Chapter 8 Magnetic resonance angiography
Introduction
Recent innovations in CMR hardware, such as stronger gradients and faster gradient switching, and software, such as newer pulse sequences and ultrafast MRA techniques, continue to ensure that it is the noninvasive imaging modality of choice in many diseases affecting the great vessels.
MRA techniques
Contrast-enhanced MRA
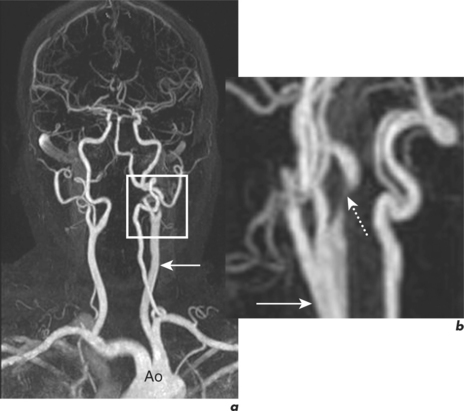
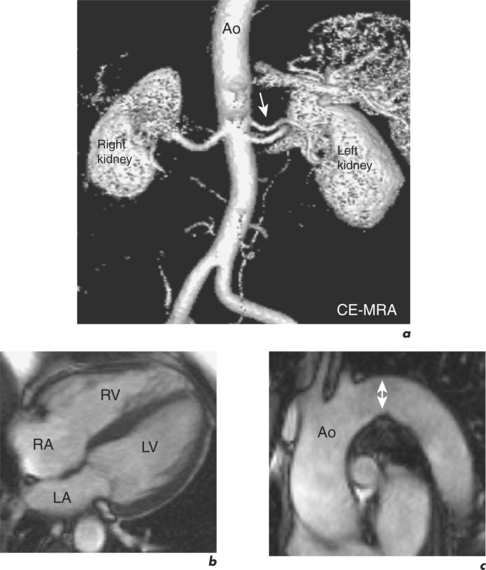
The basic pulse sequence for ultrafast CE-MRA is a 3D GE acquisition which is usually designed to acquire data encoding for contrast first—centric-ordering. The use of gadolinium contrast agent shortens the T1 value of blood so that it appears bright irrespective of flow patterns or velocities (Figure 8.1).
Time-of-flight (2D or 3D)
This is an older GE technique in which flow signal is enhanced by inflow effects. Stationary tissue within a region of interest is saturated by rapid application of RF pulses. This results in fresh blood flowing into this plane being non-saturated and therefore appearing bright. Unwanted venous signal can be eliminated by application of specific saturation bands. Time-of-flight methods are sensitive to flow velocity; for example, slow flow near the vessel wall appears less bright with this technique than faster flow in the middle of the vessel. Importantly, the 2D time-of-flight sequence has the disadvantage of overestimating vessel stenosis due to a phenomenon known as phase dispersion. This effect is less pronounced using 3D time-of-flight imaging.
Post-processing methods
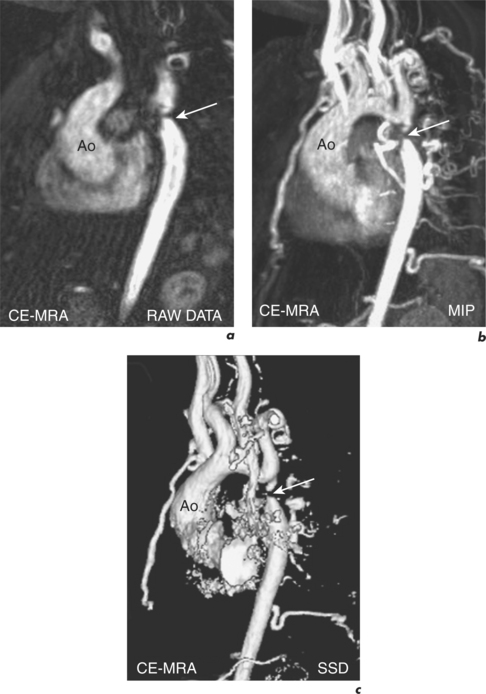
Post-processing algorithms are used to create 3D images. However, they must always be interpreted together with the source images, the ‘raw data’, to avoid misinterpretation from post-processing induced artefacts (Figure 8.2).
Maximal intensity projection
In this ray tracing post-processing algorithm, the desired viewing plane is specified first. Then the maximum intensity encountered in parallel rays along this viewing plane is assigned to the displayed pixel. MIP reconstructions are applicable to both time-of-flight and CE-MRA data and have the tendency to overestimate the degree of vessel stenosis (Figure 8.2b).
Volume rendering technique and shaded surface display
This is a ray casting algorithm which selects visible voxels by tracing rays from an instantaneous viewing position. The surfaces are identified by a threshold technique and the resulting SSD provides 3D appreciation of the vessel. Resulting images can also overestimate the degree of vessel stenosis (Figure 8.2c).
Specific Sites
Carotid arteries
The most commonly used sequences for carotid MRA are time-of-flight and CE-MRA (Figure 8.1). For imaging of the aortic arch and cervical arteries, CE-MRA is the only option. Both 3D TOF and CE-MRA are as accurate as conventional X-ray angiography in the measurement of internal carotid artery stenosis, and because of the small but significant risk of stroke with the invasive technique (0.5–1.0%), CMR is recommended as the optimal method of evaluating carotid artery disease. Data interpretation requires careful evaluation of the raw data to avoid overestimation of stenosis severity. MIP projections will aggravate signal loss and cause vessels to appear narrower because the algorithm selects brightest intensities both within the vessel and in the background. Such overestimation with MIPs is more of a problem in 3D time-of-flight than with CE-MRA, in which background intensities are suppressed.
CE-MRA can also visualize stenoses within the vertebral artery or within the basilar artery. Reversal of blood flow in the vertebral artery with subclavian steal phenomenon is recognized using CE-MRA in combination with through-plane velocity mapping CMR (after handgrip exercise) at the level of the vertebral arteries. Confirmation is with 2D time-of-flight MRA acquired first with an inferior and then a superior saturation band to confirm flow reversal.
Pulmonary vessels
Pulmonary arteries
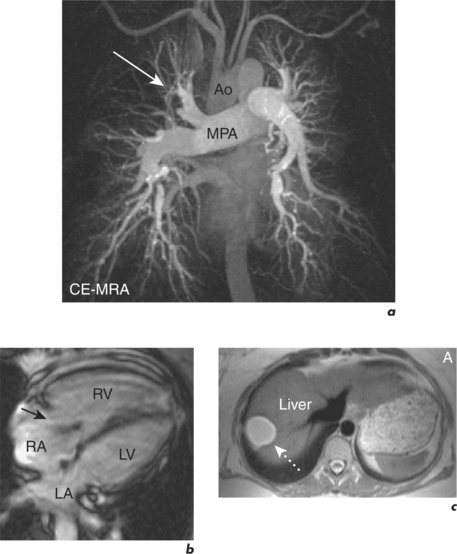
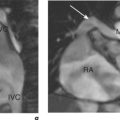
CMR is well suited for the evaluation of PA anatomy and this is widely used in patients with ACHD where evaluation of the size, patency and anatomical relations of the PAs is combined with RV assessment and PV status. It is also being increasingly used in the assessment of patients with pulmonary hypertension (Figure 8.3). CT pulmonary angiography remains the imaging modality of choice for diagnosis of acute pulmonary embolism since MRA has longer acquisition, and thus breath-hold times, and lower spatial resolution leading to smaller peripheral emboli potentially going undetected.
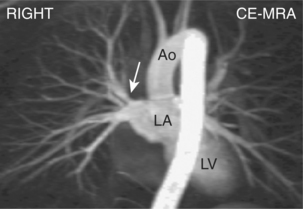
Pulmonary veins
The use of CMR in the diagnosis and differentiation of the various forms of partial and total APVD has already been discussed. Additionally, it has a role in the evaluation of the pulmonary veins and LA pre-radiofrequency ablation for cardiac arrhythmias. Subsequent assessment of pulmonary vein stenosis requires CE-MRA combined with velocity mapping (Figure 8.4).
Renal and mesenteric arteries
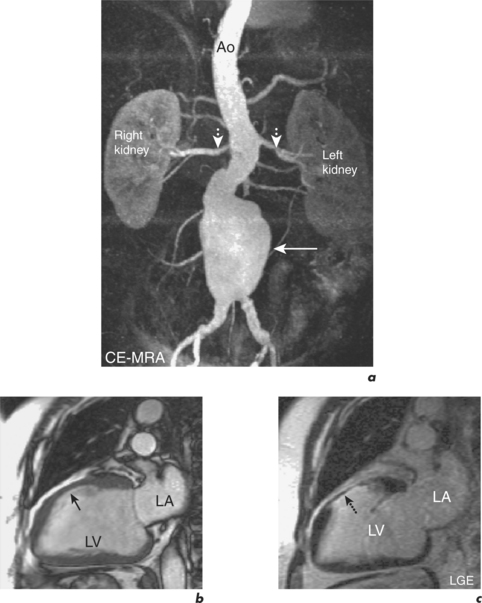
CMR screening protocols for secondary causes of hypertension conclude with angiography and are performed during an hour-long study in the following manner:
Published data related to mesenteric CE-MRA is limited. Anecdotally, results appear comparable to renal angiography. Most stenoses in the coeliac trunk and superior mesenteric artery occur within the proximal segment where the diameter of the vessel is the greatest. The inferior mesenteric artery is often less well visualized since it is smaller and consequently stenoses at this site are often overestimated by CMR.
Aorta
The thoracic aorta has already been discussed in Chapter 6. Optimal visualization of the aorta is via a combination of SE and GE techniques to ensure accurate evaluation of the aortic wall and peri-aortic tissues, and lumen, respectively. With inflammatory conditions, such as aortitis, contrast agents are used to further highlight aortic wall abnormalities. CE-MRA readily depicts location, extent and exact diameter of aortic aneurysms with measurements being made on the original images (Figure 8.6). In cases of aortic dissection where there is continuation to the abdominal aorta it is important to know whether side branches originate from the true or false lumen. CT is often the modality of choice for investigating acute pathology of the aorta, for reasons of both safety and availability, while CMR is an ideal method for patient follow-up following surgical or medical treatment.
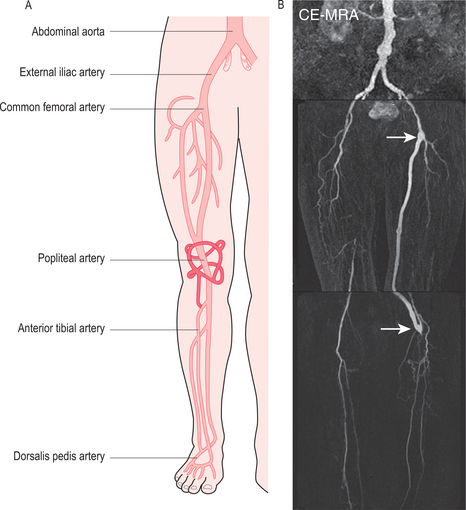
Peripheral arteries
CE-MRA is the best CMR technique for evaluating arterial disease in the upper and lower limbs. Visualization of the subclavian and brachial arteries requires a dedicated body coil, otherwise the technique is similar to that of thoracic aorta MRA. In order to avoid venous overlap the contrast should be injected in the contralateral arm. Imaging of the small arteries of the hand requires high-resolution scanning, dedicated surface coils, and precise timing of the start of imaging. An additional use of CE-MRA is in the diagnosis of thoracic outlet syndrome where images are acquired with the arms in abduction and in neutral position (Figure 8.7). High-resolution targeted T1W SE sequences are required to demonstrate the cause of compression in this condition.
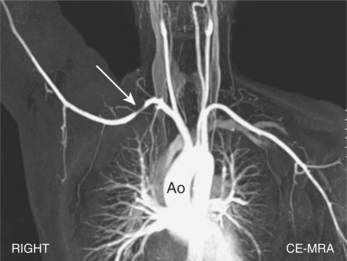
Figure 8.7 MIP reconstruction of CE-MRA data from a 30-year-old woman with thoracic outlet syndrome.
For imaging of the lower limbs, the most commonly used technique is the bolus chase technique. With this, the first step is the production of mask images of all three stations of the leg: aortoiliac region, femoral region and lower legs. Then, during constant injection of contrast, the contrast bolus is followed throughout the entire leg using a moving table. Imaging of the tibial vessels may be compromised by venous contamination. Steno-occlusive disease in the distal aorta is readily seen as in Leriche’s syndrome and CE-MRA is also useful in the surveillance of extra-anatomical bypass grafts (Figure 8.8).