Lymph Node Sampling
In contrast to a complete lymphadenectomy (see Unit 1, Chapter 12), selective lymph node sampling is performed during simple hysterectomy for women who have been diagnosed with adenocarcinoma of the endometrium (see Unit 1, Chapter 13).
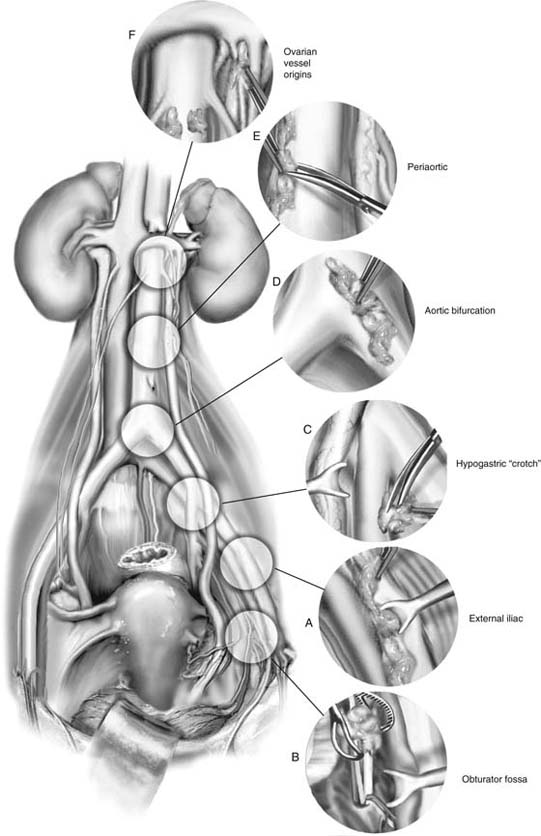
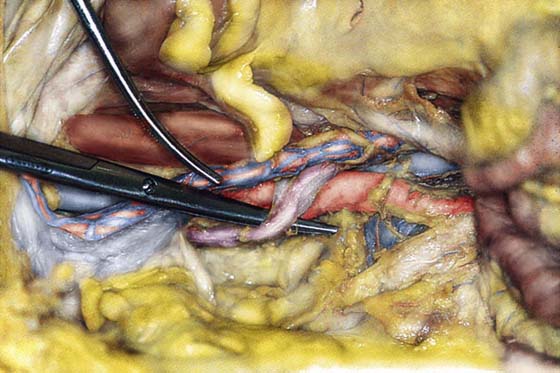
The lymph nodes typically sampled include the external iliac, internal iliac, common iliac, obturator, and periaortic nodes. These lymph nodes are closely associated with the large arteries and veins of the pelvis (Fig. 40–1).
The external iliac node sample is obtained by retracting the external iliac artery and removing some of the fatty tissue between the artery, the external iliac vein, and the lateral boundary formed by the psoas major muscle (Figs. 40–2A, 40–3 through 40–5).
The vein retractor is moved to the external iliac vein, which is gently elevated. Then with the use of ring pick-ups, some of the node-containing fatty tissue of the obturator fossa is teased away from around the obturator nerve (see Figs. 40–2B, 40–6 through 40–9).
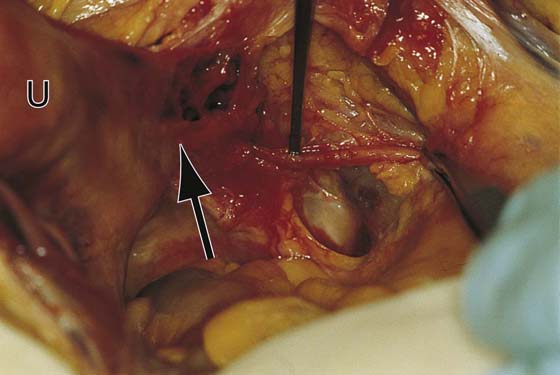
Next, nodal tissue is excised from the hypogastric artery where it joins the external iliac artery to form the common iliac artery. Here the ureter must be identified and retracted medially to gain exposure (Figs. 40–2C and 40–10).
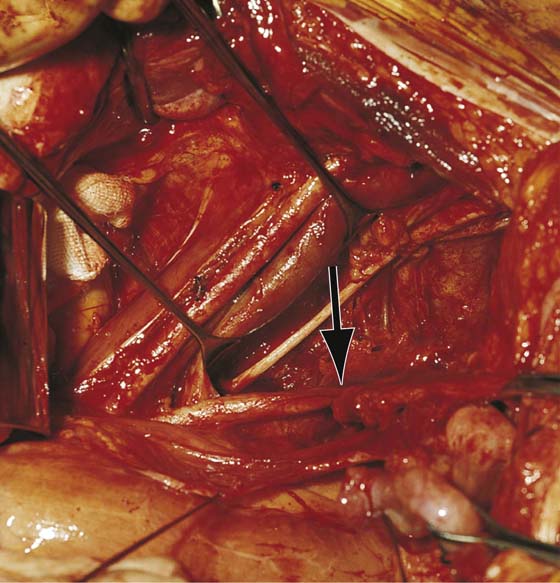
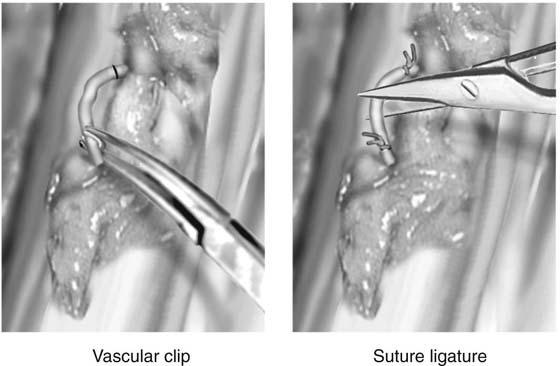
The tissue at the junction of the common iliac arteries and the aorta is sampled next (Figs. 40–2D and 40–11). Periaortic nodes are excised above the level of the takeoff of the inferior mesenteric artery (Figs. 40–12 and 40–13). The fat between the aorta and the inferior vena cava is carefully dissected and sampled (see Fig. 40–2E). When fatty tissue containing lymphatic tissue is cut, it typically bleeds. Therefore, when retroperitoneal lymph node sampling is performed, vascular clips should be applied to secure the small venules and arterioles (Fig. 40–14). Occasionally, it may be necessary to use a 3-0 or 4-0 Vicryl as a suture-ligature to achieve appropriate hemostasis (see Fig. 40–14).
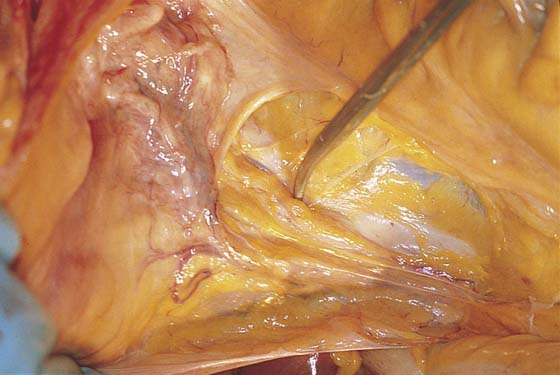
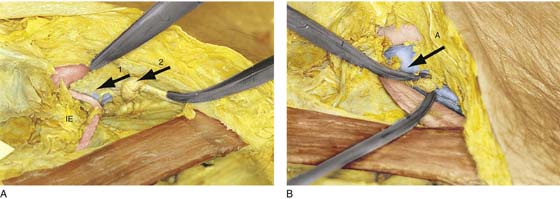
Sampling should continue upward to the origin of the ovarian arteries from the aorta and of the ovarian veins from the vena cava and left renal vein areas (see Fig. 40–2F). For vulvar carcinoma, the lowest node in the external iliac chain is sampled. This can be done extraperitoneally by locating the inferior epigastric artery and tracing it to the iliac vessels at the point where the vessels cross under the inguinal ligament. The node is located just medial to the external iliac vein and lies in the femoral canal (Fig. 40–15A, B).
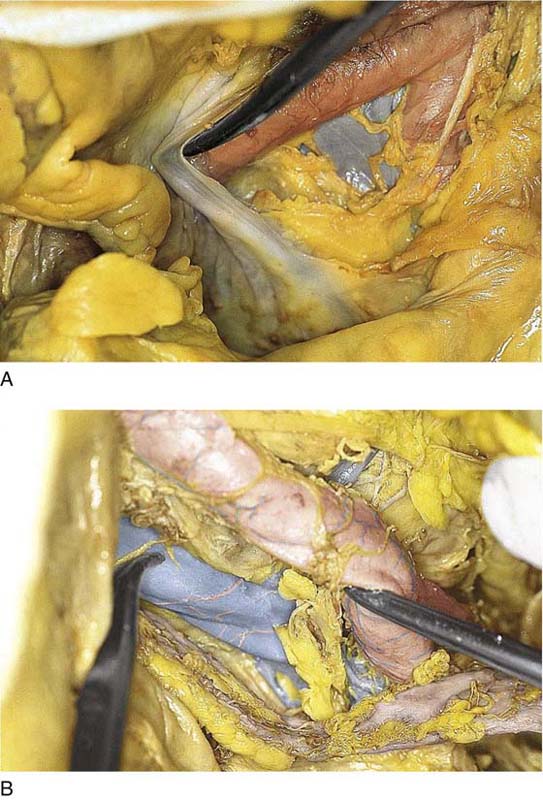
FIGURE 40–1 A. The peritoneum has been opened at the bifurcation of the right common iliac artery. The fat overlying the iliac arteries and veins contains lymphoid tissue. B. This clump of lymph nodes lies between the external iliac artery and vein. The scissor tip slightly elevates the external iliac artery; the clamp points to the external iliac vein. The ureter is in the foreground.
FIGURE 40–2 A. The external iliac artery is retracted with a vein retractor to allow the node-containing fat to be excised between the artery and the underlying external iliac vein. B. The obturator fossa is exposed by gently elevating the external iliac vein with a vein retractor. The fat is carefully teased out of the fossa with a ring forceps, and the obturator nerve and artery are exposed. C. The external iliac artery is followed cranially to reach its junction with the hypogastric artery. Fat is cleared from the crotch by sharp and blunt dissection. Care is taken to retract the ureter and to avoid injury to the underlying veins. D. The bifurcation of the aorta is located, and nodes are sampled between the aorta and vena cava and between the aortic bifurcation and the left common iliac vein. E. Periaortic nodes are sampled at and above the origin of the inferior mesenteric artery. The ureter lies close to the aorta on the left side and should be identified if the dissection carries over to the left side of the aorta. F. The ovarian arteries take origin from the aorta just below the renal arteries. Fat and nodes between these vessels typically are sampled at the upper limits of the dissection. Note that the left ovarian veins drain into the left renal vein and override the ureter.
FIGURE 40–3 A. The infundibulopelvic ligament on the left side has been triply clamped. After the ligament is divided and the incision made following division of the round ligament is connected, the psoas muscle and the external iliac artery can be exposed easily. B. The lateral portions of the round ligament have been ligated and the infundibulopelvic ligament has been ligated for retraction (arrows). Fatty node-bearing tissue is dissected from the external iliac artery.
FIGURE 40–4 The tonsil clamp is used to dissect fat and lymph nodes from the external iliac artery.
FIGURE 40–5 Metzenbaum scissors dissect the lymphatic tissues between the external iliac artery and vein.
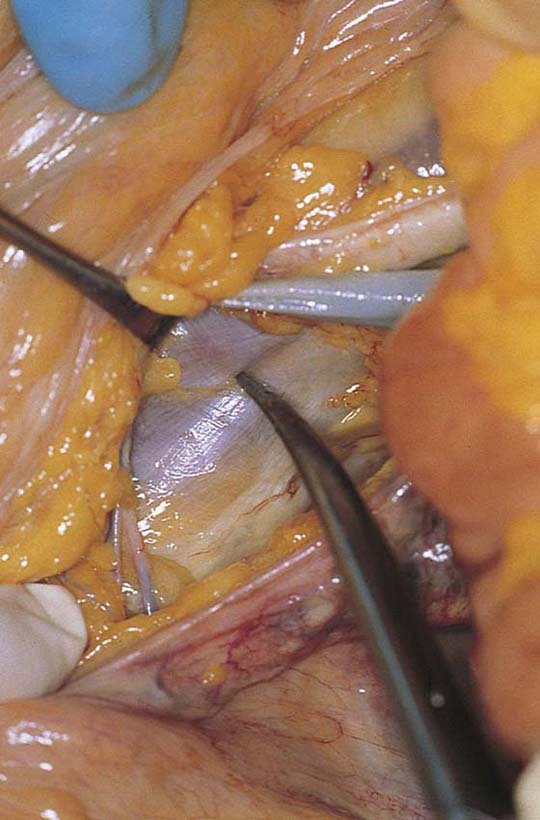
FIGURE 40–6 A vein retractor exposes the obturator fossa by retracting the external iliac vein upward.
FIGURE 40–7 The lateral border of the obturator fossa is made up of the obturator internus muscle.
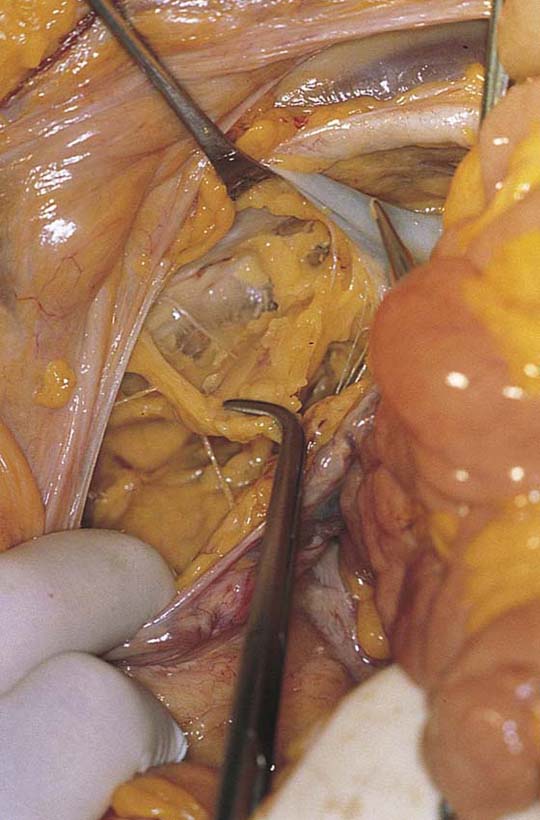
FIGURE 40–8 The instrument is placed under the ureter to identify its position relative to the obturator fossa. The arrow points to the cardinal ligament. U, uterus.
FIGURE 40–9 The obturator fossa has been cleared of fat and nodes. The obturator nerve is clearly seen crossing the fossa. The arrow points to the hypogastric artery. The ureter is pulled medially by a suture placed at the peritoneal edge. (From Baggish et al: In Diagnostic and Operative Hysteroscopy, 2nd ed. Mosby, St. Louis, 1999, with permission.)
FIGURE 40–10 The scissors lie beneath the ureter as it crosses the common iliac artery.
FIGURE 40–11 The aortic bifurcation has been exposed. Fatty node-bearing tissue lies beneath the iliac arteries and the left common iliac vein.
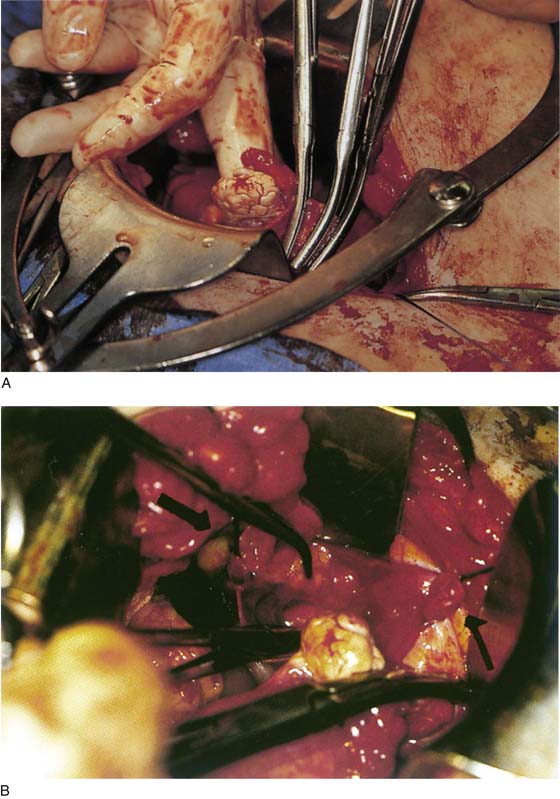
FIGURE 40–12 The sigmoid colon has been pulled to the left. The peritoneum is opened and the fat is cleared to expose the aortic bifurcation and the inferior mesenteric artery.
FIGURE 40–13 The arrow points to the fully dissected inferior mesenteric artery.
FIGURE 40–14 Small arteries and veins are typically encountered during lymphadenectomy. These may be clipped or, alternatively, clamped and ligated with 3-0 or 4-0 Vicryl.
FIGURE 40–15 A. The left rectus abdominis muscle is seen in the foreground. The transversalis fascia covers the peritoneum and has a slate blue color. The inferior epigastric (IE) vessel can be seen originating from the external iliac artery. The scissors point to the iliac artery just before it passes beneath the inguinal ligament. Arrow 1 points to the external iliac vein. Arrow 2 points to Cloquet’s node. The curved clamp rests on the inguinal ligament. B. Letter A is directly caudal to the external iliac artery. The arrow points to the external iliac vein. The lymph node is between the clamp and the scissors at the top of the femoral canal.