Chapter 44 Mangled Extremity: Are Scoring Systems Useful?
The decision to proceed with amputation or salvage of a mangled extremity is one of the most challenging decisions in orthopedic trauma. Orthopedic trauma surgeons are highly skilled at exercising heroic attempts at limb salvage. However, unsuccessful attempts at salvage are extremely costly and carry with them high morbidity and prolonged rehabilitation. Amputation, on the other hand, is commonly feared by patients. In an attempt to aid in the decision-making process regarding the need for amputation or salvage, a number of predictive indices have been proposed. All of these indices attempt to identify limbs for which salvage or amputation would be preferred.
Advances in care of the traumatized patient including microvascular surgery, nerve reconstruction, tissue transfer, and fracture management continue to expand the orthopedic trauma surgeon’s ability to preserve limbs. However, prolonged, costly, and morbid attempts at preservation may, indeed, be worse than the results of early amputation. As suggested by prominent experts in limb reconstruction,1 this may leave the patient “demoralized, divor-ced and destitute.”
Many considerations must be factored in when making the difficult decision regarding amputation versus limb salvage. These include vascular status, infection risk, tissue devitalization, fracture instability, social impact, physical healing potential, and probably psychological healing potential.2
OPTIONS: SCORING SYSTEMS
Surgeons intuitively recognize that some limbs are frankly beyond salvage, whereas in other cases, a reasonable possibility of limb salvage and restoration of function exists. For centuries before the development of scoring systems, surgical indications for amputation were considered. Kirk,3 in 1943, noted indications for amputation included any injury or disease rendering limb salvage incompatible with function. Absolute and relative indications for amputation after open tibial fractures with vascular injury were described by Lange and colleagues4 in 1985. Absolute indications included anatomically complete disruption of the posterior tibial nerve and a crush injury with a warm ischemic time greater than 6 hours. Relative indications included serious associated polytrauma, severe ipsilateral foot trauma, and an anticipated protracted reconstructive course. The authors specify that their indications for primary amputation included either of the absolute indications or two to three relative indications. Although never validated, this type of classification scheme illustrates several crucial elements of decision making used by experienced surgeons.
Mangled Extremity Syndrome Index
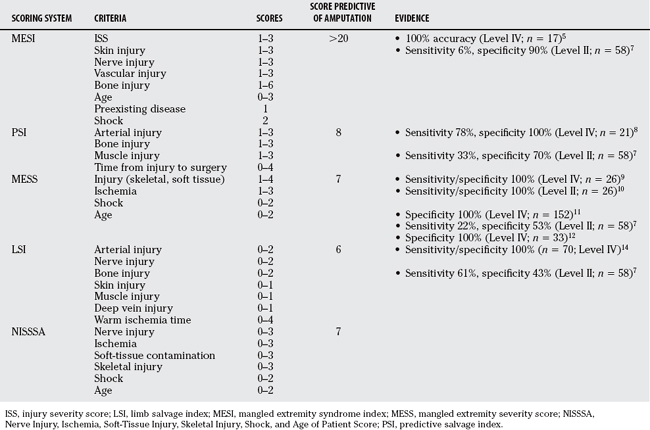
In 1985, Gregory and coworkers’5 severity grading system for multisystem extremity injury entitled “The Mangled Extremity Syndrome Index” (MESI) was published. This scale uses a point score system including the degree of injury severity score to reflect polytrauma, skin injury, nerve injury, vascular injury, bone injury, lag time to surgery and age in years, as well as preexisting disease and shock. In retrospective work, 100% of patients with an MESI of greater than 20 required amputation. However, the patient mix was heterogeneous. Concerns surrounding the MESI include the complexity and the subjectivity of the scoring system. In Roessler and coauthors’ retrospective study6 using this scoring system, the MESI predicted amputation incorrectly in five patients and incorrectly predicted salvage in four patients.
In a second study, Bonanni and colleagues7 note that the sensitivity of the MESI to predict amputation was low at only 6%; specificity was 90%. Both Bonanni and colleagues7 and Roessler and coauthors6 note that many variables included as part of the MESI were unavailable at the time of the initial assessment of the patient, making it impossible to apply this scoring system accurately.
Predictive Salvage Index
The predictive salvage index (PSI) system was introduced by Howe and researchers.8 Patients with combined orthopedic and vascular injuries were studied. Only patients with lower extremity injuries were included. The PSI system is a simplified variation of the MESI. Points are given for the level of arterial injury, the degree of bone injury, the degree of muscle injury, and the interval from injury to the operating room. An initial retrospective analysis of the PSI was performed in 21 patients. All patients who achieved salvage had a PSI < 8. In contrast, seven of nine patients who required amputation scored 8 or greater. Conclusions from this retrospective study suggest that the sensitivity of the PSI was 78% and specificity was 100%. Bonanni and colleagues7 applied the PSI retrospectively to their data as well. They found that the PSI predicted amputation with a specificity of 70%, but sensitivity of only 33%. Roessler and coauthors6 also found that the PSI predicted amputation for two patients who ultimately had their limb salvaged and predicted salvage for five patients who ultimately required amputation.
Mangled Extremity Severity Score
The mangled extremity severity score (MESS) may be the most commonly applied and heavily researched lower extremity scoring index. The MESS system was introduced by Johansen and investigators9 in 1990. Only five criteria are included in the MESS: skeletal and soft-tissue injury, limb ischemia, shock, and age. The initial MESS analysis was based on a retrospective review of 26 mangled lower extremities. It was subsequently validated in a prospective trial at a different trauma center involving 26 patients.10 In both the original retrospective analysis and the prospective trial, a MESS score of less than 7 predicted salvage with 100% accuracy. Advantages of the MESS system include simplicity and a relatively more thorough validation compared with the PSI or MESI. However, it remains subjective and includes, in particular, consideration of contamination as a relevant issue surrounding the degree of energy.
MESS data retrospectively applied by Robertson11 to 152 patients with open fractures that required vascular or soft-tissue reconstruction were also considered. All patients with a MESS score of 7 or more eventually underwent amputation. Forty-three patients whose limbs were ultimately salvaged had a score of less than 7. Sixty-five patients underwent delayed amputation. Of these, 16 had a MESS of greater than 7 at the time of initial amputation. Based on the results of this study, the authors conclude that the MESS system had 100% specificity but lacked sensitivity.
Bonanni and colleagues7 applied the MESS system to their patients and found that the sensitivity of the scoring system to predict amputation was 22% and specificity was 53%. In contrast with the good specificity reported by Robertson11 and Johansen and investigators,9 Bonanni and colleagues7 believe that the reduced complexity used in the MESS system reduces sensitivity.
McNamara and investigators12 applied the MESS system to 33 patients, all of whom had severe open tibial fractures. The authors note a significant difference between the mean MESS of the amputation group compared with the salvage group. A score of greater than 7 accurately predicted amputation. The authors conclude that the MESS system was an objective and somewhat useful guide to assist in predicting the ultimate viability of the mangled lower extremity.
Slauterbeck and coauthors13 have considered application of the MESS to the upper extremity. Forty-three patients with mangled upper extremities were considered. All nine patients with a MESS of greater than 7 underwent amputation. Thirty-four patients with a MESS of less than 7 underwent successful salvage. The authors advocate the use of the MESS as an aid to augment the surgeon’s clinical experience.
Limb Salvage Index
Russell and colleagues proposed14 the limb salvage index (LSI). These authors retrospectively reviewed 70 lower extremity injuries. The authors consider factors such as arterial injury, nature of arterial injury, nature of nerve injury, type of bone injury, type of skin injury, nature of the muscle injury, degree of deep vein injury, and warm ischemic time. Fifty-one patients with successful limb salvage had an LSI of less than 6, and 19 patients who underwent amputation had a LSI of greater than 6. Approximately 95% of amputated limbs included disruption of the sciatic, tibial, or perineal nerves.14 Bonanni and colleagues7 apply the LSI retrospectively and conclude that it had a sensitivity of 61% and a specificity of 43%. The authors believe that the degree of detail of the LSI required application to be done in the operating room, and that accurate scoring was difficult at the time of initial assessment.
Nerve Injury, Ischemia, Soft-Tissue Injury, Skeletal Injury, Shock, and Age of Patient Scoring System
The Nerve Injury, Ischemia, Soft-Tissue Injury, Skeletal Injury, Shock, and Age of Patient Score (NISSSA), a modification of the MESS score, was introduced by McNamara and investigators12 and includes nerve injury, ischemia, soft-tissue injury and contamination, skeletal injury, blood pressure, and age. This system is a modification of the MESS system. The skeletal and soft-tissue components are separated, and nerve injury is added. The authors retrospectively compare the MESS score with the NISSSA system and note an improvement in sensitivity and specificity. Concerns about the NISSSA system relate to its additional complexity compared with the MESS system.
Current Evidence
The best current evidence related to the outcome of limb salvage or reconstruction is provided by the Lower Extremity Assessment Project (LEAP) study. LEAP considers civilian injuries in the U.S. population exposed to severe lower extremity trauma. The LEAP study is the largest study of its kind and includes patients managed up to 7 years. The LEAP study was designed to compare functional outcome in patients with limb-threatening injuries treated with either amputation or limb salvage. The authors in particular note no difference in functional outcome between patients who underwent limb salvage surgery or amputation, but note overall poor functional outcomes in both groups.15–17
The LEAP study provides grade 1 evidence and large patient numbers to use in comparing injury severity scores.18 A total of 556 patients with high-energy injuries were prospectively evaluated. Sixty-three patients had immediate amputations and 86 had delayed amputations such that 407 patients were treated with definitive limb salvage. The authors considered five injury severity scoring systems: The MESS, the LSI, the PSI, the NISSSA Scale, and the Hanover Fracture Scale 97. In all of the patient subgroups, low scores successfully predicted a high potential for limb salvage. However, the converse was not true; a high score was unable to predict amputation. The results suggest that use of these scores alone, in the absence of clinical judgment, was insufficient. The authors conclude that lower extremity scores at or above the amputation threshold should be used with caution in determining the fate of a lower extremity with a high-energy injury.
The same group also considers whether an insensate foot is an indicator for amputation.19 A subset of 55 patients from the larger LEAP group was found to have an insensate extremity at the time of presentation. Twenty-six were treated with amputation, and 29 with salvage. Overall, the patients treated with limb salvage who presented with an insensate extremity had no difference in functional outcomes at 12 or 24 months, compared with patients treated with limb salvage who had sensation in the sole of the foot. Furthermore, in the group of patients with a lack of sensation, no difference was found when comparing patients with limb salvage with those treated with amputation. The authors suggest that outcome in a patient with an insensate foot at the time of presentation could not be predicted accurately. Surprisingly, more than 50% of the patients who presented with an insensate foot who were treated with primary limb reconstruction ultimately regained sensation. As a result, the authors determined that initial plantar sensation was not prognostic of long-term plantar sensory status or functional outcome (Level I evidence).
A recent prospective study from Egypt assessed the results of arterial reconstruction on 62 patients.20 Overall limb salvage rates were 93.5%. Salvage rates were high even in the presence of high MESS and MESI scores. Limbs with MESS scores greater than 7 and MESI scores greater 20 were salvaged in 91% of cases (Level 1 evidence). These results agree with those of the LEAP study; that is, salvage can often be achieved even in limbs with high mangled extremity scores.
The evidence comparing outcome after limb salvage or amputation suggests that, overall, the results of the two treatment strategies may be similar. In the end, outcomes are generally poor and comparable with serious chronic illness.15–1721 In a recent study by Dagum and coworkers,21 92% of patients preferred an attempt at salvage.
AREAS OF UNCERTAINTY
Most of the best evidence comparing limb salvage with amputation is derived from the LEAP studies. From these studies, it is reasonable to make the following conclusions:(1) limb-threatening injuries severely impair functional outcome; (2) the outcome of amputation and limb salvage is generally equivalent between 1 and 5 years; (3) scoring systems are a useful ancillary tool but do not replace clinical judgment; and (4) lack of plantar sensation does not predict a poor outcome after salvage Tables 44-1 and 44-2).
| RECOMMENDATION | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
1 Hansen STJr. The type-IIIC tibial fracture: Salvage or amputation. J Bone Joint Surg Am. 1987;69:799-800.
2 Cole P. Case controversy open tibial fracture: Amputation versus limb salvage. J Orthop Trauma. 2007;21:67-69.
3 Kirk NT. Amputations. Clin Orthop. 1989;243:3-16.
4 Lange RH, Bach AW, Hansen STJr, et al. Open tibial fractures with associated vascular injuries: Prognosis for limb salvage. J Trauma. 1985;25:203-208.
5 Gregory RT, Gould RJ, Peclet M, et al. The mangled extremity syndrome (M.E.S.): A severity grading system for multisystem injury of the extremity. J Trauma. 1985;25:1147-1150.
6 Roessler MS, Wisner DH, Holcroft JW. The mangled extremity: When to amputate? Arch Surg. 1991;126:1243-1249.
7 Bonanni F, Rhodes M, Lucke JF. The futility of predictive scoring of mangled lower extremities. J Trauma. 1993;34:99-140.
8 Howe HRJr, Poole GVJr, Hansen STJr, et al. Salvage of lower extremities following combined orthopaedic and vascular trauma: A predictive salvage index. Am Surg. 1987;53:205-208.
9 Johansen K, Daines M, Howey T, et al. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma. 1990;30:568-573.
10 Helfet DL, Howey T, Sanders R, et al. Limb salvage versus amputation: Preliminary results of the Mangled Extremity Severity Score. Clin Orthop. 1990;256:80-86.
11 Robertson PA. Prediction of amputation after severe lower limb trauma. J Bone Joint Surg Br. 1991;73:816-818.
12 McNamara MG, Heckman JD, Corley FG. Severe open fractures of the lower extremity: A retrospective evaluation of the Mangled Extremity Severity Score (MESS). J Orthop Trauma. 1994;8:81-87.
13 Slauterbeck JR, Britton C, Moneim MS, et al. Mangled Extremity Severity Score: An accurate guide to treatment of the severely injured upper extremity. J Orthop Trauma. 1994;8:282-285.
14 Russell WL, Sailors DM, Whittle TB, et al. Limb salvage versus traumatic amputation: A decision based on a seven-part predictive index. Ann Surg. 1991;213:473-481.
15 Bosse MJ, MacKenzie EJ, Kellam J, et al. An analysis of outcomes of reconstruction or amputation of leg threatening injuries. N Engl J Med. 2002;347:1924-1931.
16 MacKenzie EJ, Bosse MJ, Castillo RC, et al. Functional outcomes following lower extremity amputation for trauma. J Bone Joint Surg Am. 2004;86:1636-1645.
17 MacKenzie EJ, Bosse MJ, Pollak AN, et al. Disability persists long-term following severe lower limb trauma: Results of a seven year follow-up. J Bone Joint Surg Am. 2005;87:1801-1809.
18 Bosse MJ, MacKenzie EJ, Kellam JF, et al. A prospective evaluation of the clinical utility of lower extremity injury severity scores. J Bone Joint Surg Am. 2001;83:3-14.
19 Bosse MJ, McCarthy ML, Jones AL, et alLower Extremity Assessment Project (LEAP) study group. The Insensate foot following severe lower extremity trauma: An indication for amputation? J Bone Joint Surg Am. 2005;87:2601-2608.
20 Elsharawy MA. Arterial reconstruction after mangled extremity: Injury severity scoring Systems are not predictive of limb salvage. Vascular. 2005;13:114-119.
21 Dagum AB, Best AK, Schemitsch EH, et al. Salvage after severe lower-extremity trauma: Are the outcomes worth the means? Plast Reconstr Surg. 1999;103:1212-1220.