Male genitalia
CIRCUMCISION
Appraise
1. At birth and in very young boys, the normal foreskin is non-retractile because of glanulo-preputial adhesions but the preputial orifice is unscarred and pliant. This normal appearance is clearly distinguishable from a pathological phimosis (tight non-retractile foreskin).
2. As boys mature, the glanulo-preputial adhesions separate and the foreskin becomes retractile.
3. Pathological phimosis in boys is usually caused by lichen sclerosus. The preputial orifice is pale, scarred, and non-pliant. This condition affects less than 1% of boys, peaks in incidence at age 11 and is rarely encountered before the age of 5. The condition is the main medical indication for paediatric circumcision. Recurrent balano-posthitis is a further relative indication.
4. In adults, the medical indications for circumcision are phimosis, paraphimosis (inability to reduce a retracted foreskin over the glans penis to its naturally occurring position), recurrent balano-posthitis and suspected or established penile cancer. Some men with recurrent cracking or tearing of the foreskin or frenulum and certain skin conditions refractory to medical treatment (e.g. genital warts) also benefit from circumcision.
5. In many cultures, circumcision is performed for ritual or religious reasons.
6. Patients and parents seeking circumcision should be counselled fully about the short and long-term risks and benefits of the procedure.
7. Consent should include the risk of bleeding and superficial infection as well as alteration in sexual sensation.
8. In addition to surgical circumcision, there are several non-surgical methods using a variety of clamps or constriction devices which aim to cause ischaemic necrosis of the foreskin.
Prepare
1. Adult circumcisions can be performed under general anaesthesia or with a local anaesthetic penile ring block using a combination of short-acting (lidocaine) and long-acting (bupivicaine) local anaesthetics. Calculate the dose according to the patient’s body weight and never use adrenaline. Inject a good bolus just under the pubic symphysis in the midline where the dorsal nerves pass. Inject further anaesthetic around the base of the penis in a ring.
2. Perform paediatric circumcision under general anaesthesia.
Action
1. Firstly, retract the foreskin to clean the glans. If the phimosis is severe, this can be done by placing an artery clip through the preputial opening and opening the clip to widen the orifice. If this is not possible, the tight band can be incised with tissue scissors.
2. Once the foreskin is retracted, use a probe to release the adhesions from the glans and define the coronal margin. Use antiseptic wash to thoroughly clean the glans and remove any inspissated smegma.
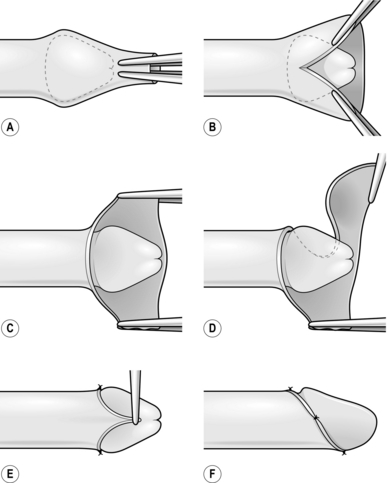
3. Replace the foreskin and apply two straight artery forceps side by side in the midline on the dorsal surface of the foreskin (Fig. 38.1A). Divide between these two forceps with scissors, taking care not to cut the glans with the inner blade of the scissors (Fig. 38.1B). Continue the incision until about 0.5 cm short of the corona (depending on the age of the child or the size of the penis), which leaves a cuff of tissue below the corona (Fig. 38.1C).
4. From the apex of this incision cut laterally around the base of the glans creating an even cuff of tissue all the way round to the frenulum on one side and then the other (Fig. 38.1D). Ensure that both the inner and outer layers of the foreskin are cut together to give a good cosmetic outcome.
5. Use bipolar diathermy to achieve haemostasis. The small artery of the frenulum may need to be tied.
6. Reconstruct the frenulum with a fine absorbable suture (Fig. 38.1E) and leave one end long to act as a stay. Place the second suture on the dorsal side in the midline and again create a stay stitch. The penis can be manipulated between the two stay sutures and the two layers of the foreskin can be opposed with fine absorbable interrupted sutures (38.1F).
ADULT CIRCUMCISION
Action
1. With a pen, mark the line of incision just above the level of the corona on the foreskin. On the ventral aspect of the penis follow the natural tapering of the corona.
2. Use a blade to incise the skin over your marked line. Take care not to sever the large veins that lie just beneath the skin. Divide the veins between clips and tie them.
3. Retract the foreskin to expose the glans. If the phimosis is very tight, use scissors to make an incision through the dorsum of the foreskin to allow retraction. Then make a second circumferential incision with the knife on the inside surface of the retracted foreskin about 0.5 cm from the corona.
4. Excise the skin between the two circumferential incisions.
5. Apply careful haemostasis with bipolar diathermy and ties where appropriate.
6. Approximate the two cleanly cut skin edges with interrupted fine absorbable sutures as described above.
FRENULOPLASTY
Appraise
1. A tight frenulum may present clinically as a non-retractile foreskin or pain on retraction, painful erections or pain on intercourse.
2. A tight frenulum may be congenital or it may result from scarring.
3. Obtain consent including possible alteration in sexual sensation, persistent symptoms and the possible need for subsequent circumcision.
Action
1. Perform this procedure under general anaesthesia or under local anaesthesia with a penile block.
2. Retract the foreskin fully and this will usually define the tight band of the frenulum.
3. Incise the frenulum transversely over the tight band, releasing the subcutaneous tissues as well as the skin. Do not incise too deeply as this may result in a urethral injury.
4. Use bipolar diathermy to achieve haemostasis.
5. Close the incision longitudinally with a fine absorbable suture. This lengthens the frenulum by 0.5–1 cm.
HYDROCELE REPAIR
Appraise
1. A hydrocele is an abnormal collection of fluid contained within the tunica vaginalis and usually surrounds the testis.
2. The testis cannot be palpated separately from the hydrocele collection.
3. Undertake surgical repair if the hydrocele produces troublesome symptoms. Asymptomatic or minimally troublesome hydroceles are best left alone.
4. Three commonly practised surgical repairs are the Lord’s plication, the Jaboulay procedure and hydrocele excision. There is minimal dissection of the hydrocele sac with Lord’s plication, resulting in a relatively bloodless procedure. This technique works well with thin-walled hydroceles that are not too large. Jaboulay eversion and excision of the hydrocele sac require more dissection of the sac, with increased opportunities for bleeding but are more suited to thick-walled hydroceles.
Action
1. Check the imaging and mark the side to be operated on.
2. Incise either along the midline raphe or use a transverse scrotal incision, avoiding small vessels in the skin.
3. Use a hand-held diathermy point to deepen the incision through the dartos layer.
4. For Lord’s procedure, incise the tunica to drain the hydrocele fluid and then extend the incision in the tunica using scissors. Make the incision large enough to deliver the testis. Note that in Lord’s procedure the hydrocele sac is not dissected from the dartos layer.
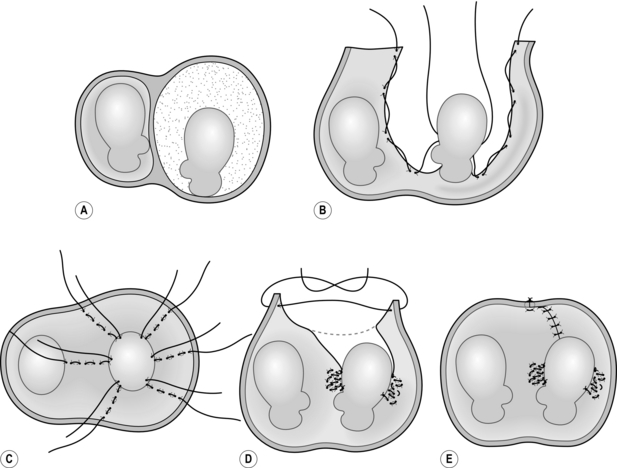
5. To perform the plication, use interrupted absorbable sutures to gather together the tunica in several small bites, starting from the cut edge and working towards the testis. Avoid placing the suture through the epididymis. After all the sutures have been placed, the tunica vaginalis appears bunched around the testis, thus obliterating the hydrocele sac (Fig. 38.2).
6. For a Jaboulay procedure, the hydrocele sac is dissected from the overlying dartos and the hydrocele and testis delivered through the incision.
7. Incise the tunica vaginalis, evert it behind the testis and re-approximate the edges around the cord and epididymis posterior to the testis, using a continuous absorbable suture.
8. Alternatively, excise the tunica vaginalis close to the testicle and achieve haemostasis by running a fine continuous absorbable suture around the cut edge.
9. Before returning the testis to the scrotum, apply meticulous haemostasis using diathermy or ties where appropriate.
10. Close the dartos using a continuous absorbable suture, taking large bites of this muscle layer to aid haemostasis.
11. Close the scrotal skin with absorbable interrupted mattress sutures.
12. A scrotal support minimizes swelling and reduces the risk of scrotal haematoma formation.
EXCISION OF EPIDIDYMAL CYSTS
Appraise
1. Excise epididymal (Greek: epi = upon + didymos = twin; upon the testes) cysts only when they become uncomfortably large.
2. Removal of epididymal cysts is relatively contraindicated in young males as it may cause epididymal damage leading to reduced fertility.
3. The condition is multiple, so warn patients that recurrent cysts are likely.
Action
1. Check any imaging and mark the side to be operated on.
2. Incise the scrotal skin as described for excision of a hydrocele sac. Deepen the incision through the scrotal layers using a handheld diathermy point or knife.
3. Deliver the testis along with its appendages, including the cysts. Remember that cysts are often multiple and commonly occur in the upper pole of the epididymis.
4. Combine blunt and scissor dissection. Hold the testis with one hand, or have an assistant hold it, while you clean off all the adventitial tissue surrounding the cyst.
5. With scissors, completely excise the cyst or else de-roof it by cutting off the whole protruding surface.
6. If there are very many cysts, excise that part of the epididymis bearing them.
7. Oversew the raw area left following this, using fine absorbable sutures.
8. Return the testis to the scrotum and close as described for hydroceles.
INGUINAL ORCHIDECTOMY
Appraise
1. Removal of a testis through a groin incision is indicated where a malignancy of the testis has been diagnosed or is suspected. This approach is taken to prevent potential seeding of tumour cells into the scrotal skin.
2. Testicular tumours usually present with a painless testicular lump which is firm and irregular on palpation, often found incidentally by the patient or his partner. When a testicular tumour is suspected, order urgent scrotal ultrasound imaging. Serum tumour markers help in the diagnosis, to predict tumour bulk and act as a marker of residual tumour after surgery. However, normal markers do not exclude malignancy.
3. Once diagnosed, testicular tumours require prompt surgery. Perform orchidectomy on the next available operating list.
4. Before surgery, offer patients the opportunity for cryogenic sperm banking, since subsequent oncological treatment may render the patient infertile.
5. If the patient requests a testicular prosthesis, this can be inserted at the time of orchidectomy or delayed until a later opportunity.
Action
1. Check the imaging and mark the side to be operated on.
2. Position the patient in the supine position and prepare the lower abdomen and external genitalia.
3. Make an incision 1–2 cm superior to the surface markings of the inguinal ligament from above the pubic tubercle extending laterally to a point just beyond the deep inguinal ring.
4. Deepen the incision through the subcutaneous tissues to expose the fibres of the external oblique aponeurosis. Clean the external oblique aponeurosis using blunt dissection, allowing clear demarcation of the inguinal ligament and external inguinal ring.
5. Use a knife to make a small incision in the external oblique aponeurosis in the direction of the fibres and, using scissors, open the inguinal canal from the deep inguinal ring to the superficial ring, exposing the spermatic cord. Locate and preserve the ilio-inguinal nerve.
6. Bluntly dissect the spermatic cord from the floor of the inguinal canal. Doubly clamp the cord close to the deep ring. The testis can then be manipulated safely.
7. Apply traction on the cord with simultaneous pressure on the scrotum to deliver the testis through the incision with its surrounding tunical coverings. The most inferior part of the testis is attached to the scrotum by the gubernaculum (Latin: rudder, from the belief it steers the line of descent of the testis). Divide and tie it.
8. Divide the cord between the double clamps thus excising the testis and cord.
9. Transfix the stump of the cord. Leave an artery clip on the surgical tie so that the stump does not retract into the abdominal cavity before complete haemostasis is achieved.
10. Control any points of bleeding in the wound and scrotal cavity to minimize the risk of scrotal haematoma.
11. Close the external oblique with a continuous 2/0 Vicryl suture and reconstruct the superficial ring. Be careful not to catch the ilio-inguinal nerve in your suture line. Scarpa’s facia can be opposed with interrupted sutures and skin closure can be with clips or a subcuticular suture.
12. A scrotal support will help to tamponade any intrascrotal bleeding.
SIMPLE ORCHIDECTOMY
Appraise
1. The indications for simple orchidectomy are:
 Severe or recurrent attacks of acute epididymitis
Severe or recurrent attacks of acute epididymitis
 Chronic epididymitis, including tuberculous epididymitis
Chronic epididymitis, including tuberculous epididymitis
 Severe testicular trauma when the testis is not salvageable
Severe testicular trauma when the testis is not salvageable
 Testicular infarction from a neglected torsion
Testicular infarction from a neglected torsion
 Hormonal treatment for advanced prostate cancer (although a subcapsular orchidectomy is often preferred in this situation).
Hormonal treatment for advanced prostate cancer (although a subcapsular orchidectomy is often preferred in this situation).
Action
1. Check any imaging and mark the side to be operated on.
2. If the condition is inflammatory and involves the skin, then make the incision in the scrotum so as to excise the overlying attached infected skin if necessary. The incision, therefore, varies in shape and size according to the condition.
3. Leave the involved skin attached to the underlying structures. Enter the scrotal sac away from the inflamed area.
4. Deliver the testicle with the overlying attached area of skin. Do not hesitate to remove all the involved surrounding skin. The scrotal skin has amazing powers of regeneration.
5. Apply gentle traction to the testicle and clean the cord structures to free about 5 cm of cord.
6. Cross-clamp the cord at this level with two strong artery forceps, dividing it between them.
7. Tie the clamped upper end with strong absorbable suture, but do not release the forceps before applying a second tie. If the cord is very thick, tease it into two structures and cross-clamp each, to avoid creating a bulky pedicle with a tie that is not secure.
8. Use finger dissection and traction on the lower divided cord to remove the testicle.
9. In the presence of severe infection, leave the scrotal wound unsutured to drain freely. Otherwise, place a corrugated Yates’ drain through the most dependent part of the scrotum and insert a few interrupted absorbable sutures to approximate the skin edges.
TESTICULAR TORSION
Appraise
1. Torsion (Latin: torquere = to twist) of the testis usually presents with acute hemi-scrotal pain in adolescents and young adults. It is rare after the age of 35 years.
2. Pain is usually severe and of sudden onset. There may be associated lower abdominal pain and vomiting.
3. The testis can become swollen and may sit high in the scrotum.
4. The testis is acutely tender on palpation.
5. The diagnosis is obvious if the patient presents with classical symptoms and signs but atypical presentation is well recognized. Always consider it when assessing any patient with acute scrotal pain.
6. Differential diagnoses include epididymo-orchitis, incarcerated inguino-scrotal hernia and, in children, torsion of the hydatid of Morgagni and idiopathic scrotal oedema.
Prepare
1. Obtain consent from the patient (and parents) for scrotal exploration, bilateral testicular fixation and possible orchidectomy for infarcted testis.
2. Inform the patient that, in the event of orchidectomy, a prosthesis can be inserted. In a child, delay this until he has reached full maturity. For an adult, a prosthesis is usually inserted at an interval after acute surgery to avoid the infective risk of inserting a foreign body into an acutely inflamed surgical site.
Action
1. Use a midline scrotal incision to allow access to both testes through the same incision. Deepen it through the dartos layer. Grasp the tunica vaginalis between two clips and open it with a knife or scissors.
2. Use scissors to further open the tunica vaginalis longitudinally. Avoid damaging the epididymis.
3. Deliver the testis and inspect it carefully. A torted testis appears dusky in colour, whilst a necrotic testis is black. Untwist the torsion and wrap the testis in a pack soaked in warm saline.
4. While you are waiting for the torted testis to recover, deliver the contralateral testis through the midline septum. Inspect it carefully and fix it using a non-absorbable prolene suture. Check the orientation of the testis before placing three sutures (medial, lateral and lower pole) between the tunica albuginea and the scrotal side wall. Avoid placing sutures in the epididymis.
5. Remove the packs from the torted testis and examine it carefully to assess viability. Remove a necrotic testis by placing heavy clips around the cord, excising the dead testis and transfixing the cord. If the testis recovers, fix it using the three-point technique as described above.
6. If the diagnosis is not torsion, look for another cause. The presence of hydrocele fluid when the tunica vaginalis is opened may suggest an intrascrotal pathology. The epididymis appears inflamed and engorged in acute epididymitis. A torted hydatid of Morgagni is recognizable as a small inflamed or necrotic piece of tissue at the upper pole of the testis. Excise it.
7. Perform careful haemostasis using diathermy before closure. Close the dartos layer with a continuous absorbable suture taking bites of the left side, the septum and the right hemiscrotum. Close the skin with interrupted undyed mattress sutures.
8. A scrotal support will help to reduce haematoma formation.
TESTICULAR TRAUMA
Appraise
1. Significant testicular trauma is uncommon and is usually a result of sporting injuries or assaults.
2. The immediate pain may be excruciating; however, the effect of adrenaline during contact sports or a brawl may lead to delayed presentation.
3. Carry out an ultrasound scan to assess for rupture of the tunica albuginea of the testis.
4. If rupture is confirmed, undertake scrotal exploration.
5. When there is no rupture and the degree of pain and swelling are stable, treat conservatively with scrotal support, rest and analgesia.
6. If ultrasound is not available, decide whether or not to explore the scrotum on clinical grounds. Recognize increasing pain and swelling as this may indicate increasing haemorrhage within the tunica vaginalis, which may compress and damage the testis.
Action
1. If the testis is completely disrupted, perform simple orchidectomy.
2. However, the testis can often be salvaged by simply evacuating the haematoma, excising any devitalized tissue and loosely tacking the split and torn tunica albuginea together. Allow plenty of space for the blood to escape. Insert a small drain if necessary.
3. Administer prophylactic antibiotics and fit a scrotal support.
VASECTOMY FOR STERILIZATION
Appraise
1. Bilateral vasectomy is a reliable and convenient method of contraception and can be performed under local anaesthesia.
2. Vasectomy is the most common cause of medical negligence claims against urologists. The most common reason for complaint is failed sterilization, but failure to warn of possible complications or to inform the patient of a positive postoperative semen analysis can also lead to claims.
3. Counsel the patient carefully before performing the procedure and document this discussion in the case notes. Enquire into the size of the patient’s family and whether the family is complete. Advise the patient that the procedure must be considered irreversible.
4. A failure rate of 1:2000 is recognized due to re-canalization of the vas.
5. Sterilization is not immediate so tell the patient to use other forms of contraception until he has been informed that two sets of semen analysis at around 12 and 14 weeks postoperatively are free of sperm (azospermia). These tests also identify the small proportion of patients with early failure due to incomplete vasal occlusion.
6. Warn the patient of a 1 in 20 risk of chronic scrotal pain. This is often caused by small sperm leaks leading to local inflammation and irritation. Sperm granulomas may cause palpable lumps as well as chronic scrotal pain.
7. Risks also include bleeding with haematoma formation and superficial skin infection.
8. Examine the scrotum and cord preoperatively to assess the accessibility of the vas. A short cord length may make a local anaesthetic procedure difficult especially in a nervous patient in a cold operating theatre.
Action
1. Palpate the cord structures through the scrotum and using your thumb, index and middle fingers identify the vas and bring it towards the scrotal skin (Fig. 38.3).
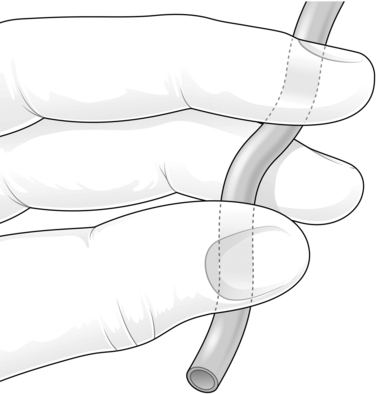
Fig. 38.3 Vasectomy: identifying the vas.
2. With the vas securely positioned, inject local anaesthetic into the scrotal skin and subcutaneous tissues over the vas.
3. Make a 0.5 cm incision in the scrotal skin directly over the vas and use a sharp tipped clip to spread the subcutaneous tissues. Use vasectomy ring forceps to grasp the vas and pull it through the skin opening. As an alternative, consider using the no-scalpel technique for this step. An extracutaneous fixation ring clamp is used to secure the vas and a sharp curved haemostat is used to puncture the scrotal skin. The no-scalpel technique is associated with a lower risk of haematoma.
4. Carefully dissect the tissue layers covering the vas using the sharp curved haemostat. When the bare white muscular coat of the vas is exposed, reposition the ring forceps so that it holds only the vas without any of the covering tissue layers.
5. Place two clips on the vas and excise a small segment for histological examination. Vasal occlusion is the next step. A number of techniques are described, for example cautery to the cut ends of the vas, tying the cut ends of the vas either simply or by doubling the vas back on itself and placing a tie around the ‘U’. Many urologists replace the two cut ends in the scrotum in separate tissue planes by suturing the loose adventitial tissue over one of the ends (fascial interposition). The choice of technique depends on the facilities available, but intra-luminal cautery of the cut end in combination with fascial interposition is associated with the lowest failure rates.
6. Apply meticulous haemostasis to reduce the incidence of haematoma formation.
7. Close the skin with one or two fine absorbable mattress sutures.
FRACTURED PENIS
Appraise
1. A fractured penis occurs as a result of blunt trauma to the erect penis with subsequent rupture of the tunica albuginea around the corpus cavernosum.
2. In Western society this is commonly due to blunt sexual trauma where the erect penis slips out of the vagina during intercourse and the penis is thrust against the partner’s perineum. If there is adequate force the erect penis will buckle and the tunica albuginea ruptures.
3. Patients often report hearing a cracking or popping noise and a sudden loss of erection. There is usually significant swelling and bruising, manifested as the ‘aubergine deformity’. Blood at the urethral meatus suggests an associated urethral injury.
4. Patients may be embarrassed to seek help, so delaying presentation.
5. Prompt repair reduces adverse long-term outcomes such as impotence or penile curvature.
6. If the diagnosis is not clear, an MRI scan may help to locate the tunical defect. Ultrasound of the penis can also be used to define the site of rupture.
Action
1. If preoperative imaging has been utilized to locate the tear in the tunica albuginea, make a 2-cm longitudinal incision over this location.
2. To explore the penis in the absence of preoperative imaging, make a distal circumferential degloving incision. This provides optimal exposure.
3. Dissect through the subcutaneous tissues, tying off any large vessels as you go. The tissues are oedematous. Keep dissecting until you reach the pale tunica albuginea. Stay in this plane and deglove the penis completely at this level.
4. You can see a haematoma at the site of the rupture. Evacuate the haematoma completely to reveal the defect in the tunica.
5. Close the laceration using a continuous or interrupted absorbable suture.
6. Perform careful haemostasis, replace the penile skin over the shaft and close the skin with fine interrupted absorbable sutures.
PRIAPISM
Appraise
1. Priapism (Greek: Priapos was an ancient god personifying male virility and sexuality), is a persistent, often painful, erection in the absence of sexual stimulation. Since it is frequently due to underlying medical conditions, consider it both as a medical and surgical emergency.
2. Whatever the cause, commence treatment as soon as possible. Involve the appropriate medical specialty; for example, if the priapism is due to a sickle cell crisis then consult the haematologists.
3. If there is delay, the resulting stasis of blood in the corpora and subsequent fibrosis lead to impotence. Even with early treatment, impotence is common.
4. Carry out the simplest procedure to obtain detumescence (Latin: de- = reversal + tumere = to swell) and then refer the patient to a specialist centre.
Aspiration
1. Initial attempts at detumescence are carried out under local anaesthesia. Perform a penile ring block as described above for circumcision.
2. Use a 20-ml syringe with a wide-bore butterfly needle. Insert the needle into the base of one of the corpora in the 3 o’clock or 9 o’clock position.
3. Aspirate blood from the penis. You may need to adjust the position of the needle for optimum results. You may need to aspirate several hundred millilitres of blood to achieve detumesence. Aspiration alone has a success rate of 30%.1
Irrigation
1. Insert a wide-bore aspiration needle into the distal end of one corpus cavernosum and another into the proximal end of the opposite one.
2. Irrigate with 100–200 ml of physiological saline or heparin saline into the proximal needle.
3. Eventually, the fluid emerging from the opposite needle is reasonably clear. Each injection of fluid causes a considerable hardening of the priapism.
4. Massage the corpora to facilitate escape of the fluid, making them flaccid. If necessary, insert four needles into the corpora.
Intracavernosal vasoconstrictors
1. For persistent priapism make up a 100 μg/ml solution of phenylephrine in normal saline (1 ml containing 10 mg, diluting it to 100 ml with normal saline). Inject 3–5 ml into the corpora, repeated at 10-minute intervals until the erection subsides.
2. Be aware of possible adverse sympathomimetic effects – hypertension, headache, reflex bradycardia, tachycardia, palpitations and arrhythmia. Monitor the patient’s blood pressure, pulse and, in patients with high cardiovascular risk, the electrocardiogram.
3. Apply a firm bandage and return the patient to the ward. This technique is highly effective if carried out within the first 12 hours of onset.2
4. It may be necessary to repeat this process three or four times over the ensuing 48 hours before the corpora remain flaccid.
5. If the priapism persists despite these measures, refer to a specialist.
REFERENCES
1. Montague, D.K., Jarow, J., Broderick, G.A., et al. American Urological Association guideline on the management of priapism. J Urol. 2003; 170:1318–1325.
2. Kulmala, R.V., Tamella, T.L. Effects of priapism lasting 24 hours or longer caused by intracavernosal injection of vasoactive drugs. Int J Impot Res. 1995; 7:131–136.
Blandy, J. Radical cure of hydrocoele. In: Blandy J., ed. Operative Urology. 2nd ed. Oxford: Blackwell Scientific; 1986:246–247.
Blandy, J., Fowler, C. Circumcision. In: Blandy J., Fowler C., eds. Urology. 2nd ed. Oxford: Blackwell Scientific; 1996:445–447.
Blandy, J., Fowler, C. Orchidopexy. In: Blandy J., Fowler C., eds. Urology. 2nd ed. Oxford: Blackwell Scientific; 1996:553–556.
Blandy, J., Fowler, C. Torsion of the testis. In: Blandy J., Fowler C., eds. Urology. 2nd ed. Oxford: Blackwell Scientific; 1996:569–571.
Dittrich, A., Albrecht, K., Bar-Moshe, O., et al. Treatment of pharmacological priapism with phenylephrine. J Urol. 1991; 146:323.
Rickwood, A.M.K. Medical indications for circumcision. BJU Int. 1999; 83(Suppl. 1):45–51.
Whitfield, H.N., Hendry, W.F., Kirby, R.S., Duckett, J.W. Textbook of Genitourinary Surgery, 2nd ed. Oxford: Blackwell Scientific, 1998.