56. Mallory-Weiss Tear
Definition
Mallory-Weiss tear is upper gastrointestinal bleeding produced by longitudinal mucosal lacerations (tears) at the gastroesophageal junction (cardiac sphincter). Initiation of the tear (and bleeding) can occur after a sudden rise in intragastric pressure or gastric prolapse into the esophagus.
Incidence
The incidence of Mallory-Weiss tear accounts for about 15% of all cases of upper gastrointestinal bleeding. Males are affected more than females at a rate of 2:1 to 4:1.
Etiology
Mallory-Weiss tear occurs as a result of large, rapid, transient, transmural pressure gradient generation across the area of the gastrointestinal junction. This injury may be precipitated by retching or vomiting or by violent prolapse or intussusception of the upper stomach into the lower esophagus.
Predisposing/Precipitating Factors in Mallory-Weiss Tears
• Blunt abdominal trauma
• Cardiopulmonary resuscitation
• Coughing
• Hiatal hernia
• Hiccupping
• Primal screaming therapy
• Retching
• Straining
• Vomiting
Signs and Symptoms
Signs and symptoms exclusive to Mallory-Weiss tears are lacking. The predominant signs and symptoms are related to the rate and degree of gastrointestinal trauma and bleeding.
• Abdominal pain
• Excessive alcohol use
• Excessive aspirin use
• Hematemesis
• Hematochezia
• Melena
• Syncope
Medical Management
Endoscopy is the definitive choice for both diagnosis and treatment modalities. The choice of endoscopic treatment depends on the endoscopist’s familiarity with that technique and the equipment available to accomplish the treatment. Active bleeding is frequently treated with a contact thermal method (e.g., multipolar electrocoagulation or a heater probe), which may or may not be combined with injection of epinephrine.
Injection of epinephrine at a concentration of 1:10,000 or 1:20,000 reduces bleeding and can terminate bleeding by vasoconstriction and tamponade. Vessel sclerosis with either alcohol or polidocanol has been reported successful; however, there are safer treatment methods available. Sclerosants introduce additional risks, including deep tissue necrosis and increased potential for perforation.
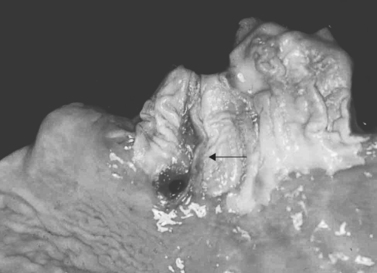 |
| Mallory-Weiss Tear. Esophageal laceration (Mallory-Weiss tears). Gross view demonstrating longitudinal lacerations extending from esophageal mucosa into stomach mucosa (arrow). |
Newer treatment modalities include argon plasma coagulation, endoscopic band ligation, and endoscopic hemoclip application. All of these modalities have demonstrated efficacy in the treatment of Mallory-Weiss tears.
Patients who are refractory to endoscopic therapies or who are at higher risk for complications from endoscopic treatment modalities may receive angiotherapy via selective vasopressin infusion or embolization of the left gastric artery.
Complications
Similar to the signs and symptoms, most complications of Mallory-Weiss tear are related to the extensiveness of gastrointestinal bleeding, the patient’s acuity, and any co-morbidities that may be present. Complications include:
• Death
• Esophageal perforation
• Hypovolemic shock
• Myocardial infarction
• Myocardial ischemia
• Organ ischemia and infarction secondary to angiotherapy
Anesthesia Implications
Mallory-Weiss tears are common among patients with alcohol abuse problems. They are also associated with patients who chronically ingest aspirin. In addition, this problem may occur after a bout of prolonged vomiting and/or retching. Endoscopic treatment modalities may necessitate general anesthesia to facilitate completion of the chosen modality. As such, rapid sequence induction must be implemented. Antiemetic measures should be administered perioperatively to minimize the development of nausea and vomiting and/or retching on emergence from the anesthetic. Vomiting and/or retching may result in a new esophageal injury with additional bleeding.
The patient’s liver function should be evaluated preoperatively because of the strong association of this malady with ethanol abuse. Co-morbidities associated with ethanol abuse may alter the intended actions of many anesthesia-related drugs.
Chronic aspirin ingestion can produce a metabolic acidosis for which the patient may compensate with a respiratory alkalosis. The metabolic alkalosis can be exacerbated by the anesthetist if the patient is hyperventilated over the course of the surgery and duration of the anesthetic. In addition, the aspirin ingestion results in interference with platelet function and may contribute to considerable intraoperative blood loss.







