CHAPTER THIRTEEN MALINGERING
INTRODUCTION
ORTHOPEDIC GAMUT 13-1 COMMONLY USED PROCEDURES IN DETERMINING EXISTENCE OF COGNITIVE MALINGERING
Not all patients who feign an illness are completely aware of their actions. Some patients embellish symptoms and physical signs as learned responses or traits, whereas others describe physical problems with hysterical emotional overlays. The latter group is influenced mostly by fear of the unknown. Depression bears a significant relationship to pain (Box 13-1).
BOX 13-1 SYMPTOMS OF DEPRESSION
Data from American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, ed 3, revised, Washington DC, 1987, American Psychiatric Association. In White AH, Schofferman JA: Spine care, vol. 1-2, St. Louis, 1995, Mosby.
ORTHOPEDIC GAMUT 13-2 DSM-IV* SYMPTOM SPECIFIC CATEGORIES IN EXCESSIVE COGNITIVE SYMPTOMS
* DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition.
NOS, Not otherwise specified.
The diagnosis of hysteria should be established based only on positive evidence. Even if the patient has an obvious hysterical disorder, a serious organic illness may still be present.
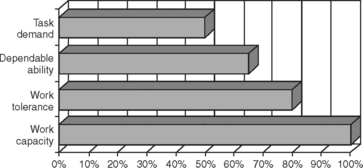
The actual percentage of patients who are malingerers is undetermined. However, estimates suggest that 2% of all patients seeking health care are malingering. Obviously, the ascertainment of the inaccuracy of a patient’s report of pain and disability is a difficult process, but the possibility of malingering should be raised in the mind of the treating physician when major discrepancies or inconsistencies appear in the patient’s medical situation. In this effort, outcome measures for the assessment of work capacity, work tolerance, dependable ability, and task demand are useful tools (Table 13-3).
TABLE 13-3 DISTINCTIONS AMONG WORK CAPACITY, WORK TOLERANCE, DEPENDABLE ABILITY, AND TASK DEMAND
 |
From Demeter SL, Andersson GBJ, Smith GM: Disability evaluation, St Louis, 1996, Mosby.
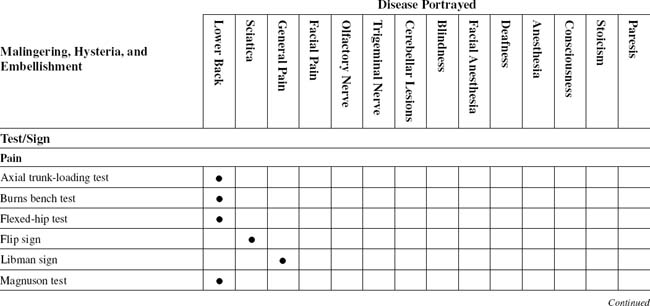
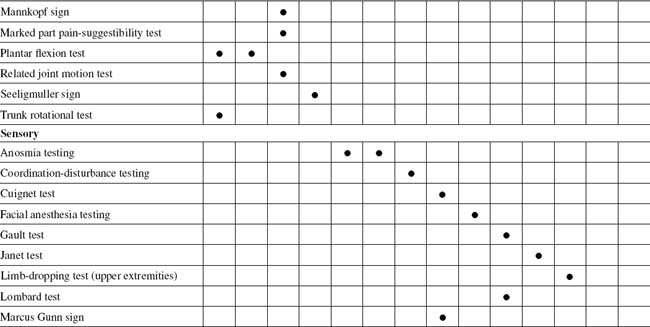
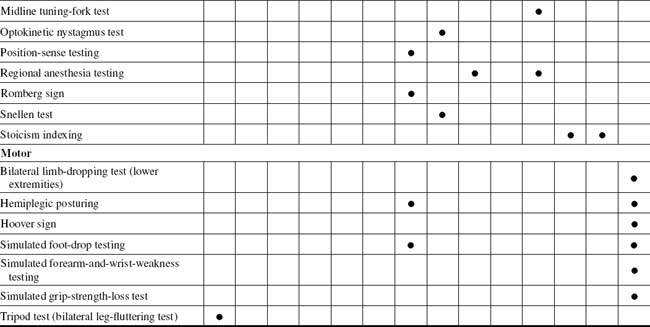
TABLE 13-2 MALINGERING, HYSTERIA, AND EMBELLISHMENT CROSS-REFERENCE TABLE BY SUSPECTED SYNDROME OR TISSUE
| Anesthesia |
ORTHOPEDIC GAMUT 13-5 IMPORTANCE OF MALINGERING ASSESSMENT
OUTCOMES ASSESSMENTS
The health assessment questionnaire (HAQ) is a self-administered instrument that assesses discomfort and disability. It is used to measure outcome in many different neuromusculoskeletal diseases. Disease-specific instruments have been produced to help follow outcomes in several other neuromusculoskeletal diseases. This area includes a fibromyalgia impact questionnaire. The activity of inflammatory neuromusculoskeletal diseases can be assessed through serologic measures. Separate measures of both tender and swollen joints can be charted on a homunculus. A generic measure of anxiety and depression, such as the hospital anxiety and depression (HAD) scale, allows psychologic variables to be assessed independently from orthopedic disease-related outcomes. The EuroQuol® thermometer is one of the instruments that uses a simple visual technique to allow people to assess their own health status; the disease repercussion profile is another such resource (Box 13-2).
BOX 13-2 DISEASE IMPACT INDEX
From Carr AJ, Thompson PW: Towards a measure of patient-perceived handicap in rheumatoid arthritis, Br J Rheumatol 33:378, 1994.
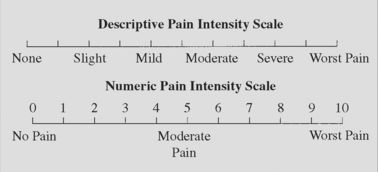
Patients report severity of problems on a 0-to-10 scale in six dimensions:
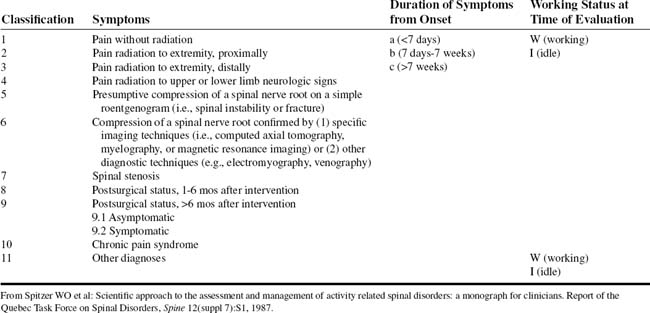
Armed with Borg pain scales, Oswestry disability indices, symptom magnification indexing, Dallas Pain Questionnaire, Waddell indexing (Table 13-4), and neuroorthopedic malingering tests, the physician is able to substantiate or refute the existence of malingering in any given case. These tests and indices are usually used in combination with the more traditional neuroorthopedic physical examinations. A singular positive finding or test does not indicate that the patient is magnifying or faking symptoms. Rather, the malingering diagnosis is based on the preponderance of positive malingering test findings and the absence of findings from traditional neuroorthopedic tests. Any positive findings must be further correlated with the medical history of the patient. The constellation of positive malingering tests, normal findings in traditional tests, and medical history discrepancies form the malingering diagnosis. Malingering and psychogenic rheumatism patients complain primarily of pain, sensory losses, or paralysis in any combination.
TABLE 13-4 NONORGANIC PHYSICAL SIGNS INDICATING ILLNESS BEHAVIOR
| Physical Disease/Normal Illness Behavior | Abnormal Illness Behavior | |
|---|---|---|
| Symptoms | ||
| Pain | Anatomic distribution | |
From Waddell G, et al: Symptoms and signs: physical disease or illness behavior? Br Med J 289:739, 1984, British Medical Association.
GENERAL PROCEDURES
Psychogenic Rheumatism Profile
ORTHOPEDIC GAMUT 13-6 REASONS FOR PSYCHOLOGIC ILLNESS THAT CAUSE THE APPEARANCE OR EXACERBATION OF PAIN
ORTHOPEDIC GAMUT 13-7 PSYCHOGENIC RHEUMATISM*
Symptoms and signs of psychogenic rheumatism are:
BOX 13-3 CLINICAL SYMPTOMS OF ANXIETY
From White AH, Schofferman JA: Spine care, vol 1-2, St Louis, 1995, Mosby.
BOX 13-4 DSM-III-R* CRITERION FOR ANXIETY
Data from American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, ed 3, revised, Washington DC, 1987, American Psychiatric Association. In White AH, Schofferman JA: Spine care, vol. 1-2, St. Louis, 1995, Mosby.
ORTHOPEDIC GAMUT 13-8 COMBINED EMORY AND ELLARD INCONSISTENCY PROFILES*
Data from Ellard J: Psychological reaction to compensable injury, Med J Australia 2:349-55, 1970; and Brena SF, Chapman SL: Pain and Iitigation: textbook of pain, London, 1984, Churchill Livingstone.
BOX 13-5 MOOD DISORDERS—DSM-III-R* CLASSIFICATIONS
Data from American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, ed 3, revised, Washington DC, 1987, American Psychiatric Association. In White AH, Schofferman JA: Spine care, vol. 1-2, St. Louis, 1995, Mosby.
* DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders, third edition, revised.
Fifth digit (x) allows coding of current state of disorder: 1 = mild; 2 = moderate; 3 = severe, without psychotic features; 4 = with psychotic features; 5 = in partial remission; 6 = in full remission; 0 = unspecified
BOX 13-6 DESCRIPTION OF MMPI-2*
From White AH, Schofferman JA: Spine care, vol 1-2, St Louis, 1995, Mosby.
L, F, and K are validity scales.
Special Hand Signals by the Patient
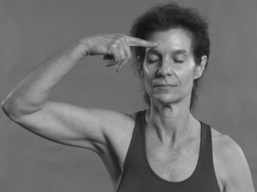
How a patient uses the hands to describe the area of pain is useful in determining the validity of the complaints. At first, malingering patients take care not to touch the area they claim experiences pain. Because the complaint is a sham, touching of the part abets the lie. The examiner often inadvertently aids this process by physically touching the area of complaint before the patient has. The patient now only has to agree with the frustrated examiner concerning the exact location of the pain (Fig. 13-1).
The psychogenic rheumatic patient uses the whole hand to paint the area of involvement with pain. Because this type of patient perceives the lesion abnormally, the distribution is painted to cover a whole body part. This pain crosses more than one dermatome boundary, and this patient’s discomfort is real. The discomfort may have origin in an organic lesion, but because of learned responses or fear, the patient rubs the whole part with the hand to indicate its extent. Careful questioning and guidance will help this patient better define the most focal trigger areas (Fig. 13-2).
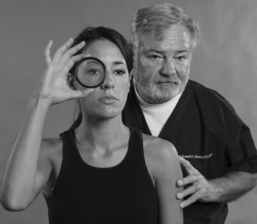
Patients with organic, pain-producing lesions are concerned that the source of the pain might be missed. When directed to point to the pain, this type of patient will touch the part with one or two fingers, which is representative of a more focal appreciation of the discomfort. In severe expression of the symptoms, this patient also may place the examiner’s hand on the exact location of the pain. These patients do not want to risk having the source missed and not treated (Fig. 13-3).
PAIN QUALIFICATION AND QUANTIFICATION
Overview
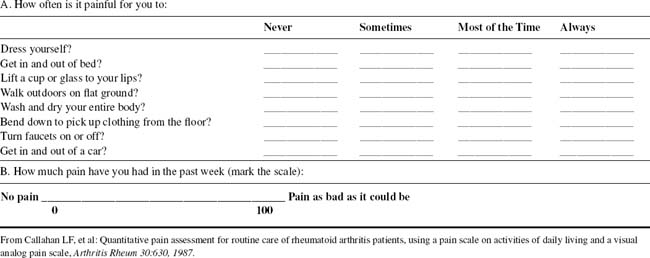
Pain disrupts the life of the individual in terms of relationships with others, self-esteem, ability to complete tasks of daily living and to work, and ability to function as a member of the community. Disability is strongly correlated with attitude to illness; these considerations underlie the importance of assessing patients’ beliefs regarding the nature and prognosis of their pain (Table 13-5).
ORTHOPEDIC GAMUT 13-9 RELAY STATIONS
Three main relay stations for sensory stimuli from the periphery to the sensory cortex include:
ORTHOPEDIC GAMUT 13-11 CLINICAL FEATURES OF BURNING MOUTH SYNDROME
Adapted from Patton LL et al: Management of burning mouth syndrome: systematic review and management recommendations, Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 103(suppl 1):S39.e1-S39.e13, 2007.
ORTHOPEDIC GAMUT 13-13 OSWESTRY-TYPE PAIN-DISABILITY QUESTIONNAIRE*
SECTION 3: LIFTING
SECTION 9: SOCIAL LIFE
AXIAL TRUNK-LOADING TEST
Assessment for Lumbar Spine Malingering
BURNS BENCH TEST
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
PLANTAR FLEXION TEST
Assessment for Feigned Low Back Pain
ORTHOPEDIC GAMUT 13-16 ACTIVE PLANTAR FLEXION
PROCEDURE
PROCEDURE
SENSORY DEFICIT QUALIFICATION AND QUANTIFICATION
Overview
ORTHOPEDIC GAMUT 13-18 SPECIFIC ASPECTS OF POSTINJURY NEUROPATHIC PAIN SYNDROMES
ANOSMIA TESTING
PROCEDURE
COORDINATION-DISTURBANCE TESTING
Assessment for Nonorganic Loss of Coordination
ORTHOPEDIC GAMUT 13-24 PRINCIPLES OF ESSENTIAL TREMOR
PROCEDURE
CUIGNET TEST
Assessment for Simulated Blindness
ORTHOPEDIC GAMUT 13-25 SUMMARY OF CLINICAL TESTS FOR FUNCTIONAL VISUAL LOSS
Adapted from Chen CS et al: Practical clinical approaches to functional visual loss, J Clin Neurosci 14(1):1-7, 2007.
| Clinical tests | Principle |
|---|---|
| Total Binocular Blindness | |
| Observation | Clue to true or simulated difficulties in visual tasks |
| Finger tip test | Proprioceptive tasks and does not require |
| Signature test | vision |
| Mirror test | Convergence, miosis and accommodation reflex |
| Optokinetic test | Optokinetic reflex of smooth pursuit |
| Pupil response | Detection of afferent and efferent pathway |
| Menace reflex | Shock value |
| Tearing reflex | Tearing with bright light |
| Monocular Blindness | |
| Pupil response | Direct afferent visual pathway light testing |
| Fogging test | Elicit better vision than claimed |
| Stereopsis testing | Require binocular vision |
| Prism shift test | Demonstrates binocular vision |
| Reduced Visual Acuity | |
| Fogging test and stereoacuity | As above |
| Reduced Visual Field | |
| Visual field to confrontation, kinetic and static perimetry | Physiological visual field characteristics |
PROCEDURE
FACIAL ANESTHESIA TESTING
Assessment for Hysterical or Simulated Face Anesthesia
PROCEDURE
GAULT TEST
Assessment for Simulated Deafness
ORTHOPEDIC GAMUT 13-28 CAUSES OF IMPAIRED HEARING
PROCEDURE
PROCEDURE
LIMB-DROPPING TEST (UPPER EXTREMITIES)
Assessment for Feigned Unconsciousness
ORTHOPEDIC GAMUT 13-31 THREE COMPONENTS OF THE GLASGOW COMA SCALE
ORTHOPEDIC GAMUT 13-32 GLASGOW COMA SCALE
| Eye Opening | |
| Spontaneous | 4 |
| To speech | 3 |
| To pain | 2 |
| None | 1 |
| Best Verbal Response | |
| Oriented | 5 |
| Confused conversation | 4 |
| Inappropriate words | 3 |
| Incomprehensible sounds | 2 |
| None | 1 |
| Best Motor Response | |
| Obeys commands | 6 |
| Localizes pain | 5 |
| Withdrawal (normal flexion) | 4 |
| Abnormal flexion (decorticate) | 3 |
| Extension (decerebrate) | 2 |
| None | 1 |
ORTHOPEDIC GAMUT 13-34 GLASGOW-LIEGE SCALE
| Brainstem Reflex | Points |
|---|---|
| Frontoorbicular | 5 |
| Vertical oculovestibular | 4 |
| Pupillary light | 3 |
| Horizontal oculovestibular | 2 |
| Oculocardiac | 1 |
| No response | 0 |
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
REGIONAL ANESTHESIA TESTING
Assessment for Feigned Anesthesia
ORTHOPEDIC GAMUT 13-35 THALAMIC PAIN
Patients with thalamic pain exhibit the following characteristics:
PROCEDURE
PROCEDURE
SNELLEN TEST
Assessment for Feigned Color Blindness
ORTHOPEDIC GAMUT 13-36 COLOR BLINDNESS
In normal (trichromatic) vision, the eye can perceive three light primaries (red, blue, and green) and can mix these in suitable portions. Thus white or any color of the spectrum can be matched. Color blindness can result from a lessened capacity to match three primary colors. It can be dichromatic vision, in which only one pair of the primary colors is perceived, the two colors being complementary to each other. Most dichromats are red-green blind and confuse red, yellow, and green (Table 13-7).
TABLE 13-7 COMPARISON OF ACQUIRED AND CONGENITAL COLOR VISION DEFICIENCIES
| Acquired Color Vision Defect | Congenital Color Vision Defect |
|---|---|
| Onset after birth | Onset at birth |
| Monocular differences in the type and severity of the defect occur frequently | Both eyes are equally affected |
| Color alterations are frequently associated with other visual problems such as low acuity and reductions in the useful visual (except in rod monochromatism) or visual field | The visual problems are specific to color perception; there are no problems with acuity field |
| The type and severity of the deficiency fluctuate throughout life | The type and severity of the defect are the same |
| The type of defect might not be easy to classify; combined or nonspecific defects occur frequently | The type of defect can be classified precisely |
| Predominantly either protan or deutan | Predominantly tritan |
| Higher incidence in men | Same incidence in both sexes |
Adapted from Lillo JA, Moreira H, Charles S: Color blindness. In Encyclopedia of applied psychology, New York, 2004, Elsevier.
PROCEDURE
PROCEDURE
PARALYSIS QUALIFICATION AND QUANTIFICATION
Overview
ORTHOPEDIC GAMUT 13-38 PSYCHOGENIC MOVEMENT DISORDERS
Psychogenic movement disorders in order of clinical frequency:
Distractibility and variability are especially common in psychogenic tremor (80% of cases) and commonly coexist with entrainment and coactivation signs (Table 13-8).
TABLE 13-8 CLINICAL CHARACTERISTICS OF PSYCHOGENIC MOVEMENT DISORDERS
| Mode of onset |
Adapted from Hinson VK, Haren WB: Psychogenic movement disorders, Lancet Neurol 5(8):695-700, 2006.
BILATERAL LIMB-DROPPING TEST (LOWER EXTREMITIES)
Assessment for Feigned Paresis of Lower Extremity
ORTHOPEDIC GAMUT 13-40 THE BARTHEL INDEX
Patient Name: ___________________________
Rater Name: ___________________________
| Activity | Score |
|---|---|
| Feeding | |
| 0 = unable | |
| 5 = needs help cutting, spreading butter, etc., or requires modified diet | |
| 10 = independent | _______ |
| Bathing | |
| 0 = dependent | |
| 5 = independent (or in shower) | _______ |
| Grooming | |
| 0 = needs to help with personal care | |
| 5 = independent face/hair/teeth/shaving (implements provided) | _______ |
| Dressing | |
| 0 = dependent | |
| 5 = needs help but can do about half unaided | |
| 10 = independent (including buttons, zips, laces, etc.) | _______ |
| Bowels | |
| 0 = incontinent (or needs to be given enemas) | |
| 5 = occasional accident | |
| 10 = continent | _______ |
| Bladder | |
| 0 = incontinent, or catheterized and unable to manage alone | |
| 5 = occasional accident | |
| 10 = continent | _______ |
| Toilet Use | |
| 0 = dependent | |
| 5 = needs some help, but can do something alone | |
| 10 = independent (on and off, dressing, wiping) | _______ |
| Transfers (bed to chair and back) | |
| 0 = unable help (one or two people, physical), can sit | |
| 10 = minor help (verbal or physical) | |
| 15 = independent | _________ |
| Mobility (on level surfaces) | |
| 0 = immobile or < 50 yards | |
| 5 = wheelchair independent, including corners, > 50 yards | |
| 10 = walks with help of one person (verbal or physical) > 50 yards | |
| 15 = independent (but may use any aid; for example, stick) > 50 yards | _________ |
| Stairs | |
| 0 = unable | |
| 5 = needs help (verbal, physical, carrying aid) | |
| 10 = independent | _________ |
| Total (0–100) | SCORE_______ |
PROCEDURE
HEMIPLEGIC POSTURING
Assessment for Nonorganic Hemiplegia
ORTHOPEDIC GAMUT 13-41 HEMIPLEGIC MOVEMENT PATTERNS IN CHILDREN WITH CEREBRAL PALSY
| Movement Patterns for the Task of Rising from a Supine Position to a Standing Position | Segmental Score |
|---|---|
| I. Upper Limb Categories | |
| a. Push and reach to bilateral push | 1 |
| b. Push and reach to asymmetric push | 2 |
| c. Symmetric push | 3 |
| d. Symmetric reach | 4 |
| e. Push and reach followed by pushing on one leg | 5 |
| f. Push and reach to bilateral push followed by pushing on leg | 6 |
| II. Axial Categories | |
| a. Full rotation with abdomen down | 1 |
| b. Full rotation with abdomen up | 2 |
| c. Partial rotation | 3 |
| d. Forward with rotation | 4 |
| e. Symmetric | 5 |
| III. Lower Limb Categories | |
| a. Pike | 1 |
| b. Pike jump to squat | 2 |
| c. Kneel | 3 |
| d. Jump to squat | 4 |
| e. Half-kneel | 5 |
| f. Asymmetric wide based squat | 6 |
| g. Narrow based symmetric squat | 7 |
PROCEDURE
HOOVER SIGN
Assessment for Feigned Leg Paresis
Neurologic loss is usually described as a sensory or motor deficit. The sensory loss may produce hypoesthesia, paresthesia, or hyperesthesia and may produce pain or numbness over a specific area. The motor deficits may be described as a weakness, as stiffness, or, more commonly, as difficulty in walking far, running, or jumping. If outright paralysis is present, the onset may have been sudden or insidious (Table 13-9). The paralysis may be flaccid or spastic. Flaccidity is associated with lower motor neuron disorders and spasticity with upper motor neuron disorders. The examiner must determine whether the symptoms have increased or decreased and to what degree the patient is disabled. The examiner must also determine whether a loss of sphincter control of the bladder and rectum has occurred.
| Potassium Deficit | |
| Group 1 | |
| Hypochloremic metabolic alkalosis | |
NH4+ Ammonium.
From Pompeo A et al: Thyrotoxic hypokalemic periodic paralysis: an overlooked pathology in Western countries, Eur J Intern Med 18(5):380–390, 2007.
PROCEDURE
PROCEDURE
SIMULATED FOREARM-AND-WRIST-WEAKNESS TESTING
PROCEDURE
SIMULATED GRIP-STRENGTH-LOSS TESTING
PROCEDURE
PROCEDURE
TABLE 13-10 CAUSES OF UNILATERAL FOOT DROP AND BILATERAL FOOT DROP
| I. Unilateral foot drop |
(Adapted from Katirji B, Michael JA, Robert BD: Causes of unilateral foot drop and bilateral foot drop. In: Encyclopedia of the neurological sciences, New York, 2003, Academic Press.)