M
M cell See cell, ganglion; cell, M.
M Units See acuity, near visual.
MacAdam ellipses See ellipses, MacAdam.
Mach bands When a light area is separated from a dark area by a transition zone in which the brightness increases or decreases regularly and rapidly, two bands are seen: one light band next to the dark area and another dark band next to the light area. The appearance of these two bands, known as Mach bands, is attributed to lateral inhibition processes occurring in the retina. The phenomenon is usually demonstrated with a rotating disc with black and white areas separated by a zone of brightness gradient. Syn. Mach rings.
macrocornea See keratoglobus.
macropsia Anomaly of visual perception in which objects appear larger than they actually are. It may occur as a result of abnormal accommodation (less than required for the fixation distance) or because of various retinal anomalies in which the visual receptors are crowded together, or because of the recent wear of either base-in prisms or a presbyopic correction, etc. Syn. megalopsia.
See dysmegalopsia; micropsia; metamorphopsia.
macula See fovea centralis; macula lutea.
macula, ectopia of the Anomaly characterized by displacement of the macula, which can be either of acquired or congenital origin. It may follow some forms of retinal scarring, retinal detachment surgery, previous inflammation, etc. It may result in reduced acuity, metamorphopsia or strabismus. Syn. dystopia of the macula; heterotopia macula.
macula, false The retinal area of the deviating eye of a strabismic subject which corresponds to the fovea of the fixating eye.
See retinal correspondence, abnormal.
macula lutea An oval area of the retina 3–5 mm in diameter, with the foveal depression at its centre, slightly below the level of the optic disc and temporal to it (its centre lies 3.5 mm from the edge of the disc). The side wall of the depression slopes gradually towards the centre where the fovea centralis is located and where the best photopic visual acuity is obtained. Around the fovea, the ganglion cells are much more numerous than elsewhere, being arranged in five to seven layers. The outer molecular layer is also thicker than elsewhere and forms the outer fibre layer of Henle and there is a progressive disappearance of rods so that at the foveola only cones are found. The area of the macula lutea is impregnated by a yellow pigment (macular pigment) in the inner layers and for that reason is often called the yellow spot. Syn. area centralis (although that area is considered to be slightly larger, about 5.5 mm in diameter); punctum luteum.
See entoptoscope, blue field; fovea centralis; pigment, macular.
macula, sparing of the See macular sparing.
macular cyst A swelling in the macular area in which fluid has accumulated after injury to the eye or cystoid macular oedema. It may eventually burst into the vitreous producing a macular hole.
macular degeneration, age-related (ARMD, AMD) A common, chronic degenerative condition found in a large percentage of elderly patients (and sometimes middle-aged ones) characterized by loss of central vision. There are two main forms of the condition: non-neovascular (dry, atrophic) AMD, which is the most common, and exudative (wet, neovascular) AMD in which the loss of vision is the most severe. The main features of dry AMD are the presence in the macular region of small, yellowish-white spots (hard drusen) and large, poorly defined, coalescing soft drusen, focal hyperpigmentation of the retinal pigment epithelium (RPE) and at a later stage geographic atrophy of the RPE and depigmentation exposing choroidal vessels. Visual acuity becomes markedly reduced, there is metamorphopsia and the condition usually becomes bilateral over several years. The condition is managed essentially by the use of low vision aids.
Exudative AMD has a similar clinical picture initially but is followed by choroidal neovascularization (CNV), which gives rise to subretinal fluid, haemorrhages, exudation, RPE detachment and subretinal fibrosis in the macular region resulting in severe loss of central vision. If detected early (usually with an Amsler chart), treatment with laser photocoagulation will reduce the risk of further visual loss. Photodynamic therapy (PDT) is another method of reducing the risk of visual loss. It allows selective destruction of the choroidal neovascularization with minimal damage to the overlying retinal tissue. It consists of injecting a photosensitizing agent (e.g. verteporfin) that is taken up by the abnormal vessels and when activated by a laser light of a given wavelength (e.g. 689 nm) it damages and shrivels up the vessels. Recent drug therapies, such as the anti-VEGF ranibizumab and bevacizumab, which are injected intravitreally at regular intervals and designed to stop the leakage and the growth of blood vessels, not only reduce loss of vision but improve visual acuity in a significant percentage of cases of wet AMD. Syn. senile macular degeneration.
See angiography, fluorescein; disciform scar; drusen; dystrophy, macular; lipofuscin; maculopathy, age-related; oxidative stress; pigment, macular; rule, Kollner’s; test, photostress; VEGF.
macular epiretinal membrane See fibrosis, preretinal macular.
macular hole A condition in which there is a partial or full thickness absence of the retina in the macular area. It may occur as a result of trauma, degeneration, old age, preretinal macular fibrosis or pathological myopia. It appears ophthalmoscopically as a round or oval, well defined, reddish spot at the macula. There is metamorphopsia, loss of visual acuity and a central scotoma. An operculum of retinal tissue may overlie the hole. The vitreous in front of the hole eventually condenses and separates from the retina. In partial macular hole a layer of photoreceptors may still be attached to the retinal pigment epithelium (lamellar hole), as in cystoid macular oedema. Treatment usually consists of reattaching the retina, if detached, and possibly vitrectomy.
See fibrosis, preretinal macular; ophthalmoscope, confocal scanning laser; retinal break; retinopathy, solar; tomography, optical coherence.
macular oedema See oedema, cystoid macular; retinopathy, background diabetic.
macular pigment See pigment, macular.
macular pucker See fibrosis, preretinal macular.
macular sparing Retention of macular function in spite of losses in the adjacent visual field as, for example, in homonymous hemianopia due to a cortical lesion (e.g. an interference in the blood flow in the middle cerebral artery). This is due to the fact that most cortical lesions are not large enough to affect the whole extensive cortical area representing the macula, thus leaving some of the area unaffected.
See magnification, cortical.
macular star Deposits of hard exudates material, mainly lipids, in Henle’s fibre layer radiating out in a star-like pattern. It can occur in neuroretinitis, hypertensive retinopathy, etc.
maculopathy, age-related A condition in which there are large whitish-yellow soft drusen in the macular area and hyperpigmentation or depigmentation of the retinal pigment epithelium associated with the drusen. Small hard drusen may also be present. It occurs most commonly in individuals over 50 years of age and represents the early stage of age-related macular degeneration. The risk of progression of this condition may be decreased by dietary supplements of vitamin C and E, antioxidants (carotenoids such as lutein and zeaxanthin) and minerals (zinc and cupric acid).
maculopathy, bull’s eye An ocular condition in which degeneration of the retinal pigment epithelium in the macular area causes alternating ring-like light and dark zones of pigmentation, as in a target. It may result from drug toxicity or hereditary conditions (e.g. cone dystrophy, Laurence–Moon–Bardet–Biedl syndrome). The main symptoms are a loss of visual acuity, reduced colour vision and aversion to bright sunlight.
maculopathy, diabetic A pathological disorder of the macula which frequently develops in diabetic patients. It is characterized by oedema, hard exudates, microaneurysms and ischaemia in the macular area. If the oedema is severe visual acuity will be reduced, but a blue-yellow colour vision defect is usually noted before the loss of acuity. Management involves laser photocoagulation.
See retinopathy, background diabetic.
madarosis Loss of, either or both, the eyebrows and the eyelashes. It may occur in blepharitis, in the presence of hair follicle mites, trauma from rubbing, in alopecia, in leprosy, or as a complication of acquired syphilis.
Maddox cross A scale for measuring the angle of heterophoria and heterotropia consisting of one horizontal and one vertical line in the form of a cross with a light source placed at the centre of intersection. The lines are graduated in prism dioptres or degrees and calibrated for use at a given distance (usually 6 metres). Syn. Maddox tangent scale.
Maddox double prism See bi-prism, Fresnel’s; test, double prism.
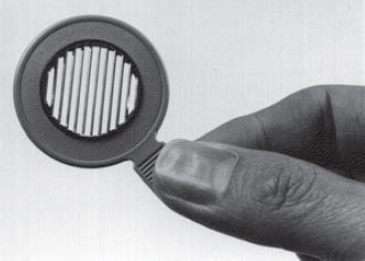
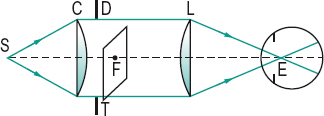
Maddox rod This is not a rod but a series of cylindrical grooves ground usually into a coloured piece of glass and mounted in a rim. (Originally it consisted of a single cylindrical rod.) It is used to measure heterophoria by placing it in front of one eye of a subject viewing a spot of light binocularly. The Maddox rod and eye together form a long streak of light perpendicular to the axis of the grooves and this retinal image is so unlike the image formed in the other eye that the fusion reflex is not stimulated. The eyes will then stay in the passive position. If there is a phoria the streak of light will not intersect the spot of light. For horizontal phorias the rod axis is placed horizontally and for vertical phorias, vertically. The amount and type of the phoria can be quantified by placing a prism of appropriate power and direction in front of either eye such that the streak appears superimposed on the spot of light. Alternatively, the angle of the phoria could be determined using a Maddox cross and placing a rod in front of one eye; the phoria can be read directly by the patient who indicates where the streak of light appears to cross the scale. The Maddox rod is also used to detect or measure cyclophoria (Fig. M1)
See position, passive; test, Maddox rod; test, Thorington.
Maddox wing Handheld device used to measure heterophoria at near. It consists of a septum and two slit apertures, one for each eye. One eye sees a double tangent scale (vertical and horizontal) calibrated to read in prism dioptres, while the other eye sees a white arrow pointing upward and a red arrow pointing horizontally to the left. As the two retinal images are quite different there is no attempt at fusion and the eyes stay in the passive position. The arrows seen by the left eye point to the numbers seen by the right eye. The numbers represent the vertical and horizontal components of the phoria, which can be read directly by the observer (Fig. M2).

magenta 1 . Hue produced by the additive mixture of red and blue. 2. Hue evoked by any combination of wavelengths which act as the complement of a wavelength of 515 nm. See colour, complementary.
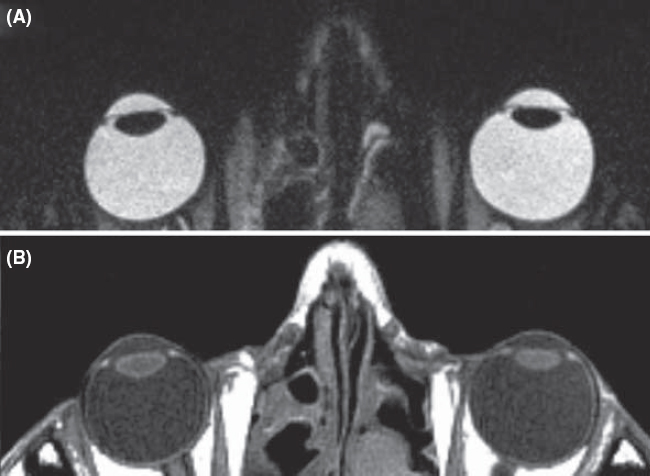
magnetic resonance imaging (MRI) Non-invasive method of imaging part of the body to facilitate diagnosis and therapy. Unlike other radiological methods, this technique does not expose the patient to ionizing radiations. It depends instead on a strong magnetic field which induces the spins of atomic nuclei within the body (e.g. hydrogen atoms) to align themselves along the axis of the magnetic field. When exposed to a pulse of electromagnetic energy at a specific radio frequency, the nuclear spins tilt momentarily then regain their original orientations thus re-emitting an electromagnetic signal at the same radio frequency, which can be detected and analysed to generate a three-dimensional image. The rate at which the radio frequency signal decays can be used to characterize the properties of different tissues, both normal and abnormal. The rates are referred to as T1 and T2 and each yields different contrasts: T1-weighted images are best for anatomical details and T2-weighted images are best for pathological details. This technique provides better image contrast than X-ray computerized tomography in many instances (e.g. the patches of demyelination in the white matter of patients with multiple sclerosis), while the reverse is true in other instances (e.g. a meningioma in the posterior visual pathway). Usage includes the detection of optic nerve disease (e.g. glioma, optic neuropathy), retrobulbar neuritis, lesions in the chiasma and orbital tumours. In general, this procedure takes longer than X-ray computerized tomography (Fig. M3).
functional MRI (fMRI) A non-invasive method used to map the various areas of the cortex, as well as brain tumour mapping, by observing brain activity in response to performing a task that engages a specific behaviour (e.g. tests of colour vision, face perception, motion perception, solving a mathematical problem). This is accomplished, within a conventional MRI scanner, by detecting the change in magnetic susceptibility of blood haemoglobin (and thus blood oxygenation) in various areas of the brain. During task execution when a brain region is active there is an increase in blood flow, which is more oxygenated and has a lower concentration of haemoglobin. This leads to a focal increase in MR image intensity, of around 1–5%, which can be detected using appropriate statistical methods.
See areas, visual association; radiology; tomography, positron emission.
magnification 1. An increase in the apparent size of an object. Syn. enlargement. 2. Specification of a magnifying device to form an enlarged image.
angular m. Magnification expressed as the ratio of the angle α’ subtended at the eye by the image to the angle α subtended at the eye by the object (assuming small angles)
< ?xml:namespace prefix = "mml" />

Syn. angular enlargement. Note: low vision practitioners consider this type of magnification in which no specific distance is specified as a synonym of apparent magnification.
apparent m. Magnification produced by a viewing instrument or lens expressed as the ratio of the angle w’ subtended at the nodal point of the eye by the image, to the angle w subtended at the nodal point by the object, when placed at a standard (reference) distance called the least distance of distinct vision’ from the unaided eye. It is conventional to take this distance as 250 mm and to place the object in the anterior focal plane of the magnifying device. The magnification M is, then, equal to (assuming small angles)
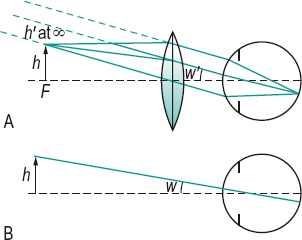
where f and F are the second focal length (in mm) and power (in dioptres) of the magnifying device, respectively (Fig. M4). In this object location the magnification (and therefore the retinal image size) is constant and independent of the distance between the magnifier and the eye, but the field of view decreases as the distance between the eye and the magnifier increases. Syn. conventional magnification; effective magnification; loupe magnification; nominal magnification; relative magnification; standard magnification.
If the object is closer to the magnifying device than its anterior focal plane so that its image is formed at the least distance of distinct vision (25 cm), and assuming that the eye is so close to the magnifier as to ignore the distance separating them and that the patient has an accommodation (or a near addition) of +4.00 D, the magnification M is, then, equal to
Example: a lens of +16.00 D provides, in these conditions, a magnification of 5×. Syn. iso-accommodative magnification; magnifying power; trade magnification.
See magnification, iso-accommodative; magnification, lateral; power, equivalent viewing.
axial m. The ratio of the distance along the optical axis between two points in image space l’ to the distance along the optical axis between the corresponding two points in object space l, i.e. l’/l. The axial magnification is approximately equal to the square of the lateral magnification when the object is far away from the optical system. This magnification is useful when considering an image in its three dimensions. Clinically, it is important when assessing the thickness of a retinal lesion in indirect ophthalmoscopy. Syn. longitudinal magnification.
Table M1
Apparent magnification (or conventional magnification) of microscopic lenses of various powers used in the correction of low vision and their corresponding reading distance (assuming emmetropia or correction for distance and that no accommodation is exerted)
| magnification | lens power (D) | reading distance (cm) |
| 1× | +4.00 | 25 |
| 1.5× | +6.00 | 16.7 |
| 2× | +8.00 | 12.5 |
| 2.5× | + 10.00 | 10 |
| 3× | + 12.00 | 8.3 |
| 4× | + 16.00 | 6.25 |
| 5× | +20.00 | 5 |
| 6× | +24.00 | 4.2 |
| 8× | +32.00 | 3.12 |
| 10× | +40.00 | 2.5 |
combined m. The product of the individual values of each type of magnification used in combination with each other. Example: if a patient uses a CCTV monitor to provide a magnification of 5× viewed at a distance of 50 cm, and then views the same screen at a distance of 25 cm, thus producing a relative distance magnification of 50/25 = 2×, the total magnification is 5 x 2 = 10×. Syn. total magnification.
conventional m. See magnification, apparent.
cortical m. Term referring to the fact that the amount of cortical area devoted to processing visual information from the central area of the retina far exceeds the amount devoted to the peripheral retina. It is estimated that about 25% of the cells in the visual cortex are devoted to processing the central 2.5° of the visual field. Syn. magnification factor.
See area, visual; macular sparing.
distance m. See magnification, relative distance.
effective m. See magnification, apparent.
electronic m. Magnification obtained using an electronic vision enhancement system (EVES), such as a closed-circuit television (CCTV). It is equal to the ratio of the size of the image on the screen to the size of the original object being viewed. Example: an object 2cm in height measures 6 cm on the screen, the magnification is 6/2 = 3×. Syn. real image magnification; transverse magnification.
m. factor See magnification, cortical.
iso-accommodative m. The magnification of a lens (or lens system) when the distance of the image from the eye (or spectacle plane) formed by a magnifier is equal to the distance of the object from the eye viewed without the magnifier. Thus the same amount of accommodation (or near addition) is required with or without the magnifier. It is equal to
where F is the power of the magnifier (assumed to be so close to the eye as to ignore the distance separating them) and D the object vergence. The special case in which the object distance from the eye is 25 cm (D = 4.00 D) is the trade magnification.
See magnification, apparent.
lateral m. Magnification of a lens or of an optical system, expressed as the ratio the size of the image h’ to the size of the object h. It is usually denoted by
Table M2
Approximate lateral magnification (in %) corresponding to various changes in spectacle lens distance and for various lens powers
| distance change | lens power (D) | |||||
| 1 | 2 | 4 | 6 | 8 | 10 | |
| 1 mm | 0.1 | 0.2 | 0.4 | 0.6 | 0.8 | 1.0 |
| 2 mm | 0.2 | 0.4 | 0.8 | 1.2 | 1.6 | 2.0 |
| 3 mm | 0.3 | 0.6 | 1.2 | 1.8 | 2.4 | 3.0 |
| 4 mm | 0.4 | 0.8 | 1.6 | 2.4 | 3.2 | 4.0 |
| 5 mm | 0.5 | 1.0 | 2.0 | 3.0 | 4.0 | 5.0 |
| 10 mm | 1.0 | 2.0 | 4.0 | 6.0 | 8.0 | 10.0 |
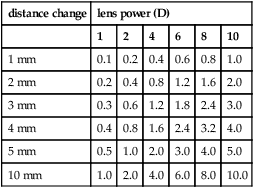
minus lens: if moved closer to the eye magnification increases; if moved further from the eye, magnification decreases plus lens: if moved closer to the eye magnification decreases; if moved further from the eye, magnification increases
where l’ and l are the distances of the image and object, respectively from the principal plane of the lens (or lens system) and L and L’ the object and image vergences, respectively. Syn. enlargement ratio (ER); linear magnification; transverse magnification.
(Note: some authors consider this last term a synonym of electronic magnification.)
See power, equivalent viewing.
linear m. See magnification, lateral.
longitudinal m. See magnification, axial.
loupe m. See magnification, apparent.
negative m. See minification.
nominal m. See magnification, apparent.
m. power See magnification, spectacle.
real image m. See magnification, electronic.
relative m. See magnification, apparent.
relative distance m. The magnification that results from decreasing the distance between an object and the eye. It is expressed as

where x and x’ are the initial distance and the new distance, respectively. Example: if the viewing distance is decreased from 60 cm to 20 cm, Md = 60/20 = 3×. Syn. distance magnification; relative distance enlargement.
relative size m. The magnification which results from increasing the actual size of an object viewed. Examples: a larger TV screen; a larger print book than one used previously. It is expressed as
Ms = h2/h1
where h2 and h1 are the sizes of the enlarged object and the initial object, respectively. Syn. size magnification; relative size enlargement.
relative spectacle m. (RSM) The ratio of the retinal image size in the corrected ametropic eye to that in a standard emmetropic eye.
shape m. Magnification resulting from a variation in the curvature of the front surface and thickness of an ophthalmic lens. In the treatment of aniseikonia it may be necessary to alter the magnification of a lens while leaving its dioptric power unchanged. Syn. shape factor.
See lens, aniseikonic; magnification, spectacle.
size m. See magnification, relative size.
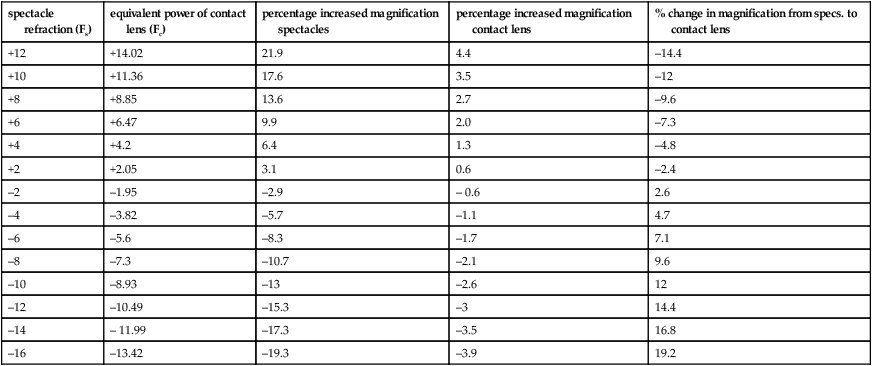
spectacle m. The ratio of the retinal image of a distant object in the corrected ametropic eye to the blurred or sharp image formed in the same eye when uncorrected. It is greater than unity in the hyperopic eye, and less than unity in myopia. With a contact lens, though, this magnification is nearly equal to unity whatever the refractive error. Spectacle magnification SM depends both on the shape of the spectacle lens (i.e. the power of its front surface and its thickness) and on the power of the lens. Thus
where F1 is the power of the front surface, F’v the back vertex power of the lens, t its thickness, n the index of refraction and d the distance from the back surface of the lens to the entrance pupil of the eye. The first term in the formula represents the shape factor (shape magnification) and the second term the power factor (power magnification). However, since the shape factor is very small for most common ophthalmic lenses (except for high plus lenses), it is often ignored in the above formula.
telescopic m. Magnification obtained with a telescope, such as a galilean telescope which gives an erect image or an astronomical telescope in which an erecting system is used. The magnification is
Table M3
Approximate spectacle magnification of lenses of various back vertex powers (F’v in D) assuming d = 15 mm and the parameters of a typical spectacle lens of that power
| F’v | shape factor (S) | power factor (P) | spectacle magnification (SM) | percentage magnification | ||
| +12 | 1.08 | 1.22 | 1.32 | 32% increase | ||
| +10 | 1.06 | 1.18 | 1.25 | 25% ” | ||
| +8 | 1.04 | 1.14 | 1.18 | 18% ” | ||
| +6 | 1.03 | 1.10 | 1.13 | 13% ” | ||
| +4 | 1.02 | 1.06 | 1.09 | 9% ” | ||
| +2 | 1.01 | 1.03 | 1.04 | 4% ” | ||
| 0 | 1.01 | 1.00 | 1.01 | 1% ” | ||
| –2 | 1.00 | 0.97 | 0.97 | 3% decrease | ||
| –4 | 1.00 | 0.94 | 0.94 | 6% ” | ||
| –6 | 1.00 | 0.92 | 0.92 | 8% ” | ||
| –8 | 1.00 | 0.89 | 0.89 | 11% ” | ||
| –10 | 1.00 | 0.87 | 0.87 | 13% ” | ||
| –12 | 1.00 | 0.85 | 0.85 | 15% ” | ||
| –14 | 1.00 | 0.83 | 0.83 | 17% ” | ||
| –16 | 1.00 | 0.81 | 0.81 | 19% ” | ||
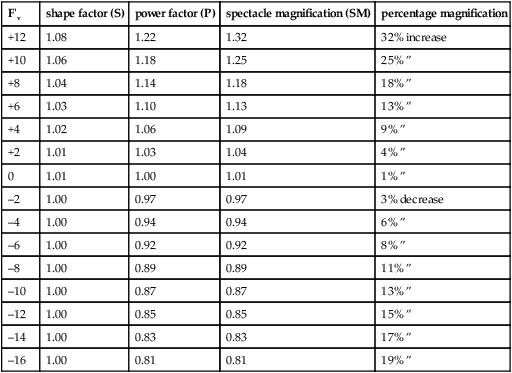
Table M4
Approximate spectacle and contact lens magnification assuming d = 15 mm (vertex distance 12 mm plus 3 mm between cornea and entrance pupil) and negligible lens thickness. The percentage change in magnification going from spectacles to contact lenses was calculated using (Fs/Fc – 1) × 100
| spectacle refraction (Fs) | equivalent power of contact lens (Fc) | percentage increased magnification spectacles | percentage increased magnification contact lens | % change in magnification from specs. to contact lens |
| +12 | +14.02 | 21.9 | 4.4 | –14.4 |
| +10 | +11.36 | 17.6 | 3.5 | –12 |
| +8 | +8.85 | 13.6 | 2.7 | –9.6 |
| +6 | +6.47 | 9.9 | 2.0 | –7.3 |
| +4 | +4.2 | 6.4 | 1.3 | –4.8 |
| +2 | +2.05 | 3.1 | 0.6 | –2.4 |
| –2 | –1.95 | –2.9 | – 0.6 | 2.6 |
| –4 | –3.82 | –5.7 | –1.1 | 4.7 |
| –6 | –5.6 | –8.3 | –1.7 | 7.1 |
| –8 | –7.3 | –10.7 | –2.1 | 9.6 |
| –10 | –8.93 | –13 | –2.6 | 12 |
| –12 | –10.49 | –15.3 | –3 | 14.4 |
| –14 | – 11.99 | –17.3 | –3.5 | 16.8 |
| –16 | –13.42 | –19.3 | –3.9 | 19.2 |
where α’ and α are the angles subtended at the eye by the image viewed through the telescope and the angle subtended at the eye by the object, respectively and Fe and Fo are the powers of the eyepiece and objective, respectively. Telescopes are used to magnify objects at distance (afocal) and placed over the spectacle correction. If the patient is uncorrected the telescope can be adjusted but the magnification will change.
They can be used for near and intermediate viewing by altering the distance between the objective and the eyepiece, or adding a plus lens in front of the objective, the result being a combined magnification (afocal telescope magnification x power of the plus lens ÷ 4).
total m. See magnification, combined.
trade m. See magnification, apparent.
transverse m. See magnification, electronic; magnification, linear.

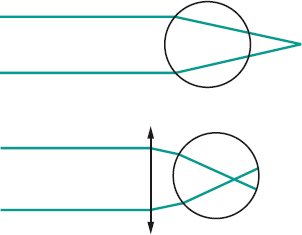
magnifier An optical device, commonly used for close viewing, which produces an apparent magnification. It can be monocular or binocular, held in the hand (hand magnifier) or mounted in front of the eye (stand magnifier). It rarely exceeds a magnification of ×10 and does not produce an inversion of the image (Fig. M5). Syn. loupe.
See distance of distinct vision; lens, magnifying; magnification, apparent; vision, low.
magnifying glass; lens See lens, magnifying.
magnifying power See magnification, apparent.
magnifying spectacles See spectacles, magnifying.
magnitude estimation A psychophysical method of evaluating stimuli above threshold. The subject assigns numbers according to the apparent magnitudes of the stimuli. The results relating the magnitude of sensation S and the stimulus intensity I usually follow a power law (or Stevens’ power law), that is S = k/n where k is a constant and n the exponent which depends on the sensory modality. Example: the magnitude perceived brightness of a 5 degrees target viewed by a dark adapted subject follows the relation S = k/0.33, that is, the intensity of the light target needs to be increased some tenfold to see it twice as bright. Syn. direct scaling.
magno cells See cell, ganglion; geniculate bodies, lateral.
magnocellular layer See geniculate bodies, lateral.
magnocellular visual system See system, magnocellular visual.
Maier, sinus of See lacrimal apparatus.
major arterial circle of the iris See arterial circle of the iris, major.
malar bone See orbit.
malingering Feigning illness or disability (often for the purpose of gaining compensation or avoiding duty).
See test, optokinetic nystagmus; vision, tunnel.
Mallett fixation disparity unit Instrument used to measure the associated heterophoria (or compensating prism). It consists of a small central fixation letter X surrounded by two letters O, one on each side of X, the three letters being seen binocularly, and two coloured polarized vertical bars in line with the centre of the X which are seen by each eye separately. The instrument can be swung through 90° to measure any vertical fixation disparity. The associated phoria is indicated by the misalignment of the two polarized bars when the subject fixates the X through cross-polarized filters in front of the eyes. The amount of associated phoria is given by the value of the base-in or base-out prism power necessary to produce alignment. The unit can also be used to detect suppression.
See Disparometer; heterophoria, associated; heterophoria, uncompensated.
malprojection See projection, false.
Mandelbaum effect See effect, Mandelbaum.
mandibulofacial dysostosis See syndrome, Treacher Collins.
mannitol See hyperosmotic agent.
manometer An instrument for measuring the pressure of gases, vapour, blood or the intraocular pressure directly.
See pressure, intraocular; tonometer.
manoptoscope Apparatus for determining the dominant eye. It consists of a hollow truncated cone that subjects hold with the base against their face and over both eyes. Subjects will view a distant object through the hole at the end of the cone, using their dominant eye.
Marcus Gunn phenomenon See phenomenon, jaw-winking.
Marcus Gunn pupil See pupil, Marcus Gunn.
Marfan’s syndrome See syndrome, Marfan’s.
Mariotte’s blind spot See spot, blind.
mask See masking.
masking A term describing any process whereby a detectable stimulus is made difficult or impossible to detect by the presentation of a second stimulus (called the mask). The main stimulus (typically called the target) may appear at the same time as the mask (simultaneous masking); or it may precede the mask (backward masking; example: metacontrast); or it may follow the mask (forward masking; example: paracontrast).
masking, dichoptic The masking of the visual function of one eye by the view presented to the other, as for example in a haploscope.
See dichoptic.
mast cell stabilizers Prophylactic drugs used to treat allergic conjunctivitis, vernal conjunctivitis, giant papillary conjunctivitis, superior limbic keratoconjunctivitis. They act by stabilizing the membranes of mast cells thus preventing the release of histamine. Common agents are sodium cromoglicate (cromolyn sodium), lodoxamide, nedocromil sodium, olopatadine hydrochloride and pemirolast potassium.
See antihistamine; hypersensitivity.
matt surface Surface which reflects light diffusely. Example: a magnesium oxide surface. Syn. diffusing surface.
See diffusion; gloss; reflection, diffuse.
Maurice’s theory See theory, Maurice’s.
Maxwell disc See disc, Maxwell.
maxwellian view Method of observation in which a converging lens forms an image in the plane of the entrance pupil of the observer. If the observer’s eye is focused on the lens, the lens will appear as a disc filled with light of uniform intensity. This optical arrangement makes it possible to choose the point of incidence within the pupil, to minimize the effect of the optical aberrations of the eye and to avoid the effect of pupil size on the amount of light entering the eye (Fig. M6).
maxwellian view system, clinical Instrument designed to measure visual acuity by using a narrow beam or beams of light focused within the entrance pupil of the eye. The location of the beam or beams within the pupil can be controlled by the clinician. Such an instrument is valuable to assess acuity when part of the pupil is obstructed by a cataract or other opacity as the beam or beams of light can be directed to enter the eye through an area of the pupil where there is no opacity, thus providing an estimate of the visual acuity unaffected by optical image degradation. The results can contribute to the decision as to whether removal of a cataract will be beneficial. There are several types of these instruments. The Potential Acuity Meter (PAM) focuses a single beam of light in the pupil and a letter chart onto the retina. Others focus two beams of light in the pupil and a grating which can be produced on the retina by interference (if the two sources are coherent). This method is called laser interferometry. Examples of these are the Lotmar Visometer and the IRAS Randwal Interferometer, which are referred to as clinical interferometers. They tend to penetrate dense cataracts better than the PAM.
See coherent sources; entoptoscope, blue field; hyperacuity; interferometer.
Maxwell’s spot See spot, Maxwell’s.
McCollough effect See effect, McCollough.
Meares–Irlen syndrome See syndrome, Meares–Irlen.
media, ocular The transparent substances of the eye, i.e. the cornea, the aqueous humour, the crystalline lens and the vitreous humour.
medial Relating to the middle; nearer the median plane.
medial rectus muscle See muscle, medial rectus.
median line; plane See under the nouns.
medium, optical Any material, substance or space through which light can be transmitted.
medullated nerve fibres See fibres, myelinated nerve.
Meesmann’s dystrophy See dystrophy, Meesmann’s.
megalocornea A non-progressive enlargement of the cornea (more than 13 mm in diameter) without significant change in corneal thickness and normal clarity and function. Intraocular pressure is normal and high myopia and astigmatism often occur. It is usually transmitted as an X-linked recessive trait. Some systemic associations include Marfan’s syndrome, Apert’s syndrome, Down’s syndrome, Weil–Marchesani syndrome and osteogenesis imperfecta.
See cornea plana; keratoglobus; microcornea.
megalophthalmos A congenital condition in which the eye is abnormally large, particularly the structures of the anterior segment. The condition is associated with megalocornea, Marfan’s syndrome and Apert’s syndrome.
megalopsia See macropsia.
meibometry A method for quantifying the amount of lipids present in the tears. It may be used to facilitate the diagnosis of meibomian gland dysfunction.
See glands, meibomian.
meibomian cyst See chalazion.
meibomian gland dysfunction; glands
See glands, meibomian.
meibomianitis Inflammation of the meibomian glands. It is believed not to be a primary bacterial disease. It is characterized by the presence of a white, frothy secretion or ‘foam’ on the eyelid margin. The posterior lid margin is hyperaemic and the meibomian gland orifices are obstructed. Meibomianitis is often associated with blepharitis and conjunctivitis. Symptoms include mild itching of the lids and occasionally blurred vision due to the oily secretion spreading over the cornea. This condition may also result from hard contact lens wear. Management of this disease consists of tarsal massage and removal of the secretion with a moist cotton-tipped applicator and antibiotic medication (e.g. tetracycline, erythromycin). Syn. meibomitis. See blepharitis, marginal; blepharitis, posterior; glands, meibomian; hordeolum, internal.
meibomitis See meibomianitis.
melanin Dark brown to black pigment normally present in the skin, the hair, the choroid, the iris, the retina, the ciliary body, the cardiac tissue, the pia mater and the substantia nigra of the brain. It is absent in albinos.
See albinism; fuscin; melanocyte; melanosis; naevus, choroidal; retinal pigment epithelium.
melanocyte A pigment-bearing cell. It is found in the iris, the choroid, the retina, the sclera, the skin, etc.
See melanin; naevus, choroidal; naevus, iris.
melanocytoma A benign, usually bilateral, pigmented tumour which is most commonly found in the optic disc arising from dendritic uveal melanocytes in the lamina cribrosa of the optic nerve head but may occur anywhere throughout the uveal tract. The patient’s visual field presents an enlarged blind spot. The condition is more frequent in dark skinned people.
melanocytosis, ocular A congenital, usually unilateral lesion, characterized by slate grey areas of increased pigmentation. The pigment is curiously not found in the conjunctival epithelium, but is located in the uvea, sclera and episcleral tissues. It may predispose the individual to uveal melanoma. Syn. congenital melanosis oculi.
See naevus of Ota.
melanoma Tumour derived from cells that are capable of forming melanin.
choroidal m. The most common primary malignant tumour in the eye in adults. It appears under ophthalmoscopic examination as a pigmented, elevated mass, usually brown in colour and sometimes with orange pigment (lipofuscin). The tumour may cause a decrease in vision or brief ‘balls of light’ moving cross the visual field, or be asymptomatic, depending on its size or location. The condition is typically unilateral. Differential diagnosis with retinal detachment or choroidal naevus is essential. Treatment may include radiotherapy or photocoagulation, or enucleation if the melanoma is large and vision irreversibly lost. Syn. malignant melanoma of the choroid.
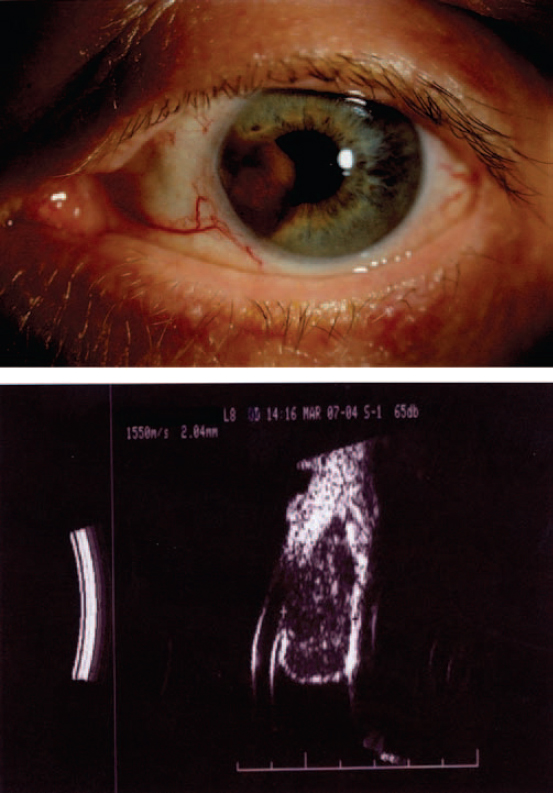
iris m. A pigmented lesion, which is easily seen on the surface of the iris. It alters the colour of the iris and may distort the shape of the pupil. A dilated episcleral vessel running towards the tumour may be present. There may be a localized cataract where the tumour is in contact with the lens and secondary glaucoma may develop if the tumour has spread to the angle of the anterior chamber. The tumour arises from the iris stroma and is composed of epitheloid or spindle cells, or a mixture of both. It is almost always unilateral and most commonly found in white patients with light irides. It is thought to originate from a previous pigmented naevus. If the tumour is found to enlarge it will usually be excised surgically. (Fig. M7)
uveal m. Tumour which may be located in the choroid, the ciliary body or the iris. Choroidal melanomas make up about 85% of the total, ciliary body about 10% and iris about 5%. Although uveal melanomas can occur at any age, the majority of patients are beyond the age of 40 years. Uveal melanomas can metastasize, especially choroidal melanomas. Diagnosis is best achieved with a B-scan ultrasound examination. The patient must be referred to an ocular oncologist without delay. See ultrasonography.
melanopsin An opsin-like protein, sensitive to light with a peak sensitivity around 480 nm, and found in the very small proportion of retinal ganglion cells which are photosensitive. It is believed to be the visual pigment that synchronizes the circadian cycle to the day-night cycle as well as being involved in the control of pupil size and the release of melatonin. This neural circuit appears to be independent of the conventional retinal phototransduction in the rods and cones.
See reflex, pupil light.
melanosis An abnormal accumulation of melanin pigment in the skin or other tissues. If there is a larger quantity than normal of pigment in the tissues of the eye, the condition is referred to as melanosis bulbi (melanosis oculi) or primary acquired melanosis when on the conjunctival epithelium and limbus. It may extend onto the peripheral cornea. It may be benign or become malignant, in which case nodules appear and excision or cryotherapy is required.
See naevus of Ota.
melanosis bulbi; oculi See melanosis.
melatonin See melanopsin.
membrane A thin layer of tissue which covers a surface, separates cellular structures or organs, or connects adjacent structures.
basement m. of the corneal epithelium A very thin non-cellular layer adjacent to Bowman’s layer and upon which the columnar basal cells of the corneal epithelium are bound by hemidesmosomes.
Bowman’s m. See layer, Bowman’s.
Bruch’s m. Thin (about 1.5 αm), shiny, nonvascular layer of the choroid located on the inner side next to the retinal pigment epithelium. It consists of two contiguous layers; the inner one called the lamina vitrea (or basement membrane of the pigment epithelium) and the outer one called the lamina elastica.
See angioid streaks.
Descemet’s m. Strong, resistant, thin (about 8 αm) layer of the cornea located between the endothelium (from which it is secreted) and the stroma. It is practically the last corneal structure to succumb to disease processes and it can regenerate after injury. Syn. lamina elastica posterior; posterior limiting layer.
See descemetocele; ring, Kayser–Fleischer.
Elschnig’s inner limiting m. A thin layer of astrocytes covering the optic disc. It is in continuity with the inner limiting membrane of the retina. In some cases this layer is thickened in the central part of the disc to form the central meniscus of Kuhnt. It is transparent and not usually visible with the ophthalmoscope.
hyaloid m. This is not really a membrane, but a concentration of cells and fibres enclosing the vitreous body.
intermuscular m. A thin, elastic membrane originating from the muscle sheath of each rectus muscle and connecting it to the neighbouring rectus muscle. The membrane fuses with the capsule of each muscle, as well as with Tenon’s capsule.
nictitating m. A fold of the conjunctival mucous membrane that can be drawn over part or all of the cornea in a winking-like action to clean and lubricate the cornea. It is present in many birds, reptiles, fishes and some mammals and is normally hidden in the inner canthus. Syn. third eyelid.
See plica semilunaris.
m. of the retina, external limiting This layer has the form of a wire netting through which pass the processes of the rods and cones of the retina. It is located between the latter and the outer nuclear layer. It is believed to be formed by the fibres of Mueller.
m. of the retina, internal limiting Glasslike membrane lying between the retina and the vitreous body and forming a boundary for both. For that reason it has sometimes also been considered to be the hyaloid membrane of the vitreous. The feet of the fibres of Mueller are attached to this membrane but do not form it. Syn. internal limiting layer of the retina.
preretinal m. See fibrosis, preretinal macular.
pupillary m. Embryonic mesodermal tissue which is present in the centre of the iris and normally disappears by the eighth fetal month to form the pupil. Some strands of the membrane may remain in adults; this is referred to as a persistent pupillary membrane.
meniscus of Kuhnt See membrane, Elschnig’s inner limiting.
meridional accommodation See accommodation, astigmatic.
meridional amblyopia See amblyopia, meridional.
meridional size lens See lens, aniseikonic.
meshwork, trabecular Meshwork of connective tissue located at the angle of the anterior chamber of the eye and containing endothelium-lined spaces (the intertrabecular spaces) through which passes the aqueous humour to Schlemm’s canal. It is usually divided into two parts: the corneoscleral meshwork which is in contact with the cornea and the sclera and opens into Schlemm’s canal and the uveal meshwork which faces the anterior chamber.
See glaucoma, phacolytic; iris, plateau; ring of Schwalbe, anterior limiting; syndrome, pigment dispersion.
mesoderm One of the three primary germinal layers of an embryo from which the eye is derived. It eventually forms the extraocular muscles and the orbital and ocular vasculature.
See ectoderm.
mesopic vision See vision, mesopic.
metacontrast This is an apparently paradoxical phenomenon because it consists of a reduction in subjective brightness of a flash of light which is caused by a second flash following shortly afterward in an adjacent region of the visual field. The effect depends upon the duration, intensity, surface areas of the two flashes, the retinal area stimulated, and particularly the interval of time between the two flashes. The phenomenon appears most clearly with an interval of about 0.1s and disappears when that interval reaches 0.3–0.4s. Syn. backward masking (this term is used to indicate when the test stimulus and the masking stimulus overlap spatially). A flash of light can also be made to appear slightly less bright when it is preceded by another flash in an adjacent region of the visual field and the interval of time is of the order of 0.05s. This second phenomenon is called paracontrast. Syn. forward masking (this term is used when the test stimulus and the masking stimulus overlap spatially).
See masking.
metal spectacle frame See spectacle frame, metal.
metameric colour See colour, metameric.
metamers See colour, metameric.
metamorphopsia An anomaly of visual perception in which objects appear distorted in shape or of different size or in a different location than the actual object. It may be due to a displacement of the visual receptors as a result of inflammation, tumour or retinal detachment, it can be of central origin (e.g. migraine, drug intoxication, neurosis or brain injury), or it can be induced by recently prescribed myopic correction (e.g. micropsia) or presbyopic correction (e.g. macropsia), etc. Metamorphopsia can be detected with an Amsler chart.
See accommodation, spasm of; dysmegalopsia; macular hole; pelopsia; teleopsia.
metarhodopsin See rhodopsin.
method A systematic procedure or process used for attaining a given objective; for example, doing an examination or an experiment.
See procedure.
Bruckner’s m. An objective method of detecting the presence of strabismus. The examiner illuminates both eyes of the patient simultaneously with an ophthalmoscope from a distance of about 1 metre. Looking through the ophthalmoscope the examiner focuses on the fundus reflexes seen in the two pupils. If one pupil appears brighter it is considered that this eye may be strabismic and perhaps amblyopic. The reason may be due to the fact that this eye will be deviated and optical aberrations will make the pupil area appear brighter and whiter. The examiner may also note the position of the corneal reflexes when carrying out this test. This test is more reliable when patients are wearing their correction. Syn. Bruckner’s test.
See method, Hirschberg’s.
cross-cylinder m. See test for astigmatism, cross-cylinder.
Donders’ m. See method, push-up.
Drysdale’s m. A method that has been applied for the determination of the radius of curvature of hard contact lenses. The principle consists of placing a light source in a modified microscope in focus at the surface of the lens and at the centre of curvature of the surface, the distance between the two being recorded on a dial as the radius of curvature.
See optic zone radius, back; Radiuscope.
duochrome m. See test, duochrome.
fogging m. Method of relaxing accommodation during the subjective measurement of ametropia. This is achieved by placing enough plus lens power (or less minus lens power) in front of an eye to form an image in front of the retina. In this condition, any effort to accommodate will produce a poorer image and relaxation of accommodation is thus achieved (Fig. M8). Then, plus lens power is decreased (or minus lens power increased) until the patient reports no further improvement in visual acuity. This point represents the maximum positive lens power (or minimum negative lens power) and it is called the best vision sphere (BVS).
See refractive error; test, fan and block; test, plus 1. 00 D blur.
von Graefe’s m. See test, diplopia.
van Herick, Shaffer and Schwartz m. A technique for estimating the angle of the anterior chamber. It is based on the fact that the width of the angle of the anterior chamber is correlated to the distance between the posterior corneal surface and the anterior iris as viewed near the corneal limbus. This is done using a slit-lamp with a narrow slit beam perpendicular to the temporal or nasal corneal surface, viewing from the straight-ahead position and comparing the depth of the anterior chamber to the thickness of the cornea. If the AC depth is equal to or greater than the corneal thickness, the angle is considered to be grade 4 (corresponding to a wide open angle). If the AC depth is equal to one-half the corneal thickness, the angle is considered to be grade 3 (this is the most common angle width). If the AC depth is equal to one-fourth the corneal thickness, it is considered to be grade 2, and if the AC depth is less than one-fourth the corneal thickness, it is considered to be grade 1 (corresponding to a very narrow angle). Grade 0 is considered to be a closed angle. The method is most useful for predicting the possibility of angle-closure glaucoma. The results of this method are in good agreement with those of the Shaffer classification using a gonioscope. Syn. van Herick’s technique.
See gonioscopy; test, shadow.
Hirschberg’s m. Method for estimating the objective angle of strabismus. The examiner’s eye is placed directly above a small penlight source fixated by the subject and observes the position of the corneal reflex of the deviating eye. The angle of strabismus can be estimated on the basis that each mm of deviation, relative to the corneal reflex in the fixating eye, represents approximately 7° (12 Δ) of strabismus (Fig. M9). Syn. Hirschberg’s test.
See method, Bruckner’s; method, Krimsky’s.
Humphriss m. Method of binocular subjective refraction in which the eye not being refracted is blurred by means of a +0.75 D (or +1.0 D) spherical lens above the correcting lens. This lens produces a suppression of foveal vision while allowing peripheral fusion to maintain binocular alignment of the two eyes during refinement of the correction to the other eye. Syn. Humphriss immediate contrast test (HIC). However, HIC differs somewhat from the above method because it relates only to one specific procedure: a +0.25 D sphere is followed by a –0.25 D sphere in front of the unfogged eye and the patient has to indicate which is the clearest. The above method can be used for many types of refractive procedures.

See refractive error; test, balancing.
Javal’s m. Method for determining the objective angle of strabismus using a perimeter. The patient is seated before a perimeter arc with the deviating eye at the centre of the arc while the other eye fixates a distant point straight ahead. The examiner moves both a light source and his eye directly above it, until the corneal reflex appears centred in the entrance pupil of the deviating eye. The position of the source on the arc can be read to give the objective angle of strabismus. Angle lambda must be added in convergent and subtracted in divergent strabismus as the criterion used was the pupillary axis, which makes an angle with the line of sight. Strictly speaking, angle kappa, rather than lambda, should be taken into account.
See angle of deviation.
Krimsky’s m. Method used to determine the objective angle of strabismus. The examiner’s own eye is placed directly above a small penlight source fixated by the subject and observes the position of the corneal reflexes. Prisms are placed in front of the deviating eye until the examiner finds the prism power that makes the corneal reflex appear to occupy the same relative position as that in the fixating eye. Syn. prism reflex test.
See method, Hirschberg’s.
minus lens m. Method of measuring the monocular amplitude of accommodation which consists in placing minus lenses in front of one eye while the subject fixates the smallest optotypes (usually subtending about one minute of arc, that is the 6/6 or 20/20 line). Progressively stronger lenses are used until the patient reports that the test appears blurred. The determination of the amplitude must take into account the vergence at the eye of the fixation point and the test must be carried out with the patient’s distance correction. If the minus lens to blur is –4 D and the fixation distance 40 cm, the amplitude will be equal to 6.5 D.
See accommodation, subjective.
preferential looking m. (PL) A method of assessing visual acuity in infants. It consists of presenting two stimuli on a uniform background, one of which contains a pattern (e.g. a checkerboard or a grating) and the other a plain field of equal shape, size and luminance, and observing the infant’s eyes. If the infant can resolve the pattern he or she tends to fixate that stimulus for a larger percentage of time. By reducing the size of the detail in the pattern, a threshold can be obtained when the infant fixates at either stimulus for the same length of time. See acuity, objective visual; acuity cards, Teller; test, Cardiff acuity.
push-out m. See method, push-up.
push-up m. Method of determining the near point of accommodation by moving a test object (made up of small optotypes subtending one minute of arc (that is the 6/6 or 20/20 line) at the eye and uniformly illuminated) closer to the patient’s eye. It is usually done monocularly and then binocularly. The near point is achieved when the small test object yields a sustained blur and not just begins to blur. Alternatively, the card is moved back after appearing blurred until the small test object just appears to clear again. This is often called the push-out method. In older patients, plus lenses may be needed to carry out the test and the power of the lens is subtracted from the reading. The amplitude of accommodation is deduced by taking into account the vergence at the eye of the far point (it is at infinity in emmetropes and corrected ametropes). Syn. Donders’ method.
See accommodation, amplitude of; rule, near point.
Smith’s m. A method of estimating the depth of the anterior chamber. It is performed with a conventional slit-lamp. The angle between the illumination beam and the microscope, which is placed along the straight-ahead position, is set at 60°. To examine the patient’s right eye the examiner looks through the right eyepiece and through the left eyepiece to examine the left eye. A beam of moderate thickness is oriented horizontally and focused on the cornea. Two horizontal images of the slit will appear separated by a dark space one sharply focused corresponding to the cornea and the other out of focus corresponding to the anterior lens surface. The slit is lengthened until the two separate reflections just touch. At this point the length of the slit is measured and multiplied by a factor of 1.4 to arrive at an estimate of the depth of the anterior chamber. The method gives optimum results within the range of 1.4 mm and 3 mm. It is most useful in assessing shallow chambers as this could lead to angle-closure glaucoma.
m. of stabilizing the retinal image See stabilized retinal image.
methotrexate See immunosuppressants.
methylcellulose A highly viscous, watersoluble, non-irritating compound used as a thickening, lubricating and clinging agent in drugs such as artificial tears, wetting and contact lens solutions.
See alacrima; keratoconjunctivitis sicca; tears, artificial.
methyl methacrylate See polymethyl methacrylate.
metipranolol hydrochloride See beta-blocker.
miconazole See antifungal agent.
microaneurysm Tiny swelling in the wall of a blood vessel. It appears in the retinal capillaries as a small, round, red spot. It is commonly found in diabetic retinopathy, retinal vein occlusion or absolute glaucoma.
microbe Any very minute living organism, such as bacteria, protozoa, fungi or viruses.
microcoria Abnormally small pupils, usually congenital and due to an absence of the dilator pupillae muscle.
microcornea An abnormally small cornea with a horizontal diameter of less than 10 mm. The condition is usually inherited, either as an autosomal dominant or autosomal recessive trait. It may be accompanied by hyperopia and glaucoma.
See cornea plana; megalocornea.
microcysts, epithelial Very small, round vesicles containing fluid and cellular debris observed on the surface of the cornea under slit-lamp examination in some types of corneal dystrophy and in wearers of extended wear contact lenses, due to chronic hypoxia. They appear to originate in the basal layer of the corneal epithelium as a result of cellular necrosis. They can be seen by slit-lamp examination using a magnification of at least ×20. If caused by extended wear contact lenses, the patient should be advised to change to daily wear contact lenses of high oxygen transmissibility. Syn. microepithelial cysts.
microfluctuations of accommodation See accommodation, microfluctuations of.
micrometre An SI unit of length equal to one millionth of a metre (10–6 m). Symbol: αm. Syn. micron (obsolete term).
See nanometre.
micron See micrometre.
micronystagmus See movements, fixation.
micropachometer See pachometer.
microphthalmia Congenital anomaly in which the eyeball is abnormally small and often deeply set in a small orbit. It is typically hyperopic. Syn. microphthalmos; microphthalmus. When there is no other abnormality (e.g. coloboma of the iris, microphthalmos with cyst), the condition is called nanophthalmos (Fig. M10).
See anophthalmia; monophthalmia; pseudoptosis.

micropsia Anomaly of visual perception in which objects appear smaller than they actually are. It may be due to a retinal disease in which the visual cells are spread apart, or to paresis of accommodation or to uncorrected presbyopia, or to the recent wear of either base-out prisms or a correction for myopia, etc.
See dysmegalopsia; macropsia; metamorphopsia.
microsaccades See movements, fixation.
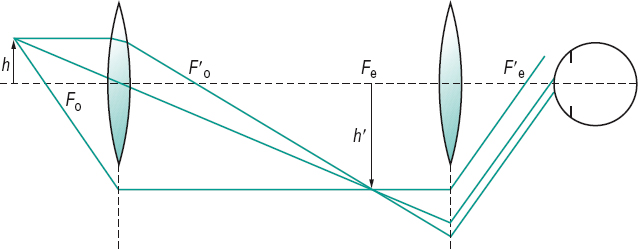
microscope An optical instrument for magnifying small near objects. It can consist of a single converging lens such as a loupe (simple microscope) or of two or more lenses or lens systems (compound microscope) (Fig. M11). In this latter case, one lens or lens system serves as an objective to form real and magnified images of the object while the other lens or lens system serves as an eyepiece to examine the aerial image formed by the objective. The final image is inverted with respect to the object. It can use light or a beam of electrons (electron microscope) which produces magnification some 50 to 100 times greater than with light. The magnification, M, of a light microscope, adjusted for a final image at infinity, is equal to
M = Mo × Me
where Mo is the lateral magnification of the objective, and Me the angular magnification of the eyepiece.
See eyepiece; lens, immersion; objective; stage.
confocal m. A microscope that provides viewing of cells, organisms (such as bacteria or fungi) and other structures within various tissues, in living patients. It allows each layer of a tissue to be viewed with much greater clarity than with a conventional microscope because signals from the viewed layer and the illumination beam have the same focus, while elements above or below the focal plane are out of focus and usually filtered out. The instrument has been used to investigate and diagnose corneal disease processes, including dystrophies and infectious keratitis, or to follow corneal healing after laser or traditional surgery. In addition, the instrument scans the object of interest by varying the plane of focus to form an image in three dimensions, of higher contrast and resolution than provided by a specular microscope.
See ophthalmoscope, confocal scanning laser.
m. magnification See microscope.
slit-lamp m. Compound microscope used in conjunction with a slit-lamp. It is designed to have a working distance of about 90–125 mm to allow room for the clinician or for placing certain accessories such as a tonometer or pachometer. Slit-lamp microscopes have a magnification that varies usually within the range of ×6 to ×40.
See distance, working; slit-lamp.
specular m. A light microscope utilizing specular reflection to view the component layers of the cornea and particularly to observe and photograph the endothelium. It consists of an objective which is divided longitudinally. Light in the form of a slit beam is directed down one half and is reflected from the cornea-aqueous interface to the other half of the objective to form a visible and photographic image of the endothelium. The microscope is usually fitted with a X 40 water immersion objective which has a working distance of 1.6 mm. The cornea is covered with silicone fluid into which the objective tip is immersed. Good resolution is achieved provided that the width of the slit beam is kept small, to reduce the light scatter from the overlying corneal layers. This microscope allows examination of the corneal endothelium in vitro.
For clinical measurements, the specular microscope is mounted horizontally using an objective with less magnification (usually × 20). The tip of the microscope has a glasswindowed, fluid-filled, screw-on cap, which applanates the cornea over a very small area. The field of view is usually increased by the insertion of a + 10 D into the incident light path before the objective. Photomicrography is accomplished with a flash unit, as otherwise eye movements make photography with long exposure impossible. However, corneal anaesthesia is necessary and clear images of the endothelium are not possible if the cornea is oedematous. For these reasons new systems have been developed which fit on a slit-lamp and facilitate photography. Their magnification is greater than other slit-lamps, being x 40 to x 70, and they do not require contact with the cornea as they have long working distances. Specular microscopy is used to monitor changes in corneal endothelium in contact lens wearers, especially those wearing extended wear lenses.
See distance, working; microscope, confocal; polymegethism, endothelial.
microspherophakia A congenital, usually bilateral, condition in which the crystalline lens is smaller than normal and spherical in shape. It may give rise to lenticular myopia, subluxation or glaucoma. It may occur independently or it may be associated with the Weill–Marchesani syndrome or more rarely with Marfan’s syndrome, Peter’s anomaly or congenital rubella.
microsquint See microtropia.
microstrabismus See microtropia.
microtropia A small-angled (usually less than 6–8 Δ in angle) inconspicuous strabismus which is not usually detected by cover test, either because the deviation is too small or because the angles of abnormal retinal correspondence and eccentric fixation coincide with the angle of deviation. There is usually amblyopia in the deviated eye and there may also be anisometropia. The patient with this condition displays nearly normal binocular vision without symptoms. Management usually consists of correcting the refractive error. Syn. microsquint; microstrabismus; small angle strabismus.
See test, four prism dioptre base out.
middle third technique See criterion, Percival.
midline 1. An imaginary line running along the surface of the brain (anterior to posterior), which separates the right and left hemispheres. 2. See line, median.
migraine An intense and recurring pain usually confined to one side of the head and often accompanied by vertigo, nausea and vomiting, photophobia and scintillating appearances of light and even hemianopia.
See aura, visual; metamorphopsia; scotoma, scintillating.
Mikulicz’s syndrome See syndrome, Mikulicz’s.
Miller–Nadler glare tester See glare tester.
millilambert Non-metric unit of luminance. It is equal to 3.183 cd/m2.
millimicron See nanometer.
miner’s nystagmus See nystagmus.
minification A reduction in the apparent size of an object. Example: viewing a distant object through the objective of a galilean telescope. Syn. negative magnification.
See field, visual expander.
minimum cognoscible The threshold of recognition of shapes or contours.
minimum legible The threshold for the recognition of letters or numbers.
minimum separable Perception of the least distance separating two objects, yet being still distinguished as two.
See resolution, limit of.
minimum visible Perception of the smallest area of light.
minus lens See lens, diverging.
minus lens method See method, minus lens.
miosis Contraction of the pupil or condition in which the pupil is very small (2 mm or less in diameter). It can be brought about by a spasm of the sphincter muscle or by the effect of a miotic drug (e.g. eserine, neostigmine, pilocarpine), or in certain spinal diseases or any stimulation of the parasympathetic supply to the eye. Miosis occurs naturally when doing close work or when stimulated by light. Note: also spelt myosis.
See reflex, corneal; reflex, pupil light; spot, baring of the blind; syndrome, Horner’s.
miotics Drugs that constrict the pupil. They may be used in the treatment of glaucoma and accommodative esotropia and, sometimes, after a mydriatic examination. Miotics are either parasympathomimetic (cholinergicstimulating) drugs which have a direct muscarinic action, such as pilocarpine and carbachol, or anticholinesterase drugs which block the effect of acetylcholinesterase thus letting acetylcholine produce its effect, such as physostigmine, neostigmine, echothiophate and demecarium. There are also some miotics which act by blocking α- or β-adrenergic receptors. For example, dapiprazole and thymoxamine block the α-adrenergic receptors and propranolol blocks the β-adrenergic receptors.
See adrenergic receptors; glaucoma, open-angle; muscle, sphincter pupillae; mydriatic; parasympathomimetic drug.
mire A pattern used in an optical instrument to guide the observer. Examples: the luminous pattern seen in a keratometer; the two halfcircles seen in an applanation tonometer.
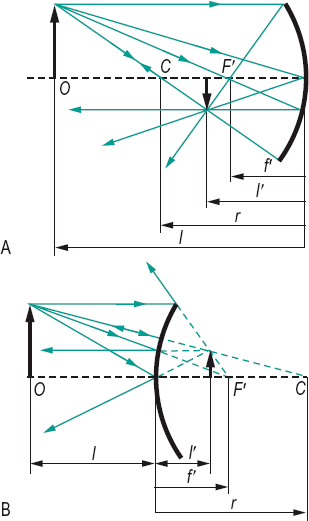
mirror A surface capable of reflecting light rays and forming optical images. Such surfaces are smooth or polished, made of highly polished metal, or a thin film of metal (e.g. aluminium) on glass, quartz or plastic. Object distance l and image distance l’ relate to the focal distance f or the radius of curvature r of the mirror, as follows
2/r represents the refractive power of the mirror, in air. If the medium that contains the incident and reflected rays is n, the power becomes F = 2n/r and the focal length, f = r/2n (Fig. M12).
See length, focal; paraxial equation, fundamental; system, catadioptric.
back surface m. A mirror which reflects from the back surface of a refracting layer, usually glass.
See mirror, front surface.
concave m. A mirror with a spherical concave surface forming an erect, magnified, virtual image when the distance from the mirror is less than the focal distance and an inverted real image when the object distance is greater than the focal distance (Fig. M12).
convex m. A mirror with a spherical convex surface forming a virtual, erect and diminished image (Fig. M12).
front surface m. A mirror that reflects directly from its front surface. The advantages of this type are that, unlike back surface mirrors, there is no chromatic effect as the glass is not used optically, therefore ultraviolet rays can be used which would otherwise be absorbed in the glass and there is no ghost reflection from the front surface. However, these mirrors can be easily scratched and the coating may tarnish. Often a coating of silicon monoxide is evaporated on top of the surface, but this causes a loss of reflectivity.
See image, ghost; mirror, back surface.
plane m. A mirror whose surface is plane and forms a virtual image of the same size as the object. Object and image distances are equal.
semi-silvered m. See beam splitter.
m. writing Writing backward, Latin letters being written from right to left and the details of the letters reversed. The writing thus appears normal when viewed in a mirror. Syn. retrography.
mitochondrial inheritance See inheritance.
mitochondrion An organelle in the cytoplasm of cells, which produces most of the energy-rich molecule adenosine triphosphate (ATP) in cells. It is produced by using oxygen to break down nutrient molecules (e.g. glucose). The number of mitochondria in a cell varies, it is greater in active cells, such as muscle and liver cells which need more ATP. Mitochondria are involved in other processes (e.g. apoptosis, cellular proliferation). Each mitochondrion contains DNA, RNA, ribosomes and granules. The DNA is distinct from that of the cell nucleus. Mitochondrial DNA is inherited only through the female. Mutations in mitochondrial DNA causes genetic disorders (e.g. Leber’s hereditary optic atrophy). Plural: mitochondria.
mitosis Process by which a cell nucleus divides into two nuclei with chromosome numbers and genetic make-up identical to that of the parent cell. Mitosis is inhibited by anaesthetics and thus tissue repair is delayed. It is also slowed by hypoxia. Example: the mitosis of the basal cells of the corneal epithelium; the mitosis of the epithelial cells of the crystalline lens adding new cells to it which eventually form new lens fibres.
See apoptosis; chromosome; corneal abrasion; cycle, Krebs.
Mittendorf’s dot See hyaloid remnant.
mixed astigmatism See astigmatism, mixed.
Mizuo’s phenomenon See phenomenon, Mizuo’s.
Mobius syndrome See syndrome, Mobius.
modality One of the types of sensation (e.g. vision). The term is usually used to specify the sense (e.g. the visual modality, the touch modality).
modulation transfer function See function, modulation transfer.
modulus of elasticity The ratio of a force applied to a material to the increment of change (e.g. increase in length; angular deformation) in that material. Materials with low modulus of elasticity are less resistant to stress, while materials with high modulus of elasticity resist stress and hold their shape better. The SI unit of modulus of elasticity E is the pascal (Pa). Examples: the modulus of elasticity of a PMMA contact lens is about 3000 MPa, it is around 0.4 to 1.5 MPa for silicone hydrogel lenses and 0.3 to 0.5 MPa for hydrogel lenses. Syn. coefficient of elasticity; Young’s modulus of elasticity.
Mohindra’s technique of retinoscopy See retinoscopy, Mohindra’s technique of.
moiré effect See effect, moiré
Moll’s glands See glands of Moll.
molluscum contagiosum A contagious disease of the skin caused by a double-stranded DNA virus of the poxvirus group. It is characterized by small, pinkish, pearly umbilicated nodules and mucoid discharge most commonly on the eyelid margins and brow area, and it may lead to conjunctivitis. It occurs most frequently in children and young adults, especially those with HIV infection. Treatment includes cauterization, cryotherapy or excision.
mondrian A complex visual display used in studies of colour perception. It consists of rectangles of various dimensions with all sides parallel or perpendicular to each other, and each rectangle of a colour or brightness different from the adjacent rectangles.
monoblepsia Condition in which monocular vision is more distinct than binocular vision.
monocentric Pertaining to a lens with only one optical centre. A monocentric bifocal lens is one in which the optical centres of the distance and near portions coincide and jump is eliminated.
monochromasia See achromatopsia.
monochromasy See achromatopsia.
monochromat Person who has a condition of monochromatism (total colour blindness). There are two types of monochromats: the cone monochromat whose photopic luminosity curve resembles the normal and who has normal visual acuity and dark adaptation; and the rod monochromat whose retina does not contain functional cones and, therefore, has poor vision, photophobia and sometimes associated nystagmus and myopia. Monochromats are very rare: estimated at about three persons in 100 000.
See achromatopsia; colour vision, defective; dystrophy, cone.
monochromatic light See light, monochromatic.
monochromatism See achromatism; achromatopsia; colour vision, defective; monochromat.
monochromator A modified spectroscope for producing nearly monochromatic light.
monocle A single ophthalmic lens, with or without a frame, which is worn by holding it between the brow and the cheek.
monocular Pertaining to one eye. Syn. uniocular.
monocular cues to depth perception See perception, depth.
monocular diplopia; vision See under the nouns.
monofixation 1. Monocular fixation. 2. See syndrome, monofixation.
monophthalmia A rare, abnormal development in which one eye is absent. The remaining eye is often microphthalmic. Syn. unilateral anophthalmia.
See anophthalmia; microphthalmia.
monoptic Relating to the presentation of different stimuli to one eye. See dichoptic.
monosomy See chromosome.
monovision Term referring to a method of correcting presbyopia by using a contact lens corrected for distance in one eye (usually the dominant one) and a contact lens corrected for near in the other eye. Binocular vision is impaired with this method, especially stereoscopic vision; however, it has been found to be relatively successful in many cases. It is assumed that at any time one eye is focused while the other is not and the cortical visual system suppresses this latter image (at least the central part of the image). Monovision may also occur without correction in a presbyopic patient who has emmetropia in one eye and myopia in the other eye.
modified m. is a method of achieving monovision using bifocal contact lenses in which the powers, lens fit or other lens parameters are modified to emphasize distance vision for one eye and near vision for the other eye, while still retaining a reasonable level of binocular vision.
moon illusion See illusion, moon.
Mooren’s ulcer See ulcer, Mooren’s.
Morax–Axenfeld, diplobacillus of See conjunctivitis.
morning glory disc See disc, morning glory.
motility test See test, motility.
motion after-effect See after-effect, waterfall.
motion blindness; parallax See under the nouns.
motor cortex See cortex, motor.
motor end-plate See muscles, extraocular.
motor field See field of fixation.
motor fusion See fusion, motor.
motor neuron See neuron.
motor pathway Pathway from the cortex to the muscles that control the movements of the eyes enabling them to act as a unit.
motor unit A group of muscle fibres that respond to a stimulus from a single motor neuron. In the extraocular muscles a motor unit consists of less than a dozen small fibres, that is considered to be a small unit. It produces a finer degree of neural control over contraction than a larger unit, which produces more powerful gross movements when activated. See neuron.
mouches volantes See image, entoptic; muscae volitantes.
mould See impression, eye.
moulding A process for making a lens in which a hot piece of glass (called a parison or gob) or liquid polymer (for contact lenses) is pressed to a predetermined shape. Frames can also be manufactured by pouring a soft material (plastic or molten metal) into a mould which takes on the desired shape after cooling (or drying). The technique is useful for large volume production.
Note: also spelt molding.
See lens, spin-cast contact; surfacing.
mount Device (usually in metal or plastic) which holds the ophthalmic lenses before the eyes in rimless spectacles or in spectacles with rims, but which do not surround the lenses, the latter being held by holes, slots or grooves in their periphery. Syn. mounting.
mounting See mount.
movement 1 . Change or apparent change in position. 2. The act of moving.
m. after-effect See after-effect, waterfall.
against m. 1. Apparent movement of an object seen through a lens in a direction opposite to that in which the lens is moved. This occurs when looking through a plus lens. 2. See retinoscope.
alpha m. A form of apparent movement perceived when different sizes of an object are presented in an alternating sequence with an interstimulus interval of about 60 ms, the object appears to expand and contract.
apparent m. The perception of movement induced by stationary separated objects, when the objects are presented rapidly on and off, one after another with a brief time interval between the two stimuli. The illusion of apparent movement is generally attributed to the stimulation of motion-sensitive neurons in area MT (V5) of the visual cortex. Examples: alpha movement, beta movement, gamma movement, phi movement, stroboscopic movements. Syn. apparent motion.
autokinetic m. See illusion, autokinetic visual.
beta m. A form of apparent movement perceived when two or more separated stationary objects are presented in rapid sequence with an interstimulus interval of between 40 ms and 60 ms, the object appears to move continuously from one position to the other. Beta movement is the basis of smooth, continuous motion perception in cinematography in which frames are commonly presented at a rate of 24 frames per second (or about 42 ms time interval). Syn. optimum movement.
See movements, stroboscopic.
compensatory eye m’s. See reflex, static eye.
conjugate eye m’s. Seeversion.
cyclofusional eye m’s. See cyclofusion.
disjugate eye m’s. See movements, disjunctive.
disjunctive eye m’s. Movements of the two eyes in which the eyes move in opposite directions, as in convergence or divergence. Syn. disconjugate movements; disjugate eye movements.
See vergence.
eye m’s. The act or process of a change in position of the globe of the eye.
See electrooculogram; fusion, motor; reflex, vestibulo-ocular; vergence; version. fixation m’s. Involuntary movements of the eye occurring when actually fixating an object. Three types of movements have been observed: the drifts, the micronystagmus (tremors) and the saccades (or microsaccades). These movements are too subtle to be seen by direct observation. The drifts are characterized by a small amplitude (1–7 minutes of arc) and a low frequency (2–5 Hz). The micronystagmus movements are characterized by a very small amplitude (5–25 seconds of arc) and a higher frequency (30–100 Hz) and the saccadic movements by a small amplitude (1–20 minutes of arc) and low frequency (0.1–1 Hz). Syn. involuntary eye movements; miniature eye movements; physiological nystagmus (Fig. M13).
See movement, saccadic eye; stabilized retinal image.
following m. See movement, pursuit.
fusional m. See fusional movements.
gamma m. A form of apparent movement that is perceived when a single stimulus is presented in an alternating sequence with an interstimulus interval of about 60 ms under high and low illumination, the object appears to expand and contract.
optimum m. See movement, beta.
optokinetic m. See nystagmus.
phi m. Illusion of movement created when one object disappears and an identical object appears in a neighbouring region of the same plane. If the time interval between the two sources is between 0.06 s and 0.2 s, the observer will see an apparent movement of the source, which appears to jump from the first to the second position without the perception of continuity. Hence it is considered as a partial illusion of movement. Some observers also see each source flickering depending on the rate of alternation. The phi phenomenon has been applied to test patients with convergent and divergent strabismus. This is the phi phenomenon test of Verhoeff: two light sources, separated by the angle of strabismus, are placed in front of the patient, as in a major amblyoscope. The two foveas are stimulated with a short time interval between stimulations and patients with normal retinal correspondence do not see a movement whereas those with abnormal retinal correspondence do. Syn. phi phenomenon.
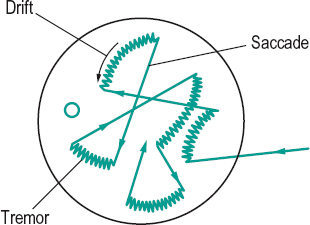
See movements, stroboscopic; retinal correspondence, abnormal; threshold, movement.
pursuit m. Movement of an eye fixating a moving object. The fixation can remain locked on the target as long as the movement is smooth and the velocity below about 40°/s. Abnormal pursuit eye movements could be due to ocular motor nerve palsy, cerebellar disease, internuclear ophthalmoplegia, systemic medication, etc. Syn. following movement.
rapid eye m’s. (REM) Fast eye movements that occur periodically during sleep and are associated with dreaming.
saccadic eye m. A short rapid and abrupt movement of the eye as occurring in reading a line of printed words or in fixating from one point to another. The peak velocity of a saccade of 10° amplitude can exceed 400°/s and be completed in 40 ms. Syn. saccade.
See antisaccade; hypermetria; movements, fixation; reading.
scissors m. 1. Apparent change in the angle between two lines seen through a rotating astigmatic lens. 2. See retinoscope.
stroboscopic m’s. Apparent movements as produced by a stroboscope. If the frequency of stroboscopic illumination is less than the rotation of a moving object it appears to rotate slowly but if the frequency is increased above that of the moving object it appears to rotate slowly in the opposite direction to its real rotation. (If the moving object is rotating at x rotations per second when the frequency is a full multiple of x, one sees the object motionless.) Beta and phi movements are types of stroboscopic movements.
See stroboscope.
m. threshold See threshold, movement.
torsional m. See torsion.
vergence m’s. See movements, disjunctive.
with m. 1. Apparent movement of an object seen through a lens in the same direction as that in which the lens is moved. This occurs when looking through a minus lens. 2. See retinoscope.
moxifloxacin See antibiotic.
moxisylyte (thymoxamine) See alpha-adrenergic antagonist.
mucin Glycoprotein, rich in carbohydrates, produced by the goblet cells and the subsurface vesicles of the conjunctiva which forms the basis of the mucous layer of the precorneal film. Mucin and the secreted glycocalyx (which consists of glycoproteins) are adsorbed by the epithelium of the cornea to convert it from a hydrophobic into a wettable hydrophilic surface. A deficiency in the production of mucin leads to an abnormally short precorneal film break-up time and to desiccation of the ocular surface. In addition, the mucous layer prevents microbial invasion of the cornea. In some contact lens wearers (especially of silicone hydrogel lenses) collapsed mucin, as well as lipids and tear proteins, accumulate behind the lens and form small, discrete spheres (called mucin balls or mucin plugs). These mucin balls cause neither discomfort nor loss of vision.
See film, precorneal; keratoconjunctivitis sicca; test, break-up time; xerophthalmia.
mucocele An abnormal enlargement of a cavity, such as the lacrimal sac when the nasolacrimal sac is blocked (or obstructed). The obstruction may occur as a result of infection, allergy, trauma or tumour, or it may cause the infection as is often the case with dacryocystitis. The patient may present with epiphora, eyelid or periorbital swelling, proptosis but rarely pain unless there is an infection. Treatment involves removal of the mucocele and perhaps construction of a new drainage channel.
mucolytic agent See tears, artificial.
mucopolysaccharidosis type 1 See syndrome, Hurler’s.
mucus A clear viscous secretion of mucous membranes consisting mainly of mucin, as well as inorganic salts suspended in water.
Mueller’s cells See cell, Mueller’s.
Müller–Lyer illusion See illusion, Müller–Lyer.
Müller’s muscle See muscle, ciliary.
Müller’s palpebral muscles See muscles, Müller’s palpebral.
multifocal lens See lens, multifocal.
multiple sclerosis See sclerosis, multiple.
multiple vision See polyopia.
Munsell colour system A system of classification of colours composed of about 1000 colour samples, each designated by a letter and number system. The letter and number of each sample indicate its hue, saturation (called chroma in this system) and brightness (called value). They are represented by a three-dimensional polar coordinate system in which the hue is represented along the circumference, the value along the vertical axis and the chroma along a radius (Fig. M14).
See colorimetry; test, Farnsworth.
Munson’s sign See sign, Munson’s.
muscae volitantes An entoptic phenomenon produced by the presence of remnants of embryonic structures floating within the vitreous humour. They appear like floating spots on a bright uniform background. As they are lighter than the vitreous body they tend to float upward but appear to the patient to move downward because of the reversal of the retinal image. Syn. mouches volantes.
See floaters; image, entoptic; myiodesopia; opacity.
muscarine See acetylcholine; mydriatic.
muscle A contractile organ of the body which produces movements of the various parts or organs. Typically it is a mass of fleshy tissue, attached at each extremity by means of a tendon to a bone or other structure. Muscles are classified according to structure as non-striated (or unstriated or unstriped or smooth) or striated (or striped), by control as voluntary or involuntary, or by location as cardiac, skeletal or visceral.
abducens m. See muscle, lateral rectus.
adducens m. See muscle, medial rectus.
agonistic m. A muscle that performs the desired movement, or does the opposite to an antagonistic muscle. Example: the left lateral rectus is the agonistic muscle when the left eye turns to the left.
See muscle, antagonistic.
antagonistic m. A muscle that opposes the action of another. Example: the right superior rectus muscle is the contralateral antagonist of the left superior oblique.
See muscle, agonistic; muscles, synergistic.
Brücke’s m. See muscle, ciliary.
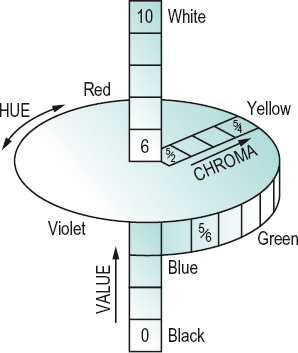
Innervation to the ciliary muscle (mainly parasympathetic fibres derived from the oculomotor nerve) is provided through the short ciliary nerves and stimulation causes a contraction of the muscle. However, a small amount of sympathetic supply is also believed to act and relax the muscle. Blood supply to the ciliary muscle is provided by the anterior and long posterior ciliary arteries. Contraction of the ciliary muscle causes a reduction in its length thus causing the whole muscle to move forward and inward. Consequently the zonule of Zinn, which suspends the lens, relaxes. This leads to a decrease in the tension in the capsule of the lens allowing it to become more convex and thereby providing accommodation. Syn. Bowman’s muscle.
Table M5
Agonistic, antagonistic and synergistic extraocular muscles
| agonist | ipsilateral antagonist | ipsilateral synergist(s) | contralateral synergist |
| lateral rectus | medial rectus | superior oblique | medial rectus |
| inferior oblique | |||
| medial rectus | lateral rectus | superior rectus | lateral rectus |
| inferior rectus | |||
| superior rectus | inferior rectus | inferior oblique | inferior oblique |
| inferior rectus | superior rectus | superior oblique | superior oblique |
| superior oblique | inferior oblique | superior rectus | inferior rectus |
| inferior oblique | superior oblique | inferior rectus | superior rectus |
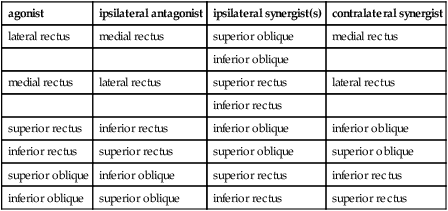
See accommodation, mechanism of; adrenergic receptors; ciliary body; scleral spur; theory, Helmholtz’s of accommodation; Zinn, zonule of.
m. cone A structure formed by the sheath of the four recti muscles as they pass forward from their common origin at the apex of the orbit in the fibrous ring called the annulus of Zinn (and around the optic nerve) to be inserted into the sclera around the eyeball. Some authors consider the muscle cone to include the superior oblique muscle.
See annulus of Zinn.
dilator pupillae m. Smooth (unstriated and involuntary) muscle whose fibres constitute the posterior membrane of the iris. This muscle extends from the ciliary body close to the margin of the iris where it fuses with the sphincter pupillae muscle. Contraction of the dilator pupillae muscle draws the pupillary margin towards the ciliary body and therefore dilates the pupil. This muscle is supplied by the sympathetic fibres in the long ciliary nerves and by a few parasympathetic fibres.
See adrenergic receptors; muscle, sphincter pupillae; mydriatic.
elevator m’s. See muscle, inferior oblique; muscle, superior rectus.
external rectus m. See muscle, lateral rectus.
extraocular m’s. The striated (voluntary) muscles that control the movements of the eyes. There are six such muscles: four recti muscles (lateral rectus, medial rectus, superior rectus and inferior rectus) which move the eye more or less around the transverse and vertical axes, and two oblique muscles (inferior oblique and superior oblique) which move the eyes obliquely. The muscles are composed of striated fibres of varying length, mostly running parallel to the direction of the muscle and united by fibrous connective tissue. They have a greater ratio of nerve fibres to muscle fibres than other striated muscles of the body. The fibre thickness varies from 3 to 50 μm, although functionally there seem to be two main types of fibres, the fast and the slow fibres. The former are the thickest and probably responsible for the fast movements of the eyes (saccades) and the latter consist of thin fibres. The tendons (bands of connective tissue) at one end of each extraocular muscle are attached to bones. This is the origin of the muscle. At the other end of the muscle the tendon is attached to the eye and this area is called the insertion. The substance proper of the muscle is called the belly. Contraction of a muscle occurs in the direction of its constituent fibres and causes a shortening of the muscle. Consequently the eye turns in a given direction depending upon which extraocular muscle is contracting. Contraction results from nervous impulses arriving at the motor end-plate (the junction between an axon and a striated muscle fibre) of the muscle through one of the ocular motor nerves. This causes a neurotransmitter substance to be discharged in the microscopic gap between the end-plate and a muscle fibre. These muscles also possess specialized receptors called muscle spindles, which are small groups of muscle fibres that are provided with both a sensory and a motor nerve supply. There are between 12 and 50 in each muscle. The muscle spindles provide a constant and continuous monitoring of the degree of tension of the muscle itself. Syn. extrinsic muscles; oculorotary muscles.
See cholinergic; fibres, felderstruktur; motor unit; strabismus surgery; test, motility; test, three-step.
extrinsic m’s. See muscles, extraocular.
eyelid retractor m’s. See muscle, levator palpebrae superioris; muscles, Müller’s palpebral.
Horner’s m. A thin layer of fibres that originates behind the lacrimal sac from the upper part of the posterior lacrimal crest (a ridge on the lacrimal bone which borders the fossa for the lacrimal sac). The muscle passes outward and forward and divides into two slips surrounding the canaliculi. It then becomes continuous with the pretarsal portions of the orbicularis muscle of the upper and lower lids and with the muscle of Riolan. Horner’s muscle may be involved in tear drainage through action on the lacrimal sac. Syn. pars lacrimalis muscle; tensor tarsi muscle.
Table M6
Innervation and action of the six extraocular muscles
| muscle | innervation | action in the primary position |
| medial rectus | oculomotor (III) | adduction |
| lateral rectus | abducens (VI) | abduction |
| inferior rectus | oculomotor (III) | depression* |
| adduction extorsion | ||
| superior rectus | oculomotor (III) | elevation adduction intorsion |
| inferior oblique | oculomotor (III) | extorsion elevation |
| abduction | ||
| superior oblique | trochlear (IV) | intorsion |
| depression | ||
| abduction |
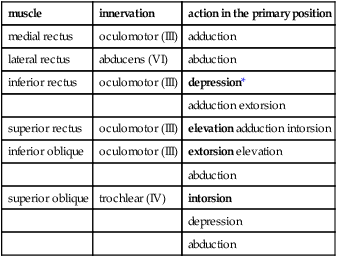
*Bold characters indicate main action.
See muscle of Riolan.
inferior oblique m. (IO) One of the extraocular muscles, it takes its origin at the antero-medial corner of the floor of the orbit. It passes underneath the inferior rectus in a backward direction (making an angle of about 50° with the sagittal plane of the eye), then under the lateral rectus to be inserted by the shortest tendon of all extraocular muscles on the posterior, temporal portion of the eyeball, for the most part below the horizontal meridian, some 5 mm away from the optic nerve. It is innervated by the oculomotor nerve and it extorts (main action), elevates and abducts the eyeball when the eye is in the primary position. Combined with the action of the superior rectus muscle, it directs the eye upward (Fig. M15).
See test, Bielschowsky’s head tilt; test, three-step.
inferior rectus m. (IR) This is the shortest of the four recti muscles. It arises from the lower part of the annulus of Zinn, runs forward, downward and outward (making an angle of about 23° with the sagittal plane) and inserts into the inferior portion of the sclera about 6.5 mm from the corneal limbus. It is innervated by the inferior division of the oculomotor nerve and it depresses (main action), adducts and extorts the eyeball when the eye is in the primary position (Fig. M15).
See annulus of Zinn; muscles, Müller’s palpebral; test, Bielschowsky’s head tilt.
inferior tarsal m. See muscles, Müller’s palpebral.
internal rectus m. See muscle, medial rectus.
intraocular m’s. The smooth (unstriated and involuntary) muscles found within the eye. They are the ciliary, the dilator pupillae and the sphincter pupillae muscles. Syn. intrinsic muscles.
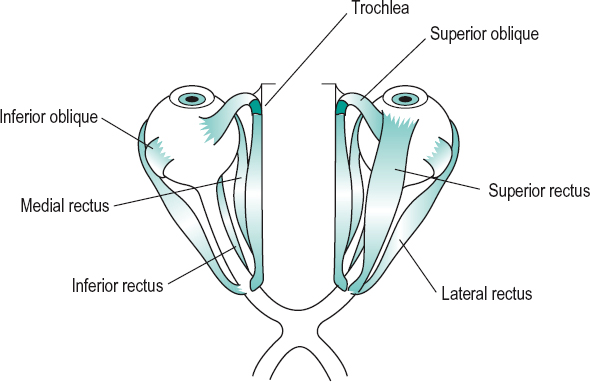
See cholinergic.
Table M7
Intraocular muscles of the eyeball (unstriated muscles)
| name of muscle | nerve supply | action |
| sphincter pupillae | parasympathetic via oculomotor nerve | constricts pupil |
| dilator pupillae | sympathetic via trigeminal nerve | dilates pupil |
| ciliary | parasympathetic via oculomotor nerve | controls shape of lens in accommodation |
lateral rectus m. (LR) One of the extraocular muscles, it arises from both the lower and upper parts of the annulus of Zinn which bridge the superior orbital fissure. The muscle passes forward along the lateral wall of the orbit, crosses the tendon of the inferior oblique muscle and inserts into the sclera about 6.9 mm from the corneal limbus. It is innervated by the abducens nerve and it abducts the eyeball when the eye is in the primary position (Fig. M15). Syn. external rectus muscle; abducens muscle.
See annulus of Zinn; ligament, check.
levator palpebrae superioris m. Striated muscle that arises from the under surface of the lesser wing of the sphenoid bone above and in front of the optic canal. It passes forward below the roof of the orbit and above the superior rectus muscle and terminates in a tendinous expansion or aponeurosis (also called levator aponeurosis), which spreads out in a fan-shaped manner so as to occupy the whole breadth of the orbit and thus gives the whole muscle the form of an isosceles triangle. From the inferior surface of the aponeurosis arises a thin sheet of smooth muscle fibres called Müller’s palpebral muscle (or superior tarsal muscle) which inserts into the posterior margin of the superior tarsal plate and into the superior fornix of the conjunctiva. These smooth muscle fibres are innervated by sympathetic nerves from the superior cervical sympathetic ganglion and assist in elevating the upper eyelid. The fibres of the aponeurosis are attached to the anterior margin of the superior tarsal plate while some fuse with bundles of the orbicularis oculi muscle to attach to the skin. These latter sets of fibres produce the horizontal skin crease of the upper eyelid. The striated levator aponeurosis is innervated by the superior division of the oculomotor nerve and elevates the upper eyelid. Its antagonist is the orbicularis muscle.
See muscle, orbicularis.
medial rectus m. (MR) One of the extraocular muscles, it arises from the medial part of the annulus of Zinn. It passes forward along the medial wall of the orbit and is inserted into the sclera about 5.5 mm from the corneal limbus. It is innervated by the inferior division of the oculomotor nerve and it adducts the eyeball when the eye is in the primary position (Fig. M15). Syn. internal rectus muscle; adducens muscle.
See annulus of Zinn; ligament, check.
Müller’s m. See muscle, ciliary.
Müller’s palpebral m’s. Smooth muscles of the eyelids. The superior one (also called superior tarsal muscle) originates from the under surface of the levator palpebrae superioris muscle and passes below to insert into the upper margin of the tarsal plate of the upper eyelid. The inferior one (also called inferior tarsal muscle) originates from the muscular fascia covering the inferior rectus muscle. It extends upward and inserts into the bulbar conjunctiva and the lower margin of the tarsal plate of the lower eyelid. Müller’s palpebral muscles are innervated by sympathetic fibres and help in lifting the upper eyelid and depressing the lower eyelid. They are sometimes referred to as the eyelid retractors.
oculorotary m’s. See muscles, extraocular.
orbicularis m. A thin oval sheet of striated muscle that surrounds the palpebral fissure, covers the eyelids and spreads out for some distance onto the temple, forehead and cheek. It consists of three portions: (1) The marginal or ciliary portion (muscle of Riolan). (2) The palpebral portion (also called the pars palpebralis muscle) which is the essential part of the muscle and is confined to the lids and may itself be divided into pretarsal portion whose fibres lie in front of the tarsal plates, and the preseptal portion whose fibres extend from the tarsal plates to the orbital margin. The palpebral portion is used in closing the eye without effort or in reflex blinking. (3) The orbital portion (also called the pars orbitalis muscle) which is found in the eyebrow, the temple, the forehead and the cheek. This portion of the muscle is used to close the eye tightly and the skin of the forehead, temple and cheek is drawn towards the inner side of the orbit. The orbicularis muscle is innervated by the facial nerve. Syn. sphincter oculi muscle.
See ectropion; muscle, Horner’s; muscle, levator palpebrae superiotis; muscle of Riolan; myokymia.
pars ciliaris m. See muscle of Riolan.
pars lacrimalis m. See muscle, Horner’s.
pars orbitalis m. See muscle, orbicularis.
pars palpebralis m. See muscle, orbicularis.
pupillary m’s. The dilator pupillae and the sphincter pupillae muscles.
m. of Riolan The ciliary portion of the orbicularis muscle, it consists of very fine striated muscle fibres which lie in the dense tissue of the eyelids near their margin. It is continuous with Horner’s muscle and encircles the eyelid margins mainly between the tarsal glands and the eyelash follicles. Its action is to bring the eyelid margins together when the eyes are closed. Syn. pars ciliaris muscle.
See muscle, Horner’s; muscle, orbicularis.
sphincter oculi m. See muscle, orbicularis.
sphincter pupillae m. Smooth, circular muscle about 1 mm broad, forming a ring all round the pupillary margin near the posterior surface of the iris. It is innervated by parasympathetic fibres of the oculomotor nerve that synapse in the ciliary ganglion and by a few sympathetic fibres. Its contraction produces a reduction in the diameter of the pupil.
See miotics; muscle, dilator pupillae; reflex, pupil light.
m. spindle See muscles, extraocular.
superior oblique m. (SO) This is the longest and thinnest of the extraocular muscles. It arises above and medial to the optic foramen on the small wing of the sphenoid bone. It passes forward between the roof and medial wall of the orbit to the trochlea (which is in the form of a pulley made of fibrocartilage) located at the front of the orbit where it loops over and turns sharply backward, downward and outward (making an angle of about 55° with the sagittal plane), passes under the superior rectus and inserts into the sclera just behind the equator on the superior temporal portion of the eyeball. It is innervated by the trochlear nerve and it intorts (main action), depresses, and also abducts the eyeball when the eye is in the primary position (Fig. M15).
See fossa, trochlear; test, Bielschowsky’s head tilt; test, three-step.
superior rectus m. (SR) One of the extraocular muscles, it arises from the upper part of the annulus of Zinn. It passes forward and outward (making an angle of about 23° with the sagittal plane) and inserts into the sclera about 7.7 mm from the corneal limbus. It is innervated by the superior division of the oculomotor nerve and elevates (main action), adducts, and also intorts the eyeball when the eye is in the primary position (Fig. M15).
See annulus of Zinn; test, Bielschowsky’s head tilt.
synergistic m’s. Muscles having a similar and mutually helpful action as, for example, the inferior rectus and superior oblique muscles in depressing the eyeball.
See Table M5.
superior tarsal m. See muscles, Müller’s palpebral.
tarsal m’s. See muscles, Müller’s palpebral.
tensor tarsi m. See muscle, Horner’s.
yoke m’s. Muscles of the two eyes which simultaneously contract to turn the eyes in a given direction. Example: the medial rectus of the right eye and the lateral rectus of the left eye when turning the eyes to the left.
See law of equal innervation, Hering’s; test, motility; version.
muscular imbalance See imbalance, muscular.
mutation A permanent transmissible change in the nucleotide sequence of the DNA within a gene, or a change in the physical structure of a chromosome. It can occur by substitution (one base or nucleotide is replaced by another), transition (a purine (adenine or guanine) is replaced by another purine or one pyrimidine (cytosine or thymine) is replaced by another pyrimidine), transversion (a pyrimidine is replaced by a purine or vice versa), deletion or insertion of one or more bases. Mutations can also occur in a chromosome as a result of inversion (a segment of chromosome is inserted in reverse order), deletion (a loss of a piece of chromosome) or translocation (a piece of chromosome attaches to another). Mutations result in the formation of a protein with an abnormal amino acid or an absence of the protein and these may result in disease but some mutations may be beneficial. Mutations may be caused by copying errors in the genetic material during cell division, by exposure to ultraviolet or ionizing radiation (X-rays, gamma rays), carcinogens, viruses, or spontaneously.
Table M8
Yoke muscles
| right eye | left eye | version* |
| lateral rectus | medial rectus | to the right |
| medial rectus | lateral rectus | to the left |
| superior rectus | inferior oblique | up and to the right |
| inferior rectus | superior oblique | down and to the right |
| superior oblique | inferior rectus | down and to the left |
| inferior oblique | superior rectus | up and to the left |
*The directions refer to those of the patient.
Table M9
Dimensions of the four recti muscles
| muscle length (mm) | insertion distance from limbus (mm) | tendon length (mm | |
| lateral rectus | 48 | 6.9 | 8.8 |
| medial rectus | 40 | 5.5 | 3.7 |
| inferior rectus | 40 | 6.5 | 5.5 |
| superior rectus | 42 | 7.7 | 5.8 |
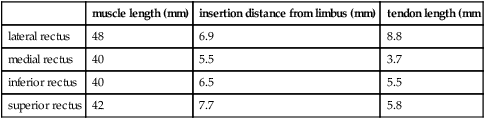
See chromosome; gene.
‘mutton fat’ See keratic precipitates.
myasthenia gravis An autoimmune disease affecting neuromuscular junctions characterized by muscle weakness and fatigability. It is due to a destruction of acetylcholine receptors in the postsynaptic membrane of the neuromuscular junction. In the eye it may result in ptosis, diplopia, keratoconjunctivitis sicca due to improper blinking and consequent dryness of the cornea, and eyelid twitch due to a paresis of the extraocular muscles. Drugs that inhibit acetylcholinesterase (e.g. neostigmine) and prolong the excitatory action of acetylcholine are used in the treatment of this disease.
See dysmetria, ocular; ophthalmoplegia, chronic progressive external; sign, Cogan’s lid twitch.
mycophthalmia A conjunctivitis caused by a fungus. The term is sometimes used to refer to inflammation of the whole eye.
See keratitis, fungal; uveitis, fungal.
mydriasis 1 . Dilatation of the pupil. 2. The condition of an eye having an abnormally large pupil diameter (5 mm in daylight). The condition may be due to a paralysis of the sphincter pupillae muscle, to an irritation of the sympathetic pathway, to a drug (e.g. atropine, homatropine), or to adaptation to darkness.
See miosis; muscle, dilator pupillae; mydriatic; pupil.
mydriatic 1 . Causing mydriasis of the pupil. 2. A drug which produces mydriasis. Mydriatics are used to carry out a thorough inspection of the fundus and lens, especially in elderly patients in whom the pupils are usually smaller. However, in older people it must be ascertained that the patient does not have glaucoma. There are two classes of mydriatics: (1) antimuscarinic (parasympatholytic, anticholinergic, atropine-like) drugs which antagonize the action of acetylcholine at muscarinic receptors in the ciliary muscle, such as atropine, cyclopentolate, homatropine, hyoscine (scopolamine) and tropicamide. Antimuscarinic drugs produce cycloplegia as well. (2) sympathomimetic (adrenergic stimulating) drugs which directly or indirectly stimulate the dilator pupillae muscle which is innervated by the sympathetic division of the autonomic nervous system. These include cocaine, ephedrine hydrochloride, adrenaline (epinephrine), naphazoline and phenylephrine hydrochloride.
See adrenergic receptors; cholinergic; cycloplegia; miotics; muscle, dilator pupillae; mydriasis; reflex, pupil light; sympathomimetic.
myectomy The excision of a portion of a muscle. It is done to decrease the effective action of an extraocular muscle in the correction of strabismus.
See myotomy; strabismus surgery.
myelinated nerve fibres See fibres, myelinated nerve.
myiasis An infection or infestation of tissues or cavities by larvae of flies. In the eye (called ophthalmomyiasis or ocular myiasis) the larvae may affect the ocular surface, the conjunctival sac, the intraocular tissues or occasionally the deeper orbital tissues. Treatment consists of the mechanical removal of the larvae following topical anaesthesia.
myoclonus, ocular Bursts of pendular eye movements normally associated with lesions in the midbrain.
See flutter, ocular; opsoclonus.
myiodesopsia The perception of spots passing across the visual field, such as muscae volitantes or floaters. Note: also spelt myiodeopsia, myodesopsia.
myodioptre The contractile power of the ciliary muscle such that it induces an increase in the accommodation of the eye of 1 D.
See dioptre.
myoid See ellipsoid.
myokymia Twitching of a few bundles of fibres of the eyelid muscle. It occurs most commonly when fatigued, sometimes on exposure to cold, and in some pathological cases (e.g. multiple sclerosis) in which case the entire muscle is involved. Superior oblique myokymia can often be diagnosed by noting fine torsional nystagmus of the affected eye on slit-lamp examination. In cases where no nystagmus is noted, a patient’s history of monocular episodic oscillopsia, associated with vertical diplopia, may be sufficient to make a diagnosis. The use of carbamazepine or propranolol has been suggested as possible treatments in stopping the myokymia.
See muscle, orbicularis; sclerosis, multiple.
myopathy, ocular See ophthalmoplegia.
myopathy, restrictive See disease, Graves’.
myope A person who has myopia.
Table M10 Approximate relationship between uncorrected myopia and visual acuity

myopia (M) Refractive condition of the eye in which the images of distant objects are focused in front of the retina when the accommodation is relaxed. Thus distance vision is blurred. In myopia the point conjugate with the retina, that is the far point of the eye, is located at some finite point in front of the eye (Fig. M16). The percentage of myopes in Caucasian populations is about 24–28%, it is much higher among Chinese (70–80%). Syn. nearsight; short sight.
See gene-environment interaction; keratectomy, photorefractive; orthokeratology; pseudomyopia; retina, lattice degeneration of the; syndrome, Marfan’s; theory, use-abuse.
acquired m. Myopia appearing after infancy, or in adulthood. Almost all myopias are acquired. Those myopias developing in the late teens and adulthood are usually referred to as late-onset myopia (or adultonset myopia), whereas those occurring earlier are often referred to as early-onset myopia (or juvenile-onset myopia).
m. control Term used to encompass the various methods aimed at slowing or arresting the progression of myopia. They include bifocals, contact lenses, pharmaceutical agents, incorrect single vision lenses (undercorrection, overcorrection), vision therapy and feedback strategies. None has yet been found to be reliably effective.
degenerative m. See myopia, pathological.
early-onset m. See myopia, acquired.
empty-field m. See myopia, space.
false m. See accommodation, spasm of.
form-deprivation m. Myopia developing in children when the retina is stimulated by a blurred image during the critical period of development. It may occur as a result of a pathological condition, such as cataract, vitreous haemorrhage, ptosis, eyelid closure, or in inordinately long occlusion therapeutic sessions.
See period, critical; occlusion therapy.
high m. Myopias above 6.0 D or more are usually considered as high myopias.
See glaucoma, open-angle; lens, high index; myopia, pathological.
Table M10
Approximate relationship between uncorrected myopia and visual acuity
| Snellen visual acuity | ||
| myopia | (m) | (ft) |
| –0.0 D | 6/600 | 20/2000 |
| –6.00 D | 6/232 | 20/775 |
| –5.00 D | 6/170 | 50/565 |
| –4.00 D | 6/126 | 20/420 |
| –3.00 D | 6/85 | 20/285 |
| –2.50 D | 6/68 | 20/225 |
| –2.00 D | 6/50 | 20/165 |
| –1.50 D | 6/33 | 20/110 |
| –1.00 D | 6/20 | 20/65 |
| –0.50 D | 6/9 | 20/30 |
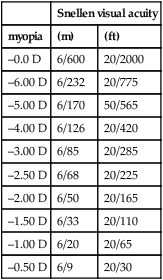
Table M11
Common ocular and systemic diseases with myopia as an associated sign
| Marfan’s syndrome | retinopathy of prematurity |
| Ehlers-Danlos syndrome | Stargardt’s disease |
| Down’s syndrome | homocystinuria |
| Cornelia de Lange syndrome | choroideremia |
| Weil–Marchesani syndrome | gyrate atrophy |
| Laurence–Moon–Bardet– Biedl syndrome | rod monochromat |
| Riley–Day syndrome | ectopia lentis |
| Turner’s syndrome congenital stationary night blindness | Fabry’s disease |
| Stickler’s syndrome pigment dispersion syndrome | Wagner’s syndrome |
hypertonic m. See accommodation, spasm of.
index m. See myopia, lenticular.
instrument m. A temporary increase in accommodation induced by looking through an optical instrument.
See accommodation, resting state of.
juvenile-onset m.; late-onset m. See myopia, acquired.
lenticular m. Myopia attributed to an increase in the index of refraction of the lens. As a result there is an increase in refractive power. Such a change usually accompanies the development of some cataracts. This type of myopia may also accompany or follow an increase in blood sugar level, in which case it is usually of a transient nature, i.e. the power of the crystalline lens diminishes after the blood sugar level returns to normal. Syn. index myopia.
See cataract, nuclear; diabetes; microspherophakia.
low m. Myopias of 3.0 D or less are usually considered as low myopias.
malignant m. See myopia, pathological.
medium m. Myopias between 3.0 and 6.0 D are usually considered as medium myopias.
night m. An increase in ocular refraction (essentially accommodation) occurring at low levels of illumination.
See accommodation, resting state of.
pathological m. Myopia attributed to retinal and choroidal degeneration resulting from excessive elongation of the eye. The myopia usually exceeds 8–10 D, tends to increase rapidly during adolescence and continues to increase during adulthood. Visual acuity is usually subnormal after correction. Pathological myopia is a potential cause of blindness. Syn. degenerative myopia; malignant myopia; progressive myopia.
See choroideremia; crescent, myopic; macular hole; retinal detachment; sclerochoroiditis; spot, Fuchs’; staphyloma, anterior; vitreous detachment.
physiological m. This is the most common type of myopia. It is believed that high myopia is due mainly to genetic factors whereas low myopia is more likely due to environmental influences. It occurs because of a failure in correlation of the refractive power of lens and cornea, and the length of the eye. Thus, the power of the eye is too great for its length. Unlike pathological myopia, this myopia usually stabilizes when the growth process has been completed. It is associated with normal visual acuity after correction. Syn. simple myopia; typical myopia.
progressive m. See myopia, pathological.
senile lenticular m. See sight, second.
simple m. See myopia, physiological.
space m. An increase in accommodation occurring when viewing a field without any stimuli to accommodation as, for example, a clear sky. Syn. empty-field myopia.
See accommodation, resting state of.
spurious m. See accommodation, spasm of.
typical m. See myopia, physiological.
myopic conus; crescent See crescent, myopic.
myopic defocus See defocus, myopic.
myopigenic Pertains to factors causing myopia. They are: genetic predisposition which includes ethnicity and a family history of high myopia; visual experiences, such as prolonged reading and extensive near work; and diseases such as congenital cataract, congenital ptosis and haemangiomas of the eyelids and orbit.
myosis See miosis.
myotomy The surgical division or dissection of a muscle. It is done to reduce the pull of an extraocular muscle in the correction of strabismus.
See myectomy; strabismus surgery.
myotonic dystrophy; pupil See under the nouns.






