Malocclusion after Orthodontics and Orthognathic Surgery
Prevention and Treatment Pitfalls
Sagittal Split Ramus Osteotomies of the Mandible: Skeletal Stability and Relapse
Immediate (Early) Malocclusion after Sagittal Split Ramus Osteotomies
An immediate (early) malocclusion that is recognized either intraoperatively or soon after surgery (i.e., during the first several days or weeks afterward) will occur after sagittal split ramus osteotomies of the mandible unless each of the following intraoperative conditions is met* (Figs. 17-1 through 17-4):
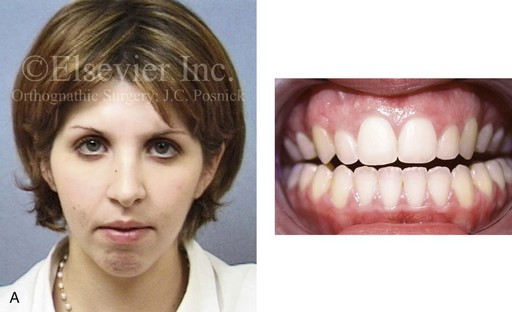


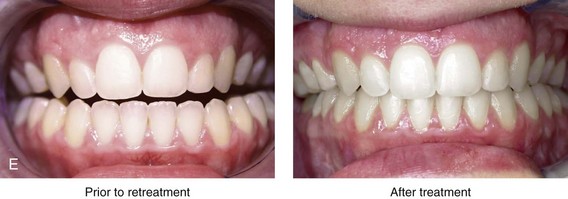
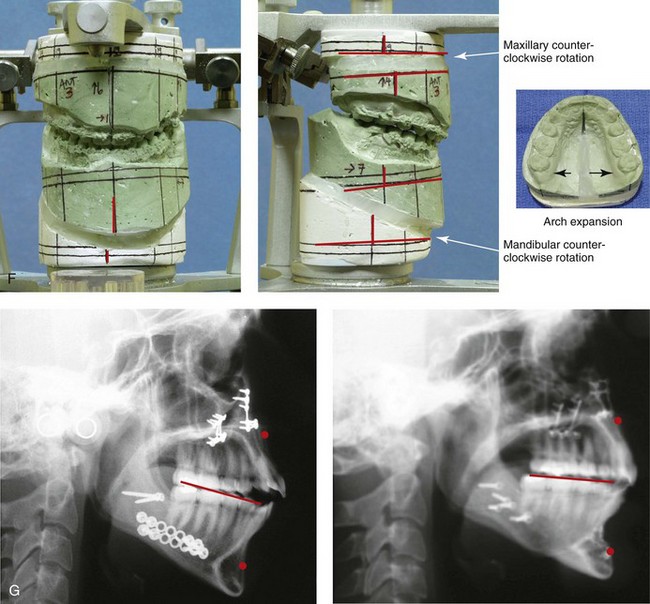
Figure 17-1 A woman in her late 20s was referred by her orthodontist for surgical evaluation. She suffered with masticatory muscle discomfort while chewing and had a jaw deformity, malocclusion, and a lifelong history of obstructed nasal breathing. A long face Class II growth pattern was evident from her childhood onward. She had undergone attempted orthodontic growth modification and then a camouflage approach, without success. She then underwent orthodontics (including upper bicuspid extractions) and surgery at another institution; this included a Le Fort I osteotomy and bilateral ramus osteotomies. Analysis confirmed both inadequate positioning of the jaws at the time of operation and then dental relapse of the maxillary arch form over time. When she presented to this surgeon, her clinical problems included the following:

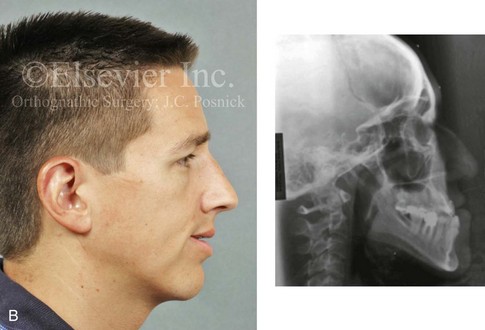


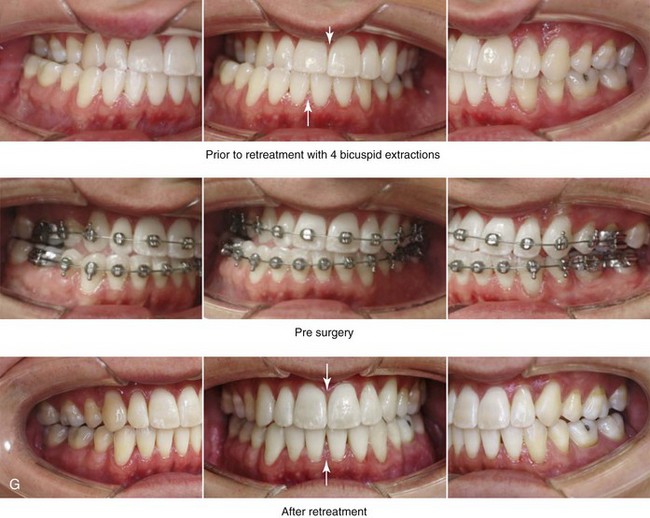
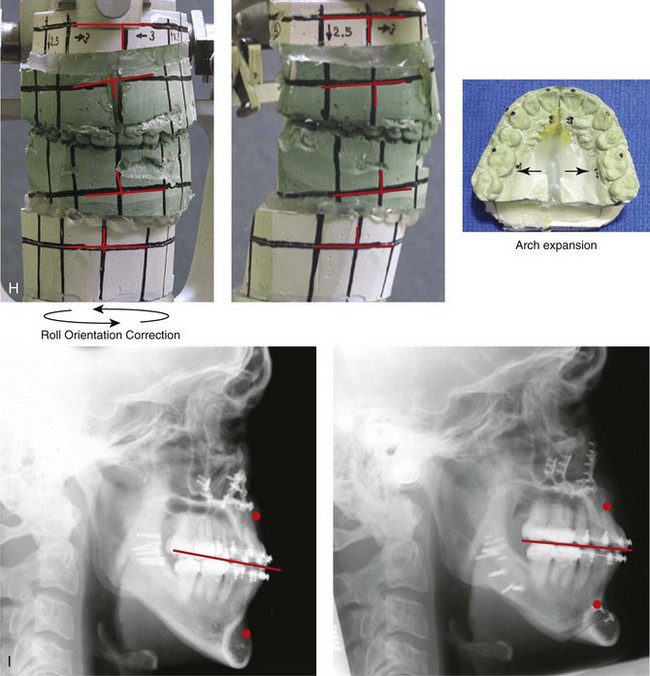
Figure 17-2 A man with a developmental jaw deformity that was characterized as an asymmetric mandibular excess growth pattern (i.e., hemimandibular elongation) presented for treatment. His orthodontist originally attempted growth modification followed by orthodontic camouflage that included four bicuspid extractions, without success. When he was 19 years old, the patient underwent further orthodontics and a surgical approach at another institution. His jaw surgery at the time included maxillary Le Fort I osteotomy and bilateral vertical oblique ramus osteotomies. An initial satisfactory surgical result was not achieved, and further orthodontic camouflage was attempted. During ongoing orthodontic treatment, alveolar bone loss and gingival recession occurred along the buccal aspect of the posterior maxillary dentition and the labial aspect of the anterior mandibular dentition. At the time of referral to this surgeon, the patient was 35 years old; thus, it had been 16 years since his suboptimal treatment. Evaluations were arranged with a periodontist; an orthodontist; a speech therapist; and an ear, nose, and throat specialist. After periodontal treatment, orthodontic decompensation was carried out in preparation for reconstruction. The patient’s surgery included maxillary Le Fort I osteotomy in segments (cant correction, transverse expansion, and minimal horizontal advancement); sagittal split ramus osteotomies (asymmetry correction and minimal horizontal advancement); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty and inferior turbinate reduction. A, Frontal and occlusal views before retreatment. B, Current profile view shown next to a lateral cephalometric radiograph taken before original surgery, when the patient was 19 years old. C, Frontal views in repose before and after retreatment. D, Frontal views with smile before and after retreatment. E, Oblique facial views before and after retreatment. F, Profile views before and after retreatment. G, Occlusal views before orthodontic retreatment, with orthodontic decompensation in progress, and after retreatment. H, Articulated dental casts after analytic model planning. I, Lateral cephalometric radiographs after first surgery and then after retreatment.
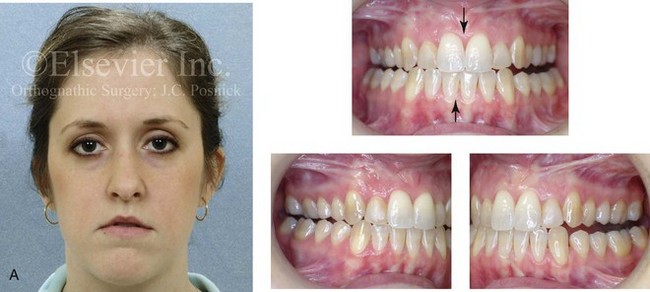

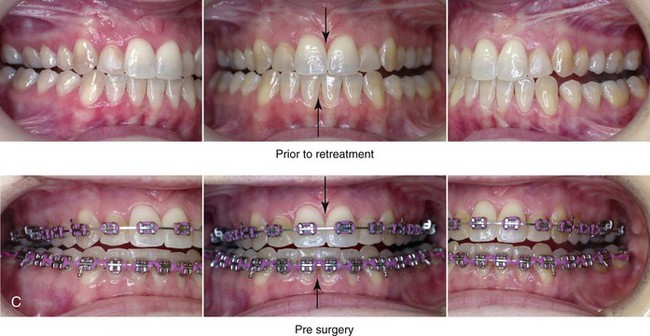
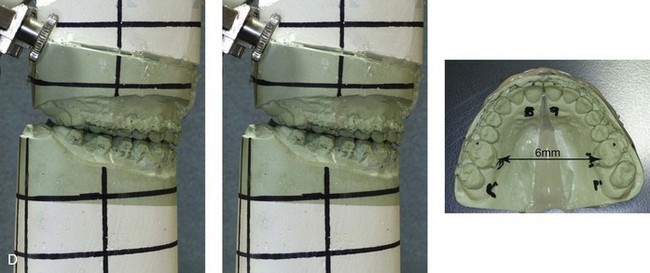

Figure 17-3 A 28-year-old woman was referred by her orthodontist for the evaluation of residual malocclusion and facial asymmetry. Eight years earlier, the patient had presented with an asymmetric mandibular excess growth pattern and underwent a combined orthodontic and surgical approach at another institution. The surgery included maxillary Le Fort I osteotomy (three segments) with iliac interpositional grafting in combination with bilateral sagittal split ramus osteotomies. Immediately after surgery, the occlusion that had been achieved was recognized to be unsatisfactory. The patient was taken back to the operating room 1 week later for the removal of the fixation of the right ramus of the mandible, the adjustment of the occlusion, and the reapplication of fixation. The occlusion remained unsatisfactory. Six months later, the patient was taken back to the operating room again, where she underwent a left vertical oblique ramus osteotomy without fixation followed by 6 weeks of intermaxillary fixation. Over the long term, the occlusion remained unsatisfactory, and the patient also had a minor degree of facial asymmetry as seen in the frontal view. At the time of referral to this surgeon, the patient stated that she hoped for the correction of the occlusion and an improvement in her current lip asymmetry. The decision was made to not operate on the mandible again. Options to improve the occlusion included maxillary Le Fort I osteotomy in segments versus surgically assisted rapid palatal expansion. Segmental maxillary surgery with immediate repositioning and interpositional grafting was carried out. The occlusion was maintained with a prefabricated acrylic splint for 6 weeks, which was followed by the immediate placement of a transpalatal arch. A, Frontal facial and occlusal views before retreatment. B, Profile facial view and lateral cephalometric radiograph before retreatment. C, Occlusal views before retreatment and preoperatively with orthodontic appliances in place. D, Articulated dental casts that indicate surgical planning. E, Demonstration of the use of the maxillary surgical model to construct a transpalatal arch wire for immediate placement at the time of splint removal (i.e., 5 weeks after surgery). The roof of the patient’s mouth is shown with the transpalatal wire in place in accordance with the surgical model. The use of orthodontic mechanics for 6 months to actively maintain the arch width achieved at operation is useful to limit a tendency toward relapse. It is also important to limit any orthodontic mechanics that may position the teeth outside of the alveolar housing, because this situation will be prone to long-term dental relapse.
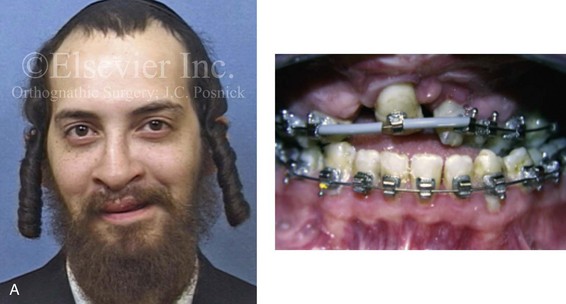
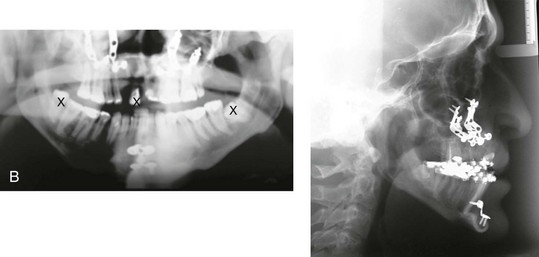
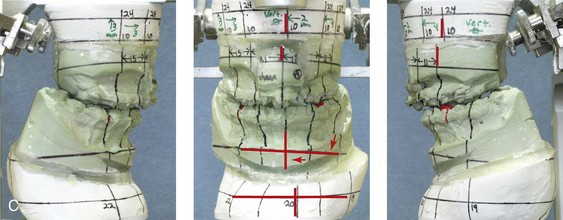


Figure 17-4 A 21-year-old man who was born with bilateral cleft lip and palate arrived for surgical evaluation. He had undergone suboptimal orthognathic surgery (Le Fort I osteotomy and osseous genioplasty) at another institution 4 years earlier. The history, physical examination, and radiographs suggested a combination of both unfavorable initial surgical healing and late dental relapse. The patient was referred to this surgeon and underwent a comprehensive surgical and dental rehabilitative approach. After periodontal evaluation and treatment, orthodontic decompensation was undertaken. The patient’s surgery included maxillary Le Fort I osteotomy in three segments with differential repositioning (cant correction, closing down of cleft dental gap, closure of fistula, horizontal advancement, counterclockwise rotation, and vertical adjustment); bilateral sagittal split ramus osteotomies (asymmetry correction); and septoplasty and inferior turbinate reduction. This was followed by planned prosthetic rehabilitation of the maxillary and mandibular arches and ongoing periodontal surveillance. A, Frontal and occlusal views at the time of surgical evaluation (i.e., 4 years after the suboptimal orthognathic procedures at another institution). B, Cephalometric and Panorex radiographs at the time of surgical evaluation. C, Articulated dental casts that indicate analytic model planning. D, Frontal views with smile before and after retreatment including dental rehabilitation. E, Occlusal views before and after retreatment including dental rehabilitation.
1. The proximal segment is successfully split from the distal mandible (i.e., no “bad” split) on each side (right and left).
2. The distal mandible is placed in the preferred occlusion and tightly held in intermaxillary fixation (IMF). Unless the natural occlusion between the upper and lower teeth is precise (i.e., without centric relation–centric occlusion slides), the IMF should be maintained with the use of an accurate prefabricated acrylic splint.
3. Each proximal segment is positioned with the condyle seated in the terminal hinge position. Each proximal segment is then secured to the distal segment with the use of either passively placed bicortical screws or monocortical screws and plates. This is accomplished without torquing or overseating the proximal segment. The following conditions should be present:
• Adequate bone contact between the proximal and distal segments, without compression or torquing
• Appropriate alignment of the proximal and distal segments to limit the rotation or torquing of each proximal segment.
4. With the release of IMF, the mandible is put through the range of motion to confirm the adequate stability of the skeletal fixation across the ramus osteotomy site on each side.
5. The occlusion is then checked for any centric relation–centric occlusion discrepancies or other causes of malocclusion. If a discrepancy is seen, each proximal segment must be released of its fixation and then again repositioned until the planned, stable, and reproducible occlusion is achieved (i.e., Steps 1 through 5 are repeated, as needed).
Late Malocclusion after Sagittal Split Ramus Osteotomies
Malocclusion after the successful initial healing of sagittal split ramus osteotomies is the result of either skeletal or dental causes.* Skeletal causes may include condylar resorption (see Chapter 36); remodeling or malunion (i.e., relapse) at the osteotomy site; or continued mandibular growth; these conditions are all described in more detail later in this chapter. Dental causes of malocclusion after sagittal split ramus osteotomies are often not appreciated until much later, but they are generally related to the unstable orthodontic positioning of the teeth outside of the boundaries of the alveolar process before or after surgery; this is discussed later in this chapter (see also Chapters 5 and 6).208
Condylar Resorption after Orthognathic Surgery
Although it is rare, idiopathic condylar resorption may present after orthognathic surgery (maxillary or mandibular osteotomies), routine orthodontic treatment, or routine dental procedures; it may also occur spontaneously and not in association with any specific form of treatment (see Chapter 36).12,117,118,143,144,148,159,202,212,237,278,327 Condylar resorption is usually bilateral, symmetric, and seen in young females who are between 15 and 35 years old. Although no agreed upon etiology has been delineated for idiopathic condylar resorption, hormonal and autoimmune causes are suspected (see Chapter 36). Unilateral condylar resorption in association with compressive forces may also be seen after the excessive use of elastics in an attempt to overcome residual malocclusion. The clinical setting may involve heavy elastic use either as part of an orthodontic camouflage approach to avoid surgery (Fig. 17-5) or after orthognathic procedures that did not achieve the desired occlusion. In either case, heavy compressive forces on the condyle may result in temporomandibular joint symptoms followed by condylar resorption with a loss of condylar (posterior facial) height.


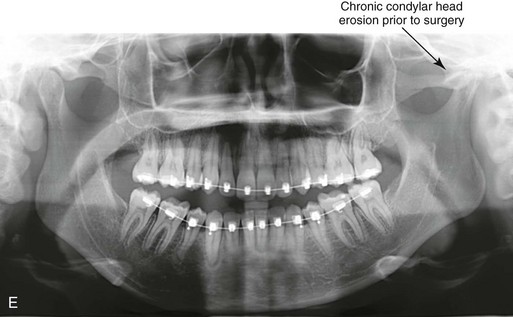
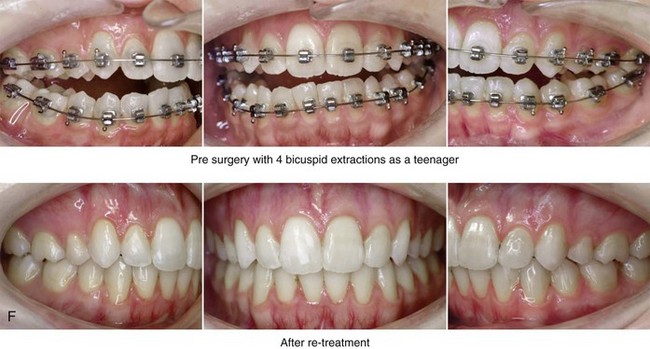
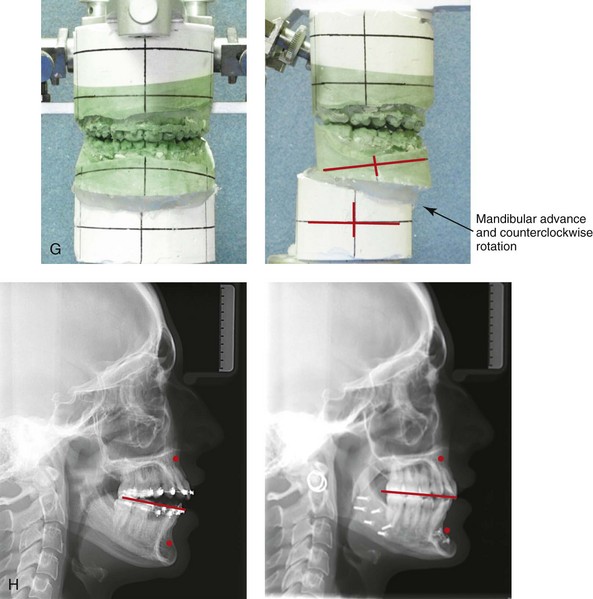
Figure 17-5 A 23-year-old woman was referred for surgical evaluation. During her high school years, she was recognized as having a malocclusion, and she underwent four bicuspid extractions and orthodontic treatment to neutralize the occlusion. During her college years, she experienced a closed lock of her jaw as a result of a dislocated disc within the left temporomandibular joint. After 3 months of conservative management, the patient underwent arthroscopy with lysis of adhesions. With a recurrence of the closed lock attributed to the disc in the left temporomandibular joint, she underwent discectomy and fat graft interposition. A review of the patient’s earlier medical records, including dental models and radiographic analyses, confirmed the primary cause of current malocclusion to be a longstanding developmental jaw deformity that was initially treated with orthodontics alone. Dental relapse had occurred, and the patient’s temporomandibular disorder was likely the result of unstable intercuspation. The relief of the temporomandibular disorder was achieved through an open-joint procedure but with the additional loss of posterior facial height and mandibular asymmetry. The patient was referred to this surgeon and agreed to a comprehensive orthodontic and orthognathic approach. The patient’s procedures included bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation) and osseous genioplasty (horizontal advancement). Facial balance and satisfactory occlusion were achieved and maintained without the return of temporomandibular disorder. A, Frontal views in repose before and after retreatment. B, Frontal views with smile before and after retreatment. C, Oblique facial views before and after retreatment. D, Profile views before and after retreatment. E, Panorex radiograph before retreatment. This image indicates a chronic flattening of the left condylar head. F, Occlusal views before retreatment, with orthodontics in progress, and after successful retreatment. G, Articulated dental casts indicate analytic model planning. H, Lateral cephalometric radiographs before and after successful retreatment.
Continued Growth of the Mandible after Orthognathic Surgery
Under normal conditions, the mandible is the last bone in the craniofacial skeleton to complete growth. In general, mandibular growth should be complete between the ages of 14 and 16 years in girls and between the ages of 16 and 18 years in boys. Chronologic and skeletal age will vary from individual to individual, and mandibular growth in men may continue beyond the age of 18 years, but this is uncommon. Jaw growth in girls is usually complete within 2 years after the onset of regular menses. The completion of jaw growth may be assessed in the following ways: 1) via the growth-plate analysis of a hand and wrist radiograph 2) via the analysis of a quantitative condylar head bone scan in comparison to a lumbar vertebra (L2) 3) via the analysis of the mandibular length with the use of serial lateral cephalometric radiographs 4) via the analysis of cervical vertebral maturation with the use of serial lateral cephalometric radiographs 5) via the assessment of serial dental models in centric relation or 6) via the assessment of serial occlusal photographs taken in centric relation.*
Mandibular growth in individuals with micrognathia is generally complete at an earlier age than it is among normal “average” mandibular growers. Alternatively, the cessation of lower jaw growth in individuals with true mandibular excess may occur later than it does in average individuals (Figs. 17-6 and 17-7) (see Chapter 20); this is especially true for individuals with asymmetric mandibular excess growth anomalies (see Chapter 22). Alternatively, the individual with a typical Class II long face growth pattern (i.e., vertical maxillary excess combined with mandibular deficiency) can be assumed to have a normal mandibular growth vector without a tendency for late development (see Chapter 21). I believe that, if the long face patient’s chronic nasal obstruction problem is simultaneously managed at the time of orthognathic surgery (i.e., septoplasty, inferior turbinate reduction, the widening of a tight nasal aperture, and the lowering of the nasal floor), further pathologic vertical growth is also likely to be arrested (see Chapter 10).
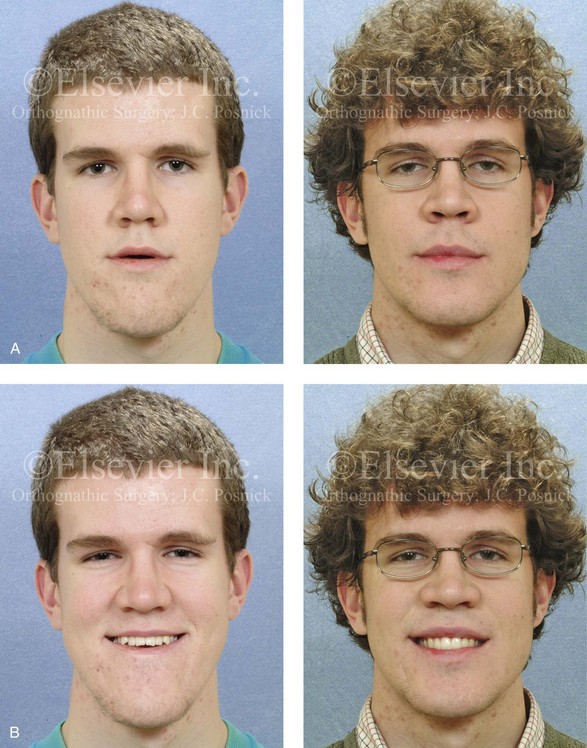
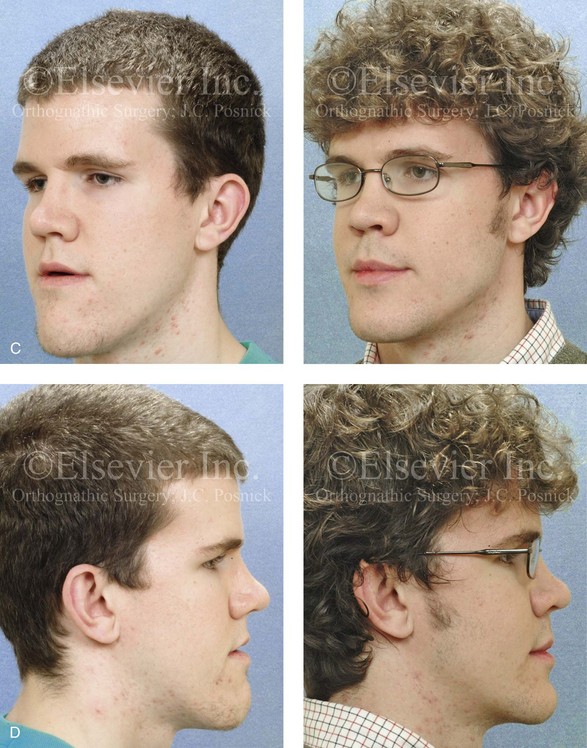
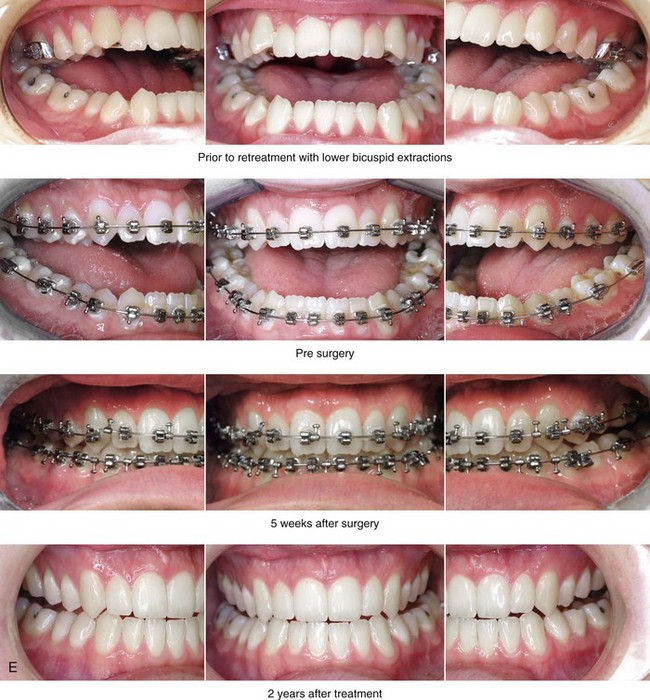
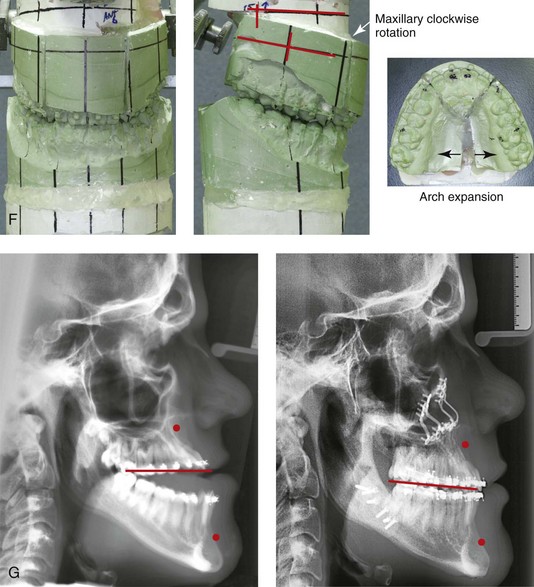
Figure 17-6 An 18-year-old man with malocclusion and a lifelong history of obstructed nasal breathing was referred for the surgical evaluation. The pattern of deformity was maxillary deficiency in combination with relative mandibular excess, which resulted in a severe Class III negative overjet anterior open bite. He had previously undergone growth modification and camouflage orthodontics including lower bicuspid extractions, without success. After a thorough evaluation, he underwent 12 months of orthodontic decompensation followed by jaw and intranasal surgery. The patient’s surgery included Le Fort I osteotomy in segments (horizontal advancement, clockwise rotation, transverse widening, and correction of the arch form) with interpositional grafting; sagittal split ramus osteotomy (minimal counterclockwise rotation); osseous genioplasty (bone burring and recontouring); and septoplasty and inferior turbinate reduction. These procedures were followed by finishing orthodontics. The occlusion achieved during the operation and maintained at the patient’s debracketing 6 months later was ideal. By 2 years after surgery, however, a symmetric Class III negative overjet malocclusion had recurred. A, Frontal views before and 2 years after reconstruction. B, Frontal views with smile before and 2 years after reconstruction. A review of the 2-year postoperative dental models indicated stable maintenance of the arch width and of the correction of the curve of Spee. The models could be articulated into a similar occlusion as had been achieved at the time of operation. Therefore, the cause of change in occlusion could not be attributed to the segmental osteotomies or dental relapse. The cause of the recurrent malocclusion was felt to be either ongoing mandibular growth or Le Fort I osteotomy site relapse. An analysis of the postoperative cephalometric radiographs—which showed an increase in the sella–nasion–B-point angle and the maintenance of the sella–nasion–A-point angle—confirmed maxillary stability. Ongoing mandibular growth was the cause of the malocclusion. Treatment options included Le Fort I osteotomy (3-mm advancement) versus sagittal split ramus osteotomies (3-mm set-back). The patient was pleased with the functional improvements (i.e., swallowing, speech, chewing, lip closure/posture, and breathing) and the enhanced facial aesthetics without temporomandibular disorders. He elected to receive no further treatment. C, Oblique facial views before and 2 years after reconstruction. D, Profile views before and 2 years after reconstruction. E, Occlusal views before retreatment, immediately before surgery, 5 weeks after surgery, and 2 years after treatment. F, Articulated dental casts after analytic model planning. G, Lateral cephalometric radiographs before and after treatment.

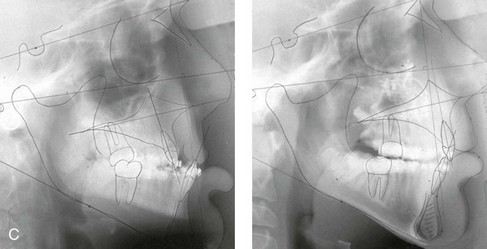
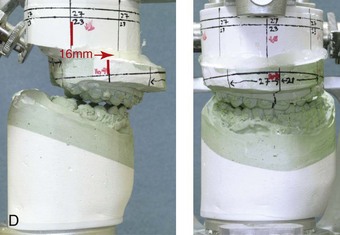

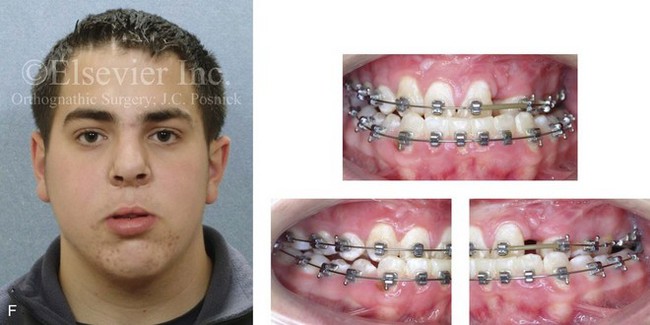
Figure 17-7 A 13-year-old boy born with bilateral cleft lip and palate arrived for surgical evaluation with a severe cleft jaw deformity. He underwent primary lip and palate repair, a pharyngeal flap procedure, bone grafting, and a columella lengthening procedure at another institution. He was referred to this surgeon with severe maxillary hypoplasia that was causing profound effects on his speech articulation, chewing ability, breathing, and self-esteem. For this reason, early jaw reconstruction was chosen. He underwent maxillary Le Fort I osteotomy (horizontal advancement and vertical lengthening with interpositional [iliac] bone grafting). This was carried out with the understanding that further maxillary growth should not be expected, whereas mandibular growth would likely continue and result in a recurrent Class III. A review of the longitudinal cephalometric radiographs after surgery confirmed no significant horizontal maxillary relapse but ongoing mandibular growth. A, Frontal views with smile before and 1 year after surgery just before the removal of the orthodontic appliances. B, Oblique facial views before and 1 year after surgery. C, Lateral cephalometric views before and 1 year after surgery. D, Articulated dental casts that indicate analytic model planning. E, Occlusal views before and 1 year after surgery, just before debanding. F, Facial and occlusal views from when the patient was 18 years old (i.e., 5 years after Le Fort I advancement) that indicate recurrent Class III malocclusion as a result of ongoing mandibular growth.
Ramus Remodeling and Malunion after Sagittal Split Ramus Osteotomy
With the use of rigid internal fixation (e.g., bicortical screws or plates and screws), the remodeling and malunion of the ramus osteotomy site is believed to be an uncommon cause of relapse.109,115,179,206,236,248,302,324 Although infrequent, infection that has led to sequestration (e.g., of the buccal shelf of the proximal segment) and malunion has been reported. In most clinical settings, there is little evidence to support the concept of late relapse at the ramus osteotomy site after satisfactory initial healing has occurred (by approximately 5 weeks). However, limited bone contact or inadequate fixation of the bony segments may cause initial fibrous union followed by malunion and resulting malocclusion. This would be documented as morphologic change in the mandibular angle (i.e., clockwise rotation of the distal segment) in the presence of unchanged condylar morphology (i.e., no ongoing erosion of the condylar head). There would also be measurable change in either the mandibular length (i.e., as measured from the condyle to the pogonion) or the sella–nasion–B-point angle documented during the analysis of the serial cephalometric radiographs after surgery.
Proffit and colleagues do make a case for ramus remodeling with relapse after mandibular set-back when managing a Class III skeletal pattern.248 These authors believe that, when the orthognathic procedure for the management of a Class III skeletal pattern is a mandibular set-back only versus a two-jaw surgery (i.e., with the primary movement being maxillary advancement in combination with only minor mandibular adjustment), then relapse at the ramus osteotomy site is a common occurrence. In a recent clinical study, Proffit and colleagues confirmed that—despite improvements in surgical fixation techniques (i.e., rigid fixation versus intraosseous wires and IMF)—when mandibular set-back only procedures are carried out for a Class III malocclusion, skeletal instability is often significant. They confirmed better long-term skeletal and occlusal stability when two-jaw surgery is performed for the management of Class III skeletal patterns (i.e., maxillary advancement with limited mandibular set-back).251
Le Fort I Osteotomy: Skeletal Stability and Relapse
Immediate (Early) Malocclusion after Le Fort I Osteotomy
Immediate (early) malocclusion that is recognized either intraoperatively or during the first several days or weeks after surgery may occur after a Le Fort I osteotomy unless the following intraoperative conditions are met (see Figs. 17-1 through Fig 17-4)*:
1. After Le Fort I down-fracture osteotomy, full mobilization of the maxilla and the segments (if segmentation has been carried out) is accomplished before the placement of fixation.
2. An accurate prefabricated acrylic splint is secured to the maxillary occlusal surfaces. The splint stabilizes the new maxillary arch form (i.e., the arch width and the curve of Spee) when segmental osteotomies are carried out.
3. After the securing of the splint to the maxillary dentition, IMF is applied to establish the new horizontal position of the maxilla; the dental midline (yaw orientation); the preferred maxillary plane orientation (pitch orientation); and any cant correction (roll orientation) required.
4. With the condyles seated in the terminal hinge position and IMF established via the prefabricated splint, the maxillomandibular complex is rotated until the desired vertical position of the maxilla is achieved.
• Bony prematurities are common with maxillary impaction. It is easy for the surgeon to overlook interferences in the posterior region of the lateral nasal walls just medial to the descending palatine vessels (see Fig. 15-25, A and B).
• Care should be taken to prevent premature contacts across the Le Fort I osteotomy site, which are followed by a “slide” into maximum bone contact during further vertical closure of the maxillomandibular complex. This would cause condylar displacement with malocclusion that should be recognized at the release of the IMF. The malocclusion would typically present as either a symmetric anterior open bite (if both condyles are displaced) or as an asymmetric lateral shift in the bite (if one condyle is displaced).
5. There must be adequate bone contact across the osteotomy site after the maxilla is stabilized with plate and screw fixation into the desired position. If not, an interpositional graft of sufficient quality should be placed and secured (see Chapters 15 and 18). Without adequate bone contact across the osteotomy site, fibrous union may occur (see Chapter 16). Another possibility is that of initial bony union with relapse (i.e., malunion) occurring as full healing proceeds during the 6 to 12 months after surgery, thereby resulting in late malocclusion.
6. Adequate plate and screw stabilization of the maxilla generally requires the placement of titanium fixation at each pyriform rim and each zygomatic buttress (see Fig. 15-26). When interpositional grafts are required, additional titanium fixation is placed from the superior maxilla and extended across the graft to the dentate segment (see Fig. 15-29, A, B, and C). Additional plate and screw fixation may also be placed horizontally across any interdental osteotomies, if needed.
7. With release of the IMF, the occlusion is checked as the mandible is rotated (opened and closed) with the condyles seated in the terminal hinge position. The occlusion must evenly contact and fit passively into the splint. If not, the plate and screw fixation across the Le Fort I osteotomy is released. Any bony interference is then identified and removed. The maxilla is again repositioned and the fixation reapplied (i.e., repeat Steps 4 through 7) until the planned occlusion is achieved and confirmed.
Late Malocclusion after Le Fort I Osteotomy
Skeletal causes of a late malocclusion after Le Fort I osteotomy may include the following: 1) remodeling (relapse) at the Le Fort I osteotomy site (as described later in this chapter) 2) fibrous union at the Le Fort I osteotomy site (as described later in this chapter) 3) remodeling (relapse) at the segmental osteotomy sites (as described later in this chapter) 4) condylar resorption (as described previously in this chapter and in Chapter 36)143 and 5) continued mandibular growth (as described previously in this chapter; see Figs. 17-6 and 17-7).* Dental causes of malocclusion after Le Fort I osteotomy are often not realized until much later. They are related to the unstable orthodontic positioning of the teeth outside of the boundaries of the alveolar process before or after surgery (as described later in this chapter and in Chapters 5 and 6).208
The precise cause of relapse at the Le Fort I osteotomy site is often difficult to pinpoint, but it is generally related to the following: 1) inadequate mobilization of the down-fractured maxilla before the placement of fixation 2) inadequate bone contact across the osteotomy site after the fixation is applied 3) inadequate (non-rigid) plate and screw fixation across the osteotomy site or 4) excessive occlusal forces or movement transmitted across the osteotomy site during initial healing.†
Fibrous union of the maxilla after Le Fort I osteotomy is an infrequent occurence. When it occurs, expect to find painless mobility of the upper jaw, with or without malocclusion. Risk factors should be recognized, at which point surgical techniques and postoperative management can be adjusted to limit this complication (see Fig. 16-21). The combination of extensive horizontal advancement and vertical lengthening will result in large osteotomy site defects with limited bone contact. Failure to form adequate bony bridges at the healing sites is likely to result in delayed healing, fibrous union, or late relapse. Negative influences on bone healing at the Le Fort I osteotomy site may include the following: (1) injury to flap circulation (2) thin osteoporotic bone at the zygomatic buttress and the pyriform rims, with inadequate fixation and (3) the decision to not place interpositional grafts when the bone gaps are of critical size. Additional postoperative healing risk factors include the following: (1) infection or wound dehiscence after surgery (2) the presence of a heavy occlusion (e.g., grinding, clenching) (3) too rapid of a return to normal chewing forces (4) excessive mouth opening against intermaxillary elastics and (5) the breakage (stress fracture) of the fixation plates. Systemic conditions that are known risk factors for poor bone healing include the following: (1) diabetes (2) collagen disease (3) vascular disease (4) osteoporosis or bisphosphonate use (5) nicotine abuse (6) poor nutritional status; and (7) previous radiation treatment.
Relapse across the segmental maxillary osteotomy sites after palatal widening is generally related to the following: (1) inadequate mobilization of the segments (2) inadequate surgical splinting of the new arch shape during initial healing (i.e., the first 5 weeks) (3) inadequate or unstable interdigitating occlusion between the maxillary and mandibular teeth after the splint is removed or (4) inadequate medium-term orthodontic maintenance (i.e., lasting approximately 6 months) with an appropriate appliance after the surgical splint is removed (see Figs. 17-3 and 17-8). Transverse relapse after the removal of the surgical splint may also occur as a result of the use of counterproductive intermaxillary elastic forces. For example, the use of vertical elastics placed on the buccal brackets of the upper and lower molars in an attempt to close posterior open bites may result in the simultaneous unintended collapse of the arch width.


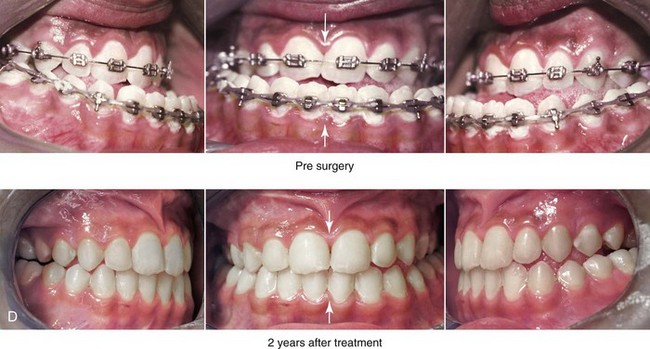
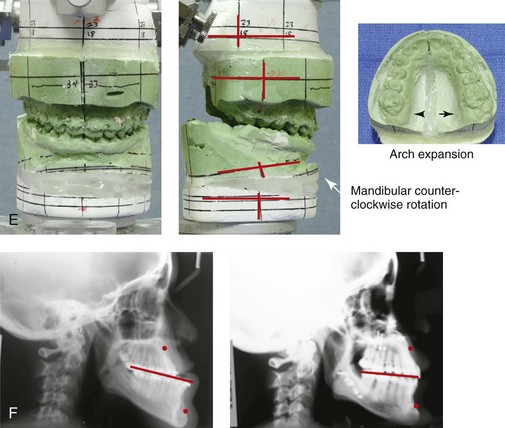
Figure 17-8 A 15-year-old high school student was referred by her orthodontist for surgical evaluation of a long-standing developmental jaw deformity with malocclusion and a lifelong history of obstructed nasal breathing. The pattern of growth disturbance was maxillary deficiency in combination with relative mandibular excess, and this resulted in a Class III negative overjet anterior open bite malocclusion. The patient had undergone growth modification and camouflage orthodontics, without success. Referral to this surgeon was followed by orthodontic decompensation in conjunction with jaw and intranasal surgery and then finishing orthodontics. The patient’s surgery included maxillary Le Fort I osteotomy in two segments (horizontal advancement, transverse widening, and vertical lengthening); sagittal split ramus osteotomies (counterclockwise rotation and minimal horizontal advancement); and septoplasty and inferior turbinate reduction. The surgical occlusion that was initially achieved at operation and then maintained during the early phase of healing was stable. By 6 to 12 months after surgery, a degree of posterior crossbite had recurred. A, Frontal views with smile before and after reconstruction. B, Oblique facial views before and after reconstruction. A review of the postoperative dental models indicated intermolar transverse constriction as compared with what was surgically planned, executed, and achieved at 5 weeks after surgery, when the prefabricated splint was removed. A review of the dental models confirmed a combination of skeletal and dental relapse that resulted in maxillary arch constriction. In retrospect, the postoperative orthodontic mechanics of the labial arch wire to maintain the surgically achieved arch width were not adequate. The use of a transpalatal wire or an acrylic palatal plate maintained for 6 months after surgery may have prevented maxillary arch form relapse after the surgical splint was removed (i.e., 5 weeks after surgery). Treatment options for the residual malocclusion include redo Le Fort I segmental osteotomies with expansion versus surgically assisted rapid palatal expansion. The patient was pleased with the improvements (i.e., chewing, speech articulation, lip closure/posture, and breathing) and the enhanced facial aesthetics. She was left with a functional occlusion without centric relation–centric occlusion discrepancies or temporomandibular disorder. She elected to receive no further treatment. C, Profile views before and after reconstruction. D, Occlusal views with orthodontic decompensation in progress and 3 years after treatment. The positive overjet overbite is maintained but with recurrent maxillary transverse constriction. E, Articulated dental casts that indicate analytic model planning. F, Lateral cephalometric radiographs before and after reconstruction.
1. Inadequate skeletal mobilization. When significant widening of the posterior maxilla is required, bilateral (rather than unilateral) parasagittal osteotomies will assist with the tension-free placement of the segments into the splint (see Chapter 15).
2. Inadequate splint strength. The use of a non-flexible splint (e.g., a reinforced U-shaped acrylic splint, transpalatal support) is essential to maintain the arch width during initial healing (see Chapter 13).
3. Inadequate soft-tissue mobilization. After the completion of segmental osteotomies, the stretching of the palatal soft tissues through the down-fracture (i.e., the use of a spreader forceps) improves the tension-free placement of the segments into the splint.
4. Inadequate postsurgical care. After the splint is removed (i.e., 5 weeks after surgery), the seamless transfer of responsibility from the surgeon to the orthodontist for ongoing maxillary arch form maintenance is essential. The effective use of orthodontic mechanics is generally needed for at least 6 months to retain the arch form. (This is described later in this chapter.)
Orthodontic Treatment: Dental Stability and Relapse
The objective of orthodontics in conjunction with jaw surgery is to align the dentition in each arch by placing the maxillary and mandibular teeth fully within the basal bone. When the jaws and jaw segments are then surgically repositioned, the preferred occlusion is achieved. Following Andrews’ Six Keys to Normal Occlusion provides the framework for the accomplishment of the orthodontic objectives (see Chapters 5 and 6).208
Moen and colleagues carried out a prospective clinical study to evaluate the short-term occlusion achieved and the long-term occlusion maintained after bilateral sagittal split ramus osteotomies with advancement for the treatment of Class II skeletal deformities.208 Prospectively, 36 patients with Class II skeletal patterns who were to undergo bilateral sagittal split ramus osteotomies agreed to participate in the study. The mean age at operation was 33 years (range, 16 to 59 years). All of the study patients underwent perioperative orthodontics and were followed clinically, with dental models and radiographs (i.e., lateral cephalometric and Panorex). These standard records were obtained at 8 weeks, 1 year, and 13 years after surgery. Interestingly, for the majority of patients, cephalometric analysis confirmed insignificant skeletal changes during long-term follow up after successful initial healing had occurred. Long-term recurrent malocclusion was found to be primarily dental rather than skeletal in origin.208 To achieve and then maintain the ideal occlusion, the importance of the stable orthodontic positioning of the teeth in the alveolus cannot be overstated (Figs. 17-9 through 17-14).



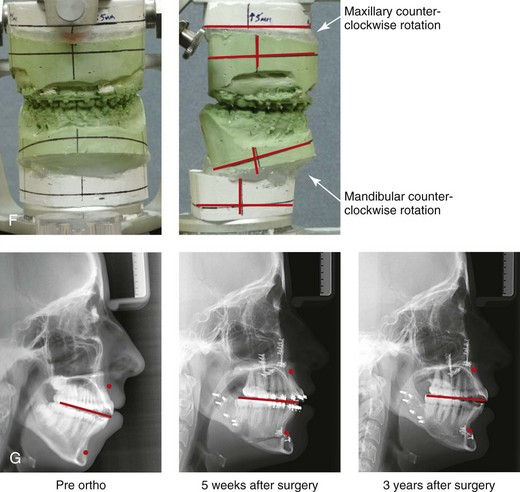
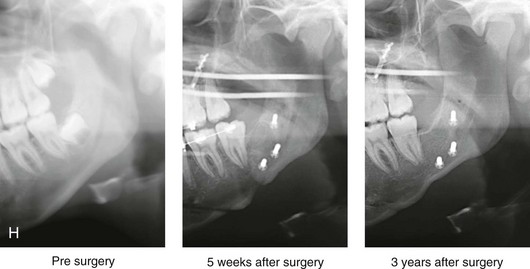
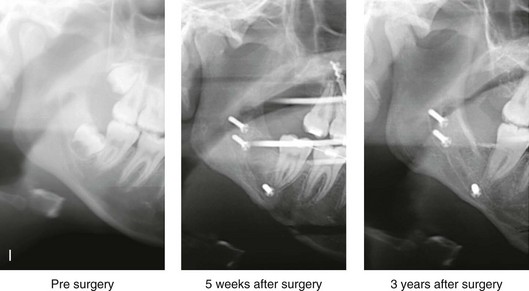
Figure 17-9 A female high-school student was referred by her orthodontist for surgical evaluation. Since her mid childhood years, the patient was known to have a long face growth pattern, and she had a lifelong history of obstructed nasal breathing. She had undergone attempted growth modification followed by orthodontic camouflage, without success. At the time of referral, the patient’s concerns included lip incompetence, gummy smile, weak profile, malocclusion, and nasal obstruction. She agreed to a surgical correction. The orthodontic treatment plan then changed in preparation for orthognathic surgery. Extractions were not carried out to correct the maxillary and mandibular arch forms. The patient then underwent maxillary Le Fort I osteotomy (horizontal advancement and vertical intrusion); bilateral sagittal split ramus osteotomies (minimal horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and recontouring of the nasal floor. Successful initial surgical healing was achieved. The occlusion maintained at splint removal (i.e., 5 weeks after surgery) was as planned. The orthodontic appliances were removed 6 months after surgery, with ideal occlusion and orthodontic retention continued. The patient returned 3 years after surgery with complaints of recurrent anterior open-bite malocclusion. A, Frontal views in repose before and 3 years after surgery. B, Frontal views with smile before and 3 years after surgery. An analysis was carried out that included the review of lateral cephalometric and Panorex radiographs taken before surgery, 5 weeks after surgery, and 3 years after surgery. The patient had no temporomandibular disorder, and there was no evidence of condylar resorption. Therefore, idiopathic condylar resorption was ruled out. Cephalometric analysis of the presurgical, early postoperative, and late postoperative cephalometric radiographs revealed satisfactory initial repositioning and healing of the jaws without skeletal relapse at 3 years. A comparison of the 5-week postoperative and 3-year postoperative sella–nasion–A-point and sella–nasion–B-point angles and facial heights confirmed skeletal stability. A review of the arch form (i.e., the dental models) suggested orthodontic relapse that included transverse maxillary constriction and incisor intrusion. The mandibular arch form also indicated dental relapse. Treatment options included redo Le Fort I osteotomy in three segments for the correction of the arch form versus surgically assisted rapid palatal expansion. Orthodontics would also be required. The advantages of four bicuspid extractions as part of dental decompensation were also discussed. The patient was pleased with the enhanced facial aesthetics (i.e., a less gummy smile, an improved profile, and lip closure) and the improved breathing that was achieved. She also did not have any temporomandibular disorder. She elected to receive no further treatment. C, Oblique facial views before and 3 years after surgery. D, Profile facial views before and 3 years after surgery. E, Occlusal views before the orthodontic retreatment, immediately before surgery, 5 weeks after surgery, and 3 years after surgery. F, Articulated dental casts that indicate analytic model planning. G, Serial lateral cephalometric views before orthodontic retreatment, 5 weeks after surgery, and 3 years after surgery. H, Serial Panorex views of the left condyle–ramus before surgery, 5 weeks after surgery, and 3 years after surgery. I, Serial Panorex views of the right condyle–ramus before surgery, 5 weeks after surgery, and 3 years after.



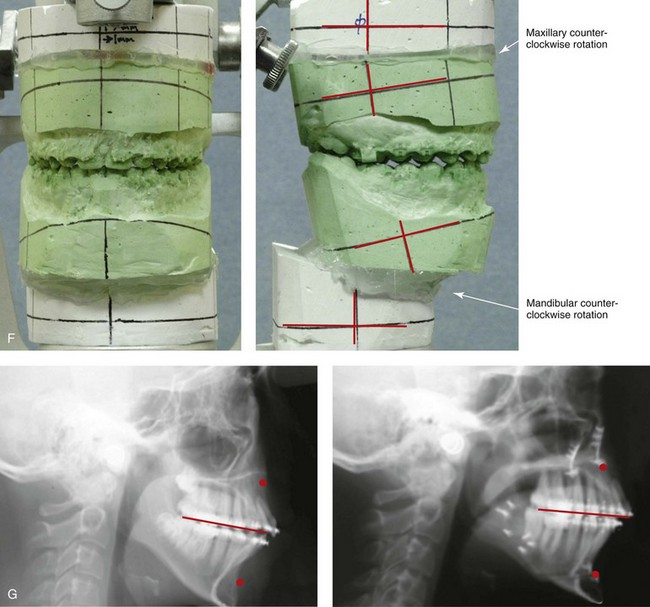
Figure 17-10 A 14-year-old girl was referred by her orthodontist for surgical evaluation. She presented with a long face Class II growth pattern and a lifelong history of obstructed nasal breathing. She underwent non-extraction orthodontics, including mechanics to correct the maxillary arch form. The patient’s surgery included maxillary Le Fort I osteotomy (vertical intrusion, horizontal advancement, and counterclockwise rotation); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical reduction and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. Healing occurred without complications. The occlusion that was initially achieved and maintained at 5 weeks after surgery was as planned. Unfortunately, the patient refused continued postoperative orthodontics and the appliances be removed 3 months after surgery. She was also not compliant with retainer use. By 1 year after surgery, there was a recurrence of the anterior open bite. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. A review of the dental models confirmed dental relapse with a recurrent accentuated curve of Spee and arch constriction of the maxilla. In retrospect, segmental orthodontic mechanics followed by segmental maxillary surgery would likely have prevented this problem. At this time, treatment options include segmental orthodontic mechanics and redo Le Fort I osteotomy in segments. The patient and her family were pleased with the improvements in lip closure/posture, a diminished gummy smile, improved profile aesthetics, and better breathing during the day and night. The patient did not have temporomandibular disorder, and she elected to received no further treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views in mixed dentition before treatment, with preoperative orthodontics complete, with initial surgical occlusion achieved (i.e., 5 weeks after surgery), and 1 year after treatment. Note: Discoloration of right maxillary central incisor crown suggests pulpal pathology. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric views before and after treatment.
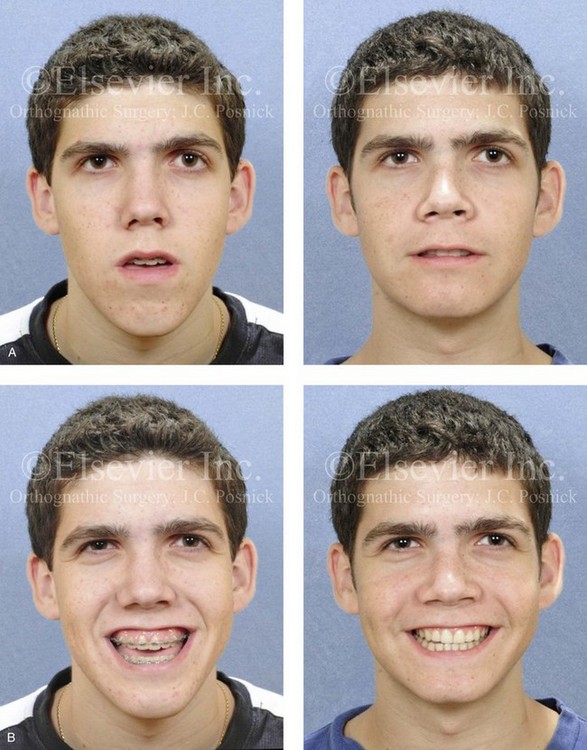
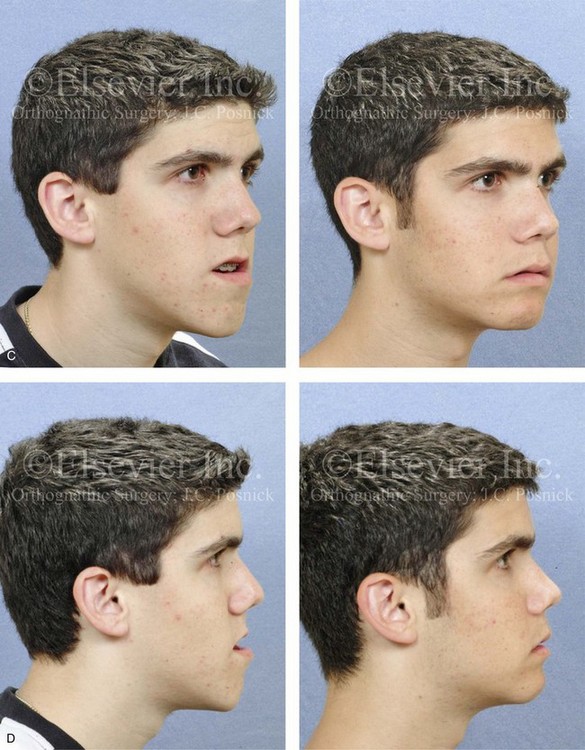
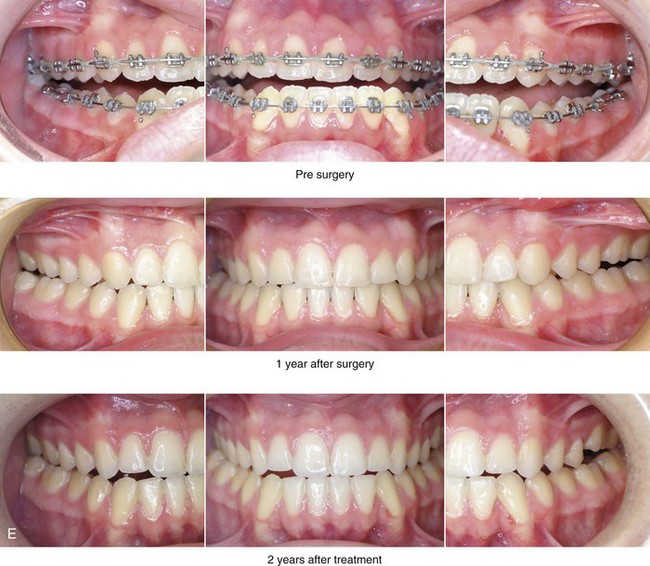
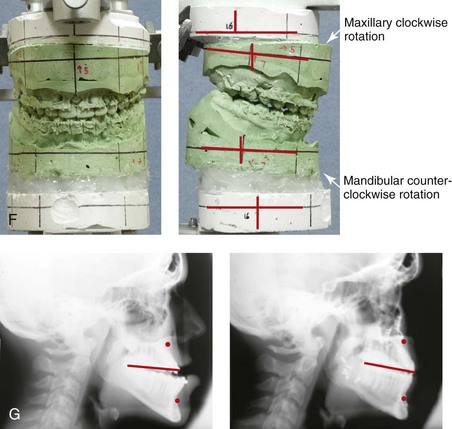
Figure 17-11 A 17-year-old boy was referred by his orthodontist for the surgical evaluation of a long-standing developmental jaw deformity with malocclusion and a lifelong history of obstructed nasal breathing. The patient had undergone both growth modification and camouflage orthodontics, without success. Examination confirmed a Class III long face growth pattern with an anterior open bite. He then underwent orthodontic mechanics in preparation for jaw surgery. The maxillary arch was leveled with orthodontic mechanics. The patient’s surgery included maxillary Le Fort I osteotomy (horizontal advancement, vertical shortening, and clockwise rotation); bilateral sagittal split osteotomies of the mandible (minimal set-back and clockwise rotation); and septoplasty, inferior turbinate reduction, and nasal base recontouring. An osseous genioplasty with horizontal advancement would have further enhanced the patient’s facial aesthetics but was refused. The surgery was followed by finishing orthodontics. The patient’s occlusion at 5 weeks after surgery was excellent, and it remained so at the time of the debracketing 6 months after surgery. By 1 year after surgery, a slight Class III tendency with posterior constriction was evident. A, Frontal views in repose before and after surgery. B, Frontal views with smile before and after surgery. By 2 years after surgery, the anterior occlusion was edge to edge, and the maxillary arch form was irregular. The cause of the recurrent malocclusion was felt to be either ongoing mandibular growth or a loss of maxillary arch form as a result of dental relapse. A review of the cephalometric data suggested stability of the mandible (i.e., the sella–nasion–A-point and sella–nasion–B-point angles were unchanged at intervals after surgery). A review of the dental models confirmed dental relapse with a change in the maxillary arch form (i.e., constriction in the arch width and an accentuated curve of Spee). Treatment options include maxillary Le Fort I osteotomy in segments for the correction of the arch form versus surgically assisted rapid palatal expansion. An osseous genioplasty was also offered to improve the patient’s profile aesthetics. The patient was pleased with the functional improvements (i.e., chewing and speech articulation), and he did not have temporomandibular disorder; he also appreciated the enhanced facial aesthetics. He elected to receive no further treatment. C, Oblique facial views before and after surgery. D, Profile views before and after surgery. E, Occlusal views immediately before surgery and at 1 year and 2 years after surgery. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


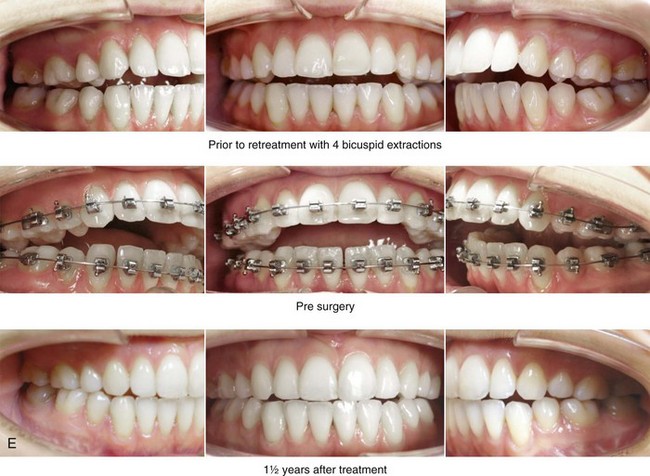
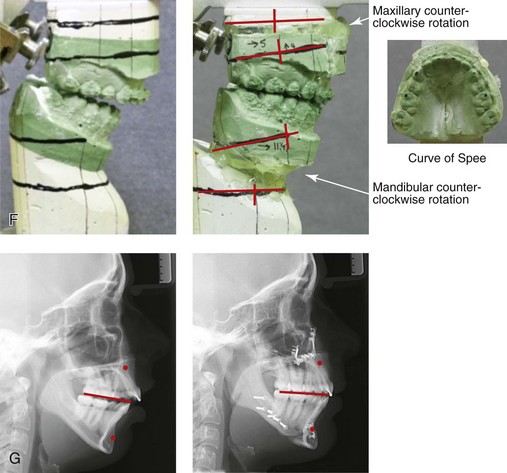
Figure 17-12 A 20-year-old female college student was referred for surgical evaluation. During the mixed dentition, she was noted to have a long face growth pattern with an anterior open bite. She was treated from the time that she was 11 to 15 years old with growth-modification followed by a four-bicuspid orthodontic camouflage approach, without success. She presented for surgical evaluation with complaints of chronic obstructed nasal breathing; an anterior open bite that caused difficulty with chewing and with speech articulation; wide lip separation with lip strain at closure; and a retrusive profile appearance. There was generalized root resorption and early anterior mandibular labial bone loss and gingival recession. A comprehensive evaluation also confirmed septal deviation and inferior turbinate hypertrophy with increased nasal airway resistance. The patient agreed to an orthodontic and orthognathic/intranasal surgical approach. Her surgery included maxillary Le Fort I osteotomy in segments (arch form correction, horizontal advancement, vertical shortening, and counterclockwise rotation); bilateral sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after treatment. B, Frontal views with smile before and after treatment. The occlusion that was initially achieved and maintained at 5 weeks after surgery was as planned. Postoperative orthodontic appointments were complicated by the patient’s attendance at an out-of-state college. At the time of appliance removal (i.e., 10 months after the operation), there was partial recurrence of the anterior open bite. The occlusion then remained stable at the 18-month postoperative interval. There was no popping, clicking, or pain in either temporomandibular joint. There was mild masticatory muscle discomfort, which was relieved with an effective night guard. An analysis of the postoperative cephalometric radiographs, which were taken at 1 month and 18 months after surgery, confirmed a stable SNB angle. The condyle-to-gonion measurement also remained stable. A review of the condyle morphology on the Panorex radiograph revealed no significant change. A review of the dental models (i.e., the surgical planning models and those from 16 months after surgery) suggested a degree of dental relapse in the form of recurrent curve of Spee issues in the maxilla and the mandible. The patient elected to undergo no further treatment. C, Oblique facial views before and after treatment. D, Profile views before and after treatment. E, Occlusal views before retreatment, with orthodontics in progress, and at 16 months after surgery. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and 16 months after surgery.
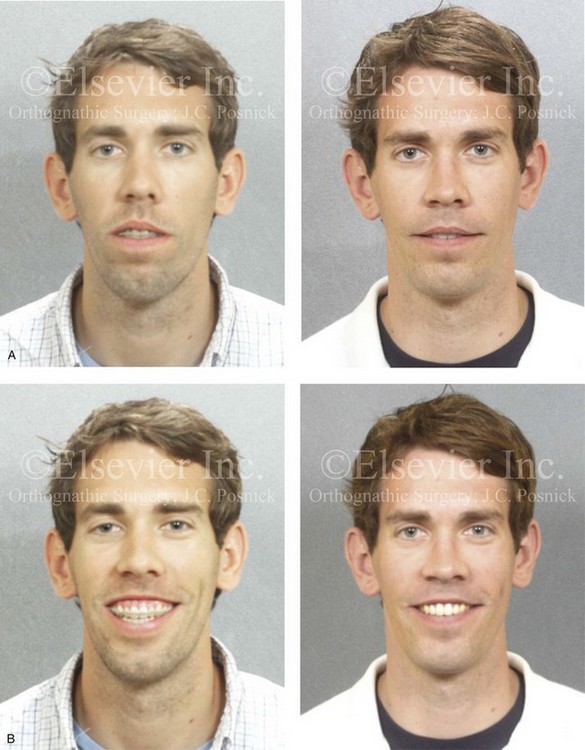
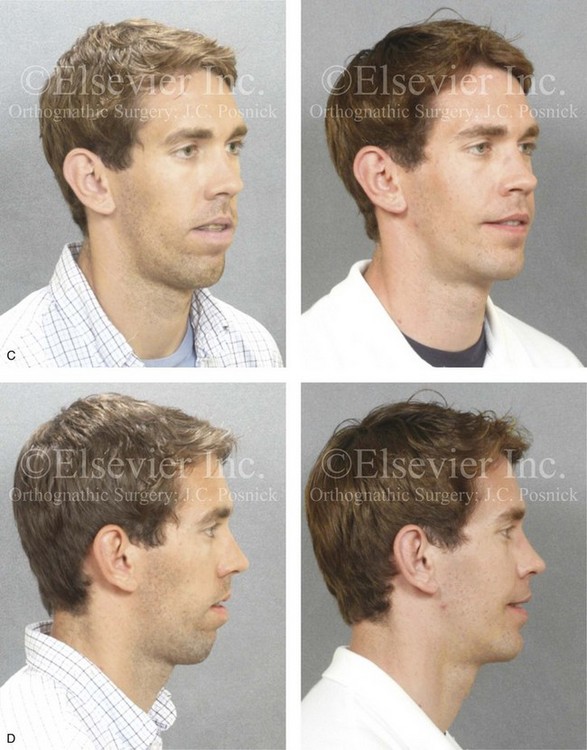

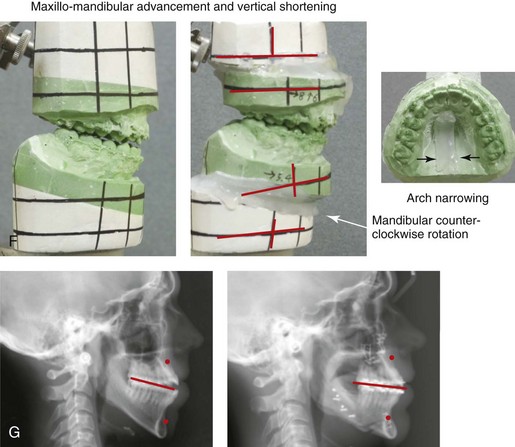

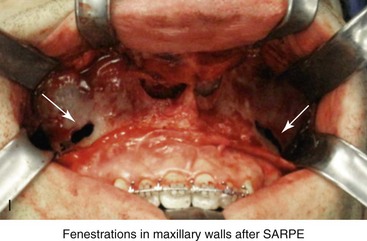
Figure 17-13 A 25-year-old man presented with a long face anterior open-bite growth pattern. He had undergone four bicuspid extractions and a surgically assisted rapid palatal expansion procedure to reduce crowding and to expand the maxillary arch width at another institution. He was referred to this surgeon with residual maxillofacial problems, including jaw discrepancy, residual malocclusion, and chronic obstructed nasal breathing. The patient agreed to additional orthodontic mechanics and surgery, including Le Fort I osteotomy in two segments (vertical shortening, horizontal advancement, and arch narrowing); sagittal ramus osteotomies (horizontal advancement and counterclockwise rotation); septoplasty; the reduction of the inferior turbinates; and osseous genioplasty (vertical shortening and horizontal advancement). He is shown before and after the completion of his final phase of treatment. A, Frontal views in repose before and after retreatment. B, Frontal views with smile before and after retreatment. C, Oblique facial views before and after retreatment. D, Profile views before and after retreatment. E, Occlusal views after earlier orthodontic treatment including four bicuspid extractions, after surgically assisted rapid palatal expansion (SARPE), just before orthognathic surgery, and after retreatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric views before and after retreatment. H, Panorex radiograph before retreatment. I, Intraoperative view of the anterior maxilla after the surgically assisted rapid palatal expansion (SARPE) procedure and just before Le Fort I osteotomy.
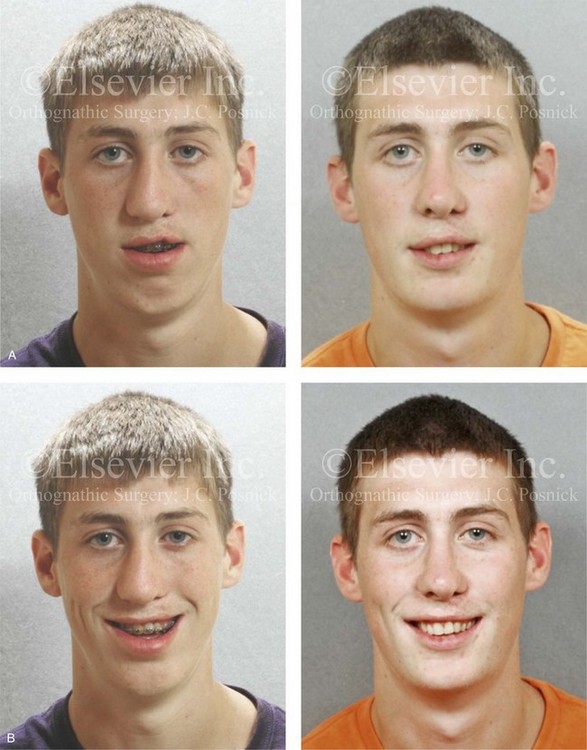


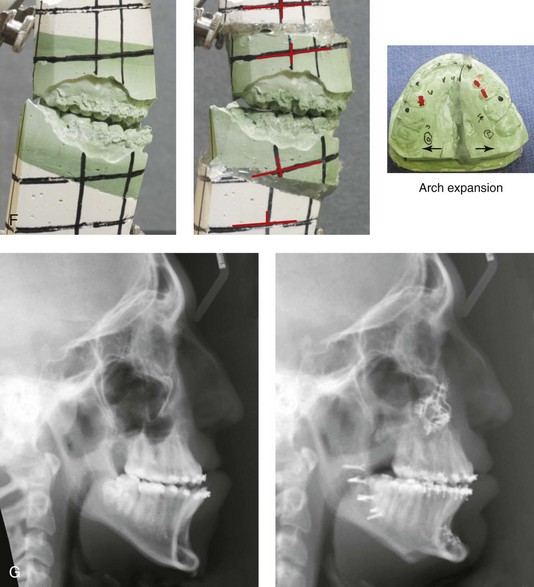
Figure 17-14 A young man born with a unilateral cleft lip and palate had been treated by other surgeons. His treatments had included primary cleft lip repair; primary cleft palate repair; two cleft lip revisions; three cleft palate revisions; the placement of a superiorly based pharyngeal flap; iliac grafting for a cleft defect; cleft rhinoplasty; and suboptimal Le Fort I osteotomy with an external RED distraction osteogenesis (DO) device. The patient was referred to this surgeon when he was 17 years old with residual cleft deformities, including the following:
• Persistent oronasal fistula and alveolar cleft
• Residual cleft jaw deformity with maxillary hypoplasia and Class III malocclusion
• Chronic nasal obstruction as a result of septal deviation and enlarged inferior turbinates
• Residual cleft nasal deformity
• Cleft lip deformity with a lack of continuity of the orbicularis–oris muscle
The lips, tongue, cheeks, soft palate, mandible and periodontal ligaments function dynamically with the stationary (immobile) maxilla and the teeth to achieve chewing, swallowing, breathing, speech, and lip closure. Parafunctional habits of these structures (e.g., posturing of the tongue, lips, and jaw) may influence the position of the teeth and the supporting skeletal structures. Dental compensations are expected biologic responses when a jaw disharmony is present at birth or when it occurs during growth. The orthodontic mechanical removal of dental compensations should position the teeth within the alveolar process to then maximize the surgical correction and also to provide a framework for long-term occlusal stability and periodontal health.*
Extraction Therapy to Eliminate Crowding
During the 1880s, Edward Angle joined other progressive restorative dentists of his time in their opposition to a casual attitude toward the extraction of teeth (see Chapter 2). Angle’s belief was that, through diligent effort, the orthodontic alignment of the full complement of teeth was possible. He felt that the orthodontist’s ultimate objective was for every person to have the potential for an ideal relationship of all 32 natural teeth.
Through trial and error, he realized that simply tipping the teeth into a new position was often inadequate. He developed the Ribbon Arch appliance and then the Edgewise appliance to “bodily” move the teeth. These were the first clearly described and reliably designed orthodontic appliances that were capable of controlling root position. At this time, Dr. Angle claimed that these were “bone-growing appliances.”10 For Angle, this work was simply an extension of Wolff’s law of bone, which states that the internal architecture of a bone represents the stress pattern that is placed on it.
Angle’s treatment philosophy involved arch expansion with the use of vectored rubber bands and other appliances, as needed, to bring the teeth into occlusion. To Angle, at least early during his career, the term relapse as it applied after orthodontic expansion that had been carried out to uncrowd and correct overjet or overbite simply meant that the achieved occlusion was inadequate or technically incorrect. According to Angle, “If a correct occlusion had been produced [by the orthodontist] the result would be stable.”10 Therefore, he felt, “if the orthodontic result was not stable, the fault was either that of the orthodontist or poor compliance by the treated patient, not the theory.”10
The acceptance of extraction therapy in orthodontics to stably position the teeth into alveolar housing coincided with an appreciation that genetic variations—with disparities between tooth root volume and jaw size—are common among normal individuals and will differ among races (see Chapter 3). That a presenting jaw or dental discrepancy could benefit from extractions was simply an admission of a patient’s individuality rather than the orthodontist’s inability to solve all problems in the same way. By the early 1960s, approximately 50% of American patients who were undergoing orthodontic treatment would experience the extraction of at least some teeth, most commonly the first premolars.
Orthodontists have also used extractions as a means to achieve a neutralized occlusion in the presence of a skeletal discrepancy (i.e., a camouflage approach). This involves achieving an improved occlusion while accepting the jaw (facial) disharmony. Examples of this approach include upper bicuspid extractions to orthodontically treat mandibular retrognathism or lower bicuspid extractions to orthodontically manage Class III skeletal patterns. Interestingly, this orthodontic camouflage approach became common practice during the 20th century, despite the fact that, by the early 1900s, mandibular surgery had been performed for both Class II and Class III skeletal deformities. In reality, corrective jaw surgery was rarely considered an option (except by a handful of orthodontists and surgeons) until the later decades of the 20th century (see Chapter 2).
By the 1990s, overemphasis on four bicuspid extractions as part of routine orthodontic treatment began to wane in favor of a more discriminating approach. The rationale for selective extractions as part of a comprehensive surgical and orthodontic approach has now been confirmed to be effective for the removal of dental compensation. Extraction orthodontic therapy in combination with jaw osteotomies to correct the occlusion, for long-term periodontal health, to improve the upper airway, and to enhance facial aesthetics is now considered routine for many patients. The interproximal reduction of enamel as an alternative to extractions was popularized by Dr. J. Sheridan during the 1990s. In borderline cases, it has been found to provide the necessary space for incisor uprighting (see Chapters 5 and 6).
Research confirms that clinicians and the general public prefer a face with full midface projection and with prominent teeth and lips.231,257,261 The “flat face” orthodontic standards of Tweed, which were typical during the 1950s and the 1960s, retracted rather than expanded (i.e., filled out) the face. In borderline cases, the patient’s facial appearance is generally judged as being better without extractions. The decision to extract should be viewed in the light of attaining Andrews’ Six Keys to Normal Occlusion and Six Elements of Orofacial Harmony (see Chapter 2). The primary goals are to achieve: (1) the placement of teeth solidly in the alveolar bone (2) ideal dental alignment within and between the arches and (3) the adequate position and projection of the maxillomandibular complex (i.e. facial harmony). If jaw surgery (with or without extractions) is required to achieve these objectives, it should be incorporated into the treatment plan from the outset for the benefit of the patient.
Orthodontic Treatment of Specific Dentofacial Growth Patterns: Dental Stability and Relapse
Primary Mandibular Deficiency Growth Pattern with or without Maxillary Arch Constriction (Skeletal Class II)
Orthodontic Approach in Conjunction with Orthognathic Surgery
The failure to remove these compensations limits the surgeon’s ability to position the mandible for ideal facial proportions, and for the relief of airway obstruction (i.e., opening of the retroglossal space). An advancement genioplasty to further enhance aesthetics and lip function is also generally beneficial to manage microgenia (see Chapter 19). If the surgeon “over-advances” the chin as a “skeletal compensation” for the inadequate orthodontic removal of incisor flaring, then further facial disproportion (i.e., a deepening of the labiomental fold with an overly prominent pogonion) is likely to occur (see Chapters 37 and 40).
If interarch-width discrepancies are present—as they are in approximately one third of cases—then simultaneous Le Fort I osteotomy with segmentation (i.e., into two or three segments) is generally carried out to widen and correct the maxillary arch form (see “Management of Transverse Maxillary Deficiency” later in this chapter). When only minimal upper arch width deficiency exists and no other reasons warrant maxillary osteotomy, mandibular narrowing to balance the arches can be considered. This may be accomplished by completing a vertical midline osteotomy between the mandibular central incisors. The use of this option for mandibular narrowing is usually a distant second choice (vs. maxillary expansion) for the resolution of interarch discrepancies. Adding width to the upper jaw is generally preferred for the airway and to enhance smile aesthetics (i.e., for the relief of dark buccal corridors).
Maxillary Deficiency with Relative Mandibular Excess Growth Pattern (Skeletal Class III)
Findings
In a patient with maxillary deficiency and relative mandibular excess, the normal dental compensations generally include maxillary incisor protrusion and upright or retroclined mandibular incisors (see Chapter 20).
Orthodontic Approach in Conjunction with Orthognathic Surgery
With this common dentofacial growth pattern, the extraction of the first bicuspids in the maxillary arch to uncrowd and reposition the incisors (approximately 120 degrees to the Frankfort plane or 102 to 104 degrees to the sella–nasion plane) should be considered. With only borderline crowding and limited incisor flaring the decision for maxillary extractions becomes more difficult. Also, a degree of maxillary incisor flaring may be aesthetically tolerated when planning bi-maxillary osteotomies, which incorporate clockwise rotation of the maxillo-mandibular complex to correct any A-point–B-point facial disharmony (see Chapter 12).
If interarch width discrepancies (posterior crossbites) require correction, then simultaneous segmentation of the down fractured maxilla (2 or 3 segments) is carried out (see “Management of Transverse Maxillary Deficiency” later in this chapter).
Long Face Growth Pattern: Maxillary Vertical Excess with Mandibular Deformity
Findings
A long face growth pattern classically includes maxillary deformity (vertical excess, transverse deficiency, and a lack of horizontal projection), mandibular deformity (high-angle retrognathia), and deformity of the chin (vertical excess and sagittal deficiency). Of note is that the mandibular deformity may also present as a Class III rather than the more common Class II growth pattern (see Chapters 4 and 21).
Orthodontic Approach in Conjunction with Orthognathic Surgery
The preoperative orthodontic leveling of a moderate to severe curve of Spee in the maxilla is ideally performed with segmental arch mechanics. This is necessary to match the dental alignment with the extent of dysmorphic anterior and posterior alveolar bone. This is done in preparation for segmental maxillary osteotomies, which will then level the curve of Spee and adjust the arch width. This segmental orthodontic preparation places the teeth solidly in the available alveolar bone within each component (segment) of the upper jaw. This avoids the extrusion of the anterior teeth and the buccal tipping of the posterior dentition. Given the usual degree of dysmorphic maxillary alveolar bone, attempts to level the dentition solely through orthodontic mechanics (i.e., via incisor extrusion and molar intrusion) are periodontally unsound; they may result in incisor root resorption, and they are prone to late dental relapse with recurrent malocclusion (see Fig. 17-9).
Surgical segmentation of the maxilla between the lateral incisors and the cuspids and then parasagittally through the hard palate is generally performed to achieve the desired arch width, the leveling of the curve of Spee, and the adjustment of incisor inclination. The canine and lateral incisor roots are naturally divergent, so there is no need (or advantage) for the orthodontist to create a space to “make the segmental surgery safe” (see Chapter 15). There is little risk of causing intraoperative injury within the periodontal ligament space or to the tooth roots or of creating periodontal pocketing when completing the interdental osteotomies in these locations.
Management of Transverse Maxillary Deficiency: Techniques and Relapse Patterns
Background
The orthodontic management of isolated transverse maxillary deficiency in children and adolescents with an open palatal suture by rapid palatal expansion (RPE) and conventional orthodontic techniques is generally possible, although stability can be troublesome.* In the non-growing individual, if standard orthodontic techniques are used for expansion beyond a few millimeters, they will produce either buccal tipping of the maxillary molars or lingual tipping of the mandibular molars with an unstable long-term occlusion and the potential for injury to the periodontium. The molars will likely relapse palatally, thereby causing clockwise rotation of the mandible with recurrent anterior open bite.
The literature confirms that a transverse maxillary deficiency that presents after palatal suture closure (i.e., an age of >14 years) should be managed surgically.* This can be done with either “surgical assistance” followed by rapid expansion using an in-place palatal appliance (the process known as surgically assisted rapid palatal expansion [SARPE]) and then orthodontic realignment or by segmental Le Fort I maxillary osteotomies in conjunction with standard orthodontics. The latter approach is carried out when clinically indicated as a one-stage procedure in combination with vertical, horizontal, and other needed surgical repositioning of the maxilla (these two approaches are discussed in more detail later in this chapter). The magnitude of segmental maxillary expansion that a surgeon is comfortable achieving is dependent on that clinician’s experience and the unique aspects of the specific patient’s palatal anatomy.
Proffit and colleagues reported that individuals who are seeking evaluation for orthognathic surgery have a 30% incidence of transverse jaw discrepancies.252 True (absolute) transverse discrepancy exists when one or both of the posterior maxillary segments are in a crossbite when the casts are placed into a normal overjet and overbite position after the relief of dental compensation. This will tend to unmask arch-width discrepancies in patients with Class II malocclusions and correct a percentage of those in patients with Class III malocclusions. True transverse arch discrepancies are frequently seen in patients with 1) Class II retrognathic mandibles 2) long face Class II anterior open bites 3) those with previous thumb-sucking habits resulting in anterior open bite and 4) patients with cleft palates and maxillary deficiency.
Vanarsdall and colleagues have defined transverse skeletal discrepancies through measurements that are made on posteroanterior cephalometric radiographs.314 The authors measured maxillary (skeletal) width from the jugular point on one side to the jugular point on the other side. They compared this measurement to the skeletal lower arch width measured from the antegonial notch on one side to the antegonial notch on the other side. From these two measurements, the determination of a differential index can be made. These researchers suggested that a preferred differential index should be approximately 20 mm in the adult Caucasian individual. Preadolescent patients will normally have a lower differential index. The authors believe that an adult with a differential of 30 mm has a significant transverse problem. According to Vanarsdall and colleagues, a differential index that varies by more than 5 mm from these values requires correction in the maxilla to establish a long-term stable occlusion and satisfactory periodontal health.314 With the advent of three-dimensional cone beam computed tomography imaging, the more accurate measurement of the transverse maxillary width is likely available. Further research is required to confirm normal values for maxillary and mandibular arch width.
Gingival recession in any given individual is likely to have multifactorial causes. Tooth position within the alveolar process is an important factor, especially in the patient who is biologically susceptible to recession (i.e., with limited attached gingiva; see Chapters 5 and 6). According to Vanarsdall and colleagues, the most common risk factors for the gingival recession of the maxillary posterior dentition include 1) friable attached gingiva 2) genetic factors 3) emotional stress 4) inadequate labial bone and 5) buccally tipped maxillary posterior teeth (i.e., dental compensation).314 These factors will cause the periodontium to “receive” rather than “transmit” forces, with likely continued bone loss and gingival recession occurring over time.
Vanarsdall and colleagues suggest that periodontal susceptibility to breakdown has a relationship to the position of the teeth within the arch and to the relationship of the opposing teeth when they are in occlusion (see Chapters 5 and 6).314 The initial experimental work of these researchers shows a decrease in the numbers of pathogenic bacteria around the teeth after the teeth have been aligned into a more natural position (i.e., to more closely agree with Andrews’ Six Keys to Normal Occlusion). With good dental alignment, the numbers of harmful bacteria were brought below the threshold at which damage to the periodontal tissues frequently occurs. It is also believed by many clinicians that the achievement of maxillomandibular occlusal harmony (i.e., the correction of molar inclination and crossbites) tends to improve long-term dental and skeletal stability after orthognathic surgery (see Chapters 5 and 6).
History of SARPE and Segmental Osteotomies to Correct Maxillary Arch Deficiencies
The recorded history of transverse maxillary expansion dates back to the mid-1800s, when Angle reported the use of a jackscrew appliance in a 14-year-old girl to create space for a labially displaced canine.9 This form of arch expansion was frequently used in children, adolescents, and adults until Hass reported that, after the age of 18 years, it was not possible to open the mid-palatal arch with appliance distraction forces because of the presence of bridging bone spicules across the suture and the increased rigidity of contiguous bones.124 It is now generally accepted that RPE without “surgical assistance” is clinically successful only until the age of approximately 14 years and in the presence of open sutures. Attempting orthopedic expansion beyond this age is likely to result in the tipping and extrusion of teeth followed by dental relapse after the removal of the appliance.
The first recorded use of “surgical separation” of a fused mid-palatal suture for the management of transverse maxillary deficiency was by Brown.49–51 Since that initial report, the clinical approach that includes the completion of maxillary osteotomies followed by orthodontic appliance expansion has continued to evolve. By the 1980s, it was recognized that a full Le Fort I osteotomy but without down-fracture—including the separation of the nasal septum from the maxilla and the separation of both pterygomaxillary sutures—in combination with a parasagittal palatal and interdental osteotomy (generally between the incisors) was required. The immediate activation of an in-place palatal expander in the operating room to verify the completion of the osteotomies is also required to confirm the reliability of postoperative skeletal expansion.
By the 1970s, the biologic safety of a Le Fort I osteotomy in segments and the ability to then three-dimensionally reconfigure the segments directly in the operating room without the need for post surgical orthodontic expansion was proven in experimental primate studies and through successful use in clinical practice (see Chapter 2). This led to questions about the value of SARPE as a first-stage procedure for the patient with a dentofacial deformity who also requires maxillary horizontal and vertical adjustments.
For the patient to undergo a two-stage orthognathic surgical approach (i.e., first-stage SARPE followed by definitive orthognathic surgery 6 to 12 months later) for the management of a multivector maxillary deformity, significant value would have to be demonstrated. Variables to consider include the following: (1) the potential for intraoperative and postoperative complications (2) the risks of multiple rounds of general anesthesia and multiple recovery periods (3) the direct financial costs to the patient, to his or her family, and to the health care system (4) the necessary patient and family time commitment (5) the facial aesthetic effects and (6) the potential for relapse and the stability of the occlusion. Most clinicians agree that the single-stage approach (i.e., Le Fort I osteotomy in segments) has clear advantages when considering each of these variables, except for differences of opinion related to potential relapse and the stability of the occlusion. The patient described in Figure 17-13 could be considered a case that would cause one to favor a two-stage approach, because the end result is favorable. However, in retrospect, the family and the treating clinicians viewed this case as involving an inefficient approach to the correction of the individual’s presenting dentofacial deformity. The two-stage approach required 1) two separate general anesthetics and recoveries 2) an extended and more elaborate course of orthodontics; and 3) an increased financial burden to the family in the form of additional surgeon and hospital fees. Also, The SARPE procedure resulted in a degree of root resorption, and the Le Fort I osteotomy (Stage II) was made more difficult by the earlier SARPE procedure (Stage I). The intraoperative view (see Figure 17-13, F) shows the resulting fenestrated maxillary walls after the SARPE procedure.
Complications of the SARPE Procedure: Review of the Literature
Although SARPE is a commonly considered procedure, the prevalence of postoperative complications and suboptimal results is not insignificant.57,72,175,177,182,195,211,254,291,315,329 Williams and colleagues examined the prevalence of complications among patients undergoing SARPE.329 This was a retrospective evaluation conducted on all individuals who underwent SARPE over a 4-year timeframe (2004 to 2008) at a single institution. The study sample (n = 120) included patients with a median age of 29.5 years (range, 22 to 39 years) and was comprised of 51.7% women. Postoperative complications were divided into two main categories: surgical and dental. Thirty-three patients (28%) developed surgical complications and 18 patients (15%) developed dental or periodontal problems. Asymmetric or inadequate expansion was the most frequent surgical complication, and it was found in 13.3% (16 out of 120 patients) of the study cohort. Dental or periodontal problems—including central incisor discoloration, gingival recession, and periodontal bone loss—occurred in 15% of the cohort. Two patients developed catastrophic bone defects with associated loss of the central incisors as a result of eccentric midline osteotomies followed by infections. The study confirms that major complications after SARPE are rare, whereas the incidences of asymmetric and inadequate expansion as well as dental or periodontal problems are not insignificant. These findings confirm that the SARPE procedure should not be considered as a risk-free alternative to segmental Le Fort I osteotomies.
Verlinden and colleagues reported on a large case series of individuals (n = 73 patients) undergoing SARPE with a bone-borne appliance.315 Although most of the problems documented were related to hardware, six patients (8%) required additional surgery for the correction of an unstable occlusion or for asymmetric expansion. Among those study patients who were followed for more than 6 months, gingival recession, periodontal bone loss, a lack of interdental bone fill, and external apical root resorption were seen in more than one third of cases. Seitz and colleagues studied patients who were undergoing SARPE (n = 22) and found that asymmetric expansion was the most frequent surgical complication. In another review of SARPE complications, Carmen and colleagues reported a 28.5% incidence of significant gingival recession.57
Occlusal Stability and Relapse: Comparing SARPE versus Segmental Le Fort I Osteotomy
When it comes to a single-stage procedure versus a two-stage approach to the management of a complex maxillary deformity, the key aspect of occlusal stability and relapse has been reviewed in the literature and argued by clinical proponents on each side. Shortcomings in the study design of most published research add to the lack of clarity. Most studies have involved only dental casts or direct measurements of dental arch dimensions. Without the use of posteroanterior (PA) cephalograms, skeletal change cannot be differentiated from tooth movement. Another shortcoming is that most studies measure stability from the end of orthodontic treatment rather than from the point of maximum expansion. The clinical practice of over-expanding the arch to end up with a satisfactory occlusion at the end of treatment results in the underestimation of the actual relapse. With limited data points, most studies cannot differentiate skeletal relapse components from dental ones. One exception is the study by Byloff and Mossaz, which overcame these limitations by using pre-expansion and postexpansion PA cephalograms and dental casts as data points.56 After SARPE, the authors observed a mean maximum expansion at the first molar of 8.7 mm, with an average of 36% (3.1 mm) relapse at the time of debanding. Only 1.3 mm (23%) of this relapse was felt to be skeletal, with the rest (77%) being dental. Berger and colleagues also used an improved study design and reported an average of 2.49 mm (48%) of skeletal expansion in combination with 2.4 mm (52%) of dental expansion for their patients when using a SARPE approach.31 Two published meta studies, which were carried out in 2005 by Koudstaal and colleagues167 and in 2006 by Lagravere and colleagues,176 both concluded that, until that time, no good evidence existed regarding the amount of relapse after SARPE.
Chamberland and Proffit studied this controversy, and, in 2008, they published their initial research.59 They continued to follow their patients for the long term, and they also added numbers to the study group (N = 38). Their study has been recognized for adding significant clarity to this important subject and is therefore reviewed in the next section of this chapter.
Skeletal Stability and Relapse of SARPE: Review of a Benchmark Study
A prospective observational study was carried out by Chamberland and Proffit to review the SARPE outcomes in 38 consecutive patients between the ages of 15 and 54 years, with an observation period that extended to 2 years after the completion of treatment.60 The data collected by these authors included measurements taken from both dental casts and PA cephalograms at the following specific time intervals:
• Before SARPE or any active orthodontic alignment
• After SARPE and at the completion of orthodontic expansion
• At the removal of the orthodontic expander (i.e., approximately 6 months after SARPE and the completion of the orthodontic goals)
• Before the final orthognathic procedure (if any was planned)
• After the final orthognathic surgery and at the end of orthodontic treatment
All patients were maximally expanded 2 mm beyond the desired final position on the basis of the researchers’ assumptions that a degree of relapse was inevitable. This overcorrection ensured that, despite a measured dental relapse of 30%, none of the patients showed posterior crossbite at the completion of treatment. One can conclude that, despite retention attempts, over the long term the teeth drift back into the basal bone (see Chapters 5 and 6).
The authors also compared their relapse and stability results with other published SARPE studies. Their measured 30% relapse rate was found to be less than the 36% relapse reported by Byloff and Mossaz.56 Alternatively, their 30% documented relapse rate was higher than that reported by either Berger and colleagues31 or Pogrel and colleagues.238 As previously stated, most SARPE studies—including these two—do not report relapse from a starting point of maximal expansion. However, not doing so will underestimate the level of actual relapse and may explain the differences reported.
Chamberland and Profit showed that, when a SARPE procedure is carried out with the use of optimal surgical and orthodontic techniques, maxillary expansion that is about 47% skeletal and 53% dental can be expected.59,60 The skeletal expansion that occurred with SARPE followed by strict orthodontic maintenance mechanics for approximately 5 months proved to be statistically stable. The overall relapse rate (30%) was almost totally attributable to lingual retraction (dental relapse) of the posterior teeth. As stated, the authors recommend a 2-mm excess expansion in anticipation of dental relapse. For example, in the case of a desired 8-mm first molar expansion, 10 mm of surgical expansion at the molars is recommended. The researchers documented the advantage of compensating for the inevitable buccal tipping of the posterior maxillary teeth during the expansion phase followed by an inevitable lingual dental relapse after the device is removed. Approximately 25% of their patients had more than 3 mm of dental relapse, whereas 42% had between 1 mm and 3 mm. A full 66% of patients experienced more than 2 mm of dental relapse over the long term (i.e., 2 years after debonding).
Stability and Relapse: Comparing SARPE in Adults versus RPE in Prepubertal Children
The literature confirms that, in the prepubertal child or the adolescent with an open palatal suture, a loss of about one third of the maximum expansion occurs across the first molars after non-surgical RPE. PA cephalograms performed for prepubertal patients with palatal implant markers who underwent RPE demonstrate that approximately 50% of the expansion achieved is skeletal, with the remainder being dental. This can be compared to Chamberland and Proffit’s adult SARPE data.59,60 Those authors demonstrated a mean of 3.47 mm of skeletal expansion and 2.25 mm of dental expansion (i.e., 5.12 mm of total expansion) at the first molars. They then documented a 30% relapse, the majority of which was dental. Therefore, a comparable 30% overall relapse in both the SARPE (adult) group and the RPE (prepubertal) group was found to occur. Interestingly, in the SARPE group, the maintenance of skeletal expansion was greater than that achieved in the RPE group.
Stability and Relapse in Adults: Comparing SARPE versus Segmental Le Fort I Osteotomies
The best data regarding stability after transverse expansion with segmental Le Fort I osteotomies were reported for 32 patients by Phillips and colleagues.215 Chamberland and Proffit compared the segmental Le Fort I osteotomy group of Phillips and colleagues to their SARPE study patients.59,60 They used a subgroup of Phillips and colleagues’ patients who had undergone levels of maxillary expansion that were equivalent to those of their own SARPE patients. A comparison of the findings demonstrated the following: 1) the mean relapse across the first molars was greater for the Le Fort I group, but the difference was not statistically significant; and 2) the mean relapse across the canines was greater for the SARPE group and was statistically significant.
With reference to the SARPE (two-stage) approach versus the Le Fort I segmental (single-stage) approach for the correction of complex maxillary deformities (i.e. combination of arch-width, vertical, and horizontal deformities), the author’s conclude:59,60
• Current data do not support the conclusion that SARPE procedures produce more stable expansion than Le Fort I segmental osteotomies.
• Published data regarding both PA cephalograms and measurements of dental models confirm the potential for postoperative relapse that is primarily dental rather than skeletal after transverse maxillary expansion (i.e., RPE, SARPE, or Le Fort I segmental osteotomies).
• Relapse after the arch width initially achieved by SARPE is comparable to that of other expansion procedures (i.e., segmental Le Fort I osteotomy in adults and RPE in children).
• Published data show that, with properly executed SARPE and a strict maintenance protocol for approximately 6 months, the relapse is almost entirely dental (i.e., 33% dental relapse). At the end of treatment, there is, on average, a net expansion of 67% of the total change.
• With non-surgical expansion carried out in growing individuals (i.e., RPE), the expectation is that only 50% of the total change will be skeletal. No data from sequential PA cephalograms exists for Le Fort I segmental expansion.
• Given the similarity of relapse in intermolar width between SARPE and Le Fort I segmental techniques, routine overcorrection and strict maintenance for 6 months after surgery should be considered part of the protocol.
• When surgery to reposition the maxilla vertically or anteroposteriorly is also required, the routine performance of a preliminary SARPE procedure followed later by a Le Fort I osteotomy with the intention of obtaining better transverse stability does not appear to be warranted.
• According to published literature, the decision to use a two-stage surgical approach (i.e. first stage SARPE) versus a single-stage Le Fort I segmental surgical approach should not be based on the expected stability of the transverse expansion. Instead, it should be based on the risk and morbidity of two surgeries versus the risk and morbidity of a one-stage multisegmented Le Fort I osteotomy for arch expansion and the other necessary vertical or anteroposterior changes required for the correction of the individual’s specific dentofacial deformity.
• Clinicians should also take into account that the SARPE procedure will result in areas of fibrous union and defects at the maxillary osteotomy sites. If a Le Fort I is later required to complete the reconstruction, the previous SARPE procedure may add to the complexity of the operation (see Fig. 17-13).
References
1. Abeloos, J, De Clercq, C, Neyt, L. Skeletal stability following miniplate fixation after bilateral sagittal split osteotomy for mandibular advancement. J Oral Maxillofac Surg. 1993; 51:366–369.
2. Ackerman, JL, Proffit, WR. Communication in orthodontic treatment planning: Bioethical and informed consent issues. Angle Orthod. 1995; 65:253–262.
3. Adlam, DM, Yau, CK, Banks, P. A retrospective study of the stability of midface osteotomies in cleft lip and palate patients. Br J Oral Maxillofac Surg. 1989; 27:265–276.
4. Ahmed, MMS. Long-term stability of anterior segmental maxillary osteotomy. Int J Adult Orthodon Orthognath Surg. 1999; 14:297.
5. Akhtar, S, Tuinzing, DB. Unfavourable splits in sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:267–268.
6. Akkaya, S, Lorenzon, S, Uçem, TT. A comparison of sagittal and vertical effects between bonded rapid and slow maxillary expansion procedures. Eur J Orthod. 1999; 21:175–180.
7. Al Yami, EA, Kuijpers-Jagtman, AM, Van’t Hof, MA. Stability of orthodontic treatment outcome: Follow-up until 10 years post-retention. Am J Orthod Dentofacial Orthop. 1999; 115:300–304.
8. Anavi, Y. Condylar positioning devices for orthognathic surgery. Are they necessary? [discussion]. J Oral Maxillofac Surg. 1994; 52:552.
9. Angell, EC. Treatment of irregularities of the permanent or adult teeth. Dent Cosmos. 1860; 540–544.
10. Angle, EH. Treatment of malocclusion of the teeth and fractures of the mandible: Angle’s system. Philadelphia: White Dental Manufacturing; 1900.
11. Araujo, A, Schendel, SA, Wolford, LM, Epker, BN. Total maxillary advancement with and without bone grafting. J Oral Surg. 1978; 36:849–858.
12. Arnett, GW. A redefinition of bilateral sagittal osteotomy (BSO) advancement relapse. Am J Orthod Dentofacial Orthop. 1993; 104:506.
13. Arpornmaeklong, P, Heggie, AA, Shand, JM. A comparison of the stability of single-piece and segmental Le Fort I maxillary advancements. J Craniofac Surg. 2003; 14:3.
14. Arpornmaeklong, P, Shand, JM, Heggie, AA. Stability of combined Le Fort I maxillary advancement and mandibular reduction. Aust Orthod J. 2003; 19:57.
15. Ayliffe, PR, Banks, P, Martin, IC. Stability of the Le Fort I osteotomy in patients with cleft lip and palate. Int J Oral Maxillofac Surg. 1995; 24:201–207.
16. Ayoub, AF, Trotman, CA, Stirrups, DR, Wilmot, JJ. Stability of bimaxillary osteotomy following surgical correction of class II skeletal deformities: A two-centre study. Br J Oral Maxillofac Surg. 1997; 35:107–115.
17. Baccetti, T, Franchi, L, Cameron, CG, McNamara, JA, Jr. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001; 71:343–350.
18. Bailey, LJ, Duong, HL, Proffit, WR. Surgical Class III treatment: Long-term stability and patient perceptions of treatment outcome. Int J Adult Orthodon Orthognath Surg. 1998; 13:35.
19. Bailey, LJ, Phillips, C, Proffit, WR, Turvey, TA. Stability following superior repositioning of the maxilla by Le Fort I osteotomy: Five-year follow-up. Int J Adult Orthodon Orthognath Surg. 1994; 9:163–173.
20. Bailey, LJ, Proffit, WR, White, RP. Trends in surgical treatment of Class III skeletal relationships. Int J Adult Orthodon Orthognath Surg. 1995; 10:108–118.
21. Bailey, LJ, White, RP, Proffit, WR, Turvey, TA. Segmental Le Fort I osteotomy for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:728–731.
22. Baker, DL, Stoelinga, PJW, Blijdorp, PA, et al. Long-term stability after inferior maxillary repositioning by miniplate fixation. Int J Oral Maxillofac Surg. 1992; 21:320.
23. Basciftci, FA, Karaman, AI. Effects of a modified acrylic bonded rapid maxillary expansion appliance and vertical chin cap on dentofacial structures. Angle Orthod. 2002; 72:61–71.
24. Baumrind, S, Korn, EL, Ben-Bassat, Y, West, EE. Quantitation of maxillary remodeling: 2. Masking of remodeling effects when an “anatomical” method of superimposition is used in the absence of metallic implant. Am J Orthod Dentofacial Orthop. 1987; 91:463–474.
25. Bays, RA, Greco, JM. Surgically assisted rapid palatal expansion: An outpatient technique with long-term stability. J Oral Maxillofac Surg. 1992; 50:110.
26. Behrents, RG. A treatise on the continuum of growth in the aging craniofacial skeleton [PhD thesis]. Ann Arbor, Mich: University of Michigan Center for Human Growth and Development; 1985.
27. Behrents, RG, An atlas of growth in the aging craniofacial skeleton. Monograph 18, Craniofacial Growth Series. McNamara, JA, eds. Monograph 18, Craniofacial Growth Series; Vol 18. University of Michigan, Ann Arbor, Mich, 1985.
28. Behrents, RG, Growth in the aging craniofacial skeleton. Monograph 17, Craniofacial Growth Serie. McNamara, JA, eds. Monograph 17, Craniofacial Growth Serie; Vol 17. University of Michigan, Ann Arbor, Mich, 1985.
29. Bell, WH, Scheidman, GB. Correction of vertical maxillary deficiency: Stability and soft tissue changes. J Oral Surg. 1981; 39:666–670.
30. Bench, RW. Growth of the cervical vertebrae as related to tongue, face, and dentine behavior. Am J Orthod. 1963; 49:183–214.
31. Berger, JL, Pangrazio-Kulbersh, V, Borgula, T, et al. Stability of orthopedic and surgically assisted rapid palatal expansion over time. Am J Orthod Dentofacial Orthop. 1998; 114:638.
32. Betts, NJ, Vanarsdall, RL, Barber, HD, et al. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995; 10:75–96.
33. Björk, A. Facial growth in man studied with the aid of metallic implants. Acta Odontol Scand. 1955; 13:9–34.
34. Björk, A. Prediction of mandibular growth rotation. Am J Orthod. 1969; 55:585–599.
35. Björk, A, Skieller, V. Facial development and tooth eruption: An implant study at the age of puberty. Am J Orthod. 1972; 62:339–383.
36. Björk, A, Skieller, V. Growth in width of the maxilla studied by the implant method. Scand J Plast Reconstr Surg. 1977; 8:26.
37. Björk, A, Skieller, V. Growth of the maxilla in three dimensions as revealed radiographically by the implant method. Br J Orthod. 1977; 4:53–64.
38. Björk, A, Skieller, V. Normal and abnormal growth of the mandible: A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983; 5:1–46.
39. Blomqvist, JE, Ahlborg, G, Isaksson, S, et al. A comparison of skeletal stability after mandibular advancement and use of two rigid internal fixation techniques. J Oral Maxillofac Surg. 1997; 55:568–573.
40. Blomqvist, JE, Ahlborg, G, Isaksson, S, Svartz, K. A comparison of skeletal stability after mandibular advancement and use of two rigid internal fixation techniques [discussion]. J Oral Maxillofac Surg. 1997; 55:574–575.
41. Blomqvist, JE, Isaksson, S. Skeletal stability after mandibular advancement: A comparison of two rigid internal fixation techniques. J Oral Maxillofac Surg. 1994; 52:1133–1137.
42. Bloomquist, DS. The stability of segmentalized Le Fort I osteotomies with miniplate fixation in patients with maxillary hypoplasia [discussion]. J Oral Maxillofac Surg. 1995; 53:1412.
43. Borstlap, WA, Stoelinga, PJ, Hoppenreijs, TJ, et al. Stabilization of sagittal split advancement osteotomies with miniplates: A prospective, multicentre study with two-year follow-up. Part II. Radiographic parameters. Int J Oral Maxillofac Surg. 2004; 33:535.
44. Bouwman, JP, Husak, A, Putnam, GD, et al. Screw fixation following bilateral sagittal ramus osteotomy for mandibular advancement: Complications in 700 consecutive cases. Br J Oral Maxillofac Surg. 1995; 33:231–234.
45. Bouwman, JPB, Tuinzing, DB, Kostense, PJ, et al. The value of long-term follow-up of mandibular advancement surgery in patients with a low to normal mandibular plane angle. Mund Kiefer Gesichtschir. 1997; 1:311.
46. Broadbent, BH, Sr., Broadbent, BH, Jr., Golden, WH. Bolton standards of dentofacial developmental growth. St Louis: CV Mosby Company; 1976.
47. Brodie, AG. On the growth pattern of the human head from third month to the eighth year of life. Am J Anat. 1941; 68:209–262.
48. Brodie, AG. Late growth changes in the human face. Angle Orthod. 1953; 23:146–157.
49. Brown, GVI. The application of orthodontia principles to the prevention of nasal disease. Dent Cosmos. 1903; 45:765–775.
50. Brown, GVI. The surgical and therapeutic aspect of maxillary readjustment with special reference to nasal stenosis, hare lip, cleft palate and speech. Dent Cosmos. 1909; 51:7–17.
51. Brown, GVI. The surgery of oral and facial diseases and malformations, ed 4. London: Kimpton; 1938.
52. Buijs, GJ, Van Der Houwen, EB, Stegenga, B, et al. Mechanical strength and stiffness of biodegradable and titanium osteofixation systems. J Oral Maxillofac Surg. 2007; 65:2148.
53. Buijs, GJ, van der Houwen, EB, Stegenga, B, et al. Torsion strength of biodegradable and titanium screws: A comparison. J Oral Maxillofac Surg. 2007; 65:2142.
54. Burstone, CJ. Lip posture and its significance in treatment planning. Am J Orthod. 1967; 53:262–284.
55. Busby, BR, Bailey, LJ, Proffit, WR, et al. Long-term stability of class III treatment: A study of 5-year postsurgical results. Int J Adult Orthodon Orthognath Surg. 2002; 17:159.
56. Byloff, FK, Mossaz, CF. Skeletal and dental changes following surgically assisted rapid palatal expansion. Eur J Orthod. 1992; 7:37.
57. Carmen, M, Marcella, P, Giuseppe, C, et al. Periodontal evaluation in patients undergoing maxillary expansion. J Craniofac Surg. 2000; 11:491.
58. Caskey, RT, Turpin, DL, Bloomquist, DS. Stability of mandibular lengthening using bicortical screw fixation. Am J Orthod Dentofacial Orthop. 1989; 96:320.
59. Chamberland, S, Proffit, WR. Closer look at the stability of surgically assisted rapid palatal expansion. J Oral Maxillofac Surg. 2008; 66:1895–1900.
60. Chamberland, S, Proffit, WR. Short-term and long-term stability of surgically assisted rapid palatal expansion revisited. Am J Orthod Dentofacial Orthop. 2011; 139:815–822.
61. Chang, YL, Moon, SC. Cephalometric evaluation of the anterior open bite treatment. Am J Orthod Dentofacial Orthop. 1999; 115:29–38.
62. Chen, YR, Yeow, V. Multiple-segment osteotomy in maxillofacial surgery. Plast Reconstr Surg. 1999; 104:381.
63. Cheung, LK, Samman, N, Hui, E, Tideman, H. The 3-dimensional stability of maxillary osteotomies in cleft palate patients with residual alveolar clefts. Br J Oral Maxillofac Surg. 1994; 32:6–12.
64. Chow, J, Hagg, U, Tideman, H. The stability of segmentalized Le Fort I osteotomies with miniplate fixation in patients with maxillary hypoplasia. J Oral Maxillofac Surg. 1995; 53:1407.
65. Chung, C-H, Goldman, AM. Dental tipping and rotation immediately after surgically assisted rapid palatal expansion. Eur J Orthod. 2003; 25:353–358.
66. Chung, C-H, Woo, A, Zagarinsky, J, et al. Maxillary sagittal and vertical displacement induced by surgically assisted rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2001; 120:144–148.
67. Ciambotti, C, Ngan, P, Durkee, M, et al. A comparison of dental and dentoalveolar changes between rapid palatal expansion and nickel-titanium palatal expansion appliances. Am J Orthod Dentofacial Orthop. 2001; 119:11–20.
68. Coben, SE. Growth and Class II treatment. Am J Orthod. 1966; 52:5–26.
69. Costa, F, Robiony, M, Politi, M. Stability of sagittal split ramus osteotomy used to correct Class III malocclusion: Review of the literature. Int J Adult Orthodon Orthognath Surg. 2001; 16:121.
70. Cross, DL, McDonald, JP. Effect of rapid maxillary expansion on skeletal, dental, and nasal structures: A postero-anterior cephalometric study. Eur J Orthod. 2000; 22:519–528.
71. Cunningham, SJ, Crean, SJ, Hunt, NP, et al. Preparation, perceptions and problems: A long-term follow-up study of orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1996; 11:41–47.
72. Cureton, SL, Cuenin, M. Surgically assisted rapid palatal expansion: Orthodontic preparation for clinical success. Am J Orthod Dentofacial Orthop. 1999; 116:46.
73. Davis, WM, Kronman, JH. Anatomical changes induced by splitting the midpalatal suture. Angle Orthod. 1969; 39:126–132.
74. Dolce, C, Hatch, JP, Van Sickels, JE, et al. Rigid versus wire fixation for mandibular advancement: Skeletal and dental changes after 5 years. Am J Orthod Dentofacial Orthop. 2002; 121:610.
75. Dolce, C, Van Sickels, JE, Bays, RA, Rugh, JD. Skeletal stability after mandibular advancement with rigid versus wire fixation. J Oral Maxillofac Surg. 2000; 58:1219–1227.
76. Douma, E, Kuftinec, MM, Moshiri, F. A comparative study of stability after mandibular advancement surgery. Am J Orthod Dentofacial Orthop. 1991; 100:141.
77. Dowling, P, Espeland, L, Krogstad, O, et al. Duration of orthodontic treatment involving orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:146.
78. Downs, WB. Variations in facial relationships: Their significance in treatment and prognosis. Am J Orthod Dentofacial Orthop. 1948; 34:812.
79. Drommer, R, Luhr, HG. The stabilization of osteotomized maxillary segments with Luhr miniplates in secondary cleft surgery. J Maxillofac Surg. 1981; 9:166–169.
80. Edler, RJ. Problems in the orthodontic management of orthognathic cases. Eur J Orthod. 1990; 12:420.
81. Edwards, CB, Marshall, SD, Qian, F, et al. Longitudinal study of facial skeletal growth completion in 3 dimensions. Am J Orthod Dentofacial Orthop. 2007; 132:762.
82. Egbert, M, Hepworth, B, Myall, R, et al. Stability of Le Fort I osteotomy with maxillary advancement: A comparison of combined wire fixation and rigid fixation. J Oral Maxillofac Surg. 1995; 53:243.
83. Eggert, JH, Götzfried, HF, Steinhäuser, EW. Relapse potential of maxillary osteotomy in lip, jaw and palatal clefts [German]. Osterr Z Stomatol. 1983; 80:148–156.
84. Ellis, E, III. Condylar positioning devices for orthognathic surgery: Are they necessary? J Oral Maxillofac Surg. 1994; 52:536.
85. Ellis, E, III., Carlson, DS. Stability two years after mandibular advancement with and without suprahyoid myotomy: An experimental study. J Oral Maxillofac Surg. 1983; 41:426.
86. Ellis, E, III., Carlson, DS, Billups, J. Osseous healing of the sagittal ramus osteotomy: A histologic comparison of rigid and nonrigid fixation in Macaca mulatta. J Oral Maxillofac Surg. 1992; 50:718.
87. Ellis, E, III., Carlson, DS, Frydenlund, S. Stability of midface augmentation: An experimental study of musculoskeletal interaction and fixation methods. J Oral Maxillofac Surg. 1989; 47:1062.
88. Ellis, E, III., Esmail, N. Malocclusions resulting from loss of fixation after sagittal split ramus osteotomies. J Oral Maxillofac Surg. 2009; 67:2528.
89. Ellis, E, III., Gallo, WJ. Relapse following mandibular movement with dental plus skeletal maxillomandibular fixation. J Oral Maxillofac Surg. 1986; 44:509.
90. Ellis, E, III., Hinton, RJ. Histologic examination of the temporomandibular joint after mandibular advancement with and without rigid fixation: An experimental investigation in adult Macaca mulatta. J Oral Maxillofac Surg. 1991; 49:1316.
91. Ellis, E, III., Reynolds, S, Carlson, DS. Stability of the mandible following advancement: A comparison of three postsurgical fixation techniques. Am J Orthod Dentofacial Orthop. 1988; 94:38.
92. Enlow, DH. Facial growth, ed 3. Pennsylvania, London: Saunders; 1990.
93. Enlow, DH, Kuroda, T, Lewis, AB. Intrinsic craniofacial compensations. Angle Orthod. 1971; 41:271–285.
94. Enlow, DH, Moyers, R, Hunter, W, McNamara, J. A procedure for the analysis of intrinsic facial form and growth. Am J Orthod. 1969; 56:6–23.
95. Epker, BN. Superior surgical repositioning of the maxilla: Long term results. J Oral Maxillofac Surg. 1981; 9:237–246.
96. Epker, BN, Fish, LC, Transverse maxillary deficiency. Dentofacial deformities: Integrated orthodontic and surgical correction. Epker, BN, Fish, LC, eds. Dentofacial deformities: Integrated orthodontic and surgical correction; Vol II. CV Mosby Co, St Louis, 1986:618–675.
97. Epker, BN, Wessberg, GA. Mechanisms of early skeletal relapse following surgical advancement of the mandible. Br J Oral Surg. 1982; 20:175.
98. Epker, BN, Wylie, A. Control of the condylar–proximal mandibular segments after sagittal split osteotomies to advance the mandible. Oral Surg Oral Med Oral Pathol. 1986; 62:613.
99. Escenazi, LB, Schendel, SA. An analysis of Le Fort I maxillary advancement in cleft lip and palate patients. Plast Reconstr Surg. 1992; 90:779–786.
100. Espeland, L, Dowling, PA, Mobarak, KA, et al. Three-year stability of open-bite correction by 1-piece maxillary osteotomy. Am J Orthod Dentofacial Orthop. 2008; 134:60.
101. Farrell, CD, Kent, JN. Evaluation of the surgical stability of 20 cases of inverted-L and C osteotomies. J Oral Surg. 1977; 35:239.
102. Ferretti, C, Reyneke, JP. Mandibular, sagittal split osteotomies fixed with biodegradable or titanium screws: A prospective, comparative study of postoperative stability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:534.
103. Fink, DF, Smith, RJ. The duration of orthodontic treatment. Am J Orthod Dentofac Orthop. 1992; 102:45.
104. Finn, RA. Biomechanical considerations in the surgical correction of mandibular deficiency. J Oral Surg. 1980; 38:257–264.
105. Fish, LC, Epker, BN. Prevention of relapse in surgical-orthodontic treatment: Part 1. Mandibular procedures. J Clin Orthod. 1986; 20:826.
106. Foley, WL. In-vitro comparison of parameters affecting the fixation strength of sagittal split osteotomies [discussion]. J Oral Maxillofac Surg. 1995; 53:1383.
107. Foley, WL, Frost, DE, Paulin, WB, et al. Internal screw fixation: Comparison of placement pattern and rigidity. J Oral Maxillofac Surg. 1989; 47:720.
108. Franco, JE, Van Sickels, JE, Thrash, WJ. Factors contributing to relapse in rigidly fixed mandibular setbacks. J Oral Maxillofac Surg. 1989; 47:451.
109. Freihofer, HP. Results of osteotomies of the facial skeleton in adolescence. J Maxillofac Surg. 1977; 5:267–297.
110. Freihofer, HPM, Jr., Petresevic, D. Late results after advancing the mandible by sagittal splitting of the rami. J Maxillofac Surg. 1975; 3:250.
111. Fujioka, M, Fujii, T, Hirano, A. Comparative study of mandibular stability after sagittal split osteotomies: Bicortical versus monocortical osteosynthesis. Cleft Palate Craniofac J. 2000; 37:551–555.
112. Fujioka, M, Fujii, T, Hirano, A. Complete breakage of three-dimensional miniplates: Unusual complication of osteosynthesis after sagittal split osteotomy. Scand J Plast Reconstr Hand Surg. 2000; 34:259.
113. Gallo, W, Moss, M, Gaul, J. Modification of the sagittal split ramus osteotomy for retrognathia. J Oral Surg. 1976; 34:178–179.
114. Garrison, BT, Lapp, TH, Bussard, DA. The stability of Le Fort I maxillary osteotomies in patients with simultaneous alveolar cleft bone grafts. J Oral Maxillofac Surg. 1987; 45:761–766.
115. Gassman, CJ, Van Sickels, JE, Thrash, WJ. Causes, location, and timing of relapse following rigid fixation after mandibular advancement. J Oral Maxillofac Surg. 1990; 48:450.
116. Gerressen, M, Stockbrink, G, Smeets, R, et al. Skeletal stability following bilateral sagittal split osteotomy (BSSO) with and without condylar positioning device. J Oral Maxillofac Surg. 2007; 65:1297.
117. Gill, DS, El Maaytah, M, Naini, FB. Risk factors for post-orthognathic condylar resorption: A review. World J Orthod. 2008; 9:21.
118. Gonçalves, JR, Cassano, DS, Wolford, LM, et al. Postsurgical stability of counterclockwise maxillomandibular advancement surgery: Affect of articular disc repositioning. J Oral Maxillofac Surg. 2008; 66:724.
119. Greulich, WW, Pyle, SI. Radiographic atlas of skeletal development of the hand and wrist, ed 2. Stanford, Calif: Stanford University Press; 1959.
120. Guernse, YL. Stability of treatment results in Class II malocclusion corrected by full mandibular advancement surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1974; 37:668.
121. Gurstein, KW, Sather, AH, An, KN, et al. Stability after inferior or anterior maxillary repositioning by Le Fort I osteotomy: A biplanar stereocephalometric study. Int J Adult Orthodon Orthognath Surg. 1998; 13:131.
122. Haas, AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961; 31:73–90.
123. Haas, AJ. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965; 35:200–217.
124. Haas, AJ. Palatal expansion: Just the beginning of dentofacial orthopedics. Am J Orthod. 1970; 57:219–255.
125. Haas, AJ. Rapid palatal expansion: A recommended prerequisite to Class III treatment. Trans Eur Orthod Soc. 1973; 311–318.
126. Hackney, FL, Van Sickels, JE, Nummikoski, PV. Condylar displacement and temporomandibular joint dysfunction following bilateral sagittal split osteotomy and rigid fixation. J Oral Maxillofac Surg. 1989; 47:223.
127. Hadjianghelou, O, Luder, HU, von Weydlich, G. Rezidivursachen nach korrektur der progenie mit sagittaler spaltung. Informationen aus der kieferorthopädie. 1985; 17:185–204.
128. Haers, PE, Sailer, HF. Biodegradable self-reinforced poly-L/DL-lactide plate and screws in bimaxillary orthognathic surgery: Short-term skeletal stability and material related failures. J Craniomaxillofac Surg. 1998; 26:363.
129. Hagg, U, Taranger, J. Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt. Acta Odontol Scand. 1980; 38:187.
130. Hagg, U, Taranger, J. Maturational indicators and the pubertal growth spurt. Am J Orthod. 1982; 82:299–309.
131. Harada, K, Enomoto, S. Stability after surgical correction of mandibular prognathism using the sagittal split ramus osteotomy and fixation with poly-L-lactic acid screws. J Oral Maxillofac Surg. 1997; 55:464.
132. Harada, K, Tajima, K, Enomoto, S. Stability after sagittal split ramus osteotomy without post-operative maxillomandibular fixation in the treatment of prognathic patients with asymmetric mandibles. Clin Orthod Res. 1999; 2:27.
133. Hartgerink, DV, Vig, PS, Abbot, DW. The effect of rapid maxillary expansion on nasal airway resistance. Am J Orthod. 1987; 92:381–389.
134. Haymond, CS, Stoelinga, PJW, Blijdorp, PA, et al. Surgical orthodontic treatment of anterior skeletal open bite using small plate internal fixation. One to five year follow up. Int J Oral Maxillofac Surg. 1991; 20:223.
135. Hedemark, A, Freihofer, HP. The behaviour of the maxilla in vertical movements after the Le Fort I osteotomy. J Maxillofac Surg. 1978; 6:244–249.
136. Hilbe, M, Puelacher, W. Die stabilität nach sagittaler unterkieferosteotomie zur korrektur distaler und progener bisslagen. Inf Kieferortho. 1994; 26:63.
137. Hing, RN. Early relapse following bilateral sagittal split advancement. Aust Orthod J. 1989; 11:100.
138. Hirano, A, Suzuki, H. Factors related to relapse after Le-Fort I maxillary advancement osteotomy in patients with cleft lip and palate. Cleft Palate Craniofac J. 2001; 38:1–10.
139. Hochban, W, Ganss, C, Austermann, KH. Long-term results after maxillary advancement in patients with clefts. Cleft Palate Craniofac J. 1993; 30:237–243.
140. Hoffman, GR, Moloney, FB. The stability of facial osteotomies: 2. Mandibular advancement with bicortical screw fixation. Aust Dent J. 1995; 40:213.
141. Höltje, WJ, Scheuer, H. Skeletal stability and relapse patterns after Le Fort I osteotomy using miniplate fixation in patients with isolated cleft palate [discussion]. Plast Reconstr Surg. 1994; 94:59–60.
142. Hoppenreijs, TJ, Freihofer, HP, Stoelinga, PJ, et al. Skeletal and dento-alveolar stability of Le Fort I intrusion osteotomies and bimaxillary osteotomies in anterior open bite deformities: A retrospective three-centre study. Int J Oral Maxillofac Surg. 1997; 26:161–175.
143. Hoppenreijs, TJ, Freihofer, HP, Stoelinga, PJ, et al. Condylar remodelling and resorption after Le Fort I and bimaxillary osteotomies in patients with anterior open bite: A clinical and radiological study. Int J Oral Maxillofac Surg. 1998; 27:81.
144. Hoppenrejis, TJM, Stoelinga, PJW, Grace, KL, et al. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery. Int J Oral Maxillofac Surg. 1999; 28:411.
145. Hörster, W. Experience with functionally stable plate osteosynthesis after forward displacement of the upper jaw. J Maxillofac Surg. 1980; 8:176–181.
146. Houston, WJB, James, DR, Jones, E, Kavvadia, S. Le Fort I maxillary osteotomies in cleft palate cases: Surgical changes and stability. J Craniomaxillofac Surg. 1989; 17:9–15.
147. Houston, WJB, Jones, E, James, DR. A method of recording change in maxillary position following orthognathic surgery. Eur J Orthod. 1987; 9:9–14.
148. Hwang, SJ, Haers, PE, Sailer, HF. The role of a posteriorly inclined condylar neck in condylar resorption after orthognathic surgery. J Craniomaxillofac Surg. 2000; 28:85.
149. Iannetti, G, Chimenti, C, Di Paolo, C. Five-year follow-up of Le Fort I osteotomies. J Craniomaxillofac Surg. 1987; 15:238.
150. Ingervall, B, Thüer, U, Vuillemin, T. Stability and effect on the soft tissue profile of mandibular setback with sagittal split osteotomy and rigid internal fixation. Int J Adult Orthodon Orthognath Surg. 1995; 10:15–25.
151. Isaacson, RJ, Ingram, AH. Forces produced by rapid maxillary expansion. II. Forces present during treatment. Angle Orthod. 1964; 34:261–270.
152. Jäger, A, Kubein-Meesenburg, D, Luhr, HG. Longitudinal study of combined orthodontic and surgical treatment of class II malocclusion with deep overbite. Int J Adult Orthodon Orthognath Surg. 1991; 6:29.
153. Jeter, TS, Van Sickels, JE, Dolwick, MF. Modified techniques for internal fixation of sagittal ramus osteotomies. J Oral Maxillofac Surg. 1984; 42:270–272.
154. Joss, CU, Thüer, UW. Stability of hard and soft tissue profile after mandibular advancement in sagittal split osteotomies: A longitudinal and long-term follow-up study. Eur J Orthod. 2008; 30:16–23.
155. Kahnberg, KE, Kashani, H, Owman-Moll, P. Sagittal split advancement osteotomy: Comparison of the tendency to relapse after two different methods of rigid fixation. Scand J Plast Reconstr Surg Hand Surg. 2007; 41:167.
156. Kallela, I, Laine, P, Suuronen, R, et al. Skeletal stability following mandibular advancement and rigid fixation with polylactide biodegradable screws. Int J Oral Maxillofac Surg. 1998; 27:3.
157. Keeling, SD, Dolce, C, Van Sickels, JE, et al. A comparative study of skeletal and dental stability between rigid and wire fixation for mandibular advancement. Am J Orthod Dentofacial Orthop. 2000; 117:638.
158. Keeling, SD, LaBanc, JP, Van Sickels, JE, et al. Skeletal change at surgery as a predictor of long-term soft tissue profile change after mandibular advancement. J Oral Maxillofac Surg. 1996; 54:134.
159. Kerstens, JCK, Tuinzig, DB, Golding, RP, et al. Condylar atrophy and osteoarthritis after bimaxillary surgery. Oral Surg Oral Med Oral Pathol. 1990; 69:274.
160. Kierl, MJ, Nanda, RS, Currier, GF. A 3-year evaluation of skeletal stability of mandibular advancement with rigid fixation. J Oral Maxillofac Surg. 1990; 48:587.
161. Kim, YJ, Oh, KM, Hong, JS, et al. Do patients treated with bimaxillary surgery have more stable condylar positions than those who have undergone single jaw surgery. J Oral Maxillofac Surg. 2012; 70:2143–2152.
162. Kirkpatrick, TB, Woods, MG, Swift, JQ, et al. Skeletal stability following mandibular advancement and rigid fixation. J Oral Maxillofac Surg. 1987; 45:472.
163. Knaup, CA, Wallen, TR, Bloomquist, DS. Linear and rotational changes in large mandibular advancements using three or four fixation screws. Int J Adult Orthodon Orthognath Surg. 1993; 8:245.
164. Kobayashi, T, Watanabe, I, Ueda, K, Nakajima, T. Stability of the mandible after sagittal ramus osteotomy for correction of prognathism. J Oral Maxillofac Surg. 1986; 44:693–697.
165. Kohn, DH, Richmond, EM, Dootz, ER, et al. In vitro comparison of parameters affecting the fixation strength of sagittal split osteotomies. J Oral Maxillofac Surg. 1995; 53:1374.
166. Komori, E, Aigase, K, Sugisaki, M, Tanabe, H. Skeletal fixation versus skeletal relapse. Am J Orthod Dentofacial Orthop. 1987; 92:412–421.
167. Koudstaal, MJ, Poort, LJ, van der Wal, KG, et al. Surgically assisted rapid maxillary expansion (SARME): A review of the literature. Int J Oral Maxillofac Surg. 2005; 34:709.
168. Krebs, A. Midpalatal suture expansion studied by the implant method over a seven-year period. Trans Eur Orthod Soc. 1964; 40:131–142.
169. Krekmanov, L. Orthognathic surgery without the use of postoperative intermaxillary fixation: A clinical and cephalometric evaluation of surgical correction of mandibular and maxillary deformities. Swed Dent J Suppl. 1989; 61:8–62.
170. Krekmanov, L, Lilja, J, Ringqvist, M. Simultaneous correction of maxillary and mandibular dentofacial deformities without the use of postoperative intermaxillary fixation: A clinical and cephalometric study. Int J Oral Maxillofac Surg. 1988; 17:363–370.
171. Kretschmer, WB, Baciut, G, Baciut, M, et al. Transverse stability of 3-piece Le Fort I osteotomies. J Oral Maxillofac Surg. 2011; 69:861–869.
172. Kufner, J. Four-year experience with major maxillary osteotomy for retrusion. J Oral Surg. 1971; 29:549–553.
173. Kundert, M, Hadjianghelou, O. Condylar displacement after sagittal splitting of the mandibular rami. J Maxillofac Surg. 1980; 8:278–287.
174. LaBanc, JP, Turvey, TA, Epker, BN. Results following simultaneous mobilization of the maxilla and mandible for the correction of dentofacial deformities: Analysis of 100 consecutive patients. Oral Surg. 1982; 54:607–612.
175. Lagravere, MO, Carey, J, Heo, G, et al. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion: A randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010; 137:e1.
176. Lagravere, MO, Major, PW, Flores-Mir, C. Dental and skeletal changes following surgically assisted rapid maxillary expansion. Int J Oral Maxillofac Surg. 2006; 35:481.
177. Lanigan, DT, Romanchuk, K, Olson, CK. Ophthalmic complications associated with orthognathic surgery. J Oral Maxillofac Surg. 1993; 51:480.
178. Larsen, AJ, Van Sickels, JE, Thrash, WJ. Postsurgical maxillary movement: A comparison study of bone plate versus wire osseous fixation. Am J Orthod Dentofacial Orthop. 1989; 95:334.
179. Lavergne, J, Gasson, N. A metal implant study of mandibular rotation. Angle Orthod. 1976; 46:144–150.
180. Lee, J, Piecuch, JF. The sagittal ramus osteotomy: Stability of fixation with internal miniplates. Int J Oral Maxillofac Surg. 1992; 21:326.
181. Leonard, MS. Maintenance of condylar position after sagittal split osteotomy of the mandible. J Oral Maxillofac Surg. 1985; 43:391.
182. Li, KK, Meara, JG, Rubin, PA. Orbital compartment syndrome following orthognathic surgery. J Oral Maxillofac Surg. 1995; 53:964.
183. Lindorf, HH. Functionally stable tandem screw fixation in sagittal ramus osteotomy. Surgical technique. Dtsch Z Mund Kiefer Gesichtschir. 1984; 8:367–373.
184. Lindorf, HH. Sagittal ramus osteotomy with tandem screw fixation: Technique and results. J Maxillofac Surg. 1986; 14:311.
185. Lines, PA. Adult rapid maxillary expansion with corticotomy. Am J Orthod. 1975; 67:44–56.
186. Lo, FM, Shapiro, PA. Effect of presurgical incisor extrusion on stability of anterior open bite malocclusion treated with orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1998; 13:23–34.
187. Louis, PJ, Waite, PD, Austin, RB. Long-term skeletal stability after rigid fixation of Le Fort I osteotomies with advancements. Int J Oral Maxillofac Surg. 1993; 22:82–86.
188. Luhr, HG. Zur stabilen osteosynthese bei unterkiefer–frakturen. Dtsch Zahnarztl Z. 1968; 23:754.
189. Luhr, HG. Skelettverlagernde operationen zur harmonisierung des gesichtsprofils––probleme der stabilen fixation von osteotomiesegmenten. In: Pfeifer Gvon, ed. Die esthetik von form und funktion in der plastischen und wiederherstellungs–chirurgie. Berlin: Springer-Verlag; 1985:87.
190. Luther, F, Morris, DO, Hart, C. Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study. Br J Oral Maxillofac Surg. 2003; 41:401.
191. Luyk, NH, Ward, BR. The stability of Le Fort I advancement osteotomies using bone plates without bone grafts. J Maxillofac Surg. 1985; 13:250–253.
192. Macintosh, RB. Experience with the sagittal split osteotomy of the mandibular ramus. A 13-year review. J Maxillofac Surg. 1981; 9:151–164.
193. Major, PW, Philippson, GE, Glover, KE, et al. Stability of maxilla downgrafting after rigid or wire fixation. J Oral Maxillofac Surg. 1996; 54:1287.
194. Marchetti, C, Gentile, L, Bianchi, A, Bassi, M. Semirigid fixation of the mandible in bimaxillary orthognathic surgery: Stability after 18 months. Int J Adult Orthodon Orthognath Surg. 1999; 14:37–45.
195. Marchetti, C, Pironi, M, Bianchi, A, et al. Surgically assisted rapid palatal expansion vs. segmental Le Fort I osteotomy: Transverse stability over a 2-year period. J Craniomaxillofac Surg. 2009; 37:74.
196. Mayo, KH, Ellis, E, III. Stability of the mandible after advancement and use of dental plus skeletal maxillomandibular fixation: An experimental investigation in Macaca mulatta. J Oral Maxillofac Surg. 1987; 45:243.
197. McCance, AM, Moss, JP, James, DR. Stability of surgical correction of patients with skeletal III and skeletal II anterior open bite, with increased maxillary mandibular planes angle. Eur J Orthod. 1992; 14:198.
198. McDonald, WR, Stoelinga, PJ, Blijdorp, PA, Schoenaers, JA. Champy bone plate fixation in sagittal split osteotomies for mandibular advancement. Int J Adult Orthodon Orthognath Surg. 1987; 2:89–97.
199. Melsen, B. A histological study of the influence of sutural morphology and skeletal maturation on rapid palatal expansion in children. Trans Eur Orthod Soc. 1972; 48:499–507.
200. Memikoglu, TU, Iseri, H. Effect of a bonded rapid maxillary expansion appliance during orthodontic treatment. Angle Orthod. 1999; 69:251–256.
201. Meng, H, Goorhuis, J, Kapila, S, Nanda, S. Growth changes in the nasal profile from 7 to 18 years of age. Am J Orthod Dentofacial Orthop. 1988; 94:317–326.
202. Merkx, MA, Van Damme, PA. Condylar resorption after orthognathic surgery: Evaluation of treatment in 8 patients. J Craniomaxillofac Surg. 1994; 22:53.
203. Miguel, JA, Turvey, TA, Phillips, C, Proffit, WR. Long-term stability of two-jaw surgery for treatment of mandibular deficiency and vertical maxillary excess. Int J Adult Orthodon Orthognath Surg. 1995; 10:235–245.
204. Miguel, JA, Turvey, TA, Phillips, G, Proffit, WR. Long-term stability of two-jaw surgery for treatment of mandibular treatment outcome. Int J Adult Orthodon Orthognath Surg. 1998; 13:35–44.
205. Mihalik, CA, Proffit, WR, Phillips, C. Long-term follow-up of Class II adults treated with orthodontic camouflage: A comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2003; 123:266–278.
206. Mobarak, KA, Espeland, L, Krogstad, O, et al. Mandibular advancement surgery in high-angle and low-angle class II patients: Different long-term skeletal responses. Am J Orthod Dentofacial Orthop. 2001; 119:368.
207. Mobarak, KA, Krogstad, O, Espeland, L, Lyberg, T. Long-term stability of mandibular setback surgery: A follow-up of 80 bilateral sagittal split osteotomy patients. Int J Adult Orthodon Orthognath Surg. 2000; 15:83–95.
208. Moen, K, Wisth, PJ, Skaale, S, et al. Dental or skeletal relapse after sagittal split osteotomy advancement surgery? Long-term follow up. J Oral Maxillofac Surg. 2011; 69:e461–e468.
209. Moenning, JE, Bussard, DA, Lapp, TH, et al. A comparison of relapse in bilateral sagittal split osteotomies for mandibular advancement: Rigid internal fixation (screws) versus inferior border wiring with anterior skeletal fixation. Int J Adult Orthodon Orthognath Surg. 1990; 5:175.
210. Moldez, MA, Sugawara, J, Umemori, M, et al. Long-term dentofacial stability after bimaxillary surgery in skeletal Class III open bite patients. Int J Adult Orthodon Orthognath Surg. 2000; 15:309.
211. Mommaerts, MY, Collado, J, Mareque Bueno, J. Morbidity related to “endo-corticotomies” for transpalatal osteodistraction. J Craniomaxillofac Surg. 2008; 36:198.
212. Moore, KE, Gooris, PJ, Stoelinga, PJ. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: Report of five cases. J Oral Maxillofac Surg. 1991; 49:448.
213. Moser, K, Freihofer, HPM. Long-term experience with simultaneous movement of the upper and lower jaw. J Maxillofac Surg. 1980; 10:271–277.
214. Moyers, RE, van der Linden, FPGM, Riolo, ML, et al. Standards of human occlusal development. Ann Arbor, Mich: University of Michigan Center for Human Growth and Development; 1976.
215. Muller, G. Growth and development of the middle face. J Dent Res. 1963; 42:385–399.
216. Nagai, I, Tanaka, N, Noguchi, M, et al. Changes in occlusal state of patients with mandibular prognathism after orthognathic surgery: A pilot study. Br J Oral Maxillofac Surg. 2001; 39:429.
217. Nance, HN. The limitations of orthodontic treatment. Am J Orthod. 1947; 33:177–223.
218. Nanda, RS. The rates of growth of several facial components measured from serial cephalometric roentgenograms. Am J Orthod. 1955; 41:658–673.
219. Nanda, RS. Growth changes in skeletal-facial profile and their significance in orthodontic diagnosis. Am J Orthod. 1971; 59:501–513.
220. Nanda, RS. Patterns of vertical growth in the face. Am J Orthod. 1988; 93:103–116.
221. Nanda, RS. Circumpubertal growth spurt related to vertical dysplasia. Angle Orthod. 1989; 59–60:113–122.
222. Nanda, RS. Growth patterns in subjects with long and short faces. Am J Orthod Dentofacial Orthop. 1990; 98:247–258.
223. Nanda, RS, Meng, H, Kapila, S, Goorhuis, J. Growth changes in the soft tissue facial profile. Angle Orthod. 1990; 60:177–190.
224. Nanda, RS, Nanda, SK. Considerations of dentofacial growth in long-term retention and stability: Is active retention needed? Am J Orthod Dentofacial Orthop. 1992; 101:297–302.
225. Northway, WM, Meade, JB, Jr. Surgically assisted rapid maxillary expansion: A comparison of technique, response, and stability. Angle Orthod. 1997; 67:309.
226. Ochoa, BK, Nanda, RS. Comparison of maxillary and mandibular growth. Am J Orthod Dentofacial Orthop. 2004; 125:148.
227. Oliveira, JA, Bloomquist, DS. The stability of the use of bilateral sagittal split osteotomy in the closure of anterior open bite. Int J Adult Orthodon Orthognath Surg. 1997; 12:101–108.
228. Ow, A, Cheung, LK. Skeletal stability and complications of bilateral sagittal split osteotomies and mandibular distraction osteogenesis: An evidence-based review. J Oral Maxillofac Surg. 2009; 67:2344.
229. Pangrazio-Kulbersh, V, Berger, JL, Kaczynski, R, et al. Stability of skeletal class II correction with 2 surgical techniques: The sagittal split ramus osteotomy and the total mandibular subapical alveolar osteotomy. Am J Orthod Dentofacial Orthop. 2001; 120:134.
230. Paulus, GW, Steinhauser, EW. A comparative study of wire osteosynthesis versus bone screws in the treatment of mandibular prognathism. Oral Surg Oral Med Oral Pathol. 1982; 54:2–6.
231. Peck, H, Peck, S. A concept of facial esthetics. Angle Orthod. 1970; 40:284–318.
232. Pepersack, WJ, Chausse, JM. Long term follow-up of the sagittal splitting technique for correction of mandibular prognathism. J Maxillofacial Surg. 1978; 6:117–140.
233. Perez, MM, Sameshima, GT, Sinclair, PM. The long-term stability of Le Fort I maxillary downgrafts with rigid fixation to correct vertical maxillary deficiency. Am J Orthod Dentofacial Orthop. 1997; 112:104.
234. Persson, G, Hellem, S, Nord, PG. Bone-plates for stabilizing Le Fort I osteotomies. J Maxillofac Surg. 1986; 14:69–73.
235. Phillips, C, Medland, WH, Fields, HW, Jr., et al. Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg. 1992; 7:139.
236. Phillips, C, Zaytoun, HS, Thomas, PM, Terry, BC. Skeletal alterations following TOVRO or BSSO procedures. Int J Adult Orthodon Orthognath Surg. 1986; 3:203–213.
237. Phillips, RM, Bell, WH. Atrophy of mandibular condyles after sagittal ramus split osteotomy: Report of case. J Oral Surg. 1978; 36:45.
238. Pogrel, MA, Kaban, LB, Vargerik, K, Baumrind, S. Surgically assisted rapid maxillary expansion in adults. Int J Adult Orthodon Orthognath Surg. 1992; 7:37–41.
239. Posnick, JC, Dagys, AP. Skeletal stability and relapse patterns after Le Fort I maxillary osteotomy fixed with miniplates: The unilateral cleft lip and palate deformity. Plast Reconstr Surg. 1994; 94:924–932.
240. Posnick, JC, Ewing, MP. Skeletal stability after Le Fort I maxillary advancement in patients with unilateral cleft lip and palate. Plast Reconstr Surg. 1990; 85:706–710.
241. Posnick, JC, Taylor, M. Skeletal stability and relapse patterns after Le Fort I osteotomy using miniplate fixation in patients with isolated cleft palate. Plast Reconstr Surg. 1994; 94:51–58.
242. Posnick, JC, Tompson, B. Modification of the maxillary Le Fort I osteotomy in cleft-orthognathic surgery: The unilateral cleft lip and palate deformity. J Oral Maxillofac Surg. 1992; 50:666–675.
243. Posnick, JC, Tompson, B. Cleft-orthognathic surgery: Complications and long-term results. Plast Reconstr Surg. 1995; 96:255–266.
244. Proffit, WR. Stability of Le Fort I osteotomy with maxillary advancement: A comparison of combined wire fixation and rigid fixation [discussion]. J Oral Maxillofac Surg. 1995; 53:248.
245. Proffit, WR, Bailey, LJ, Phillips, C, Turvey, TA. Long-term stability of surgical open-bite correction by Le Fort I osteotomy. Angle Orthod. 2000; 70:112.
246. Proffit, WR, Miguel, JA. The duration and sequencing of surgical-orthodontic treatment. Int J Adult Orthodon Orthognath Surg. 1995; 10:35.
247. Proffit, WR, Phillips, C, Dann, C, IV. Who seeks surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990; 5:153–160.
248. Proffit, W, Phillips, C, Dann, C, Turvey, T. Stability after surgical-orthodontic correction of skeletal class III malocclusion: I. Mandibular set-back. Int J Adult Orthodon Orthognath Surg. 1991; 6:7–18.
249. Proffit, WR, Phillips, C, Prewitt, JW, Turvey, TA. Stability after surgical-orthodontic correction of skeletal Class III malocclusion: II. Maxillary advancement. Int J Adult Orthodon Orthognath Surg. 1991; 6:71–80.
250. Proffit, WR, Phillips, C, Turvey, TA. Stability following superior repositioning of the maxilla by Le Fort I osteotomy. Am J Orthod Dentofacial Orthop. 1987; 92:151–161.
251. Proffitt, WR, Phillips, C, Turvey, TA. Stability after mandibular setback: Mandible-only versus 2-jaw surgery. J Oral Maxillofac Surg. 2012; 70:e408–e414.
252. Proffit, WR, Turvey, TA, Philips, C. Orthognathic surgery: A hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996; 11:191–204.
253. Quejada, JG, Bell, WH, Kawamura, H, Zhang, X. Skeletal stability after inferior maxillary repositioning. Int J Adult Orthodon Orthognath Surg. 1987; 2:67–74.
254. Ramieri, GA, Spada, MC, Austa, M, et al. Transverse maxillary distraction with a bone-anchored appliance: dento-periodontal effects and clinical and radiological results. Int J Oral Maxillofac Surg. 2005; 34:357.
255. Raveh, J, Vuillemin, T, Lädrach, K, Sutter, F. New techniques for reproduction of the condyle relation and reduction of complications after sagittal ramus split osteotomy of the mandible. J Oral Maxillofac Surg. 1988; 46:751–757.
256. Reitzik, M. Skeletal and dental changes after surgical correction of mandibular prognathism. J Oral Surg. 1980; 38:109.
257. Ricketts, RM. The biologic significance of the divine proportion and Fibonacci series. Am J Orthod. 1982; 81(5):351–370.
258. Riolo, ML, Moyers, RE, McNamara, JA, Jr., Hunter, WST. An atlas of craniofacial growth. Ann Arbor, Mich: University of Michigan; 1974.
259. Rosen, HM. Miniplate fixation of Le Fort I osteotomies. Plast Reconstr Surg. 1986; 78:748–754.
260. Rosen, HM. Segmental osteotomies of the maxilla. Clin Plast Surg. 1989; 16:785.
261. Rosen, HM. Facial skeletal expansion: Treatment strategies and rationale. Plast Reconstr Surg. 1992; 89:798.
262. Rosenquist, B, Rune, B, Peterssen, A, et al. Condylar displacement after oblique sliding osteotomy of the mandibular rami: A stereometric and plain radiographic study. J Craniomaxillofac Surg. 1988; 16:301.
263. Rotskoff, KS, Herbosa, EG, Villa, P. Maintenance of condyle-proximal segment position in orthognathic surgery. J Oral Maxillofac Surg. 1991; 49:2.
264. Rotter, BE, Zeitler, DL. Stability of the Le Fort I maxillary osteotomy after rigid internal fixation. J Oral Maxillofac Surg. 1999; 57:1080.
265. Rubens, BC, Stoelinga, PJ, Blijdorp, PA, et al. Skeletal stability following sagittal split osteotomy using monocortical miniplate internal fixation. Int J Oral Maxillofac Surg. 1988; 17:371–376.
266. Ruston, MA. Growth at the mandibular condyle in relation to some deformities. Br Dent J. 1944; 76:57–68.
267. Sabri, R. Orthodontic objectives in orthognathic surgery: State of the art today. World J Orthod. 2006; 7:177–191.
268. Sandlkçloglu, M, Hazar, S. Skeletal and dental changes after maxillary expansion in the mixed dentition. Am J Orthod Dentofacial Orthop. 1997; 111:321–327.
269. Sarver, DM, Johnston, MW. Skeletal changes in vertical and anterior displacement of the maxilla with bonded rapid palatal expansion appliances. Am J Orthod Dentofacial Orthop. 1989; 95:462–466.
270. Savara, BS, Singh, IJ. Norms of size and annual increments of seven anatomical measures of maxillae in boys from 3 to 16 years of age. Angle Orthod. 1968; 38:104.
271. Schatz, J-P, Tsimas, P. Cephalometric evaluation of surgical-orthodontic treatment of skeletal Class III malocclusion. Int J Adult Orthodon Orthognath Surg. 1995; 10:173–180.
272. Scheerlinck, JP, Stoelinga, PJW, Blijdorp, PA, et al. Sagittal split advancement osteotomies stabilized with miniplates: A 2–5-year follow-up. Int J Oral Maxillofac Surg. 1994; 23:127–131.
273. Schubert, P, Bailey, LJ, White, RP, Proffit, WR. Long-term cephalometric changes in untreated adults compared to those treated with orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:91–99.
274. Schudy, F. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964; 34–35:75–93.
275. Scott, J. The analysis of facial growth: I. The anteroposterior and vertical dimensions. Am J Orthod. 1958; 44:507–512.
276. Seigel, ML. Mechanisms of early maxillary growth: Implications for surgery. J Oral Surg. 1976; 34:106.
277. Seitz, O, Landes, CA, Philipp, DJ, et al. Reliable surgically assisted rapid palatal expansion by maxillary widening device. J Craniofac Surg. 2008; 19:846.
278. Sesenna, E, Raffaini, M. Bilateral condylar atrophy after combined osteotomy for correction of retrusion: A case report. J Oral Maxillofac Surg. 1985; 13:263.
279. Shand, JM, Heggie, AA. Use of a resorbable fixation system in orthognathic surgery. Br J Oral Maxillofac Surg. 2000; 38:335.
280. Shuttleworth, FK. Sexual maturation and the physical growth of girls age six to nineteen. Monograph No 5. Soc Res Child Dev (serial no 12). 1937.
281. Sillman, JH. Dimensional changes in the dental arches: Longitudinal study from birth to 25 years. Am J Orthod Dentofacial Orthop. 1964; 50:824.
282. Silva Filho, OG, Montes, LA, Torelly, LF. Rapid maxillary expansion in the deciduous and mixed dentition evaluated through posteroanterior cephalometric analysis. Am J Orthod Dentofacial Orthop. 1995; 107:268–275.
283. Silva Filho, OG, Villas Boas, MC, Capelozza Filho, L. Rapid maxillary expansion in the primary and mixed dentitions: A cephalometric evaluation. Am J Orthod Dentofacial Orthop. 1991; 100:171–181.
284. Silverstein, K, Quinn, PD. Surgically-assisted rapid palatal expansion for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:725–727.
285. Simmons, KE, Turvey, TA, Phillips, C, Proffit, WR. Surgical-orthodontic correction of mandibular deficiency: Five-year follow-up. Int J Adult Orthodon Orthognath Surg. 1992; 7:67–79.
286. Singh, IJ, Savara, BS. Norms of size and annual increments of seven anatomical measures of maxillae in girls from 3 to 17 years of age. Angle Orthod. 1968; 36:312.
287. Sittitavornwong, S, Waite, PD, Dann, JJ, et al. The stability of maxillary osteotomies fixated with biodegradable mesh in orthognathic surgery. J Oral Maxillofac Surg. 2006; 64:1631.
288. Skidmore, KJ, Brook, KJ, Thomson, WM, et al. Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofacial Orthop. 2006; 129:230.
289. Skieller, V, Björk, A, Linde-Hanson, T. Prediction of mandibular growth rotation evaluated from a longitudinal implant sample. Am J Orthod. 1984; 86:359–370.
290. Snow, MD, Turvey, TA, Walker, D, Proffit, WR. Surgical mandibular advancement in adolescents: postsurgical growth related to stability. Int J Adult Orthodon Orthognath Surg. 1991; 6:143–151.
291. Sokucu, O, Kosger, HH, Bicakci, AA, et al. Stability in dental changes in RME and SARME: A 2-year followup. Angle Orthod. 2009; 79:207.
292. Sorokolit, CA, Nanda, RS. Assessment of the stability of mandibular setback procedures with rigid fixation. J Oral Maxillofac Surg. 1990; 48:817–822.
293. Souyris, F. Sagittal splitting and bicortical screw fixation of the ascending ramus. J Maxillofac Surg. 1978; 6:198.
294. Spiessel, B. Osteosynthese bei sagittaler osteotomie nach Obwegeser/Dal Pont. Fortschr Kiefer Gesichts Chir. 1974; 18:145.
295. Spiessel, B. Rigid internal fixation after sagittal split osteotomy of the ascending ramus. In: Spiessl B, ed. New Concepts in Maxillofacial Bone Surgery. New York: Springer-Verlag; 1976:115–122.
296. Steinhäuser, EW. Advancement of the mandible by sagittal ramus split and suprahyoid myotomy. J Oral Surg. 1973; 31:516.
297. Stella, JP, Astrand, P, Epker, BN. Patterns and etiology of relapse after correction of class III open bite via subcondylar ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1986; 1:91.
298. Stoelinga, PJW, Borstlap, WA. The fixation of sagittal split osteotomies with miniplates: The versatility of a technique. J Oral Maxillofac Surg. 2003; 61:1471–1476.
299. Stromberg, C, Holm, J. Surgically-assisted rapid maxillary expansion in adults: A retrospective long-term follow-up study. J Craniomaxillofac Surg. 1995; 23:222.
300. Stroster, TG, Pangrazio-Kulbersh, J. Assessment of condylar position following bilateral sagittal split ramus osteotomy with wire fixation or rigid fixation. Int J Adult Orthodon Orthognath Surg. 1994; 9:55–63.
301. Subtelny, JD. The soft tissue profile, growth and treatment changes. Angle Orthod. 1961; 31:105–122.
302. Tanner, JM. Growth at adolescence. Oxford, UK: Blackwell Scientific; 1962.
303. Thaller, SR. Re: A comparison of the stability of single-piece and segmental Le Fort I maxillary advancements. J Craniofac Surg. 2003; 14:599.
304. Thomas, PM, Tucker, MR, Prewitt, JR, et al. Early skeletal and dental changes following mandibular advancement and rigid internal fixation. Int J Adult Orthodon Orthognath Surg. 1986; 3:171.
305. Thüer, U, Ingervall, B, Vuillemin, T. Stability and effect on the soft tissue profile of mandibular advancement with sagittal split osteotomy and rigid internal fixation. Int J Adult Orthodon Orthognath Surg. 1994; 9:175.
306. Timms, DJ. A study of basal movement with rapid maxillary expansion. Am J Orthod. 1980; 77:500–507.
307. Turvey, TA, Bell, RB, Phillips, C, et al. Self-reinforced biodegradable screw fixation compared with titanium screw fixation in mandibular advancement. J Oral Maxillofac Surg. 2006; 64:40.
308. Turvey, TA, Philips, C, Zaytoun, HS, et al. Simultaneous superior repositioning of the maxilla and mandibular advancement. Am J Orthod Dentofacial Orthop. 1988; 94:372.
309. Van Sickels, JE. A comparative study of bicortical screw and suspension wires versus bicortical screws in large mandibular advancements. J Oral Maxillofac Surg. 1991; 49:1293.
310. Van Sickels, JE, Dolce, C, Keeling, S, et al. Technical factors accounting for stability of bilateral sagittal split osteotomy advancement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:19.
311. Van Sickels, JE, Flanary, CM. Stability associated with mandibular advancement treated by rigid osseous fixation. J Oral Maxillofac Surg. 1985; 43:338–341.
312. Van Sickels, JE, Richardson, DA. Stability of orthognathic surgery: A review of rigid fixation. Br J Oral Maxillofac Surg. 1996; 34:279.
313. Van Sickels, JE, Tiner, BD, Keeling, SD, et al. Condylar position with rigid fixation versus wire osteosynthesis of a sagittal split advancement. J Oral Maxillofac Surg. 1999; 57:31.
314. Vanarsdall, RL. Transverse dimension and long-term stability. Semin Orthod. 1999; 5(3):171–180.
315. Verlinden, CR, Gooris, PG, Becking, AG. Complications in transpalatal distraction osteogenesis: A retrospective clinical study. J Oral Maxillofac Surg. 2011; 69:899.
316. Vijayaraghaven, K, Richardson, A, Whitlock, R. Post-operative relapse following sagittal split osteotomy. Br J Oral Surg. 1974; 12:63.
317. Wardrop, RW, Wolford, LM. Maxillary stability following downgraft and/or advancement procedures with stabilization using rigid fixation and porous block hydroxyapatite implants. J Oral Maxillofac Surg. 1989; 47:336–342.
318. Watzke, IM, Tucker, MR, Turvey, TA. Lag screw versus position screw techniques for rigid internal fixation of sagittal osteotomies: A comparison of stability. Int J Adult Orthodon Orthognath Surg. 1991; 6:19.
319. Watzke, IM, Turvey, TA, Phillips, C, et al. Stability of mandibular advancement after sagittal osteotomy with screw or wire fixation: A comparative study. J Oral Maxillofac Surg. 1990; 48:108.
320. Weinberg, S, Taliano, A, Taliano, A. Condylar dislocation: An unusual complication observed after mandibular osteotomy. Oral Surg Oral Med Oral Pathol. 1983; 56:581.
321. Welch, TB. Stability in the correction of dentofacial deformities: A comprehensive review. J Oral Maxillofac Surg. 1989; 47:1142–1149.
322. Wertz, R, Dreskin, M. Midpalatal suture opening: A normative study. Am J Orthod. 1977; 71:367–381.
323. Wertz, RA. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970; 58:41–66.
324. Wessberg, GA, Schendel, SA, Epker, BN. The role of suprahyoid myotomy in surgical advancement of the mandible via sagittal split ramus osteotomies. J Oral Maxillofac Surg. 1982; 40:273.
325. Westermark, A. LactoSorb resorbable osteosynthesis after sagittal split osteotomy of the mandible: A 2-year follow-up. J Craniofac Surg. 1999; 10:519.
326. White, RP, Jr., Peters, PB, Costich, ER, Page, HL, Jr. Evaluation of sagittal split-ramus osteotomy in 17 patients. J Oral Surg. 1969; 27:851.
327. Will, LA, Joondeph, DR, Hohl, TH, et al. Condylar position following mandibular advancement: its relationship to relapse. J Oral Maxillofac Surg. 1984; 42:578.
328. Will, LA, West, RA. Factors influencing the stability of sagittal split osteotomy for mandibular advancement. J Oral Maxillofac Surg. 1989; 47:813.
329. Williams, BJD, Currimbhoy, S, Silva, A, O’Ryan, FS. Complications following surgically assisted rapid palatal expansion: A retrospective cohort study. J Oral Maxillofac Surg. 2012; 70:2394–2402.
330. Williams, RL. Occlusal treatment for the postorthodontic patient. Am J Orthod. 1971; 59:431.
331. Willmar, K. On Le-Fort I osteotomy: A follow-up study of 106 operated patients with maxillo-facial deformity. Scand J Plast Reconstr Surg. 1974; 12((0):suppl 12):1–68.
332. Wolford, LM, Karras, SC, Mehra, P. Considerations for orthognathic surgery during growth: Part 1. Mandibular deformities. Am J Orthod Dentofacial Orthop. 2001; 119:95.
333. Wolford, LM, Karras, SC, Mehra, P. Considerations for orthognathic surgery during growth: Part 2. Maxillary deformities. Am J Orthod Dentofacial Orthop. 2001; 119:102.
334. Worms, FW, Spiedel, TM, Bevis, RR, Waite, DE. Post treatment stability and aesthetics of orthognathic surgery. Angle Orthod. 1980; 50(4):251–273.
335. Yaqoob, O, Patel, A, O’Neill, J. Active postsurgical orthodontic treatment: How long does it take? Br Orthod Soc Clin Effect Bull. 2006; 19:12.
336. Yashiro, K, Takada, K. Tongue muscle activity after orthodontic treatment of anterior open bite: A case report. Am J Orthod Dentofacial Orthop. 1999; 115:660–666.
337. Zimring, JF, Isaacson, RJ. Forces produced by rapid maxillary expansion: III. Forces present during retention. Angle Orthod. 1965; 35:178–186.
*References 1, 5, 8, 39–41, 43, 44, 52, 53, 58, 74, 75, 84, 86, 88, 90, 91, 98, 102, 106–108, 111–113, 116, 126–128, 131, 132, 136, 137, 140, 150, 153, 155, 156, 160–163, 165, 166, 173, 180, 181, 183, 184, 188, 189, 194, 198, 209, 230, 255, 262, 263, 265, 271, 279, 292–295, 299, 301, 304, 305, 307, 309–311, 313, 318–321, 326
*References 14, 16, 18, 20, 45, 54, 69, 76, 85, 89, 97, 101, 104, 105, 110, 120, 152, 154, 158, 164, 169, 170, 174, 192, 196, 197, 203, 204, 207, 210, 213, 216, 227–229, 232, 252, 256, 272, 273, 285, 297, 308, 312, 316, 326, 328, 334
*References 26–28, 30, 33–38, 46–48, 68, 81, 92, 94, 119, 129, 130, 201, 214, 215, 218–224, 226, 258, 266, 270, 274–276, 280, 281, 286, 289, 290, 302, 332
*References 22, 26, 52, 53, 79, 82, 87, 128, 134, 145, 147, 178, 187–189, 191, 193, 194, 233, 234, 239, 241, 244, 259, 264, 279, 287, 307, 317
*References 27, 28, 30, 33–38, 46–48, 68, 81, 92, 94, 119, 129, 130, 201, 214, 215, 218–224, 226, 258, 266, 270, 274–276, 280, 281, 286, 289, 301, 302
†References 3, 4, 11, 14–16, 18–20, 24, 29, 63, 83, 95, 99, 109, 114, 121, 135, 138, 139, 141, 142, 146, 149, 172, 179, 240, 242, 243, 245, 249, 250, 253, 273, 321, 331, 333, 334
*References 2, 7, 55, 61, 71, 77, 78, 80, 93, 100, 103, 157, 186, 190, 205, 217, 247, 246, 267, 288, 330, 335, 336
*References 6, 17, 23, 67, 70, 73, 96, 122–125, 133, 151, 168, 185, 199, 200, 268, 269, 277, 282, 283, 306, 322, 323, 337
*References 13, 21, 25, 31, 32, 42, 56, 59, 60, 62, 64–66, 167, 171, 176, 225, 235, 238, 252, 260, 284, 299, 303, 314



