks and the resulting strain on antibiotic supplies in 2001, more attention has been paid to the national repository of lifesaving pharmaceuticals and medical supplies called the National Pharmaceutical Stockpile Program. This response is a component of the CDC’s larger Bioterrorism Preparedness and Response Initiative and is composed of a stockpile of pharmaceuticals, vaccines, medical supplies, and equipment to augment local and state resources in a disaster situation. After a federal decision to deploy, a “push package” will arrive by ground or air in 12 hours or less at any location in the United States. A CDC team accompanying the push package will then determine the amount and type of shipments in the second phase.102
Security and Casualty Reception
Security is a major concern during natural or manmade disasters. Desire to seek immediate medical evaluation, panic, and curiosity are some of the forces that place the healthcare facility and its personnel under enormous strain. Internal and external traffic control, protection of personnel who are involved in the response effort, and strict enforcement of staging and triage areas are key security-related issues. Law enforcement plays a more critical role during terrorist attacks or during bioterrorism, and failure to maintain order will lead to rapid overwhelming of the facility’s resources and a disorganized medical response. Because most of the victims will arrive at the hospital by foot or by personal vehicles, provision must be made for a predetermined staging area with adequate mass decontamination facilities and respiratory protective equipment.98,103
 Issues Unique to the Intensive Care Unit
Issues Unique to the Intensive Care Unit
The responsibility of caring for the most serious salvageable casualties in natural and manmade disasters will ultimately involve the critical care physician. As opposed to overwhelming shortage of resources, lack of coordination among various agencies and specialties has been often cited as the main contributing factor to an ineffective emergency medical response. This response therefore requires the cooperation of not just physicians but also between prehospital medical personnel, nurses, and ancillary services such as radiology and laboratory services.53
Possible roles for the intensivist as part of a disaster management planning team include:
 Critical Care in Unconventional Situations
Critical Care in Unconventional Situations
Mobile ICU Teams
Personnel
Based on the anticipated needs of the disaster, appropriate specialists and ancillary personnel are chosen. Given the complexity and inherent unpredictability of staffing for disaster management, a flexible and adaptable approach must be taken to staffing such events.104
Training
Adequate predeparture training is essential for a coordinated and effective response. In addition, interaction and on-site training ensures effective functioning of a foreign medical unit and allows for the smooth transition of care to local physicians when the foreign team departs.84
Casualty Assessment
Studies from the past and more recently the experience of the Israeli defense forces in providing care to earthquake victims in Turkey showed that the effectiveness of mobile ICU teams was limited by time. It sometimes takes 3 days to mobilize such an effort, and crucial time is lost before delivery of intended care. Efforts must therefore be made to epidemiologically assess the efficacy of such teams. They should include review of the overall effort and adequacy of the ICU teams, outcome of victims, operational costs, and analysis of the structure and process of the ICU in the field.104
 Critical Care Transport
Critical Care Transport
Common principles involved in the safe transport of patients include104:
Key Points
Auf Der Heide E. Disaster response: principles of preparation and coordination. St Louis: Mosby; 1989.
Devereaux AV, Dichter JR, Christian MD, et al. Definitive care for the critically ill during a disaster: a framework for allocation of scarce resources in mass critical care: from a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133:51S-66S.
Karwa M, Bronzert P, Kvetan V. Bioterrorism and critical care. Crit Care Clin. 2003;19:279-313.
Rice DH, Kotti G, Beninati W. Clinical review: critical care transport and austere critical care. Crit Care. 2008;12:207.
A focused, relevant review on issues germane to critical care transport and mobile ICUs.
Geiling JA, editor. Fundamental disaster management. Mount Prospect, IL: Society of Critical Care Medicine, 2009.
1 Office of US Foreign Disaster Assistance. Disaster History. Significant Data on Major Disasters Worldwide. United States Agency for International Development. http://www.usaid.gov, 2010. Accessed at
2 Wijkman A, Timberlake L. Natural Disasters: Acts of God or Acts of Man?. New York: Earthscan; 1984.
3 Auf Der Heide E. Disaster Response: Principles of Preparation and Coordination. St. Louis: Mosby; 1989.
4 Rubinson L, Hick JL, Hanfling DG, et al. Definitive care for the critically ill during a disaster: a framework for optimizing critical care surge capacity: from a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133:18S-31S.
5 Geiling JA, editor. Fundamental Disaster Management. Mount Prospect, IL: Society of Critical Care Medicine, 2009.
6 World Disasters Report. Focus on early warning, early action: International Federation of Red Cross and Red Crescent Societies. http://www.ifrc.org/publicat/wdr2009/, 2009. Accessed at
7 Koenig KL, Dinerman N, Kuehl AE. Disaster nomenclature—a functional impact approach: the PICE system. Acad Emerg Med. 1996;3:723-727.
8 de Boer J, Brismar B, Eldar R, Rutherford WH. The medical severity index of disasters. J Emerg Med. 1989;7:269-273.
9 Debacker M, Domres B, de Boer J. Glossary of new concepts in disaster medicine: a supplement to Gunn’s Multilingual Dictionary of Disaster Medicine. Prehosp Disaster Med. 1999;14:146-149.
10 Gunn SW. Multilingual Dictionary of Disaster Medicine and International Relief. Boston: Kluwer Academic Publishers; 1990.
11 McLaughlin S. Ready for anything. A look at the Joint Commission’s new emergency management standards. Health Facil Manage. 2007;20:39-40. 2
12 Adini B, Goldberg A, Laor D, Cohen R, Bar-Dayan Y. Factors that may influence the preparation of standards of procedures for dealing with mass-casualty incidents. Prehosp Disaster Med. 2007;22:175-180.
13 Hick JL, Christian MD, Sprung CL. Chapter 2. Surge capacity and infrastructure considerations for mass critical care. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(Suppl. 1)):S11-S20.
14 Analyzing your vulnerability to hazards. Jt Comm Perspect. 2001;21:8-9.
15 The Disaster process and disaster aid programs: Federal Emergency Management Agency. http://www.fema.gov/hazard/dproc.shtm, 2010. Accessed at
16 Davis JR, Wilson S, Brock-Martin A, Glover S, Svendsen ER. The impact of disasters on populations with health and health care disparities. Disaster Med Public Health Prep. 2010;4:30-38.
17 Billham R. The seismic future of cities. Bull Earthq Eng. 2009;7:839-887.
18 Merin O, Ash N, Levy G, Schwaber MJ, Kreiss Y. The Israeli field hospital in Haiti—ethical dilemmas in early disaster response. N Engl J Med. 2010;362:e38.
19 Boren D, Forbus R, Bibeau P, McKenzie R, McKinsey K. Managing critical care casualties on the Navy’s hospital ships. Crit Care Nurs Clin North Am. 2003;15:183-191.
20 Amundson D, Dadekian G, Etienne M, et al. Practicing internal medicine onboard the USNS COMFORT in the aftermath of the Haitian earthquake. Ann Intern Med. 2010;152:733-737.
21 Auerbach PS, Norris RL, Menon AS, et al. Civil-military collaboration in the initial medical response to the earthquake in Haiti. N Engl J Med. 2010;362:e32.
22 Jaffer AK, Campo RE, Gaski G, et al. An academic center’s delivery of care after the Haitian earthquake. Ann Intern Med. 2010;153:262-265.
23 Benjamin E. Trip Report Dr. Ernest Benjamin, Feb 2010: Association of Hatian Physicians Abroad. http://amheflorida.org/index.php?option=com_content&view=article&id=117:trip-report-dr-ernest-benjamin-feb-2010&catid=48:reports-from-trips-to-haiti&Itemid=88, 2010. Accessed at
24 Noji EK. Public health in the aftermath of disasters. BMJ. 2005;330:1379-1381.
25 Volcano: Federal Emergency Management Agency. http://www.fema.gov/hazard/volcano/index.shtm, 2010. Accessed at
26 Gueri M, Perez LJ. Medical aspects of the “El Ruiz” avalanche disaster, Colombia. Disasters. 1986;10:150-157.
27 Volcanic Eruptions–natural disaster profile–technical hazard sheet: World Health Organization. http://www.who.int/hac/techguidance/ems/volcanos/en/, 2010. Accessed at
28 Hansell A, Oppenheimer C. Health hazards from volcanic gases: a systematic literature review. Arch Environ Health. 2004;59:628-639.
29 Hurricane: Federal Emergency Management Agency. http://www.fema.gov/hazard/hurricane/index.shtm, 2010. Accessed at
30 The Saffir-Simpson Hurricane Wind Scale: National Weather Service National Hurricane Center. http://www.nhc.noaa.gov/aboutsshws.shtml, 2010. Accessed at
31 Tropical cyclones–technical hazard sheet–natural disaster profiles: World Health Organization. http://www.who.int/hac/techguidance/ems/tropical_cyclones/en/index.html, 2010. Accessed at
32 Sommer A, Mosley WH. East Bengal cyclone of November, 1970. Epidemiological approach to disaster assessment. Lancet. 1972;1:1029-1036.
33 National Weather Service National Hurricane Center. http://www.nhc.noaa.gov/, 2010. Accessed at
34 Brevard SB, Weintraub SL, Aiken JB, et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: lessons learned from a level I trauma center. J Trauma. 2008;65:1126-1132.
35 Sullivent EE3rd, West CA, Noe RS, Thomas KE, Wallace LJ, Leeb RT. Nonfatal injuries following Hurricane Katrina—New Orleans, Louisiana, 2005. J Safety Res. 2006;37:213-217.
36 Mattox KL. Hurricanes Katrina and Rita: role of individuals and collaborative networks in mobilizing/coordinating societal and professional resources for major disasters. Crit Care. 2006;10:205.
37 Flood: Federal Emergency Management Agency. http://www.fema.gov/hazard/flood/index.shtm, 2010. Accessed at
38 Floods-Technical Hazard Sheet: World Health Organization. http://www.who.int/hac/techguidance/ems/floods/en/, 2010. Accessed at
39 Flooding and communicable diseases fact sheet: World Health Organization. http://www.who.int/hac/techguidance/ems/flood_cds/en/, 2010. Accessed at
40 Vasconcelos P. Flooding in Europe: a brief review of the health risks. Euro Surveill. 2006;11:E060420 2.
41 Landslide and Debris Flow (Mudslide): Federal Emergency Management Agency. http://www.fema.gov/hazard/landslide/index.shtm, 2010. Accessed at
42 Landslides–technical hazard sheet–natural disaster profiles: World Health Organization. http://www.who.int/hac/techguidance/ems/landslides/en/, 2010. Accessed at
43 The 2009 H1N1 Pandemic: Summary Highlights, April 2009-April 2010: Centers for Disease Control and Prevention. http://www.cdc.gov/h1n1flu/cdcresponse.htm, 2010. Accessed at
44 Steel J, Lowen AC, Wang T, et al. Influenza virus vaccine based on the conserved hemagglutinin stalk domain. MBio. 1, 2010. e00018-e00010 pii
45 Bishop JF, Murnane MP, Owen R. Australia’s winter with the 2009 pandemic influenza A (H1N1) virus. N Engl J Med. 2009;361:2591-2594.
46 Dominguez-Cherit G, Lapinsky SE, Macias AE, et al. Critically Ill patients with 2009 influenza A(H1N1) in Mexico. JAMA. 2009;302:1880-1887.
47 Echevarria-Zuno S, Mejia-Arangure JM, Mar-Obeso AJ, et al. Infection and death from influenza A H1N1 virus in Mexico: a retrospective analysis. Lancet. 2009;374:2072-2079.
48 Jain S, Kamimoto L, Bramley AM, et al. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361:1935-1944.
49 Kumar A, Zarychanski R, Pinto R, et al. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009;302:1872-1879.
50 Rello J, Rodriguez A, Ibanez P, et al. Intensive care adult patients with severe respiratory failure caused by Influenza A (H1N1)v in Spain. Crit Care. 2009;13:R148.
51 Webb SA, Pettila V, Seppelt I, et al. Critical care services and 2009 H1N1 influenza in Australia and New Zealand. N Engl J Med. 2009;361:1925-1934.
52 Sprung CL, Zimmerman JL, Christian MD, et al. Recommendations for intensive care unit and hospital preparations for an influenza epidemic or mass disaster: summary report of the European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Intensive Care Med. 2010;36:428-443.
53 Devereaux AV, Dichter JR, Christian MD, et al. Definitive care for the critically ill during a disaster: a framework for allocation of scarce resources in mass critical care: from a Task Force for Mass Critical Care summit meeting, January 26-27, 2007, Chicago, IL. Chest. 2008;133:51S-66S.
54 Spronk PE, Schultz MJ. Mechanical ventilation in critically ill patients with 2009 influenza A(H1N1). JAMA. 2010;303:939-940. author reply 40-1
55 Freed DH, Henzler D, White CW, et al. Extracorporeal lung support for patients who had severe respiratory failure secondary to influenza A (H1N1) 2009 infection in Canada. Can J Anaesth. 2010;57:240-247.
56 Davies A, Jones D, Bailey M, et al. Extracorporeal membrane oxygenation for 2009 influenza A (H1N1) acute respiratory distress syndrome. JAMA. 2009;302:1888-1895.
57 CDC estimates of 2009 H1N1 influenza cases, hospitalizations and deaths in the United States, April 2009—March 13, 2010: Centers for Disease Control and Prevention. http://www.cdc.gov/h1n1flu/estimates/April_March_13.htm, 2010. Accessed at
58 Tornado: Federal Emergency Management Corporation. http://www.fema.gov/hazard/tornado/index.shtm, 2010. Accessed at
59 Bohonos JJ, Hogan DE. The medical impact of tornadoes in North America. J Emerg Med. 1999;17:67-73.
60 Winter Storms and Extreme Cold. Federal Emergency Management Agency. http://www.fema.gov/hazard/winter/index.shtm, 2010. Accessed at
61 Wildfire: Federal Emergency Management Agency. http://www.fema.gov/hazard/wildfire/index.shtm, 2010. Accessed at
62 Fire: Federal Emergency Management Agency. http://www.fema.gov/hazard/fire/index.shtm, 2010. Accessed at
63 Vegetation Fires–technical hazard sheet-natural disaster profiles: World Health Organization. http://www.who.int/hac/techguidance/ems/vegetation_fires/en/index.html, 2010. Accessed at
64 Horton DK, Berkowitz Z, Haugh GS, Orr MF, Kaye WE. Acute public health consequences associated with hazardous substances released during transit, 1993-2000. J Hazard Mater. 2003;98:161-175.
65 Levinson J, Granot H. Transportation Disaster Response Handbook, 1st ed. Maryland Heights: Academic Press; 2002.
66 Biological and chemical terrorism: strategic plan for preparedness and response. Recommendations of the CDC Strategic Planning Workgroup. MMWR Recomm Rep. 2000;49:1-14.
67 Developing Objectives, Content, and Competencies for the Training of Emergency Medical Technicians, Emergency Physicians, and Emergency Nurses to Care for Casualties Resulting From Nuclear, Biological, or Chemical (NBC) Incidents: American College of Emergency Physicians. http://www.acep.org/workarea/downloadasset.aspx?id=4848, 2001. Accessed at
68 Positioning America’s Emergency Health Care System to respond to acts of terrorism: American College of Emergency Physicians. http://www.acep.org/workarea/downloadasset.aspx?id=4852, 2002. Accessed at
69 Bioterrorism Agents/Diseases: Centers for Disease Control and Prevention. http://www.bt.cdc.gov/agent/agentlist-category.asp, 2010. Accessed at
70 Bozeman WP, Dilbero D, Schauben JL. Biologic and chemical weapons of mass destruction. Emerg Med Clin North Am. 2002;20:975-993. xii
71 Protocols: Interim recommended notification procedures for local and state public health departement leaders in the event of a bioterrorist incident: Centers for Disease Control and Prevention. http://www.bt.cdc.gov/EmContact/Protocols.asp, 2001. Accessed at
72 Bioterrorism readiness plan: a template for healthcare facilities: Centers for Disease Control and Prevention. http://www.cdc.gov/ncidod/dhqp/pdf/bt/13apr99APIC-CDCBioterrorism.PDF, 1999. Accessed at
73 Karwa M, Currie B, Kvetan V. Bioterrorism: Preparing for the impossible or the improbable. Crit Care Med. 2005;33:S75-S95.
74 Karwa M, Bronzert P, Kvetan V. Bioterrorism and critical care. Crit Care Clin. 2003;19:279-313.
75 Hurst G, Tuorinsky S, Madsen J, et al, editors. Medical Managment of Chemical Casualties Handbook, 4th ed, Aberdeen Proving Ground: US Army Medical Research Institute of Chemical Defense (USAMRICD), 2007.
76 Belson MG, Schier JG, Patel MM. Case definitions for chemical poisoning. MMWR Recomm Rep. 2005;54:1-24.
77 Zajtchuk R, Bellamy R. Medical Aspects of Chemical and Biological Warfare, Textbook of Military Medicine. Bethesda: Office of the Surgeon General; 1997.
78 Radiation emergencies: information for clinicians: Centers for Disease Control and Prevention. http://www.bt.cdc.gov/radiation/clinicians.asp, 2010. Accessed at
79 National Disaster Medical System: US Department of Health & Human Services. http://www.phe.gov/PREPAREDNESS/RESPONDERS/NDMS/Pages/default.aspx, 2010. Accessed at
80 Acute Radiation Syndrome: A Fact Sheet for Physicians: Centers for Disease Control and Prevention. http://www.bt.cdc.gov/radiation/arsphysicianfactsheet.asp, 2010. Accessed at
81 Levitin HW, Siegelson HJ. Hazardous materials. Disaster medical planning and response. Emerg Med Clin North Am. 1996;14:327-348.
82 Hazardous Materials: Centers for Disease Control and Prevention. http://www.cdc.gov/nceh/ehs/etp/hazardous.htm, 2010. Accessed at
83 Avidan V, Hersch M, Armon Y, et al. Blast lung injury: clinical manifestations, treatment, and outcome. Am J Surg. 2005;190:927-931.
84 Garner J, Brett SJ. Mechanisms of injury by explosive devices. Anesthesiol Clin. 2007;25:147-160.
85 Sharma BR. Disaster management following explosion. Am J Disaster Med. 2008;3:113-119.
86 Sheffy N, Mintz Y, Rivkind AI, Shapira SC. Terror-related injuries: a comparison of gunshot wounds versus secondary-fragments-induced injuries from explosives. J Am Coll Surg. 2006;203:297-303.
87 Tsokos M, Paulsen F, Petri S, Madea B, Puschel K, Turk EE. Histologic, immunohistochemical, and ultrastructural findings in human blast lung injury. Am J Respir Crit Care Med. 2003;168:549-555.
88 Ritenour AE, Baskin TW. Primary blast injury: update on diagnosis and treatment. Crit Care Med. 2008;36:S311-S317.
89 James T. Management of patients with acute crush injuries of the extremities. Int Anesthesiol Clin. 2007;45:19-29.
90 Aldrich TK, Gustave J, Hall CB, et al. Lung function in rescue workers at the World Trade Center after 7 years. N Engl J Med. 2010;362:1263-1272.
91 Miller K, Chang A. Acute inhalation injury. Emerg Med Clin North Am. 2003;21:533-557.
92 Rabinowitz PM, Siegel MD. Acute inhalation injury. Clin Chest Med. 2002;23:707-715.
93 Silove D, Steel Z. Understanding community psychosocial needs after disasters: implications for mental health services. J Postgrad Med. 2006;52:121-125.
94 Auf der Heide E. Disaster planning, Part II. Disaster problems, issues, and challenges identified in the research literature. Emerg Med Clin North Am. 1996;14:453-480.
95 Barbara JA, Macintyre AG. Medical Surge Capacity and Capability: A Management System for Integrating Medical and Health Resources During Large-Scale Emergencies. Washington, D.C.: U.S. Department of Health and Human Services; 2007.
96 Sasser SM, Hunt RC, Sullivent EE, et al. Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage. MMWR Recomm Rep. 2009;58:1-35.
97 Mass Casualty Management Systems: Strategies and guidelines for building health sector capacity: World Health Organization. http://www.who.int/hac/techguidance/MCM_guidelines_inside_final.pdf, 2007. Accessed at
98 2010 Hospital Accreditation Standards: Joint Commission Resources. http://www.jointcommission.org/, 2010. Accessed at
99 Emergency Management Institute: Incident Command Center Resource Center: Federal Emergency Management Agency. http://training.fema.gov/EMIWeb/IS/ICSResource/index.htm, 2010. Accessed at
100 Christian MD, Hawryluck L, Wax RS, et al. Development of a triage protocol for critical care during an influenza pandemic. CMAJ. 2006;175:1377-1381.
101 Christian MD, Joynt GM, Hick JL, Colvin J, Danis M, Sprung CL. Chapter 7. Critical care triage. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster. Intensive Care Med. 2010;36(Suppl 1):S55-S64.
102 Strategic National Stockpile. Atlanta, GA: Centers for Disease Control and Prevention. http://www.bt.cdc.gov/stockpile/, 2010. Accessed at
103 Parker MM. Critical care and disaster management. Crit Care Med. 2006;34:S52-S55.
104 Rice DH, Kotti G, Beninati W. Clinical review: critical care transport and austere critical care. Crit Care. 2008;12:207.