Chapter 14 Managing the Allergic Child
Classification of the Problem
Children are usually classified by the allergic disorders from which they suffer. These are likely to include one or more of atopic dermatitis, atopic gastrointestinal disease (gastroesophageal reflux, food allergy, failure to thrive, eosinophilic esophagitis, etc.), atopic respiratory disease (asthma, rhinoconjunctivitis), anaphylaxis, urticaria (rarely allergic in childhood), and drug allergy. Children very rarely exhibit allergy to occupational allergens such as latex, nor to aspirin. An alternative classification is by allergen sensitivity – food allergy, inhalant allergy, or both.
Diagnosis
▪ History
A family history of atopic disease should be noted as well as a very detailed environmental history, feeding, pets, nursery placement, smoking in the home, etc. Many children lead complicated lives and live in a least two places – symptoms occurring at one only can give a clue to causation, for example the child who coughs when visiting his father who has a cat. Any treatments given, including alternative and complementary ones, need to be accurately recorded, plus the response to these.
Investigations
▪ Laboratory Tests
Treatment
▪ Pharmacologic Therapy
Corticosteroids
These act at multiple sites in the allergy cascade and are the single most effective treatment for rhinitis, asthma, and atopic dermatitis. Topical use in microgram amounts is possible via the inhaled nasal and dermal routes. However, since many allergic children suffer not only from asthma, but also rhinitis and atopic dermatitis and are treated with corticosteroids at all three sites the microgram amounts can become sufficient to cause adrenal suppression and other corticosteroid side effects. Thus continued monitoring of the child, particularly of growth which is a very sensitive measure of corticosteroid systemic effect, is mandatory. This is also a reason for just one allergist physician looking after the child rather than three separate physicians or surgeons each treating one site.
Antihistamines
Second generation antihistamines such as loratadine, cetirizine, desloratadine, levocetirizine, fexofenadine, and mizolastine have less sedative effects in most children and are equally efficacious as the first generation with no tachyphylaxis. Once daily administration of a long-acting antihistamine will ensure better compliance than medication which requires multiple daily doses. These are useful if rhinorrhoea and sneezing are main symptoms, or for conjunctivitis or urticarial rashes. Desloratidine, levocetirizine, and fexofenadine may also be beneficial for symptoms of nasal congestion.
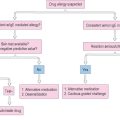
Epinephrine (adrenaline)
Each child should have a proforma detailing when and how to use this rescue treatment. The form needs to be countersigned by anyone who is looking after the child. The form should detail the likely allergen, the possible reactions and those which need merely antihistamines (localized itching or rash), compared to those which require epinephrine therapy such as a generalized reaction involving either collapse or airway problems.
▪ Immunotherapy
This is the only form of treatment which can alter the natural history of allergic disease.
1 Kalliomaki M, Salminen S, Poussa T, Arvilommi H, Isolauri E. Probiotics and prevention of atopic disease: 4-year follow-up of a randomized placebo-controlled trial. Lancet. 2003;361(9372):1869-1871.
2 Wilson DR, Torres Lima M, Durham SR. Sublingual immunotherapy for allergic rhinitis. Cochrane Database Syst Rev. 2003. CD002893.
3 Alves B, Sheikh A, Hurwitz B, Durham SR. Allergen injection immunotherapy for seasonal allergic rhinitis. Cochrane Database Syst Rev. 2000. CD001936.
4 Stevenson J. ETAC Study Group: Relationship between behavior and asthma in children with atopic dermatitis. Psychosom Med. 2003;65:971-975.
5 Diepgen TL/Early Treatment of the Atopic Child Study Group. long-term treatment with cetirizine of infants with atopic dermatitis: a multi-country, double-blind, randomized, placebo-controlled trial (the ETAC trial) over 18 months. Pediatr Allergy Immunol. 2002;13:278-286.
6 Stevenson J, Cornah D, Evrard P, et al. ETAC Study Group: long-term evaluation of the impact of the H1-receptor antagonist cetirizine on the behavioral, cognitive, and psychomotor development of very young children with atopic dermatitis. Pediatr Res. 2002;52:251-257.
7 Wolkerstorfer A, Wahn U, Kjellman NI, Diepgen TL, De Longueville M, Oranje AP. Natural course of sensitization to cow’s milk and hen’s egg in childhood atopic dermatitis: ETAC study group. Clin Exp Allergy. 2002;32:70-73.
8 Warner JO, on behalf of the ETAC Study Group. A double-blinded, randomized, placebo-controlled trial of cetirizine in preventing the onset of asthma in children with atopic dermatitis: 18 months’ treatment and 18 months’ posttreatment follow-up. J Allergy Clin Immunol. 2001;108:929-937.
9 Simon FE. Prospective, long-term safety evaluation of the H1-receptor antagonist cetirizine in very young children with atopic dermatitis. ETAC Study Group. Early Treatment of the Atopic Child. J Allergy Clin Immunol. 1999;104(2 Pt 1):433-440.
10 Bustos GJ, Bustos D, Romero O. Prevention of asthma with ketotifen in preasthmatic children: a three-year follow-up study. Clin Exp Allergy. 1995;25:568-573.
11 Iikura Y, Naspitz CK, Mikawa H, et al. Prevention of asthma by ketotifen in infants with atopic dermatitis. Ann Allergy. 1992;68:233-236.
12 Kharitonov SA, Walker L, Barnes PJ. Repeatability of standardized nasal nitric oxide measurements in healthy and asthmatic adults and children. Respir Med. 2005;99:1105-1114. EPub 2005 Mar 17.
13 Corbelli R, Bringolf-Isler B, Amacher A, Sasse B, Spycher M, Hammer J. Nasal nitric oxide measurements to screen children for primary ciliary dyskinesia. Chest. 2004;126:1054-1059.
14 Kurukulaaratchy RJ, Matthews S, Arshad SH. Defining childhood atopic phenotypes to investigate the association of atopic sensitization with allergic disease. Allergy. 2005;60:1280-1286.
15 Hahn EL, Bacharier LB. The atopic march: the pattern of allergic disease development in childhood. Immunol Allergy Clin North Am. 2005;25:231-246.
16 Spergel JM. Atopic march: link to upper airways. Curr Opin Allergy Clin Immunol. 2005;5:17-21.
17 Gilbert TW, Morgan WJ, Zeiger RS, et al. Atopic characteristics of children with recurrent wheezing at high risk for the development of childhood asthma. J Allergy Clin Immunol. 2004;114:1282-1287.
18 Mastrandrea F. The potential role of allergen-specific sublingual immunotherapy in atopic dermatitis. Am J Clin Dermatol. 2004;5:281-294.
19 Heymann PW, Carper HT, Murphy DD, et al. Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezing. J Allergy Clin Immunol. 2004;114:239-247.
20 Gruber C, Niggemann B, Wahn U. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol. 2004;113:925-931.
21 Leung DY, Boguniewicz H, Howell MD, Nomura I, Hamid QA. New insights into atopic dermatitis. J Clin Invest. 2004;113:651-657.
22 Wuthrich B, Schmid-Grendelmeier P. The atopic eczema/dermatitis syndrome. Epidemiology, natural course, and immunology of the IgE-associated (“extrinsic”) and the nonallergic (“intrinsic”) AEDS. J Investig Allergol Clin Immunol. 2003;13:1-5.
23 Yimyaem P, Chongsrisawat V, Vivatvakin B, Wisedopas N. Gastrointestinal manifestations of cow’s milk protein allergy during the first year of life. J Med Assoc Thai. 2003;86:116-123.
24 Austin JB, Kaur B, Anderson HR, et al. Hay fever, eczema, and wheeze: a nationwide UK study (ISAAC, international study of asthma and allergies in childhood). Arch Dis Child. 1999;81:225-230.