Corpus Luteum and Hemorrhagic Cyst
Synonyms/Description
Etiology
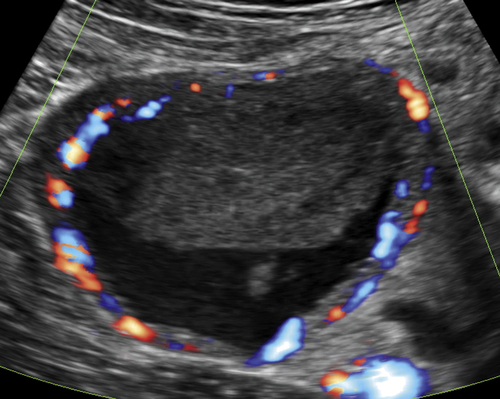
Ultrasound Findings
Differential Diagnosis
Clinical Aspects and Recommendations
Figures
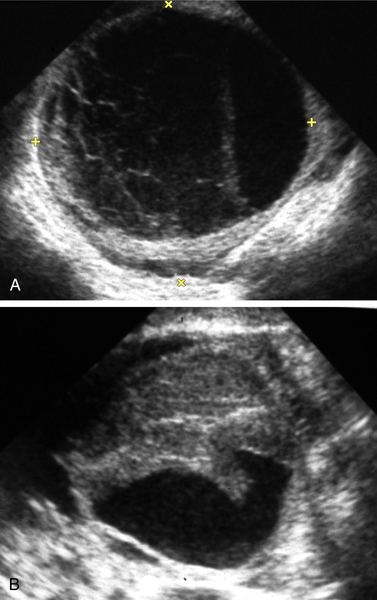
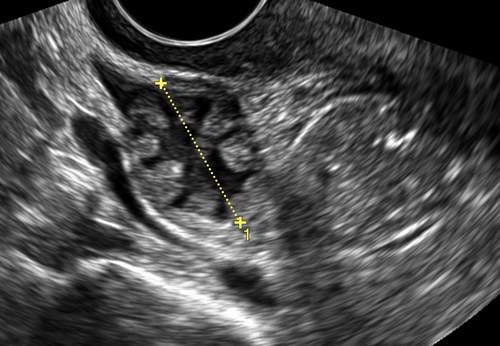
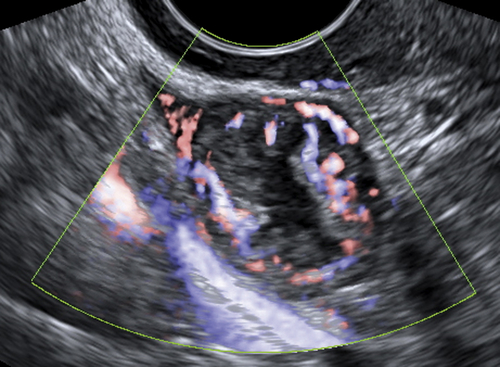
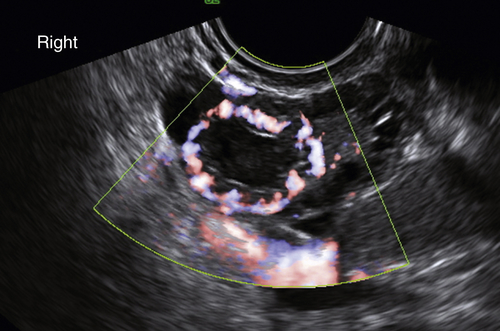
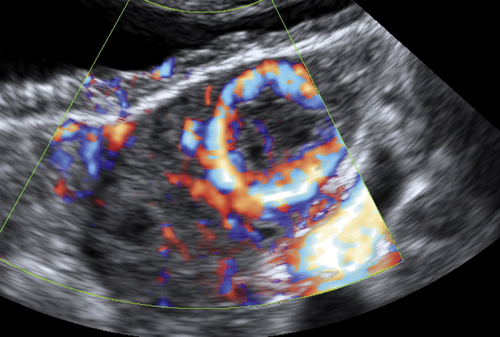
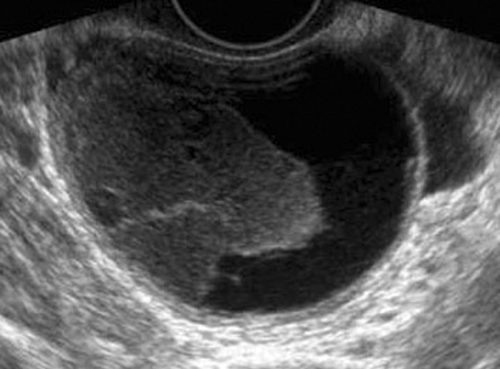
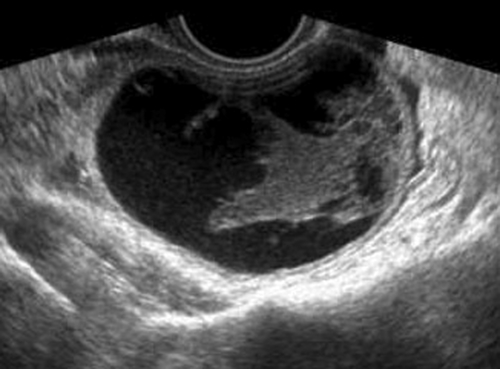
Figure C3-4 Two different cases of hemorrhagic cysts with retracting clot. A, The typical reticular or fishnet internal structure consistent with a retracting clot. B, A more solid internal structure of the cyst. Note that the solid areas are retracting toward the periphery of the cyst rather than growing into the center, as would a neoplasm. No flow was seen within the clot.
Suggested Reading
Guerriero S., Ajossa S., Melis G.B. Luteal dynamics during the human menstrual cycle: new insight from imaging. Ultrasound Obstet Gynecol. 2005;25:425–427.
Jain K.A. Sonographic spectrum of hemorrhagic ovarian cysts. J Ultrasound Med. 2002;21:879–886.
Parsons A.K. Imaging the human corpus luteum. J Ultrasound Med. 2001;20:811–819.
Stein M.W., Ricci Z.J., Novak L., Roberts J.H., Koenigsberg M. Sonographic comparison of the tubal ring of ectopic pregnancy with the corpus luteum. J Ultrasound Med. 2004;23:57–62.
Swire M.N., Castro-Aragon I., Levine D. Various sonographic appearances of the hemorrhagic corpus luteum cyst. Ultrasound Q. 2004;20:45–58.