13. Manipulation
Alan Breen
Chapter contents
Introduction255
What is manipulation?256
The manipulation ‘package of care’264
Researching clinical effectiveness266
Research and access to manipulation in the UK269
Manipulation and the transition to mainstream health care270
Conclusion270
Introduction
Manipulation is a mechanical treatment that has often been recommended in national evidence-based guidelines for common musculoskeletal disorders (Agency for Health Care Policy Research, 1994, Waddell et al., 1999, (NHMRC) NHaMRC, 2003, Airaksinen et al., 2006, van Tulder et al., 2006, Haldeman et al., 2008 and NICE, 2008). Such is the volume of evidence for its clinical value that it may be reasonable to ask why it is still sometimes regarded as a complementary therapy. However, part of the reason for this probably lies in gaps in the research literature in relation to its role in care. Firstly, manipulative treatment implies a rationale that links a reduction of mechanical dysfunction to improvement in health, but the relevance of mechanical dysfunction models in health remains unclear in the research literature. Secondly, manipulation is not generally practised as a monotherapy, because practitioners usually provide other interventions along with it (Burton, 1981, Huisman and Breen, 1990, Pedersen, 1994, Wilson, 2003 and Chown et al., 2008). The effects of manipulation cannot therefore be the only factors in play. This requires us to consider those of the other interventions that may often accompany it (Harvey et al. 2003). Research in this context is relatively new.
The third reason relates to its provision in health care. Manipulation and the other components of the care that surrounds it take a long time to learn if they are to be practised competently. This makes it difficult, if not impossible, to incorporate manipulation into undergraduate medical training. More importantly, the musculoskeletal conditions for which it is mainly used do not fit well into a purely biomedical model of health, even though they do constitute a huge societal cost to industrialized nations (World Health Organization 2001). Instead, they also usually call for a functional approach. Because the health, social and societal costs of musculoskeletal disorders are generally considered separately, their real impact on the gross domestic product of western countries is seldom fully appreciated. Public resources for their care are generally given relatively low priority compared to, for example, cancer and heart disease. Sufferers are also sometimes denigrated as the ‘walking wounded’ and their practitioners regarded as somewhat marginal (Coulter & Shekelle 2005).
The scope for gaining useful knowledge around this topic through research is therefore very wide and ranges from the most intrinsic to the most global of health issues. This chapter will attempt to provide an overview of these.
What is manipulation?
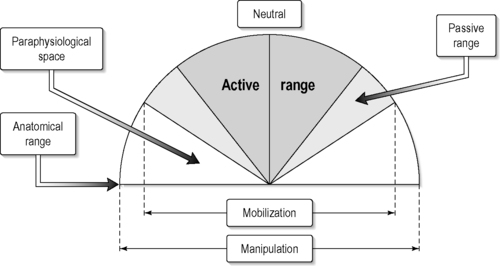
Manipulation is most commonly defined as: ‘a small amplitude, high velocity movement at the limit of joint range taking the joint beyond its passive range of movement, without exceeding its anatomical integrity’ (Sandoz 1969; Figure 13.1). This is therapeutically different from mobilization, which is a repetitive passive movement (i.e. within the passive range) (Harvey et al. 2003) (Figure 13.2). Manipulation is sometimes accompanied by an audible pop, or cavitation (Unsworth et al. 1971). However it has been argued that this is not necessary to qualify as a successful procedure (Flynn et al. 2003). Apparently, when it does occur, it may also come from multiple surrounding joints (Ross et al. 2004). The possible effects of cavitation manipulation on the mechanics of joints have been extensively discussed (Evans, 2002 and Breen et al., 2007), but useful experimental studies in living subjects are difficult to perform (Reeves et al. 2007).
 |
| FIGURE 13.1 |
The mechanical dysfunction model
Until relatively recently, the mechanical dysfunction model of health was portrayed as an alternative paradigm, propounded by heterodox practitioners who offered it for all manner of conditions (Hewitt & Wood 1975). However, we now know that such care is used by the public more to complement conventional practice than to replace it (Eisenberg et al., 1993 and Thomas et al., 2001), mainly for common musculoskeletal complaints and especially for low-back pain (Breen, 1977, Burton, 1981 and Pedersen, 1994). Trial evidence reviews have shown that spinal manipulation, which depends on such a model, has moderately positive effects for low-back pain (Assendelft et al. 2004). The problem is that this evidence is not consistent, which tempts a certain amount of selective reporting by reviewers. It also reflects the heterogeneity of the samples, interventions, trial designs and outcome measures. Nonetheless, its recommendation as a treatment in most back pain guidelines (European Commission CBMC, 2006, Chou and Huffman, 2007 and Hurwitz et al., 2008) is on the basis of reducing pain and disability in people who are not recovering spontaneously from acute back pain (van Tulder et al. 2006) or are suffering exacerbations of chronic back pain (Airaksinen et al. 2006). More research has been called for to identify the kinds of patients who will benefit most from manipulation (van Tulder et al. 2006).
The establishment of subgroups
One approach to identifying subgroups has been to develop and test prediction rules based on accessible clinical findings (Childs et al. 2004). For example, patients with recent-onset back pain, without leg pain, are thought to respond better to manipulation than those with longer-duration pain which radiates down the leg. However, these rules are said to require further validation (Hancock et al. 2008). In the meantime, the accepted model of care for people who are not recovering, once serious pathology has been excluded, is to adopt a psychosocial and general physical fitness approach (Waddell 1998). Despite reasonable rationales for a relationship between biomechanics and spinal pain, therefore, we lack scientific explanation of how manipulation confers benefit. Furthermore biomechanical measures themselves are seldom recommended for use for assessing outcomes (Pincus et al. 2008a).
How then could manipulation contribute to reduction in pain and disability for such conditions? It is common to refer to laboratory studies of cadaveric spines (White & Panjabi 1990) to try to understand how mechanical interventions reduce spinal pain and disability. These studies have shown, for example, that during trunk movement, stiff segments transfer mechanical stress to adjacent ones, causing abnormal force concentrations there (Bowden et al. 2008). Motion segments that become lax may repeatedly tug at their attachments during unguarded movements. It makes sense to think that this could result in pain and a variety of other neuromuscular effects (Panjabi, 1992a, Panjabi, 1992b and Panjabi et al., 1992). It is not difficult to imagine how spinal manipulation could influence this, but there is no good clinical evidence that it happens in patients and is related to pain.
How do we investigate the mechanical dysfunction model?
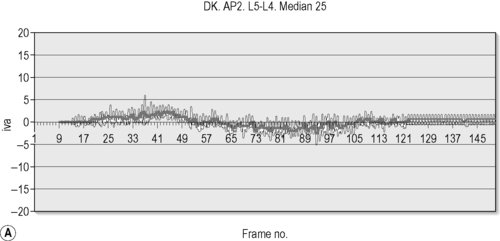
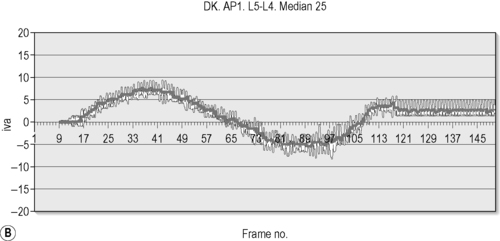
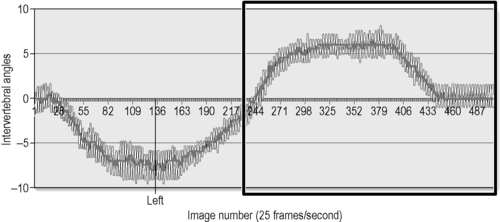
Part of the rationale for manipulation is to increase intervertebral motion and reduce painful deformation of intervertebral discs and ligaments (Haldeman 1996). For example, there is some evidence that manipulation may increase overall range in the cervical spine (Nansel et al., 1989, Cassidy et al., 1992 and Nilsson et al., 1996). However, increasing range of motion has not been confirmed as being associated with reduced disability or pain (Nattrass et al. 1999) and evidence that the manipulation of spinal segments actually does increase their range is rare. This is largely due to poor reliability in the measurement of intervertebral motion from the end-of-range radiographs that are traditionally used for this (Shaffer et al., 1990, Panjabi et al., 1992 and Mayer et al., 1995). The field of spine stabilization surgery suffers from similar problems (Reeves et al. 2007) and we have long needed an objective and reliable way of measuring spine kinematics in living subjects. However, this is gradually becoming possible using quantitative fluoroscopy, which is a combination of digital fluoroscopy and image processing (Teyhen et al., 2005, Breen et al., 2006 and Wong et al., 2006) where hundreds of digital X-ray images are recorded as the patient is moved and the motions of the vertebrae are tracked and recorded using computer programs (Figure 13.3). A graphical example of increased range of motion following lumbar manipulation is shown using this technology in Figure 13.4.
 |
| FIGURE 13.3 |
These quantitative fluoroscopic studies have the potential to reveal what previously only cadaveric studies could show. Since most back and neck pain is not associated with either serious pathology or nerve compression, subgrouping of ‘non-specific’ spinal pain is essential and some of these subgroups may be mechanical ones.
‘Instability’
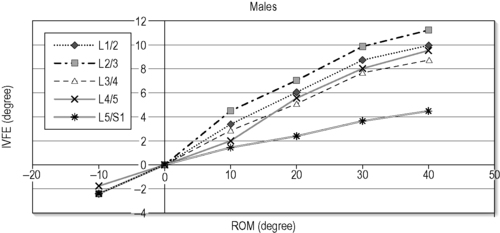
Perhaps the most popular model of pain-producing mechanical dysfunction of the spine is segmental ‘instability’, which until recently has only been quantifiable in specimens (Reeves et al. 2007). The term ‘instability’ is probably inappropriate in relation to non-traumatic mechanical spinal disorders and investigators have traditionally used alternatives such as ‘hypermobility’ (Van Akkerveeken et al. 1979) and ‘laxity’ (Fernandez-Bermego et al. 1993). However, given the wide variation of the normal range of intervertebral motion, ‘hypermobility’, taken as increased range alone, would be difficult to associate with pain. Laxity, however, may be another matter. A lax joint does not necessarily move too far under normal physiological stresses – it moves too fast. This distinction is embedded in Panjabi’s ‘neutral zone’ theory (Panjabi, 1992a and Panjabi, 1992b), in which pain is generated when tissues fail to restrain their vertebrae near the neutral position (Figure 13.5), causing altered loading during motion and irritation at its end-range. It is a small step to imagine how manual therapies, aimed at the vertebral levels involved, or their adjacent levels, could influence this.
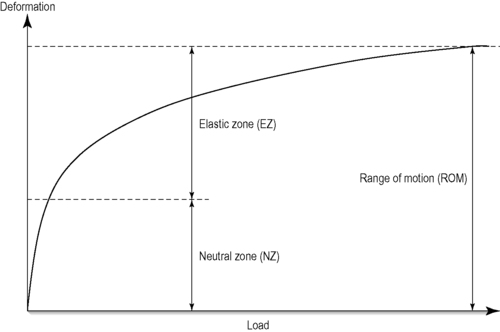 |
| FIGURE 13.5 |
There are long-established theories (Gertzbein et al., 1985 and Kirkaldy-Willis, 1992), as well as cadaveric evidence (Mimura et al. 1994) that intervertebral laxity occurs with early-stage disc degeneration. Such laxity seems to be caused by loss of normal intradiscal pressure, which, under load, is a major restraining influence between vertebrae (Zhao et al. 2005). Early-stage disc degeneration is much more readily detectible with magnetic resonance than with plain X-rays (Pfirrmann et al. 2001) but there is emerging evidence, also from magnetic resonance studies, of an association between aberrant (paradoxical) intervertebral motion and disc degeneration as detected by magnetic resonance (Fowler et al. 2006), adding weight to the concept of aberrant motion as a source of mechanical pain.
Recent quantitative fluoroscopy research has moved this model of mechanical dysfunction from the realm of theory to that of biomechanical measurement and from cadaveric to patient studies. Separate from this, and using cadaveric studies, Mimura et al., 1994 and Zhao et al., 2005 established a relationship between laxity and early disc degeneration, expressing it as the proportion of overall intervertebral range that is achieved in the neutral zone. Using quantitative fluoroscopy, Wong et al., 2004 and Breen et al., 2000a then measured it in living subjects. The latter also demonstrated lax appearance in the motion patterns of lumbar motion segments adjacent to surgically stabilized ones (Figure 13.6).
 |
| FIGURE 13.6
(from quantitative fluoroscopic studies).
|
It is important to have a practical measurement of laxity to use in patient studies. Wong et al. (2004) used the slope of intervertebral motion against trunk motion to express laxity (Figure 13.7). Mellor et al. (2008) used both the slope of intervertebral to trunk motion and the proportion of the intervertebral range in the first 10o of trunk motion. Such studies are gradually accumulating normative reference information with which to compare patient data.
What this amounts to is the capability to measure intervertebral laxity and the influence that physical therapies may have upon it in living subjects. This is a new horizon in research into spinal manipulation that could lead to better trials of efficacy. It should then also be possible to establish whether manipulation does, as in Figure 13.4, restore mobility to stiff spinal joints. This old concept of the mechanism of spinal manipulation (Haldeman, 1992, Peterson and Bergmann, 2002, Liebenson, 2006 and Morris, 2006) would then at last be testable. However, this is just the beginning. The mechanical effects of manipulation could also be explained by changes in muscle activity and length (Sihvonen et al., 1991, Kaigle et al., 1998, Mannion, 1999 and Lariviere et al., 2002) and by neurological and circulatory effects (Sandoz, 1978 and Wyke, 1985). This adds further levels of complexity and calls for even more sophistication in study design.
How safe is manipulation?
Given the higher range of motion intended with manipulation, there are implications for both clinical effectiveness and patient safety. Mainly used for low-back pain, the risk of serious adverse effects is thought to be extremely low in skilled hands, therefore guidelines generally stipulate only that practitioners should be adequately trained (van Tulder et al. 2006).
The second most frequent use of manipulation is for neck pain (Pedersen 1994), where there have been reports in the research literature, plus considerable press speculation, about the (rare) occurrence of postmanipulation stroke (Ernst 2002). In a recent prospective study of 529 chiropractic patients who received neck manipulation, the main adverse effects, albeit transient, were reported to be headache or a temporary worsening of neck symptoms (Rubinstein et al. 2008). Even the most severe of these did not have long-term effects. In a subsequent large prospective cohort study of 50 275 neck manipulations (Thiel et al. 2007) no serious adverse effects were reported.
The Neck Pain Task Force of the World Health Organization found that neck mobilization and manipulation have similar degrees of effectiveness (Gross et al., 2005 and Hurwitz et al., 2008). Combined with exercise, they are reported to be more effective than the alternative strategies to which they have been compared. In the absence of any good evidence of a greater risk from manipulation, the authors recommended that the choice between the two should be guided by patient preference (Hurwitz et al. 2008). However, given the concerns that have been voiced, it is essential to try to balance the good that manual therapies do against any possible harm that might occur.
The quality of studies about harm
Researching the risk of serious harm from a treatment sometimes brings researchers into contact with stakeholders with strong ontic commitment to certain conceptions of the physical system in play (Martin 1962). Where the research question and the interpretation of evidence are also difficult, there is great pressure on investigators. It therefore makes sense to choose the best methodology to determine whether there is a significant risk of stroke as a result of manipulation and there are a range of approaches to choose from. These include: hypothetical estimates of absolute risk (Klougart et al. 1996), retrospective surveys of practices (Dvorak & Orelli 1985), reviews of case reports (Ernst 2002), case-control studies (Rothwell et al., 2001, Smith et al., 2003 and Cassidy et al., 2008), prospective cohort studies without controls (Thiel et al., 2007 and Rubinstein et al., 2008) and prospective cohort studies with controls. Whichever technique is chosen, the rigour of both the research design and its execution will determine the authority with which the result is ultimately regarded (Levine et al. 1994). At the low end are estimates from numbers of patients treated against incidence from other studies. Then come estimates from case reports. Then probably come retrospective surveys of practices and unblinded prospective cohort studies without controls. Close to the top, as far as quality is concerned, are case-control studies that allow the inference of causation (and which give us our current best evidence) and, finally, prospective cohort studies with controls (of which none yet exist).
To study risk in a prospective cohort would probably be most feasible in a community stroke study, where strokes and transient ischaemic attacks, reported in primary care and confirmed by a neurologist, are investigated for exposure, or otherwise, to manipulation. (This would be superior to a study based on hospital discharge because many patients with mild strokes are never hospitalized.) These would then be compared with a matched population from the community, who have not had strokes, for exposure to manipulation. This helps to avoid errors in case ascertainment and failure to include all relevant cases (such as carotid strokes) as in retrospective hospital discharge studies (Cassidy et al. 2008). It also ensures that study populations are relevant and avoids having to use controls who have had other kinds of strokes (Smith et al. 2003). Finally, and importantly, it helps to avoid comparing cases and controls with different risk factors for cerebrobasilar stroke (Rothwell et al. 2001).
Such an opportunity did once present itself in a 10-year follow-up to the Oxford Community Stroke Study (Bamford et al. 1990), but was not taken up. In the meantime, although case-control studies do seem consistently to suggest that there is a relationship between manipulation and stroke, especially in younger patients with neck pain or headaches (Rothwell et al., 2001, Smith et al., 2003 and Cassidy et al., 2008); although it seems to have been established that the manipulation is unlikely to be causal. This was found by concurrently investigating the relationship to general practitioner visits and finding it to be similar. In other words (and as suggested 6 years before: Breen 2002), patients who are about to have a cerebrobasilar stroke may visit either their manipulation practitioner or their general practitioner and thereafter suffer the same event as part of natural history and not as a result of seeing either practitioner.
Nevertheless, this does not make the problem go away. Some people may not discriminate between manipulation causing a stroke and manipulation being associated with it for another reason. Others may ignore the evidence base and remain bound to their own preconceptions. The question may, therefore, continue to be raised in the popular press. Replication of the Cassidy study (Cassidy et al. 2008) may therefore be necessary before minds are set at rest and we can focus more on research that would help the patients who are at risk. This research should address the question of what good it would do to be able to recognize these patients in primary care practice. Are there interventions that could minimize progression to infarction if the risks were recognized in time? Are the risk factors sufficiently well known and accessible to be detected by practitioners? Could they be? A systematic review of risk factors for cervical artery dissection (Rubinstein et al. 2005) (Table 13.1) suggests that the main ones (increased aortic root diameter and change in carotid arterial diameter) could not be detected without vascular imaging studies, although the lesser ones (minor trauma, classical migraine and recent infection) certainly could.
| CI, confidence interval. | |
| Risk factor | Odds ratio (95% CI) |
|---|---|
| Aortic root diameter >34mm | 14.2 (3.2–63.6) |
| Carotid artery diameter change | 10.0 (1.8–54.2) |
| during cardiac cycle | |
| Migraine | 3.6 (1.5–8.6) |
| Trivial trauma (neck manipulation) | 3.8 (1.3–11.0) |
| Recent infection | 1.6 (0.7–3.8) |
| Homocysteine | (unknown) (1.1–1.5) |
The manipulation ‘package of care’
For people with spinal problems, the reduction of pain and the return to normal activity may also benefit any concurrent cardiovascular, mental and general health problems (Ong et al., 2004 and Waddell and Burton, 2004). This approach in rehabilitation implies that the practitioner who uses manipulation should also engage with the psychological and social factors that influence the course of chronic pain (Truchon 2001). This is very much in keeping with the wider biopsychosocial understanding of health that has come to be expected of most practitioners who deal with musculoskeletal conditions (Weigl et al. 2006). Thus, manipulation is not the mainstay of treatment for either of these conditions, but a useful addition to evidence-based care. This evidence-based management comes with a few simple messages:
• A case history and physical examination should be carried out.
• People should be given information and person-specific advice about how to manage pain and recover.
• Progress should be reviewed and management revised as needed.
• Most people are best managed in primary care.
If a person consults early in the course of the problem, the main consideration is to control pain while avoiding withdrawal and inactivity. If the patient’s condition is chronic, then practitioners are advised to assess prognostic factors and provide a consistent, cognitive behavioural approach.
Adherence to the evidence and doing it better
The practice styles of many manipulation practitioners already reflect this closely, but manipulation may be overutilized by them while pain control is underutilized. This may be rooted in the natural healing tradition of the professions and an in-principle aversion to drugs. However, there is evidence that many manipulation practitioners already have evidence-based care within their traditions. Indeed, before guidelines began to be published, a survey of 1012 chiropractic patients throughout Europe in the early 1990s (Pedersen 1994) had found that virtually all had received a comprehensive case history and examination and an explanation of their symptoms. Within 3 months of their first attendance, 65% of them had had reassessments recorded in their clinical records. Eighty-seven per cent were advised to stay active and only 2% and 5% (respectively) were advised to have bed rest and/or stay off work. However, only 4% were advised to take analgesics to control pain while almost all were given a manual treatment at most attendances. Explanation of symptoms, ergonomic advice and psychological and social advice were consistently provided for patients across the first five visits. In a subsequent study of UK chiropractors (Lauridsen 1999), 98% of respondents were found to use some form of exercises for chronic low-back pain. The use of X-rays, which is not recommended for back and neck pain unless pathology is suspected, has reduced sharply in chiropractic from an estimated 5112 new films annually in 1973 (Breen 1977) to only 158 in 2000 (Breen et al. 2000b).
Taking account of societal factors
With a few exceptions, therefore, the care traditionally offered by many practitioners of manipulation already reflects the evidence base. This assumes, however, that our biopsychosocial understanding of common health problems is wide enough. The overall cost of back pain alone is thought to be 2–3% of the gross domestic product of western European economies (Nachemson et al. 2000). In the UK in 2007, this was estimated at £1333 billion (National Statistics 2007), which would put this cost in the region of £27bn ($40bn). These are apparently mainly from lost production and other societal costs, especially in chronic cases (Clinical Standards Advisory Group Epidemiology Review 1994), while the total UK health care bill for back pain has been estimated at around £1bn (Maniadakis & Gray 2000). One explanation may be that it is the social and societal spectrum of problems associated with chronic back pain that is generating most of the cost and not just the back pain itself. If this is the case, a biomedical approach to back pain is not only inadequate (Foster et al. 2003), but fundamentally inappropriate. The social and societal factors are:
• work problems (unemployment, job dissatisfaction)
• financial problems (low economic status, low education)
• legal limitations (compensation pending and insurance rules)
• health care system (low priority, poor integration)
• social problems (poor housing, low support, low sense of control) (Pincus et al. 2008b).
These, together with other health problems, multisite pain and psychological problems (distress and depression), help to explain the high impact of back pain-related disability, which is not solvable by physical treatment alone. The sheer size of this impact means that the attention of policy-makers is urgently required and a multidisciplinary, biopsychosocial approach needs to be expected of all who attempt to help the sufferer. Among those who do offer such help are, or course, practitioners who use manipulation. Research has already shown, and may continue to reveal, to what extent practice remains aligned to the evidence, or even improves by addressing this wider spectrum of prognostic factors. Central to this will be whether manipulation remains the focus of their approach or becomes a tool within it.
Regular surveys of practice are crucial if the manipulating professions are to develop themselves optimally. Studies of patient cohorts could reveal the relationship between these new issues, such as the engagement of the practitioner with the wider context of health and its effect on clinical outcomes. However, this also calls for new outcome measures. How do we measure the impact of social and societal factors? To what extent do practitioners who use manipulation in primary care make an explicit attempt to improve them as part of their clinical management? There is reasonable international consensus that the above factors are the main ones (Pincus et al. 2008b) and that the appropriate method for measuring their effect sizes is inception cohort studies. However, we do not have instruments that measure, for example, ‘the influence of compensation litigation’ or ‘employer intransigence’. It is also worth finding out if practice in the private and public sectors is equally effective for patients.
Researching clinical effectiveness
The randomized trial is generally considered to be the best study design for comparing the effectiveness of treatments, but a truly valid comparison is sometimes very difficult, to the extent that some regard the randomized controlled trial as being of dubious value and potentially misleading (Bolton 1997). Koes (2004) outlined the main problems as:
• being able to compare populations that otherwise have the same prognosis
• standardizing the interventions
• blinding patients, therapists and outcome measurement
• recruiting an adequate sample size
• drop-outs and loss to follow-up.
Guidelines
The importance of having high-quality trials is that they form a large part of the basis of clinical guidelines. The consequences of adopting misleading conclusions from low-quality clinical trials surface particularly when guidelines based on them are monodisciplinary or based on trial evidence alone, to the exclusion of clinical expertise and patient preference (Sackett et al. 1996). In some back pain guidelines, for example, manipulation is not even mentioned (Philadelphia Panel, 2001 and Bekkering et al., 2003), despite the amount of evidence that surrounds it.
The potential consequences of low-quality guidelines are:
• poor patient care
• inflexibility
• disruption of practice
• threat to livelihood
• medicolegal liability (if not following) (Breen 2006).
This also makes useful social policy reform difficult and is a reason why guideline appraisal is essential before dissemination and implementation are attempted (AGREE 2001). Although manipulation is seldom administered as a monotherapy (Pedersen 1994), none of the individual components of the packages of care that include it have large therapeutic effects in populations (Assendelft et al. 2004). Some recent trials of physical therapy have sought to compare some components of such packages against others, or with the whole, but with little or no difference detected (Frost et al., 2004 and Klaber Moffett et al., 2005) and scholars often disagree about the level of causation that trials of physical therapies could reasonably be expected to reveal (Cornwall & Murrell 1993). Certainly attenuation or enhancement of treatment effects could be related to trial design and it is useful to consider how such systematic effects could influence outcomes and some ways in which to avoid these pitfalls.
The quality of manipulation trials
Key quality criteria for clinical trials of manual therapies have been offered in a previous edition of this chapter (Breen 2001) as: adequate randomization, blinding of outcome assessment, no exclusions from analysis and numbers and reasons for drop-out and withdrawal recorded (Table 13.2). These are principally aimed at eliminating assessor bias. However, there may be others that could affect results to the extent that any attempt to infer causation could be dubious (Phillips & Goodman 2004). These other quality criteria mainly relate to what actually happened to the subjects. For example, patients with musculoskeletal disorders may have strong preferences for one or other of the treatments (Meade et al. 1990), increasing the danger of selective drop-out or cross-over. ‘Intention-to-treat’ analysis, which is a standard quality requirement, will only tell us which group assignment was the most successful and not necessarily which treatment was superior. Because blinding is often impossible and patients generally prefer to be in the treatment group than the control group, intention-to-treat analysis may show an inflated level of effectiveness for controls if there are high levels of cross-over to manipulation treatment. It has therefore been suggested that an ‘as treated’ analysis should also be conducted to compare the effectiveness of the treatments themselves and not just the ‘intention’ to use them (M Campbell, personal communication).
| aRandom numbers generated by computer, random numbers table, shuffled cards or tossed coins and minimization. Randomization clearly (authors explicitly state method) and adequately concealed from treatment and assessment. |
|
| bOutcome evaluators shielded from knowledge of treatment assignments. |
|
| cNo exclusions from analysis regardless of whether they: (1) deviated from protocol; (2) withdrew; (3) dropped out; (4) were lost to follow-up. |
|
| Adapted from: Schulz et al., 1995 and Moher et al., 1998. | |
| Criterion | Points |
|---|---|
| Randomization | |
| Randomized | +1 |
| Method described and appropriatea | +1 |
| Method inappropriatea | –1 |
| Blinding of outcome assessmentb | |
| Double-blind | +1 |
| Masking described and appropriate | +1 |
| Method inappropriate | –1 |
| Intention-to-treat analysisc Drop-outs and withdrawals |
+1 |
| Numbers and reasons for withdrawal reported | +1 |
| Maximum total points | 6 |
Does it really make a difference?
Emphasis is traditionally placed on the statistical significance of differences found in trials (Bouter et al., 1998, van Tulder et al., 2003 and Ferrer et al., 2006). This is generally placed at the 95% level with at least 80% power to show the expected difference. However there have been calls for the application of minimum clinically important differences (MCID) to the outcome. A good example of this has evolved for the Roland and Morris Back Pain Disability Questionnaire (Roland & Morris 1983), which has a 24-point scale, and is among the most commonly used disability measures in manipulation trials. For such trials, the MCID could be considered as the lowest score in patients who improve according to their scores on a concurrently applied pain transition scale (Stratford et al. 1996a). Studies in the UK have determined that this is around 2.5 points out of the 24 (Klaber-Moffett et al., 1999 and UK BEAM TT, 2004). For clinical practice, as opposed to research use, this has been recommended as the change score reached at the lower 95% confidence interval of the mean scores in a group of patients (Stratford et al. 1996b), or, alternatively, a change score of more than 30% of their initial score in patients who say they have improved. The higher the MCID is taken to be, the more relevant will be the results of treatment for the patients for whom it is achieved, but the more difficult it will be to achieve in the first place. This is a challenge to all interventions for common musculoskeletal problems, which have so far shown only modest improvements at most. However, lower levels of improvement may also be important, given the huge costs of these conditions (UK BEAM TT 2004). Future research will have to demonstrate a credible trade-off between these two priorities.
Finally, recommendations for improved methodology in trials of non- pharmacologic interventions have been made in an extension of the Consolidated Standards of Reporting Trials (CONSORT) statement (Altman et al., 2001, Moher et al., 2001, Boutron et al., 2008a and Boutron et al., 2008b). This suggests that, although the practitioners who apply interventions such as manipulation cannot be blinded to treatment allocation, any others who supply co-interventions, such as exercises, should at least be blinded. Further, the expertise of care providers, and any clustering thereof in factorial design trials, need also to be taken into account.
Research and access to manipulation in the UK
Chiropractors and osteopaths, the main practitioners of manipulation, provide the most sought-after of complementary interventions by the public in England, but not the most commissioned by the National Health Service (NHS) on its behalf (Thomas et al. 2001). This reflects a continuing lack of acceptance that is difficult to explain. Before manipulation became accepted in health care, its practitioners were widely viewed with scepticism by mainstream colleagues and people sought manipulative treatment late in the course of their conditions (Breen, 1977 and Burton, 1981). More recently, however, they have tended to consult much earlier (Pedersen 1994). Yet despite the public recognition and regulation of chiropractic and osteopathy, only 4–10% of these professionals’ services are available through the UK NHS (Wadsworth 1998). This is consistent with evidence that a different part of society receives manipulation for back pain from chiropractors and osteopaths than from physiotherapists (Ong et al. 2004). These former are the higher wage earners with better general health and are apparently well motivated to recover from their problems (Langworthy & Breen 2007).
The continuing isolation of manipulation practitioners may be in part caused by their own mistrust of the health care system and of each other and be a reason why a minority of them may continue treatment when patients are not responding in preference to referring into what may be perceived as an abyss (Pincus et al. 2006). The answer to why they are rather less welcomed than might be expected may also lie in poor communication in primary care, or in competing priorities in general practice, where the greatest proportion of musculoskeletal patients seek help (Parsons et al. 2007). It is unlikely to be because GPs are adverse to receiving patient reports from them, but perhaps more because they find their terminology confusing (Brussee et al. 2000, 2001). Such reports may, however, be infrequent and therefore miss the opportunity to familiarize GPs with the context of manipulation in the community. Much more research is needed into the relationships, and potential relationships, of practitioners of manipulation with mainstream health care.
Manipulation and the transition to mainstream health care
There appear also to be barriers to commissioning manipulation services in the NHS. Despite the low-tech, evidence-based service that guidelines call for, care pathways are not always compatible with ways of working in primary care. Referrals for musculoskeletal problems may be poorly documented in practice databases and it may therefore be difficult to locate a starting point for innovatory change. Patients may be averse to an evidence-based approach if they have already set their minds on sick certification, X-rays or consultant referral. There may also be other factors, for example, managerial policies of ‘no return until fully fit’, that conflict, or legal or insurance coverage provisions that work against a supported rehabilitation programme. Finally and importantly, evidence-based management of musculoskeletal problems is not included within the NHS Quality and Outcomes Framework. These are major reasons for poor uptake of guidelines (Bird, 2000, Langworthy et al., 2002 and Langworthy et al., 2005) and will continue to be until they are addressed as health and social policy issues.
Conclusion
Research relating to manipulation needs to include the mechanisms of action, the trends in practice and the influence of the settings and social circumstances in which the therapy is used. Clinical value is generally understood to be based on clinical outcomes, functional outcomes, satisfaction and cost factors (Nelson et al. 1996). Yet, for example, there may be little association between patient satisfaction with care and recovery (Breen & Breen 2003). This may require uncomfortable trade-offs in service arrangements.
We may also now have new opportunities to investigate the mechanical effects of the intervention. This will depend on further technological innovations in biomechanical measurement in vivo and, in particular, defining the limits of normality of new, but relevant, physiological values. We may then be able to determine whether there is any relationship between biomechanics and health measures such as pain and disability. This would allow the long-awaited explanatory trials of manipulation in returning biomechanics to normal to be carried out.
Pragmatic trials of optimized packages of care that include manipulation are also needed. For example, previous trials have not generally included the manipulator as a prescriber of pain control and exercise, yet these are important parts of evidence-based care with which manipulation is normally associated. There also needs to be greater clarity about the importance of short-term relief. This is often important to patients and there are sometimes conflicts between providing interventions that last, but take time to act, and those that may act quickly, even if recovery is to be expected eventually, without any intervention. Future trials could also usefully control for the presence of prognostic factors, such as multisite pain (Carnes et al. 2007), distress, high pain at onset and minor comorbidity (Breen et al. 2005).
The UK’s Musculoskeletal Services Framework (Department of Health 2006) calls for practitioners who can provide evidence-based assessment and management of people with common musculoskeletal disorders to supply the expertise for the interface between primary and secondary care. This raises intriguing questions for primary care commissioning, as well as for health care quality improvement. These could be investigated using carefully designed qualitative outcomes and health service utilization studies involving primary and secondary care practitioners and commissioners. To do justice to the problem, however, these will require the cooperation and active participation of the chiropractors, osteopaths and specialist physiotherapists who provide manipulation. The role of these practitioners in the management of chronic pain is by no means clear. The stumbling block is bound up with understanding and providing a ‘multi-disciplinary bio-psychosocial intervention’ (Karljalainen et al. 2001). Commissioners have begun to articulate what this might involve (NHS 2008), but given the number of stakeholders, implementation will always be challenging.
The overall message of the evidence for common musculoskeletal problems is a simple one. In populations, the effects of the best interventions are on average only moderate and these interventions are not high-tech ((NHMRC) NHaMRC, 2003 and European Commission CBMC, 2006). Seen in this light, it makes sense to make service arrangements that allow patients to have access to all of these interventions from one practitioner, if possible. It will help if we work, through research, to determine where manipulation has the strongest rationale for care and where other physical or psychosocial interventions do.
References
Agency for Health Care Policy Research, Clinical practice guidelines no.14 – acute low back pain problems in adults. Report No.: 14. (1994) Agency for Health Care Policy Research, US Department of Health and Human Services, Washington DC.
A.G.R.E.E, Appraisal of guidelines for research and evaluation. (2001) St George’s Hospital Medical School, London.
Airaksinen, O.; Brox, J.I.; Cedraschi, C.; et al., European guidelines for the management of chronic nonspecific low back pain, Eur. Spine J. 15 (2006) S192–S300.
Altman, D.G.; Schulz, K.F.; Moher, D.; et al., The revised CONSORT statement for reporting randomized trials: explanation and elaboration, Ann. Intern. Med. 134 (8) (2001) 663–694.
In: (Editors: Assendelft, W.J.J.; Morton, S.C.; Yu, E.I.; et al.) Spinal manipulative therapy for low back pain (Cochrane Review) (2004) John Wiley, Chichester, UK.
Bamford, J.; Sandercock, P.; Dennis, M.; et al., A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project – 1981–86 1. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrihage, J. Neurol. Neurosurg. Psychiatry 53 (1990) 16–22.
Bekkering, G.E.; Hendriks, H.J.M.; Koes, B.W.; et al., Dutch physiotherapy guidelines for low back pain, Physiotherapy 89 (2) (2003) 82–96.
Bird, C., Commissioned R&D Programmes: Implementation of low back pain guidelines in North Thames. (2000) NHS Executive London Regional Office, London.
Bolton, J.E., Future directions for outcomes research in back pain, European Journal of Chiropractic 45 (1997) 57–64.
Bouter, L.M.; van Tulder, M.W.; Koes, B.W., Methodologic Issues in Low Back Pain Research in Primary Care, Spine 23 (18) (1998) 2014–2020.
Boutron, I.; Moher, D.; Altman, D.G.; et al., Methods and Processes of the CONSORT Group: Example of an Extension for Trials Assessing Nonpharmacologic Treatments, Ann. Intern. Med. 148 (4) (2008) 61–66.
Boutron, I.; Moher, D.; Altman, D.G.; et al., Extending the CONSORT Statement to Randomized Trails of Nonpharmacologic Treatment: Explanation and Elaboration, Ann. Intern. Med. 148 (4) (2008) 295–309.
Bowden, A.E.; Guerin, H.L.; Villarraga, M.L.; et al., Quality of motion considerations in numercial analysis of motion restoring implants of the spine, Clin. Biomech. 23 (2008) 536–544.
Breen, A.C., Chiropractors and the treatment of back pain, Rheumatol. Rehabil. 16 (1977) 46–53.
Breen, A.C., Manual Therapies, In: (Editors: Lewith, G.; Jonas, W.B.; Walach, H.) Clinical Research in Complementary Therapies (2001) Churchill Livingstone, Edinburgh, pp. 247–261.
Breen, A.C., Manipulation of the neck and stroke: time for more rigorous evidence, Med. J. Aust. 176 (2002) 363–364; (15 April).
Breen, A., From guidelines to practice: what is the practitioner’s role? In: (Editor: Liebenson, C.) Rehabilitation of the Spinesecond ed. (2006) Lippincott, Williams & Wilkins, Philadelphia, pp. 933–945.
Breen, A.; Breen, R., Back pain and satisfaction with chiropractic treatment: What role does the physical outcome play?Clin. J. Pain 19 (2003) 263–268.
Breen, A.C.; Langworthy, J.; Vogel, S.; et al., Primary care audit toolkit: acute low back pain. (2000) Institute for Musculoskeletal Research and Clinical Implementation, Bournemouth.
Breen, A.; Carrington, M.; Collier, R.; et al., Communication between general and manipulative practitioners: a survey, Complement. Ther. Med. 8 (2000) 8–14.
Breen, A.; Langworthy, J.; Bagust, J., Improved early pain management for musculoskeletal disorders: Health and Safety Executive. (2005) ; Report No: 399. Available online athttp://www.hse.gov.uk/research/rrhtm/rr399.htm.
Breen, A.; Muggleton, J.; Mellor, F., An objective spinal motion imaging assessment (OSMIA): reliability, accuracy and exposure data, BMC Musculoskelet. Disord. 7 (1) (2006) 1–10.
Breen, A.; Fowler, J.; Mellor, F., Adjacent segment motion and posterior lumbar spine instrumention: a comparison of patient groups. Spine Arthroplasty Society Global Symposium on Motion Preservation Technology. (2007) ; Berlin.
Brussee, W.J.; Assendelft, W.J.J.; Breen, A.C., Communication between general practitioners and chiropractors, J. Manipulative Physiol. Ther. 24 (1) (2001) 12–16.
Burton, A.K., Back pain in osteopathic practice, Rheumatol. Rehabil. 20 (1981) 239–246.
Carnes, D.; Parsons, S.; Ashby, D.; et al., Chronic musculoskeletal pain rarely presents in a single body site: results from a UK population study, Rheumatology 46 (1) (2007) 1168–1170.
Cassidy, J.D.; Lopes, A.A.; Yong-Hing, K., The immediate effect of manipulation versus mobilisation on pain and range of motion in the cervical spine: a randomised controlled trial, J. Manipulative Physiol. Ther. 15 (9) (1992) 570–575.
Cassidy, J.D.; Boyle, E.; Cote, P.; et al., Risk of Vertebrobasilar Stroke and Chiropractic Care: Results of a Population-Based Case-Control and Case-Crossover Study, Spine 33 (4S) (2008) S176–S183; Neck Pain Task Force(Supplement):.
Childs, J.D.; Fritz, J.M.; Flynn, T.W.; et al., A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study, Ann. Intern. Med. 141 (12) (2004) 920–928.
Chou, R.; Huffman, L.H., Nonpharmacologic Therapies for Acute and Chronic Low Back Pain: A Review of the Evidence for an American Pain Society/American College of Physicians Clinical Practice Guideline, Ann. Intern. Med. 147 (7) (2007) 492–504.
Chown, M.; Whittamore, L.; Rush, M.; et al., A prospective study of patients with chronic back pain randomised to group exercise, physiotherapy or osteopathy, Physiotherapy 94 (2008) 21–28.
Clinical Standards Advisory Group Epidemiology Review, The epidemiology and cost of back pain. Report of a Clinical Standards Advisory Group Committee on Back Pain. (1994) Department of Health, London.
Cornwall, M.W.; Murrell, P., Pre-experimental, Experimental and Quasi-experimental Research Designs, In: Handbook of Physical Therapy Research (1993) J.B. Lippincott, Philadelphia, pp. 143–175.
Coulter, I.D.; Shekelle, P.G., Chiropractic in North America: a descriptive analysis, J. Manipulative Physiol. Ther. 28 (2005) 83–89.
Department of Health, The Musculoskeletal Services Framework. (2006) Department of Health, London.
Dvorak, J.O.; Orelli, F.V., How dangerous is manipulation to the cervical spine?Manual Medicine 2 (1985) 1–4.
Eisenberg, D.M.; Kessler, R.C.; Foster, C.; et al., Unconventional medicine in the United States: prevalence, costs and patterns of use, N. Engl. J. Med. 328 (4) (1993) 246–252.
Ernst, E., Manipulation of the cervical spine: a systematic review of case reports of serious adverse events, 1995–2001, Med. J. Aust. 176 (2002) 376–380; (15 April).
European Commission CBMC, COST B13: European Guidelines for the management of low back pain, Eur. Spine J. 15 (Suppl. 2) (2006).
Evans, D.W., Mechanisms and effects of spinal high-velocity, low-amplitude thrust manipulation: previous theories, J. Manipulative Physiol. Ther. 25 (2002) 251–262.
Evans, D.W.; Breen, A.C., A biomechanical model for mechanically efficient caitation production during spinal manipulation: prethrust position and the neutral zone, J. Manipulative Physiol. Ther. 29 (1) (2006) 72–82.
Fernandez-Bermego, E.; Garcia-Jimenez, M.A.; Fernandez-Palomeque, C.; et al., Adolescent idiopathic scoliosis and joint laxity: a study with somatosensory evoked potentials, Spine 18 (7) (1993) 918–922.
Ferrer, M.; Pellise, F.; Escudero, O.; et al., Validation of a Minimum Outcome Core Set in the Evaluation of Patients With Back Pain, Spine 31 (12) (2006) 1372–1379.
Flynn, T.W.; Fritz, J.; Wainner, R.S.; et al., The audible pop is not necessary for successful spinal high-velocity thrust manipulation in individuals with low back pain, Arch. Phys. Med. Rehabil. 84 (2003) 1057–1060.
Foster, N.E.; Pincus, T.; Underwood, M.R.; et al., Editorial: Understanding the process of care for musculoskeletal conditions – why a biomedical approach is inadequate, Rheumatology 42 (2003) 401–403.
Fowler, J.; Mellor, F.; Muggleton, J.; et al., Abnormal inter-vertebral motion is associated with chronic low back pain and MR disc degeneration. (2006) Spine Society of Europe Annual Meeting, Istanbul.
Frost, H.; Lamb, S.E.; Doll, H.A.; Carver, P.T.; Stewart-Brown, S., Randomised controlled trial of physiotherapy compared with advice for low back pain, Br. Med. J. 329 (2004) 708–711.
Gertzbein, S.D.; Seligman, J.; Holtby, K., Centrode patterns and segmental instability in degenerative disc disease, Spine 10 (3) (1985) 257–261.
Gross, A.R.; Hoving, J.L.; Haines, T.A.; et al., Manipulation and mobilisation for mechanical neck disorders (Review). The Cochrane Library. (2005) ;http://wwwthecochranelibrarycom; (2).
In: (Editor: Haldeman, S.) Principles and Practice of Chiropracticsecond ed. (1992) Appleton & Lange, Norwalk, Connecticut.
Haldeman, S.D., Spinal manipulation: when, how and who?Bulletin: Hospital for Joint Diseases 55 (3) (1996) 135–137.
Haldeman, S.; Carroll, L.; Cassidy, J.D.; et al., The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: Executive Summary, Spine 33 (4S) (2008) S5–S7; Neck Pain Task Force(Supplement).
Hancock, M.J.; Maher, C.G.; Latimer, J.; et al., Independent evaluation of a clinical prediction rule for spinal manipulative therapy: a randomised controlled trial, Eur. Spine J. 17 (2008) 936–943.
Harvey, E.; Burton, A.K.; Moffett, J.K.; et al., Spinal manipulation for low-back pain: a treatment package agreed by the UK chiropractic, osteopathy and physiotherapy professional associations, Man. Ther. 8 (1) (2003) 46–51.
Hewitt, D.; Wood, P.H., Heterodox Practitioners and the availability of specialist advice, Rheumatol. Rehabil. 14 (3) (1975) 191–199.
Huisman, M.; Breen, A., The Changing Face of British Chiropractic, Contact 4 (2) (1990) 11–12.
Hurwitz, E.L.; Carragee, E.J.; van der Velde, G.; et al., Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders, Spine 33 (4S) (2008) S123–S152; Neck Pain Task Force(Supplement).
Kaigle, A.M.; Wesberg, P.; Hansson, T.H., Muscular and kinematic behavior of the lumbar spine during flexion-extension, J. Spinal Disord. 11 (2) (1998) 163–174.
Karljalainen, K.; Malmivaara, A.; van Tulder, M.; et al., Multidisciplinary biopsychosocial rehabilitation for subacute low-back pain among working age adults, Spine 26 (2001) 262–269.
Kirkaldy-Willis, W.H., Pathology and pathogenesis of low back pain, In: (Editors: Kirkaldy-Willis, W.H.; Burton, C.V.) Managing Low Back Pain (1992) Churchill Livingstone, New York, pp. 49–79.
Klaber-Moffett, J.; Torgerson, D.; Bell-Syer, S.; et al., Randomised controlled trial of exercise for low back pain: clinical outcomes, costs and preferences, Br. Med. J. 319 (1999) 279–283.
Klaber Moffett, J.A.; Jackson, D.A.; Richmond, S.; et al., Randomised trial of a brief physiotherapy intervention compared with usual physiotherapy for neck pain patients: outcomes and patients’ preference, Br. Med. J. 330 (2005) 75–78.
Klougart, N.; Leboeuf-Yde, C.; Rasmussen, L.R., Safety in chiropractic practice. Part II: Treatment to the upper neck and the rate of cerebrovasulcar incidents, J. Manipulative Physiol. Ther. 19 (9) (1996) 563–569.
Koes, B.W., How to evaluate manual therapy: value and pitfalls of randomized clinical trials, Man. Ther. 9 (2004) 183–184.
Langworthy, J.; Breen, A., Psychosocial factors and their predictive value in chiropractic patients with low back pain: a prospective inception cohort study, Chiropractic & Osteopathy 15 (1) (2007) 5.
Langworthy, J.M.; Breen, A.C.; Vogel, S.; et al., Chiropractic and the National Health Care system: a basis for partnership in the UK, J. Manipulative Physiol. Ther. 25 (1) (2002) 21–33.
Langworthy, J.; Clow, W.; Breen, A., Low back pain: barriers to effective clinical governance, Clinical Governance: An International Journal 10 (4) (2005) 281–290.
Lariviere, C.; Gagnon, D.; Loisel, P., A biomechanical comparison of lifting techniques between subjects with and without chronic low back pain during freestyle lifting and lowering tasks, Clin. Biomech. 17 (2) (2002) 89–98.
Lauridsen, H., Are chiropractors in the United Kingdom using intensive physical training programmes for patients with chronic low back pain? MSc thesis. (1999) Anglo-European College of Chiropractic.
Levine, M.; Walter, S.; Lee, H.; et al., Users’ guides to the medical literature – IV. How to use an article about harm, JAMA 271 (20) (1994) 1615–1619.
Liebenson, C., Rehabilitation of the Spine: a practitioner’s manual. (2006) Lippincott, Williams & Wilkins, Philadelphia.
Maniadakis, N.; Gray, A., The economic burden of back pain in the UK, Pain 84 (1) (2000) 95–103.
Mannion, A.F., Fibre type characteristics and function of the human paraspinal muscles: normal values and changes in association with low back pain, J. Electromyogr. Kinesiol 9 (1999) 363–377.
Martin, R.M., On denotation and ontic commitment, Philos. Stud. 13 (3) (1962) 35–39.
Mayer, R.S.; Chen, I.H.; Lavender, S.A.; et al., Variance in the Measurement of Sagittal Lumbar Spine Range of Motion Among Examiners, Subjects, and Instruments, Spine 20 (13) (1995) 1489–1493.
Meade, T.W.; Dyer, S.; Browne, W.; et al., Low back pain of mechanical origin: randomised comparison of chiropractic and hospital outpatient treatment, Br. Med. J. 300 (1990) 1431–1437.
Mellor, F.; Muggleton, J.M.; Bagust, J.; et al., Mid-lumbar lateral flexion stability measured in healthy volunteers by in-vivo fluoroscopy, Spine 34 (2008) E811–E817.
Mimura, M.; Panjabi, M.M.; Oxland, T.R.; et al., Disc Degeneration Affects the Multidirectional Flexibility of the Lumbar Spine, Spine 19 (12) (1994) 1371–1380.
Moher, D.; Pham, B.; Jones, A., Does quality of reports of randomized trials affect estimates of intervention efficacy reported in meta-analyses?Lancet 352 (1998) 609–613.
Moher, D.; Schulz, K.F.; Altman, D., The CONSORT Statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials, J. Am. Med. Assoc. 285 (15) (2001) 1987–1991.
Morris, C.E., Low Back Syndromes: Integrated clinical management. (2006) McGraw-Hill Medical, New York.
In: (Editors: Nachemson, A.; Carlsson, C.A.; Englund, L.; et al.) Back pain, Neck pain: an evidence based review – Summary and conclusions (2000) Swedish Council on Technology Assessment in Health Care, Stockholm.
Nansel, D.; Cremata, E.; Carlson, J.; et al., Effect of unilateral spinal adjustments on goniometrically-assessed cervical lateral-flexion end-range asymmetries in otherwise asymptomatic subjects, J. Manipulative Physiol. Ther. 12 (6) (1989) 419–427.
National Statistics, (2007) ; Available online at:http://www.statistics.gov.uk/cci/nugget.asp?id=192.
Nattrass, C.L.; Nitschke, J.E.; Disler, P.B.; et al., Lumbar spine range of motion as a measure of physical and functional impairment: an investigation of validity, Clin. Rehabil. 24 (1999) 211–218.
Nelson, E.C.; Mohr, J.J.; Batalden, P.B.; et al., Improving Health Care, Part 1: The Clinical Value Compass, Journal on Quality Improvement 22 (4) (1996) 243–256.
(NHMRC) NHaMRC, Evidence-based management of acute musculoskeletal pain. Australian Acute Musculoskeletal Pain Guidelines Group. (2003) University of Queensland and the Commonwealth Department of Health and Ageing, Brisbane.
NHS, Service Development and Commissioning Directives: Chronic, Non-Malignant Pain. (2008) Cardiff, Welsh Assembly Government.
NICE, Low back pain: the acute management of patients with chronic (longer than 6 weeks) non-specific low back pain (consultation version). (2008) National Institute of Health and Clinical Excellence, London.
Nilsson, N.; Christensen, H.W.; Hartvigsen, J., Lasting changes in passive range of motion after spinal manipulation: a randomised, blind, controlled trial, J. Manipulative Physiol. Ther. 19 (3) (1996) 165–168.
Ong, C.K.; Doll, H.; Bodeker, G.; et al., Use of osteopathic or chiropractic services among people with back pain: a UK population survey, Health and Social Care in the Community 12 (3) (2004) 265–273.
Panjabi, M.M., The stabilising system of the spine – Part 1: Function, dysfunction, adaptation and enhancement, J. Spinal Disord. 5 (4) (1992) 383–389.
Panjabi, M.M., The stabilising system of the spine – Part 2: Neutral zone and instability hypothesis, J. Spinal Disord. 5 (4) (1992) 390–397.
Panjabi, M.; Chang, D.; Dvorak, J., An analysis of errors in kinematic parameters associated with in vivo functional radiographs, Spine 17 (2) (1992) 200–205.
Parsons, S.; Harding, G.; Breen, A.; et al., The Influence of Patients’ and Primary Care Practitioners’ Beliefs and Expectations About Chronic Musculoskeletal Pain on the Process of Care, Clin. J. Pain. 23 (1) (2007) 91–98.
Pedersen, P., A survey of chiropractic practice in Europe, European Journal of Chiropractic 42 (S) (1994) 3–28.
Peterson, D.H.; Bergmann, T.F., Chiropractic technique: principles and procedures. second ed. (2002) Mosby, St Louis, Missouri.
Pfirrmann, C.W.A.; Metzdorf, A.; Zanetti, M.; et al., Magnetic resonance classification of lumbar intervertebral disc degeneration, Spine 26 (17) (2001) 1873–1878.
Philadelphia Panel, Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for neck pain, Phys. Ther. 81 (10) (2001) 1701–1717.
Phillips, C.V.; Goodman, K.J., The missed lessons of Sir Austin Bradford Hill, Epidemiologic Perspectives and Innovations 1 (3) (2004).
Pincus, T.; Vogel, S.; Breen, A.; et al., Persistent back pain – why do physical therapy practitioners continue treatment? A qualitative study of chiropractors, osteopaths and physiotherapists, Eur. J. Pain 10 (2006) 67–76.
Pincus, T.; Santos, R.; Breen, A.; et al., A review and proposal for a core set of factors for prospective cohorts in low back pain: A consensus statement, Arthritis Rheum. 59 (1) (2008) 14–24.
Pincus, T.; Santos, R.; Breen, A.; et al., A Review and Proposal for a Core Set of Factors for Prospective Cohorts in Low Back Pain: A Consensus Statement, Arthritis Rheum. 59 (1) (2008) 14–24.
Reeves, N.P.; Narendra, K.S.; Cholewicki, J., Spine stability: The six blind men and the elephant, Clin. Biomech. 22 (2007) 266–274.
Roland, M.; Morris, R.A., Study of the natural history of pack pain: Part I – development of a reliable and sensitive measure of disability in low back pain, Spine 8 (2) (1983) 141–144.
Ross, J.K.; Bereznick, D.E.; McGill, S.M., Determining cavitation location during lumbar and thoracic spinal manipulation. Is spinal manipulation accurate and specific, Spine 29 (13) (2004) 1452–1457.
Rothwell, D.M.; Bondy, S.J.; Williams, J.I., Chiropractic manipulation and stroke: a population-based case-control study, Stroke 32 (10) (2001) 1054–1060.
Rubinstein, S.M.; Peerdeman, S.M.; van Tulder, M.W.; et al., A systematic review of the risk factors for cervical artery dissection, Stroke 36 (2005) 1575–1580.
Rubinstein, S.M.; Leboeuf-Yde, C.; Knol, D.L.; et al., Predictors of Adverse Events Following Chiropractic Care for Patients With Neck Pain, J. Manipulative Physiol. Ther. 31 (2) (2008) 94–103.
Sackett, D.L.; Rosenberg, W.M.C.; Gray, J.A.M.; et al., Evidence based medicine; what it is and what it isn’t, Br. Med. J. 312 (1996) 71–72.
Sandoz, R., The significance of the manipulative crack and of other articular noises. Annals of the Swiss Chiropractors, Association 4 (1969) 47–68.
Sandoz, R.W., Some reflex phenomena associated with spinal derangements and adjustments. Annals of the Swiss Chiropractors, Association VII (1978) 45–65.
Schulz, K.F.; Chalmers, I.; Hayes, R.J.; et al., Review: empirical evidence of bias, J. Am. Med. Assoc. 273 (1995) 408–412.
Shaffer, W.O.; Spratt, K.F.; Weinstein, J.D.; et al., Volvo Award in Clinical Sciences: The Consistency and Accuracy of Roentgenograms for Measuring Sagittal Translation in the Lumbar Vertebral Motion Segment: An Experimental Model, Spine 15 (8) (1990) 741–750.
Sihvonen, T.; Partanen, J.; Hanninen, O.; et al., Electric behavior of low back muscles during lumbar pelvic rhythm in low back pain patients and health controls, Arch. Phys. Med. Rehabil. 72 (1991) 1080–1087.
Smith, W.S.; Johnston, S.C.; Skalabrin, E.J.; et al., Spinal manipulative therapy is an independent risk factor for vertebral artery dissection, Neurology 60 (2003) 1424–1428.
Stratford, P.W.; Binkley, J.; Solomon, P.; et al., Defining the minimum level of detectable change for the Roland-Morris Questionnaire, Phys. Ther. 76 (4) (1996) 359–365.
Stratford, P.W.; Finch, E.; Solomon, P.; et al., Using the Roland-Morris Questionnaire to make decisions about individual patients, Physiother. Can. 48 (2) (1996) 107–110.
Teyhen, D.S.; Flynn, T.W.; Bovik, A.C.; et al., A new technique for digital fluoroscopic video assessment of sagittal plane lumbar spine motion, Spine 30 (14) (2005) E406–E413.
Thiel, H.W.; Bolton, J.E.; Docherty, S.; et al., Safety of chiropractic manipulation of the cervical spine; A prospective national survey, Spine 32 (21) (2007) 2375–2378.
Thomas, K.J.; Nicholl, J.P.; Coleman, P., Use and expenditure on complementary medicine in England: a population based survey, Complement. Ther. Med. 9 (2001) 2–11.
Truchon, M., Determinants of chronic disability related to low back pain: Towards an integrative biopsychosocial model, Disability & Rehabilitation. 23 (17) (2001) 758–767.
UK BEAM TT, United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care, Br. Med. J. 329 (2004) 1377–1384.
Unsworth, A.; Dowson, D.; Wright, V., ‘Cracking Joints’. A bioengineering study of cavitation in the metacarpophalangeal joint, Ann. Rheum. Dis. 30 (1971) 348–358.
Van Akkerveeken, P.F.; O’Brien, J.P.; Park, W.M., Experimentally induced hypermobility in the lumbar spine: a pathologic and radiologic study of the posterior ligament and annulus fibrosus, Spine 4 (3) (1979) 236–241.
van Tulder, M.; Furlan, A.; Bombardier, C.; et al., Updated Method Guidelines for Systematic Reviews in the Cochrane Collaboration Back Review Group, Spine 28 (12) (2003) 1290–1299.
van Tulder, M.; Becker, A.; Bekkering, T.; et al., Chapter 3: European guidelines for the management of acute nonspecific low back pain in primary care, Eur. Spine J. 15 (Suppl. 2) (2006) s169–s191.
Waddell, G., The Back Pain Revolution. (1998) Churchill Livingstone, Edinburgh.
Waddell, G.; McIntosh, A.; Hutchinson, A.; et al., Low back pain evidence review. (1999) Royal College of General Practitioners, London.
Waddell, G.; Burton, A., Concepts of rehabilitation for the management of common health problems. (2004) The Stationery Office, London.
Wadsworth, R., Commissioning complemerntary medicine, In: Quality in Complementary Medicine: A Meeting of the Forum on Quality in Health Care of the Royal Society of Medicine (1998) Royal Society of Medicine, London, pp. 22–24.
Weigl, M.; Ciezam, A.; Kostanjsek, N.; et al., The ICF comprehensively covers the spectrum of health problems encountered by health professionals in patients with musculoskeletal conditions, Rheumatology 45 (2006) 1247–1254.
White, A.A.; Panjabi, M.M., Clinical Biomechanics of the Spine. (1990) JB Lippincott, Philadelphia.
Wilson, F., A survey of chiropractors in the United Kingdom, European Journal of Chiropractic 50 (3) (2003) 185–198.
Wong, K.W.N.; Leong, J.C.Y.; Chan, M-K.; et al., The flexion–extension profile of lumbar spine in 100 healthy volunteers, Spine 29 (15) (2004) 1636–1641.
Wong, K.; Luk, K.; Leong, J.; et al., Continuous dynamic spinal motion analysis, Spine 31 (4) (2006) 414–419.
World Health Organization, ICF (International Classification of Functioning, Disability and Health) – Revision of the International Classification of Impairments, Disabilities and Handicaps (ICIDH). Resolution no. WHA54.21. (2001) World Health Organization, Geneva.
Wyke, B.D., Articular neurology and manipulative therapy, In: (Editors: Glasgow, E.F.; Twomey, L.T.; Scull, E.R.; Kleyham, A.M.; et al.) Aspects of Manipulative Therapy (1985) Churchill Livingstone, London, pp. 72–77.
Zhao, F.; Pollintine, P.; Hole, B.D.; et al., Discogenic Origins of Spinal Instability, Spine 30 (23) (2005) 2621–2630.