Macular Telangiectasia
Clinical Features:
Type 1 MacTel is typically unilateral and features aneurysmal dilatations of capillaries within the macula. Surrounding exudates are common (Fig. 11.2.1). Type 2 MacTel is typically bilateral and features a loss of the temporal juxtafoveal retinal transparency followed by the development of ectatic capillaries in this region (Fig. 11.2.2). Over time, RPE hyperplasia and pigment deposition may occur along with crystal deposits (Fig. 11.2.3).
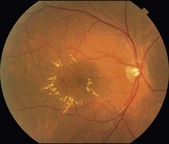
Figure 11.2.1 Color photograph of MacTel type 1 shows numerous aneurysmal abnormalities of varying size within the temporal macula. There is associated retinal thickening and surrounding hard exudate. The fellow macula was normal in appearance.
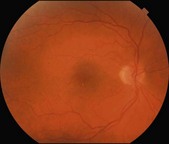
Figure 11.2.2 Color photograph of MacTel type 2 shows loss of the foveal reflex with subtle microaneurysmal abnormalities in the temporal parafoveal region. Fine, crystalline deposits in the same region are barely discernable, but could be seen clinically. Similar findings were seen in the fellow eye.
OCT Features
▶ MacTel type 1: there is cystoid intraretinal edema similar in appearance to cystoid macular edema from other etiologies (Fig. 11.2.4).
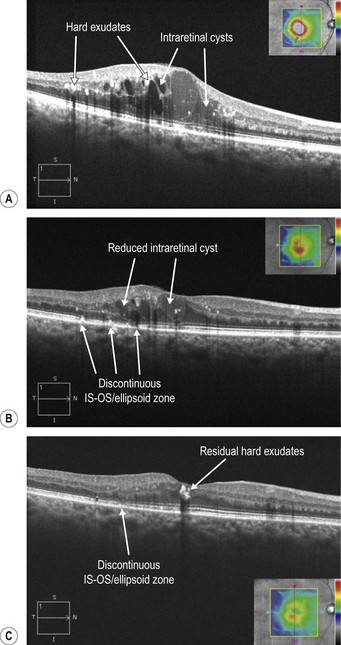
Figure 11.2.4 (A) OCT (corresponding to Figure 11.2.1) in MacTel type 1 shows numerous intraretinal cystic cavities of low and medium reflectivity and small hyperreflective deposits within the retina, corresponding to hard exudates. (B) OCT four months following treatment with focal grid laser shows a significant reduction in the cystoid macular edema and hard exudates. There are multiple discontinuous areas in the IS–OS/ellipsoid zone (arrowheads), which represent laser scars. (C) OCT two and a half years following focal laser treatment (no additional treatment was performed) shows resolution of cystoid macular edema with a small amount of residual exudate. The laser scars have faded (arrowhead).
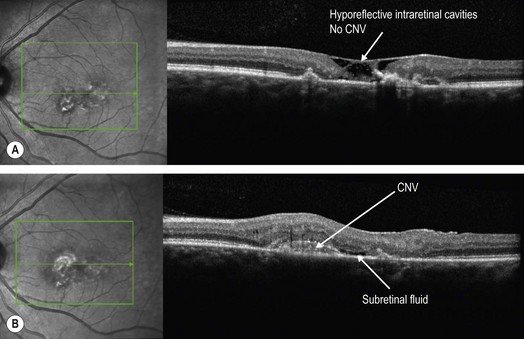
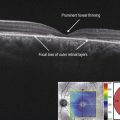
▶ MacTel type 2: there are lamellar defects within various layers of the retina, characteristically involving the region just temporal to the fovea, which are seen on OCT as irregular, hyporeflective cavities (Fig. 11.2.5). These hyporeflective cavities can have varying appearances (Fig. 11.2.6), though the region temporal to the fovea rather than nasal is more involved. With chronic disease, pigment deposition and atrophy may develop (Fig. 11.2.7). Rarely, a secondary CNV can also occur (Fig. 11.2.8).
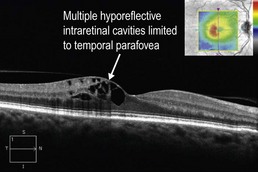
Figure 11.2.5 OCT (corresponding to Figure 11.2.2) in MacTel type 2 shows numerous hyporeflective cavities throughout multiple retinal layers, but limited to the temporal parafoveal region.
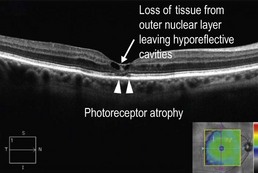
Figure 11.2.6 OCT in MacTel type 2 shows loss of tissue from the outer nuclear layer within the fovea, leaving hyporeflective cystic cavities, more prominent temporally. There is also underlying photoreceptor atrophy (arrowhead).
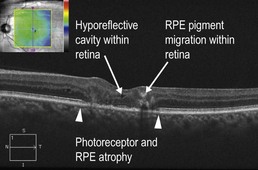
Figure 11.2.7 OCT (corresponding to Figure 11.2.3) in MacTel type 2 shows significant photoreceptor and retinal pigment epithelium (RPE) atrophy (between arrowheads). There is pigment migration from the RPE within the layers of the retina. A small hyporeflective cavity is present within the fovea. The crystalline deposits are not clearly seen.
Ancillary Testing:
Fluorescein angiography can be helpful in both types of MacTel. In MacTel type 1, there are aneurysms of varying size and distribution associated with an abnormal capillary plexus or areas of non-perfusion (Fig. 11.2.9). In MacTel type 2, there are prominent telangiectatic capillaries in the temporal parafoveal region, which leak (Fig. 11.2.10). The cystic changes seen on OCT do not have corresponding leakage on FA. The FA changes may come before or after OCT evidence of the disease is present.
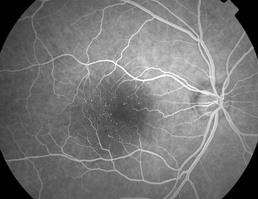
Figure 11.2.9 FA (corresponding to Figure 11.2.1) shows numerous hyper-fluorescent aneurysmal capillary dilatations within an abnormal capillary network, most prominent in the temporal parafoveal region.
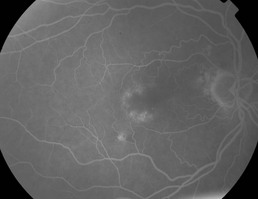
Figure 11.2.10 Fluorescein angiography (corresponding to Figure 11.2.2) shows an enlarged foveal avascular zone bordered by leaking capillary abnormalities in the temporal parafoveal region.