CHAPTER 91 Manipulation and Manual Methods
INTRODUCTION
Central axis pain is, perhaps, the core enigma of spine disorders. The diagnosis is one often made by exception and involving many forms of trial therapy before conclusion. Like all other sources of spine pain, the diagnosis may be confounded by the presence of other potential pain generators that have overlapping clinical and physical symptoms. Discogenic pain has variable presentation from primary, centralized aching spinal and paraspinal pain to bizarre sclerotomal pain of the lower extremities. Severity may wax and wane as patients undergo differing levels of weight-bearing load to their spine with episodes of overstrain to the disc material. Various forms of treatment from medication to spinal manipulation give relief that is temporary. Exercise may be relieving or aggravating. In a retrospective study, Smith and colleagues1 noted that 68% of patients with positive discography improved without surgery over a 4-year interval while 24% deteriorated. Some patients require more treatment to relieve their suffering than others. However, weight-bearing and activity intolerance is a consistent pattern among the various presentations of central axis pain.
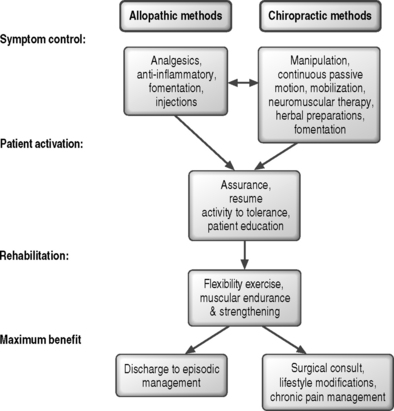
The key purposes for providing treatments (Fig. 91.1) are to relieve suffering, improve function, and maximize healing capacity. The nonoperative allopathic methods most often employ biochemical mediators to manage symptoms, followed by biomechanical interventions to modify loading of the spinal tissues to reduce local stress concentrations and strengthen core muscles while maximizing pain-free flexibility. The chiropractic methods seek to minimize or alter local physical tissue stress through the use of applied forces and moments, followed by interventions to modify behaviors that load the tissues, strengthen muscle and increase trunk stiffness, and improve pain-free flexibility. Should either approach be insufficient, a surgical consultation can be considered. The practical difference, ignoring the debates over disciplinary jargon, is the relative emphasis on the best means to reduce tissue stress, inflammation, and pain. The allopathic view relies heavily on chemical intervention to block pain and suppress inflammation followed by efforts to reduce tissue stress. The chiropractic view prefers to alter the mechanical environment, allowing inflammation and pain to subside. Patients often consult both types of care simultaneously without disclosing to either. Increasing professional interactions between the groups suggest that a meaningful number of cases may benefit from both approaches.
Spinal manipulation is a mechanically applied therapy used to relieve nociceptive pain and improve function. A number of clinical and physiological effects are known2–4 and their attributes require appropriate and skillful application to achieve safe and successful outcomes.5–9 The clinical benefit from use of these procedures has been studied10,11 in subacute and chronic back pain cases, a heterogeneous population of patients including many with central axis pain. This chapter will discuss the theoretical underpinnings of spinal manipulation and its use in the management of central axis pain.
THE BASIS OF SPINAL MANIPULATION
The lesion
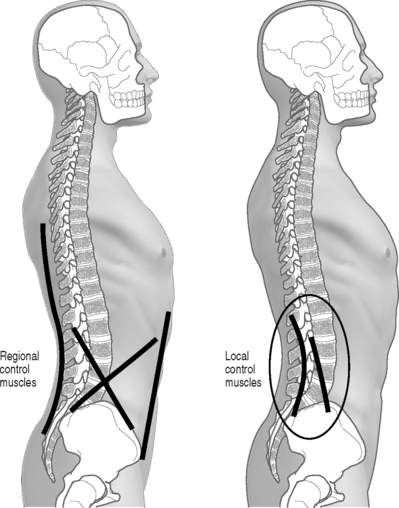
The mechanism of the manipulable spinal lesion is characterized biomechanically as a buckling event. These phenomena have been observed in orthopedics for some time among some patients with an unstable wrist carpus12,13 and are associated with multiarticular kinetic chain systems like the spine that rely on biarticular muscles for establishing local mechanical equilibrium and control. Detailed review of the biomechanics of these lesions can be found elsewhere.14–16 Briefly, buckling may involve single functional spinal units or an entire spinal region. They are caused by a mismatch in timing or amplitude of response between the local and regional muscular control systems (Fig. 91.2). A local shift of intersegmental joint configuration occurs within the bounds of normal range that is disproportionate to the task at hand. Symptoms arise from the increase in local tissue strain. The clinical presentation of the patient and the exact symptoms depend on the identity of the tissues strained to injury threshold and the presence of comorbid conditions.
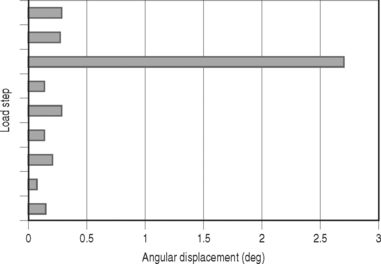
The mismatch between the demand of spinal load and appropriate local intersegmental stiffness results in a sudden shift in relative joint configuration (Fig. 91.3). That is, there is a disproportionate repositioning of the joint within the bounds of its normal functional range. Instead of supporting the patient’s posture and activity with minimum local tissue strain, the new configuration may result in a local stress concentration leading to symptoms of the involved tissue. Effectively, while the buckled equilibrium may be functional, it is with increased cost in terms of comfort. These types of buckling phenomena have now been observed under biomechanical testing conditions in vitro for isolated segments17–19 as well as the lumbar region20 and, by happenstance, during experimental studies of weight lifters when an unexpected injury occurred.16,21
The factors associated with development of local buckling are found in Table 91.1. Prior injury or degenerative disease potentiates buckling, allowing it to occur more easily, effectively lowering the critical load requirements and reducing the ultimate load capacity. Fig. 91.4 describes the chain of events leading to symptoms.
Table 91.1 Etiologic factors for local joint buckling events based on available biomechanical experiments in vitro and in vivo15,16
| Causative | Facilitating |
|---|---|
| Sudden incremental load after prolonged static posture | Vibrating environments |
| Unexpected load | Disc damage |
| Rapid load events (500 lb/sec) | |
| Uncoordinated/fatigued effort |
Diagnostic findings
The determination of a manipulable lesion in isolation is relatively straightforward but is made more complicated by the presence of other pathology. Table 91.2 provides a review of findings warranting a trial of spinal manipulation. Unraveling symptoms that may respond to manipulative methods, however, is easily achieved through a trial therapy interval. Provocative testing can be used to identify the specific directions of loading that give comfort and relieve symptoms. Such maneuvers guide the selection of treatment procedures that match patient needs. These maneuvers apply controlled forces and moments, often involving postural positioning or tasks, to the suspected dysfunctional joint. Based on knowledge of any comorbid pathoanatomical diagnosis and associated findings (palpation sensitivity, flexibility, orthopedic/neurologic testing and imaging/laboratory test results), initial trials of provocation are performed in an effort to reduce local tissues stress. The principal governing diagnostic interpretation is the partitioning of patient response to applied loads into categories of those that relieve or those that aggravate symptoms. Results that reduce symptoms and any referred or radicular pain components are the desired motions for directing the choice of procedure and the application of manipulative methods. Joint or nerve blocks may be helpful in identifying the pain generator (facet, sacroiliac, or nerve root) and quelling local inflammatory responses that may be interfering with patient recovery.
Table 91.2 Signs and symptoms of the isolated manipulable lesion
| Local back pain with or without limb pain absent progressive neural signs |
| Focal sensitivity to manual pressure |
| Local muscular hypertonicity with or without tender points |
| Limited joint compliance in mid-range position and/or end-range limitations with pain on overpressure testing |
| Reproduction of symptoms with joint compliance or end-range motion testing |
| Local soft tissue edema |
| Altered local skin turgor, temperature or color |
Manipulation skill and control factors
Manipulation, like all other therapy, must be performed using sufficient skill and knowledge. Applications include the ability to use thrusting and nonthrusting techniques where appropriate, which requires an in-depth clinical assessment and differential diagnosis.22 Used in trained hands, these methods are remarkably safe.23–25 Evidence shows that minimally skilled individuals are ineffective in producing good outcomes6 with recovery from a symptomatic episode. Efforts to extend one’s practice into the field of manipulation based on superficial weekend training programs may be pedagogically wrong and potentially dangerous.26,27
Threshold is defined as the application of necessary and sufficient joint load to effect a change in its behavior and symptoms. Threshold levels are a function of patient joint stiffness, soft tissue viscoelastic properties, and muscular tension that may vary themselves, based on age, severity or acuteness of symptoms, and patient anxiety levels. Assessment of tissue condition to guide application of the procedures is a skill developed through supervised practice and experience. In cases where there are multiple tissue elements involved (e.g. reactive muscle tension, capsular swelling, adhesions, hemorrhage), sequential procedures may be necessary. Staged procedures can speed the removal of local fluid or breakdown interstitial adhesions without exceeding patient tolerance for more severely injured or sensitive tissues. Choice of treatment modality is dependent on the presence or absence of pain during the examination (provocation testing). Empirically, patients with localized pain seem to respond better to impulse loads as long as the preliminary joint positioning can be engaged without difficulty.22 Patients who are unable to be effectively positioned or have chronic or referred pain may initially benefit more rapidly using procedures without impulse.
Effective dosage and duration of therapy varies with patient cooperation on reducing aggravating factors, performing recommended exercises to gain stability, the presence of other pathology or degenerative change, and condition severity. In general practice, initial treatment dosage is 2–3 sessions per week. Haas et al.28 have shown a direct relationship between treatment frequency and outcome scores for pain and disability for patients with chronic low back pain. A statistically significant linear relationship noted greater improvement for patients treated 3–4 times per week over a 3-week period. Across the literature, the average number of treatment sessions to maximum improvement for uncomplicated cases ranges from 8 to 18 with a range of approximately 1–40 treatments, depending on complexity and complications.29,30
TREATMENT METHODS
Manual therapy concerns itself with the treatment of functional disturbances of muscle and joints including their local or remote symptoms. There are a number of ways in which manual therapy has been divided for discussion. Manipulation is a specific form of manual method that uses rapid impulse loads to the body structures. Manipulation can be quantitatively differentiated from other methods on the basis of speed of application14 and the differing response of the body tissues to rapid loading. While many systems of manual treatment methods exist, including manipulation, the common factor is the controlled application of loads (forces and moments) to the spine. The various approaches may be most easily understood when broken down into their biomechanical control parameters. Such classifications also help to align treatment objectives to therapeutic goals. That is, the body’s biomechanical response to load application will depend on tissue properties and their reserve viscoelastic and stiffness characteristics. The various procedures span a spectrum of force and moment amplitude, speed, and direction of application that are designed to influence joint and disc strain and normalize mobility.
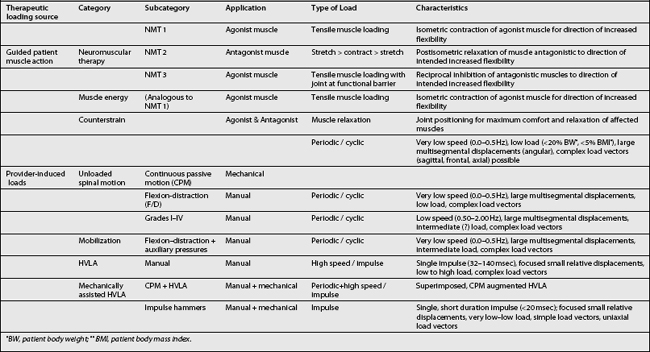
The therapeutic loads can arise from two primary sources. They are generated either by action of the treating physician or from patient muscle action (stretching, relaxing, or contracting) under the guidance of the provider. Depending on the clinical discipline base (chiropractic, osteopathy, or manipulative medicine) of the provider administering these procedures, the specific name will vary (Table 91.3). Guided patient muscle action may be termed neuromuscular therapy, muscle energy, or counterstrain maneuvers. Provider-induced motions are typically characterized by repetition rate, speed, and amplitude and fall under the terms manipulation or adjustment and mobilization. Finally, various assistive devices that may be used to control the patient motion direction, rate, and amplitude are termed mechanically assisted procedures. These latter may be coupled with manipulation methods to provide motion assisted manipulation procedures.
Guided patient muscle activation
Neuromuscular therapy (NMT) utilizes direct muscle action as well as associated neuromuscular reflex mechanisms to improve mobility and normalize muscle tone. Its action is based on the principle that inhibited or weakened agonists or competition of hypertonic antagonists may limit joint function. For example, spinal motion of rotation may be limited by inhibited contralateral transversospinal groups or by shortened ipsilateral transversospinal muscles. The pattern is determined by provoking local joint motion and determining its relative compliance in a direction and contrasting that with the presence of muscle tenderness and relative hypertonicity.22 There are three types of NMT, their use being dependent on whether the desired effect is to relax hypertonic agonists or strengthen them or to relax hypertonic antagonists as noted below.
NMT1: Agonist muscle considered weakened or hypotonic.
NMT2: Postisometric relaxation of shortened, tonic antagonists muscles
NMT3: Mobilization using reciprocal inhibition of the antagonists
Whereas the action of NMT procedures is directed in altering joint mobility through muscle action (stretching, relaxation, and isometric tensing), the mechanism of muscle energy and counterstrain is believed to be more associated with the effects of direct alteration of muscle tone. As noted by Murphy31 the restoration of joint functional range and normal muscle tone arises from several hypothesized benefits. They include relaxing hypertonic muscle to decrease oxygen demand and local pain, increasing circulation to the area to wash out metabolic waste products, and promoting greater venous and lymphatic drainage to reduce edema.
Provider-induced loading
Loads applied by the treating doctor to the patient’s spine are controlled in terms of their speed, amplitude, displacement, frequency, duration, and direction. They may be induced manually, through use of instrumented treatment tables and devices, or a combination of both. The procedures fall into categories of continuous passive spinal motion (CPM); mobilization; high-velocity, low-amplitude (HVLA) thrusting techniques, and mechanically assisted procedures (see Table 91.3).
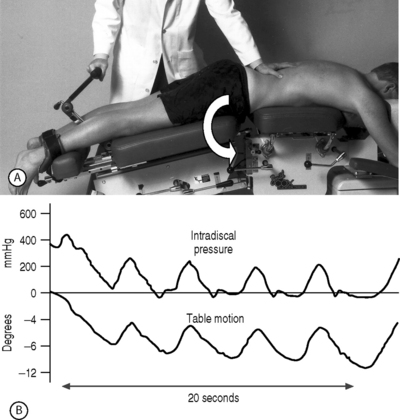
Slow, externally applied procedures such as continuous passive motion (CPM), mobilization methods, and flexion distraction techniques result in decreasing internal disc pressures,32 as shown in Figure 91.5. Other benefits include the dispersion of local edema,15,33 prevention or disruption of joint adhesions and stimulation of connective tissue healing34–36 within functional limits. The slow, cycled motions influence time-dependent viscoelastic characteristics within the affected tissues, shifting fluid between various body compartments.
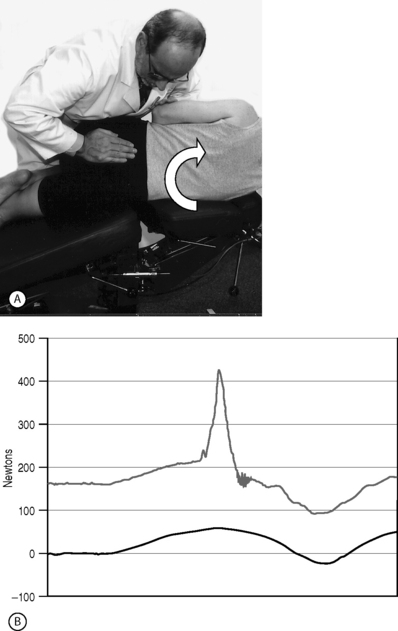
Pulsed procedures include high-velocity, low-amplitude (HVLA) methods that impart a rapid thrust to the body segments bounding the joint of interest and transmitting forces and moments through the vertebral disc and surrounding structures. These methods tend to more quickly influence relative functional restrictions in vertebral motion and local tissue strains. In general, where a patient can be comfortably positioned for these procedures, they are considered by some to be more effective in achieving a more quick clinical change in the patient’s condition.22
Formal training in HVLA methods requires intense rehearsal of a series of procedures for each region of the spine. The names of the procedures, once again, may vary based on the discipline in which the doctor has been trained. Once familiar with the basic procedures, skilled providers can frequently modify procedures to meet individual clinical needs under unusual and novel circumstances to provide safe and effective treatment. With the exception of the contraindications noted in Table 91.7 (below), the presence of local pathology or prior surgical intervention is not a contraindication to use of manipulative methods. The skilled provider can modify procedures to accommodate the pathology or can elect nonpulsing methods as may be appropriate.
Table 91.7 Relative and absolute contraindications to spinal manipulation with examples of exceptions
| Contraindications | Exceptions |
|---|---|
| Undiagnosed progressive neurologic deficit | None |
| Undiagnosed loss of bowel or bladder control | None |
| Cauda equina syndrome | None |
| Procedures incompatible with the direction of unstable motion | None |
| Bone weakening disorders | Sites distant to the pathologic site may undergo manipulation if appropriate |
| Primary or metastatic tumor | Sites distant to the pathologic site may undergo manipulation if appropriate |
| Acute fracture | Stable compression fracture of the anterior column |
| Bleeding disorder | Unloaded motion procedures may be used avoiding extremes of motion |
| Acute inflammatory rheumatoid disease or septic joints. | None |
Procedure modifications include the selection from the various procedural options, adaptation of applied forces, moments and motions, as well as variation of patient postures. Triano and Schultz7 demonstrated effectively that the specific load components acting on the spine can be increased or decreased accordingly through strategies that combine these factors. For the most common system of manipulation used by chiropractors, the diversified method, there are as many as 45 different approaches to the lumbar spine, 17 to the thoracic, and 25 to the cervical region. Patients with disc protrusion that is aggravated by extension maneuvers may receive manipulative treatment by minimizing extension moments. In like manner, desired directions that relieve may be accentuated as necessary.
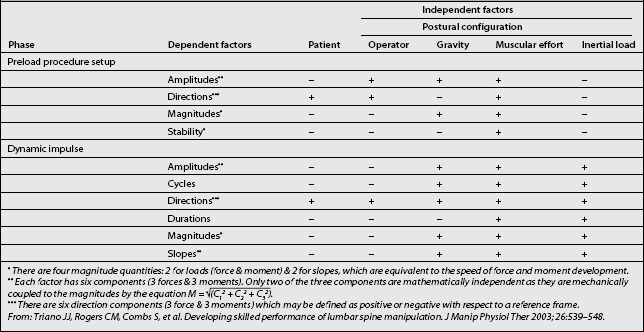
Adaptation of forces and moments applied by provider-induced loading requires the adjustment of control factors (Table 91.4) enhancing or diminishing specific load components in order to accommodate stature, comorbid pathology, or postoperative changes.37 Control strategies fall into two categories. Patient factors include postural positioning to open or close the articulations of the target segments. Once positioned, the loads may be applied using static prepositioning or with dynamic oscillation manually or through therapeutic tables that mechanically assist. The acceleration of the patient’s body segments induces inertial loads within the target joints that will either add to or subtract from the provider-induced loads. The operator may elect to further modify the application point, force and moment amplitudes, directions, rate, and duration.
Table 91.4 Control strategies for provider-induced loading manual methods
| Patient-based factors | Provider-based factors |
|---|---|
| Patient posture | Preload amplitude |
| Initial conditions | Load direction |
| Static posture | Load peak amplitude |
| Dynamic motion | Load impulse rate |
| Mobilization | Load duration |
| Mechanically assisted | Transient pulse |
| Sustained |
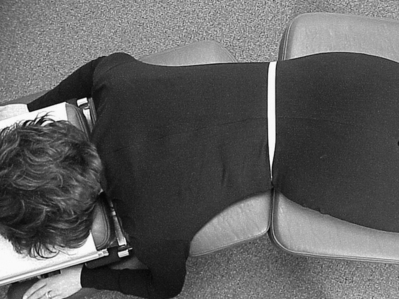
Figures 91.6A-D demonstrate examples of differing control strategies based on patient positioning. The resulting changes in loads transmitted through the targeted lumbar spine were reported by Triano and Schultz7 and are shown in Table 91.5. In Fig. 91.6A, treatment to the lumbosacral spine is delivered with a combination of muscular effort through the arm and use of upper body mass to generate the applied loads. The patient has been positioned without any lateral bend or twisting of the torso. This strategy will create, within the targeted level, a relatively low flexion moment while boosting the tendency for lateral shear and lateral bending. Fig. 91.6B modifies the initial position by inducing a prepositioning of lumbar flexion and left axial rotation. Under these conditions, the patient’s left intervertebral foramen and zygapophyseal joint will be maximally opened during the impulse delivery.

Fig. 91.6 (A) Treatment applied to the lumbosacral segments using a patient positioning strategy to provide low flexion moment and higher lateral shear and lateral bending. See the text for details. (B) Positioning to maximally open the left intervertebral foramen and zygapophyseal joint by adding torso flexion and left axial rotation to the procedure shown in Fig. 91.6A. (C) A pelvic procedure applied through the ischial tuberosity may be used to treat the sacroiliac joint or to modify loads acting on the lumbosacral spine by enhancing flexion moment, limiting anterior shear. (D) Long-lever procedures apply operator body mass differently than those in Figs 91.6A-C. Body mass is applied here through the contact between the provider’s hip and the patient’s flexed thigh.
Table 91.5 Manipulation load components organized by hierarchy in producing individual load components7
| Loading action at the lumbosacral segments | Hierarchy of effectiveness (procedure + initial patient position yields load amplitude) |
|---|---|
| Flexion | MPar = HIar >LLar >LLur = MPur > HIur |
| Rotation | LLar = MPar > HIar |
| Lateral bending | HIur > MPur >LLur = HIar > MPar > LLar |
| Lateral shear | HIur > MPur = HIar >LLur > MPar > LLar |
| Axial compression | HIar > MPar > LLar |
| Anterior shear | MPar > MPur >LLur = LLar > HIar > HIur |
Procedures: MP, mammillary push procedure; HI, hypothenar ischium; LL, long lever. Patient positioning: ar, axially rotated; ur, unrotated.
Fig. 91.6C uses the same patient positioning as in Fig. 91.6B but a different loading application point. This procedure, originally conceived as treatment of the sacroiliac joint, accentuates flexion moments at the lumbosacral region while providing relatively little anterior shear and a moderate level of additional lateral bending or rotation component.
Finally, Fig. 91.6D demonstrates the use of a long-lever maneuver that alters how the provider uses his/her body mass to affect loading of the spine. Here, the application of load to the lumbosacral segments is derived through arm action as before but with pressure from the hip acting through the patient’s flexed femur. This strategy will accentuate spinal axial rotation, depending on the degree of patient prepositioning, while moderating or minimizing all other components.
While knowledge of the control strategies is helpful, their application comes from understanding of manipulation dynamics and how the loads are developed. The total load acting on the target joint is the sum of the applied forces and moments with the inertial forces and moments derived from the motions induced by the patient’s body segment masses. A third factor is the relative muscular activity surrounding the joint which can attenuate the loads transmitted, acting either as dampers if tight during the delivery of the procedure or as an after-load if contracting in response. Table 91.6 relates the characteristics of the loads themselves as dependent factors to the parameters that influence them as independent factors. For the purposes here, intrinsic muscle action is assumed as an insignificant value, an ideal sought by each provider through various relaxation techniques.
Motion-assisted methods are also available that couple CPM and HVLA methods (Fig. 91.7), taking advantage of momentum to either amplify or diminish the amplitude of loads passing through the targeted joint system while preserving the speed effects.
Therapeutic joint loading may also be accomplished through the directed application of patient positioning and internal muscular action. Termed neuromuscular therapy (NMT) in European medical circles,22 or divided into categories of muscle energy and counterstrain techniques in North American osteopathic practice, these methods focus patient effort to assist in resolving local tissues strains.
DIAGNOSTIC INDEPENDENCE OF MANIPULATION
Significant cross-discipline confusion exists regarding the issue of pathoanatomical diagnosis. The disarray of thought revolves around two factors. First is the failure of the medical model to adequately predict treatment outcomes as a function of pathoanatomical diagnosis.38 The second is the continuing inability to quantitatively measure the manipulable lesion (buckling event) in a clinical setting. Spine dysfunction and disease is a continuum of interrelated severity and stages that may arrest with local healing or progress based on many extrinsic and intrinsic variables. Despite the occasional clarion calls for a ‘specific diagnosis’ to drive selection of treatment for a predictable outcome, widespread evidence shows that only the extremes of some pathology reach that level of predictability. For the remainder, significant proportions of the population have abnormal structure on X-ray or advanced imaging that is clinically silent. Others with no identifiable abnormality suffer serious activity limitation because of pain. Likewise, patients with asymptomatic pathoanatomy may become symptomatic under given circumstances. These factors were discussed under the section on the evidence of buckling as the mechanism of the spinal lesion. Both those with pathoanatomy and those without are included among those patients who may benefit from use of manipulation methods in their care.
The objective of altering local tissue strains, then, forces the doctor to view diagnosis differently. It is less from a classical perspective and more as a means of anticipating necessary modifications. For example, presence of degenerative spondylosis or a disc bulge narrowing the lateral recess will cause the provider to identify patient positioning for delivery of the treatment that will facilitate a maximum volume of the canal and recess. Similarly, patients with radicular syndrome must be positioned and treated using methods that decompress the offended nerve and are generally identified by those postures that are relieving rather than provoking of discomfort. Only those patients with distinct contraindications cannot undergo a trial of manipulation.
TREATMENT EFFECTIVENESS
As in all other forms of treatment, the Hawthorne or placebo effect plays a role in treatment outcome. In numerous studies, chiropractic patients record greater satisfaction with their treatment experience than when they are attended by other providers,39,40 an observation often triggering the assumption of placebo as the sole operational mechanism. At least two controlled clinical trials have addressed the question of placebo effect directly.41,42 In both studies, all treatment groups showed improvement over time. However, the patients receiving thrusting procedures demonstrated significantly greater and more rapid rates of improvement from their symptoms and in their ability to function than in the control group. While physician attention, in any form, appears to benefit patients with back pain, the data also shows that, at least for thrusting techniques of manipulation, there is a treatment-specific advantage beyond the non-specific effects.
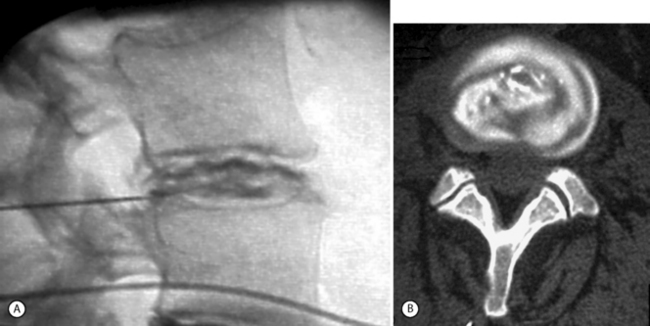
Review and best evidence synthesis of the English and Northern European literature on randomized trials by Bronfort and colleagues11 summarizes the information on utility of manipulation methods in contrast to sham and alternate treatments. For acute episodes, there is moderate evidence that HVLA provides more short-term pain relief than mobilization methods and detuned diathermy, and limited evidence of faster recovery than a commonly used physical therapy treatment strategy. For patients with more chronic pain, HVLA has an effect similar to11 or better than10 use of nonsteroidal antiinflammatory medication. It is effective in the short term when compared with placebo and general practitioner care, and in the long term compared to physical therapy. There is limited evidence that HVLA is superior to chemonucleolysis for disc herniation in the short term. Triano et al.,43 in a small sample of patients, showed evidence that painful internal disc derangement on CT discography will respond with symptom reduction using HVLA procedures.
In a trial contrasting the effects of medication management versus manipulation, Giles and Muller10 showed that the highest proportion of early suppression of symptoms was found for manipulation at 27.3% with medication achieving 5%. In those not reaching asymptomatic status, manipulation achieved the best overall results as reported by pain scales, Oswestry scores, and range of motion. However, the data do not strongly support the use of only manipulation or only nonsteroidal antiinflammatory medication for the treatment of chronic spinal pain.10 As evidenced by patients who often elect to consult medical providers and chiropractors simultaneously without informing either, there appears to be a synergistic effect from both.
CASE EXAMPLES
Fig. 91.8 shows the discogram of a 36-year-old female patient with chronic low back pain onset following a heavy lifting incident 6 months earlier. Medical management and physical therapy procedures had failed. An intradiscal electrothermal therapy procedure was attempted following discography, yielding 2 months of pain relief. With renewed symptoms, she became increasingly weight-bearing and activity intolerant with low back and pseudoradicular leg pain. Her range of motion, particularly in flexion, was limited to 30 degrees. The spinous processes of L4 and L5 were tender and there was significant muscle tone asymmetry in the paraspinal group and quadratus lumborum. Efforts to test midrange joint compliance reproduced pain when extension, right bending, or axial rotation provocation was attempted.
The patient was initially treated with in-office prone CPM in flexion with left lateral bending (Fig. 91.9) followed by left lateral decubitus position using left lateral bending CPM coupled with flexion (Fig. 91.10). As CPM methods helped reduce immediate discomfort, motion-assisted HVLA was applied with the patient in left lateral decubitus posture with CPM in right lateral bending. Home exercise focused on flexibility in range of motion and spine stabilizing exercises. She experienced good relief of symptoms and a gradual return to normal activities of daily living over a period of 7 weeks. The patient remained sensitive to heavy lifting, push–pull tasks, and sudden or awkward trunk postures. Over a 3-year period, she has experienced decreasing frequency of episodes at 1–2 per year requiring 1–2 weeks of treatment.
SAFETY AND CONTRAINDICATIONS
No discussion of the use of spinal manipulation would be complete without addressing the issue of safety. Rare reports of adverse effects from spinal manipulation to the lumbar spine have been recorded.24 Based on the rate of utilization for these procedures in the reported literature, the incidence of serious complication is negligible (<1:107). Cauda equina syndrome is the most serious adverse event suspected to follow spinal manipulation, with less than 30 cases reported since the early twentieth century. The proposed mechanism of injury is hypothesized to be the spinal manipulative loads applied to an already significantly compromised disc. Presence of undiagnosed neurologic deficit or the appearance of progressive deficit should result in immediate cessation of treatment and further diagnostic work-up.
The contraindications to manipulation are based on the pathomechanics of specific conditions rather than an extensive epidemiological database. Table 91.7 lists the relative and absolute contraindications.
1 Smith SE, Darden BV, Rhyne AL, et al. Outcome of unoperated discogram-positive low back pain. Spine. 1996;21:1394-1395.
2 Herzog W. The mechanical, neuromuscular and physiologic effects produced by the spinal manipulation. In: Herzog W, editor. Clinical biomechanics of spinal manipulation. New York: Churchill Livingstone; 2000:191-207.
3 Pickar JG. Neurophysiological effects of spinal manipulation [review] [127 refs]. Spine Journal: Official Journal of the North American Spine Society. 2002;2:357-371.
4 Pickar JG, Sung PS, Kang Y. The effect of a spinal manipulation’s impulse speed on l0w-threshold mechanoreceptors in lumbar paraspinal muscles. J Chiro Educat. 2004;18:25-26.
5 Cohen E, Triano JJ, Mcgregor M, et al. Biomechanical performance of spinal manipulation therapy by newly trained vs. practicing providers: does experience transfer to unfamiliar procedures? J Manip Physiol Ther. 1995;18:347-352.
6 Curtis P, Carey T, Evans P, et al. Training primary care physicians to give limited manual therapy for low back pain: patient outcomes. Spine. 2000;22:2954-2959.
7 Triano J, Schultz AB. Loads transmitted during lumbosacral spinal manipulative therapy. Spine. 1997;22:1955-1964.
8 Triano JJ, Bougie JD, Rogers CM, et al. Procedural skills in spinal manipulation: does preparation matter? Spine. 2003. In submission
9 Triano JJ, Rogers CM, Combs SB, et al. Quantitative feedback vs. standard training for cervical and thoracic manipulation. J Manip Physiol Ther. 2003;26:131-138.
10 Giles LG, Muller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation [see comment]. J Manip Physiol Ther. 1999;22:376-381.
11 Bronfort G, Haas M, Evans RL, et al. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4:335-336.
12 Landsmeer JMF. Studies in the anatomy of articulation. I: the equilibrium of the ‘intercalated’ bone. Acta Morphol Neerl Scand. 1961;3:287-321.
13 Landsmeer JMF. Atlas of the anatomy of the hand. New York: Churchill Livingstone, 1976.
14 Triano J. The mechanics of spinal manipulation. In: Herzog W, editor. Clinical biomechanics of spinal manipulation. New York: Churchill Livingstone; 2000:92-190.
15 Triano J. Biomechanics of spinal manipulation. Spine. 2001;1:121-130.
16 McGill SM. Low back disorders. Human Kinetics. 2002.
17 Wilder DG, Pope MH, Seroussi RE, et al. The balance point of the intervertebral motion segment: an experimental study. Bull Hosp Jt Dis Orthop Inst. 1989;49:155-169.
18 Wilder DG, Pope MH, Magnusson M. Mechanical stress reduction during seated jolt/vibration exposure. Semin Perinatol. 1996;20:54-60.
19 Ogon M, Bender BR, Hooper DM, et al. A dynamic approach to spinal instability. Part II: hesitation and giving-way during interspinal motion. Spine. 1997;22:2859-2866.
20 Crisco JJIII, Panjabi MM, Yamamoto I, et al. Euler stability of the human ligamentous lumbar spine. Part II: experiment. Clin Biomech. 1992;7:27-32.
21 Cholewicki J, Mcgill SM, Norman RW. Lumbar spine load during the lifting of extremely heavy weights. Med Sci Sports Exer. 1991;23:1179-1181.
22 Schneider W, Dvorak J, Dvorak V, et al. Manual medicine therapy. New York: Theime Medical Publishers, 1988.
23 Haldeman S, Rubinstein SM. Compression fractures in patients undergoing spinal manipulative therapy. J Manip Physiol Ther. 1992;15:44-48.
24 Haldeman S, Rubinstein SM. Cauda equina syndrome in patients undergoing manipulation of the lumbar spine. Spine. 1992;17:1469-1473.
25 Haldeman S, Rubinstein SM. The precipitation or aggravation of musculoskeletal pain in patients receiving spinal manipulative therapy. J Manip Physiol Ther. 1993;16:47-50.
26 Triano JJ, Bougie J, Rogers C, et al. Procedural skills in spinal manipulation: do prerequisites matter? Spine J. 2004;4:557-566.
27 Schneider G. Manual therapy techniques for the cervical spine require special skills. (Comment on Refshauge et al., Austr J Physiother 48:171–179) [comment]. Austr J Physiother. 2002;48:314.
28 Haas M, Groupp E, Kraemer DF. Dose–response for chiropractic care of chronic low back pain. Spine. 2004;4:574-583.
29 Triano JJ, Hondras M, McGregor M. Differences in treatment history with manipulation for acute, subacute, chronic and recurrent spine pain. J Manip Physiol Ther. 1992;15:24-30.
30 Haldeman S, Chapman-Smith D, Peterson DH. Guidelines for chiropractic quality assurance and practice parameters. Gaithersburg, MD: Aspen Publishers, 1993;1-216.
31 Murphey T. Myofascial Techniques. In: DiGiovanna EL, Schiowitz S, editors. An osteopathic approach to diagnosis and treatment. Philadelphia: JB Lippincott, 1991.
32 Gudavalli MR, Cox JM, Baker JA, et al. Intervertebral disc pressure changes during the flexion-distraction procedure for low back pain. ISSLS. 1997:165-166.
33 Triano J. Manipulative therapy in the management of pain. In: Tollison CD, Satterthwaite JR, Tollison JW, editors. Clinical pain management: a practical approach. 3rd edn. Philadelphia: Lippincott, Williams & Wilkins; 2002:109-119.
34 O’Driscoll SW, Kumar A, Salter RB. The effect of the volume of effusion, joint position and continuous passive motion on intraarticular pressure in the rabbit knee. J Rheumatol. 1983;10:360-363.
35 Salter RB. The biologic concept of continuous passive motion of synovial joints. The first 18 years of basic research and its clinical application. Clin Orthop. 1989;242:12-25.
36 Kim HK, Kerr RG, Cruz TF, et al. Effects of continuous passive motion and immobilization on synovitis and cartilage degradation in anigen induced arthritis. J Rheumatol. 1995;22:1714-1721.
37 Triano J. Managing geriatric spine patients. In: Bougie J, Morganthal P, editors. The aging body. New York: McGraw Hill, 2001.
38 Haldeman S. Presidential address, North American Spine Society: Failure of the pathology model to predict back pain. Spine. 1990;15:718-724.
39 Cherkin D, Hart LG, Rosenblatt RA. Patient satisfaction with family physicians and general internists: is there a difference? J Fam Pract. 1988;26:543-551.
40 Carey TS, Garrett J, Jackman A. The outcomes and costs of care for acute low back pain among patients seen by primary care practitioners chiropractors, and orthopedic surgeons. N Engl J Med. 1995;333:913-917.
41 Hadler NM, Curtis P, Gillings A. Benefit of spinal manipulation as adjunctive therapy for acute low back pain: a stratified controlled trial. Spine. 1987;12:703-706.
42 Triano JJ, McGregor M, Hondras MA, et al. Manipulative therapy versus education programs in chronic low back pain. Spine. 1995;20:948-955.
43 Triano J, Vanharanta H, McGregor M. Manipulation for painful disc syndrome. Washington, DC: NASS, 1995.
44 Triano JJ, Rogers CM, Combs S, et al. Developing skilled performance of lumbar spine manipulation. J Manip Physiol Ther. 2003;26:539-548.
45 Bergmark A. Mechanical stability of the human lumbar spine. 1–85. 1987. Lund University, Department of Sold Mechanics. Ref Type: Thesis/Dissertation.